41
- entsurgery.net
- ent kent.com
- umm.edu ENT
- ENT Referals Pulse Learning Module Nov 2011
- See Hear Rural Health West au
ENT examination routines
- hacking-medschool/ent-exam
- meded.ucsd.edu Head and Neck Exam
- youtu.be/RbYt7CssiRg
- youtu.be/AYaGMf5Edm8
- youtu.be/R7hd3u29DsI
ENT diagnostic sets
- Macroview Otoscope
- Digital Macroview Otoscope
- Dino lite Digital Video Otoscope
- ENT diagnostic sets @ Amazon
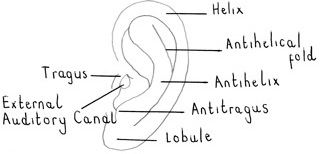
Ear anatomy and physiology
Ear drum anatomy
doctorsgates.blogspot.com anatomy of the ear drum
Ear examination and otoscopy
Tympanic membrane appearances
A Mini-Atlas of Ear-drum Pathology NCBI
Tuning fork tests
Rinnes test – hold vibrating tuning fork on mastoid until it is no longer heared. Then move it to EAM where it will be heared again ie AC is better than BC (normal or sensineural deafness). If BC is better than AC then a conduction defect (wax, otosclerosis) may be present.
Webers test – place vibrating tuning fork in middle of forehead. It should be heared equally in both ears. In conduction deafness it will be heared better in the affected ear. In sensineural deafness it will not be heared in the affected ear.
| Rinnes and Weber tuning fork tests | ||
|---|---|---|
| Result | Rinne | Weber loudest in |
| Normal Hearing | +ve | Both Ears |
| Left Conductive Loss | -ve | Left Ear |
| Left Parial sensineural loss | +ve | Right Ear |
| Left Complete sensineural loss | -ve | Right Ear |
Congenital ear problems and deafness
ASHA congenital hearing disorders
National Childrens Deaf Assosciation org.uk
Hearing Loss
Audiograms
- youtu.be/A8pPuhRKmIA
- youtu.be/ie1SdWdWErg
- youtu.be/9u9Ja4wyUaU
- Wisconsin Online Audiograms
- Audiogram raising deaf kids.org
Age related deafness presbyacusis
Age-related hearing loss Medlineplus
Sudden sensineural hearing loss
ENT care wordpress.com Management of sudden sensorineural hearing loss
Sudden deafness should be treated as an emergency.
History: how long, URTI, trauma, previous ear problems
Examination: ear, nose, PNS, throat
Investigations
FBC U+E’s TFT syphillis serology ESRANCAECG Audiometry AC + BC
If cause can be identified the treatment is specific to the cause.
Management of idiopathic sudden SNHL is controversial but includes prednisolone 60mg/daily 2w Famcyclovir 500mg tds p.o. 1 week Diuretics and low salt diet +/- Carbogen
Hearing aids
- youtu.be/CqO5C__vK7s
- Hearing aids mayo clinic.com
- youtu.be/UZ5Lqa436eU
- umm.edu Bone Anchored Hearing Aids
How to speak to a deaf person
- Communicating with Deaf patients Medscape
- Communicating With Hearing-Impaired Patients WJM/PubMed
- PUK Dealing with Hearing Impaired Patients
Dizziness (ENT)
- youtu.be/MSwQPw35MUQ
- Dizzyness NHS Choices
- Dizziness and balance problems A guide for patients and carers Brain and Spine Foundation
- Dizzyness PUK
- Dizziness Vertigo Imbalance Medscape
Acute viral labrynthitis
Acute viral labrynthitis aka Vestibulitis Vestibular Neuronitis
Symptoms include severe vertigo, nausea and vomiting, but no tinnitus or hearing loss.
