4
Systems and processes for ensuring acceptable standards of care and safety and promoting continuous improvement
| 7 pillars of clinical governance |
|---|
| Patient and Public Involvement |
| Information and IT |
| Risk Management |
| Audit |
| Training/Education |
| Clinical Effectiveness |
| Staff Management |
Clinical Governance Lead
Practice Clinical Governance Lead
accountable and responsible for:
Providing and encouraging appropriate education and training
Managing audit and acting on the outcomes
Risk management
Positive Critical Event Analysis
Identifying, reporting and managing poor performance
Ensuring that the wider MDT is involved in a structured appraisal system.
PCO Clinical Governance Lead
accountable and responsible for:
To champion a culture of high quality care across the PCT
To work with PCT Executive Directors to ensure delivery of the PCT’s Clinical Governance Strategy
Ensuring robust commissioning arrangements including ensuring quality of care.
Providing and encouraging appropriate education and training opportunities
Identification of good and poor performance
Facilitating change of poor performing services
Provision of incentives and penalties relating to service quality
Quality assurance
Quality improvement
QI (pdf) S Pairojkul Khon Kean University
Formal approach to the analysis of performance and systematic efforts to improve it.
examples PDSA Six Sigma CQI TQM
Aims to improve quality and efficiency and reduce errors.
examples
• Are we creating an environment encouraging clinicians to report errors?
• Which staff member failed to transfer the call to the correct extension?
• How do we reduce production errors on the widget line?
• Patient had a bad outcome; were the doctors or nurses at fault?
• What could we do to increase the efficiency of chart filing?
Postgraduate medical education accreditation and QI
• Practice-Based Learning and Improvement that involves investigation and evaluation of their own patient care, appraisal and assimilation of scientific evidence, and improvements in patient care
• Systems-Based Practice, as manifested by actions that demonstrate an awareness of and responsiveness to the larger context and system of health care and the ability to effectively call on system resources to provide care that is of optimal value
QI for primary care providers in private practice?
• Providing “best” or “better care” in a consistent manner
• “Right” treatment in accordance with established guidelines
• Assessing current level, looking for effects, and designing better systems
Barriers to QI in primary care
• Cost, time, staffing, data-gathering/retrieval, unreasonable expectations
• Clinical inertia, “system” constraints,acute problem orientation
• Physician misconceptions/traps
Parallelisms
The Scientific Method Caring for Patients
Quality Improvement
hypothesis chief complaint problem
Do research, gather data
Do a history and physical, gather data
Set up a project team, gather data
Develop tentative conclusions
Develop a working diagnosis
Develop a tentative set of causes to be addressed
Make the conclusions available to others
Enact an initial treatment plan
Introduce a pilot improvement plan
Others validate and build upon conclusions
Follow up and adjust treatment
Gather data and adjust improvements
Continue the above indefinitely
http://www.youtube.com/watch?v=_gb4CUo3btA
| Clinical guidelines |
|---|
NICE
National Institute of Clinical Excellence
Government sponsored agency charged with examining evidence base for medical interventions and developing guidelines based on evidence for efficacy and affordability.