Tinnitus
Meniere’s disease
- youtu.be/TFksAtUpTfg
- youtu.be/b91ughElY
- youtu.be/a0JiByEcwt8
- menieres disease Clinical Knowlege Summaries
- Menieres.org.uk
- Meniere’s disease ent uk.org
Dix Hallpike testing
- Brandt BPPV demonstration tchain.com
- Benign Positional Vertigo in Emergency Medicine Medscape
- youtu.be/mmBB2bu1gEQ
- youtu.be/IHfU2cA7eRo
- youtu.be/59EIKztATiw
- youtu.be/Rpwf2mI3SU
Epley’s manoevre
canalith repositioning procedure
Epleys manoeuvre entcare.co.uk
Dix Hallpike = testing
Epleys = treatment
Acoustic neuroma
Unilateral (or unequal) sensineural hearing loss with vertigo then dizzyness and unsteadyness
BPPV
Benign paroxysmal positional vertigo
- Vertigo BMJ 2009
- DTB 2009;47:62-66
- Vertigo diagnosis and management in primary care bjmp.org
- Vertigo PUK
Ear pain earache
- Otitis Externa
- Furuncle/Boil External Ear
- Shingles (Ramsay Hunt)
- Otitis Media
- Labyrinthitis
- Ruptured Tympanic Membrane
- Foreign Body
Ear trauma
Perichondral Haematoma Boxers Ear
Blunt trauma causes bleeding between auricular cartilage and the perichondrium.
Untreated will lead to cauliflower ear deformity from proliferative fibrosis.
Aspirate under LA consider instillation of 0.5ml Depo-medrone, pack firmly and closely with cotton wool/soft foam under turban dressing and refer next ENT clinic.
Rx fluclox 500ng qds to prevent perichondritis.
Large bleeds or those involving cartlidge itself refer ENT/Plastics directly.
FB ear
Most commonly occurs in children under the age of 5 years. Beads, small stones, beans, corn, and dry cereal are also common. Insects may also fly into the ear causing distress and anxiety. Suctioning, irrigation, or use of special tools can be used to remove foreign objects. A few drops of olive will kill live insects.
Any irrigants should be warmed to 37 degrees Celsius before installation to prevent dizziness, nausea, and vomiting.
FB may cause pain deafness and discharge if left
Remove under direct vision if possible. May need GA especially children.
Use loop, blunt hook, skill experience. Suction +/microscope will help.
If in doubt about chances to remove slickly then offer ENT first chance to remove.
Insect
Drown with warm olive oil or liquid paraffin before removing with forceps or syringe.
Chondrodermatitis nodularis helicis
Wax and srynging
Ear syringing is a procedure commonly used to remove impacted wax (and occasionally FBs) from the external auditory canal.
Its use has declined recently due to the high incidence of litigation for perforation and other injuries, and patients are encouraged to try using olive oil or other cerumen solvents prior to and as an alternative to srynging.
Where possible removal of wax with an ear probe under direct vision /magnification by a trained practitioner is preferred.
Red Flags
Known h/o Perforated tympanic membrane, or
Prior middle ear surgery; tympanostomy tubes or grommets
Acutely Vertigo, nausea or vomiting
Otitis externa
Inflammation of the external ear canal and auricle.
Can be caused by swimming in contaminated water (swimmers ear – more common in summer), exposure to chemical irritants, cleaning/poking the ear canal with a foreign object, regular use of ear devices, and a perforated tympanic membrane.
Resistant otitis externa may be due to a fungal infection or organisms such as psuedomonas. Take swabs.
Symptoms include pain, swelling, redness, and purulent drainage of the auricle and ear canal.
Chewing or movement of the tragus or pinna usually increases pain.
Usually resolves in 7 days but can reoccur become chronic in some.
Bacterial or fungal infection.
May follow exposure to water (swimmers ear).
Pain (especially on pressing tragus) desquamation of skin and a thin scanty discharge that may become purulent.
Chronic OE can lead to narrowing and stenosis of the canal.
Management
Aural toilet using cotton wick to gently remove debris.
Give antibiotic/steroid drops or spray.
Refer ENT follow up as appropriate
Treatment of otitis externa
Betnesol® drops (betamethasone 0.1%)
Dose: Ear, apply 2-3 drops every 2-3 hours, reduce frequency when relief obtained.