NICE guidelines have been criticised as being over-complex, not grounded in everyday practice and over-biased towards cost-containment, and slow to endorse new treatments
a camel is a horse designed by a committee
When NICE approves a treatment, PCTs or CGGs should not be able to deny that treatment to their patients – although this may be no longer when the new NHS bill becomes law
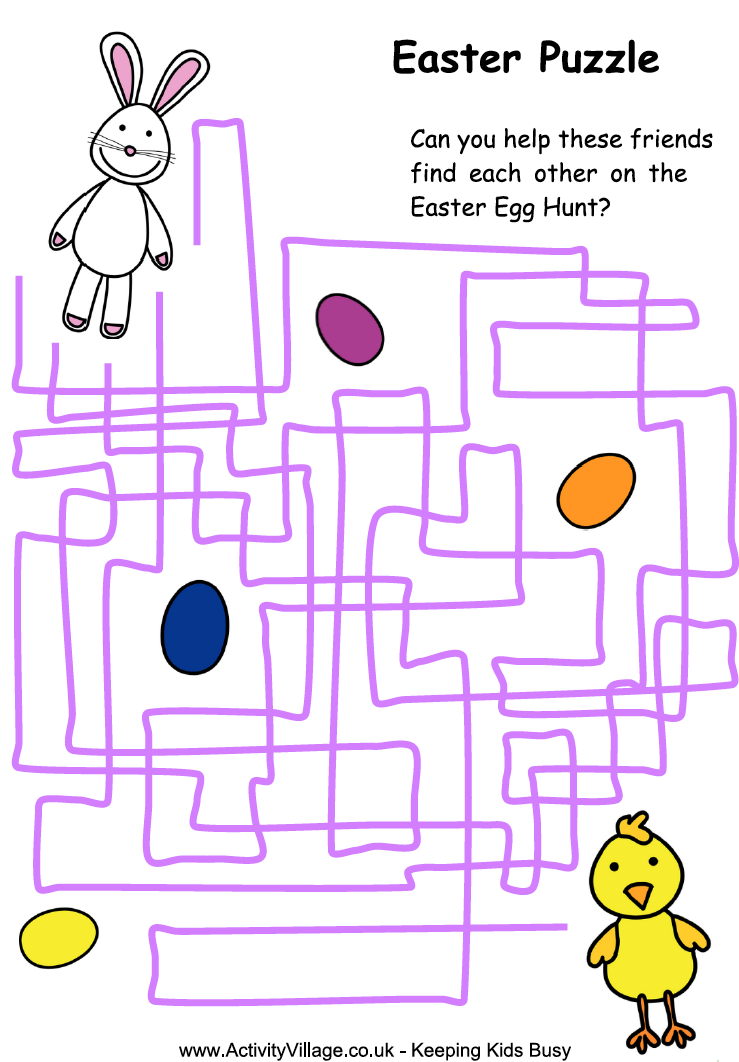
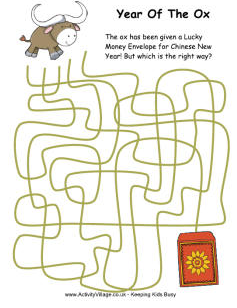
The NICE website has been revamped and NICE Pathways is almost navigable – if you’re the type who likes those puzzles where 3 or 4 eskimos are sat round a hole in the ice and you have to trace with your finger which one of their tangled lines leads to the fish.
- NICE Clinical Guidelines
- NICE TAs – mainly latest drugs between CG updates
- NICE Bites NHS East Lancs
- SIGN – Scottish Intercollegiate Guidelines Network
- Office of Health Economics
- http://youtu.be/Y3oTetctHKU
| Clinical audit | |
|---|---|
| Measuring performance against defined standards with a view to improving care | |
| 1 | Preparation Identify problem and local resources for audit Choose something which interests you. Choose audit topics based on importance /interest eg high risk, high volume, or high cost problems, or on national clinical audits, national service frameworks, or guidelines from the National Institute for Health and Clinical ExcellenceAudit can include assessment of structure process or outcome: eg resources such as the use of GPwSI clinics or complex chronic disease management services. eg waiting times in the Practice or availability of appointments. eg blood pressure reduction in response to therapy.Try to reduce the question you wish to answer to a single sentenceHigh volume—such as requests for appointments, antibiotics, Xrays or blood tests by patients. High risk to staff—such as needle stick injuries. High risk to patients—such as certain treatment complications or side effects. High cost—such as new non generic drugs. Involve patients in choosing priorities |
| 2 | Select criteria Derive standards from good quality sources – local or national guidelines NICE, SIGN Criteria should be SMART (specific, measurable, achievable, reliable, timely) |
| 3 | Data Collection Define the patients to be included and excluded, the audit criteria, and the time period |
| 4 | Data Analysis Compare results with criteria and standards Conclude how well the standards were met If they were not met, identify reasons for this. Use action plans which identify those responsible for specific aspects. |
| 5 | Sustaining improvements Rinse and Repeat Repeat the audit after an agreed period to find out whether improvements in care have been implemented/achieved. |
| http://youtu.be/q4xrfH9AeTs | |
Eight Stage Clinical Audit
Audit vs Research
Research: “what is the right thing to do?” = finding new knowledge
Clinical audit “are we applying that knowledge appropriately?”
Information governance
| Data Protection Act 8 principles |
|---|
| personal data must be: |
| 1 Processed fairly and lawfully |
| 2 Obtained for specified and lawful purposes |
| 3 Adequate, relevant and not excessive |
| 4 Accurate and up to date |
| 5 Not kept any longer than necessary |
| 6 Processed in accordance with the “data subject’s” (the individual’s) rights |
| 7 Securely kept |
| 8 Not transferred to any other country without adequate protection in situ |
Information Governance (UC)
For all types of records, all staff working in offices where records may be seen must:
• Wear building passes/ID badges.
• Know who to tell if anything suspicious or worrying is noted.
• Only take essential notes/records/documents out of Urgent Care 24 premises.
• Lock any equipment or data out of sight in the boot of your car if not required for that visit.
• Ideally all records should be returned to base at the end of the day but if this has not been possible, any equipment or data must be removed from your vehicle at night.
Manual records must be:
• Stored securely within the Walk in Centre or office.
• Stored closed when not in use so that contents are not seen.
• Locked so that all sensitive/confidential data out of sight when leaving your desk/office space
• Inaccessible to members of the public and not left unattended, even for short periods where they might be looked at by unauthorised persons.
• Handwritten notes for disposal must be taken back to base and shredded – they must not disposed of in personal domestic waste.
With electronic records, staff must:
• Never reveal passwords to others.
• Always lock your computer before leaving your desk.
• Always log-out of any computer system or application when work on it is finished.
• Change passwords at regular intervals to prevent anyone else using them.
• Use an Urgent Care 24 approved encrypted memory stick/device.
• Never use non-Urgent Care 24 storage devices (such as USB sticks) on your Urgent Care 24 computer.
• Always clear the screen of a previous patient’s information before seeing another.
Know your Policies: All staff are contractually expected to be familiar with and comply with Urgent Care 24 policies and procedures in relation to Information Governance. These policies include:
• Information Governance
• Information Security
• Internet and Email
• Confidentiality and Data Protection
| Caldicott Principles |
|---|
| Guidelines for Social Care and Health professionals regarding the use of person-identifiable and confidential information. |
| Justify the purpose(s) of using personidentifiable and confidential information |
| Only use it when absolutely necessary |
| Use the minimum that is required |
| Access should be on a strict need-to-know basis |
| Everyone must understand his or her responsibilities |
| Understand and comply with the law |
Information commissioner
Independent public body set up to promote access to official information and protect personal information by promoting good practice, ruling on eligible complaints, providing information to individuals and organisations, and taking appropriate action when the law is broken.
Enforces and oversees Data Protection Act, Freedom of Information Act, Environmental Information Regulations, and Privacy and Electronic Communications Regulations.
| CQC |
|---|
| Regulators of health and adult social care services in England, including NHS, local authorities, private companies or voluntary organisations., also people detained under the Mental Health Act.Focus on equalities and human rights, and pay particular attention to the needs of people in more vulnerable circumstances. |
| Four main activities Registration and enforcement (of all NHS and private Health & Social Care providers) Improving health and social care Mental Health Act visits Reporting health and social care information |
| NHS complaints | |
|---|---|
| Stage1 | Local Resolution – practice or PCT tries to resolve the complain |
| Stage2 | complainant asks for an Independent Review by the Healthcare Commission |
| Complaints Procedures/Policy |
|---|
| Responsibility for complaints One person should be nominated to manage complaints. Depending on the nature of the complaint, the complaints manager will attempt to resolve the matter to the satisfaction of the complainant. |
| Publicising the procedure The practice’s complaints procedure should be publicised to your patients so they know how the procedure works, including details of the conciliation service, ICAS, the HCC and the Health Service Ombudsman. |
| Who can complain?A complaint can be made by a patient or person affected, or likely to be affected, by the action or decision of an NHS organisation or primary care practitioner. A complaint can also be made by someone acting on behalf of the patient or person with their written consent.Possible claims for compensation are excluded from the NHS complaints procedure – contact Defence Organisation if this seems possible/likely |
| Confidentiality issues You must ensure that the patient has given their written consent before you can disclose clinical information to a third party. It can be a complex matter, particularly if the patient has died, was a child or an adult without capacity: in which case we advise you to contact MPS for further advice. |
| Receiving and acknowledging complaints All complainants should be contacted within three working days to acknowledge that their complaint has been received, explain the procedure and, where necessary, clarify any issues arising from the complaint. A full response should be provided within ten working days in primary care and within 25 working days in a hospital setting. If a complaint is made verbally and documented by the practice, the complainant should be asked to confirm in writing that they agree with what has been recorded. |
| Replying to the complainant The way a response is written, or the way a meeting is conducted, can often be the deciding factor as to whether or not a complaint proceeds further. Sometimes acknowledging that the person’s feelings of frustration, anger or emotion at what happened are real and understandable, regardless of whether the complaint is justified or not, and is often enough to defuse the situation. The complaints manager should inform the complainant of the results of the investigation in writing. This should include a detailed account of what happened. It should also include an apology, full explanation of events, lessons learned and reassurance of any changes which might be implemented in the future. |
| Time limits Normally a complaint should be made within six months of the incident that caused the problem, or within six months of the complainant discovering the problem – as long as this is not more than one year after the event. However, you can extend the time limits, where it would be unreasonable to expect the complaint to have been made earlier. |
| Deputising and out-of-hours services Where there is a complaint against a deputising doctor, it can be made directly to the deputising service, or the practice may make the complaint on behalf of the complainant. The registered GP would not necessarily be involved in the investigation at all, though he/she should be told of the complaint out of courtesy. If the practice had opted out of providing out of hours service, the trust is responsible for ensuring that the complaint is investigated. |
| Locums and trainees Complaints against locums or doctors in training should be investigated by the practice and, if they have left the practice, the doctors concerned contacted if possible for their comments. |
| Records A separate file must be kept for complaints records; these should not be included in the patient’s medical records. Clear and accurate documentation is essential for complaints handling. In cases where a complaint has been resolved by the practice procedures, the practice should keep records of complaints for ten years – the same length of time as for litigation. This should include copies of all correspondence between the complainant and the practice, but not draft documentation unless you are prepared for the possibility that this might be disclosed in the future. |
| Conciliation You may wish to consider using the PCT’s free conciliation service, whereby they appoint an independent person to facilitate a discussion or meeting. Please contact your local PCT for further information. http://youtu.be/_lgrNmpT7W4 |
PALS
Patient advcocay and liason service
Advocacy service offering NHS patients, families and carers advice and support with health-related questions, concerns or problems including complaints, and advice on how to get more involved in their own healthcare
Health Service Ombudsman
Statutory body which can indipendantly investigate complaints about the NHS (in England) if complainant dissatisfied with outcome of local resolution procedures. Does not cover private care/treatment unless paid for by the NHS.
Complaints should usually go to the ombudsman within a year of when the claimant became aware of the problem. The time limit can be extended in special circumstances, such as where the local complaints procedure took longer than it should have done.
- the wrong treatment
- poor treatment
- errors in diagnosis or treatment
- significant mistakes over appointments to see a doctor or go to hospital
- failure to provide or pay for a service such as continuing care
- delay that could have been avoided
- faulty procedures, or failing to follow correct procedures
- unfairness, bias or prejudice
- giving advice which is misleading, or inadequate
- rudeness, and not apologizing for mistakes
- not putting things right when something has gone wrong
- The Ombudsman is cannot investigate complaints subject to legal action.
http://hacking-medschool.com/the-health-service-ombudsman
Parliamentary and Health Service Ombudsman
http://www.ombudsman.org.uk/healthchp
http://youtu.be/ELHPDF7YvoA
| Drug reps |
|---|