Gentisone-HC® drops (gentamicin 0.3%/hydrocortisone 1%)
Dose: Apply 2-4 drops into the ear 3 to 4 times daily and at night.
Locorten-Vioform® drops (flumetasone pivalate 0.02%/clioquinol 1%)
Dose: Apply 2-3 drops into the ear twice daily.
These preparations should be used for no longer than 7 days to prevent fungal overgrowth. Preparations containing aminoglycosides or polymyxin should not be used if the eardrum is perforated.
Antifungal preparations
Clotrimazole solution 1%
Dose: Apply 2-3 drops daily continuing for at least 14 days after disappearance of infection
Malignant otitis externa
Furuncle external ear
Very painful boil or pimple in outer part of external auditory canal.
Pain worse on moving examining the ear.
Hearing not usually affected.
Management
Insert wick soaked in 10% ichthammol in glycerine to encourage discharge of pus.
Rx flucloxaciilin 500mg qds and strong analgesic.
Check urine for glucose.
Swimmers osteoma
Ear discharge
Aural polyp
Perforated ear drum
Causes
Bacterial infection
Trauma – skull fracture, foreign body insertion, instrumentation/srynging
Barotrauma – explosions, direct blows, or deep sea diving
Most ruptured TM’s occur in children with chronic ear infections.
Symptoms include pain, bloody or purulent discharge, hearing loss, vertigo, and fever.
Patients may be pain free if the membrane has already ruptured.
The TM will appear slit-shaped or irregular.
Tympanosclerosis
Otosclerosis
Acute otitis media (ENT)
- youtube.com/watch?v=T8g62Fygepg
- youtube.com/watch?v=1kmsPEd2Efk
- youtube.com/watch?v=1kmsPEd2Efk
- youtube.com/watch?v=3EhLwCpnuGM
- Acute Otitis media in Children SIGN 66 2003
- Acute Otitis Media Guidelines,Paediatrics 2010
Acute otitis media JAMA 2010;304:2161–9
Infection of the middle ear occurring most often in children between 6 months and 3 years of age.
Usually preceded by a viral upper respiratory infection.
Symptoms include rapid onset of pain, headache, tinnitus, hearing loss, and nausea or vomiting.
Pediatric patients may present with irritability, crying, rubbing or pulling the ears, restless sleep, and lethargy.
Visualization of the tympanic membrane usually reveals a dull light later becoming red and bulging.
Uncommon but serious complications include ruptured tympanic membrane, meningitis, acute mastoiditis, intracranial or neck abscess, facial nerve damage, or permanent hearing damage. Chronic or persistent OM may require myringotomy tube placement in pediatric patients.
Many infections are viral.
Illness will resolve within 4 days in 80% of cases with no antibiotics. Ensure adequate analgesia available.
Antibiotics will not reduce pain in the first 24 hours, subsequent attacks or deafness though will reduce duration particularly in young children
Children with otorrhoea, or <2 years with bilateral acute otitis media, may have greater benefit from antibiotics but delayed prescribing may still be considered.
Organism S.pneumoniae. H.influenzae. M.catarrhalis
1st line Amoxicillin 40mg/kg/day, five days treatment. Clarithromycin in penicillin allergic individuals.
2nd line Co-amoxiclav or azithromycin (if penicillin allergic) for 5 days..
Xylitol for preventing acute otitis media Cochrane Nov 2011
Otitis media NNT
Glue ear
CSOM / otitis media with effusion / glue ear
- Glue ear hearing central.com
- NICE CG60 Surgical management of OME Feb 2008
- QRG
- http://www.youtube.com/watch?v=ML7ttN-55TY
- http://youtu.be/gYrEh025hqU
Tympanograms
Grommets and T-tubes
- ENT.uk
- Grommets @ BUPA
- http://youtu.be/KFkV5qVYs3Y
- http://youtu.be/T0HY4fgejCQ
- http://youtu.be/F_KJUzmqj_A
Cholesteatoma
- http://www.youtube.com/watch?v=acqxAkF5l4c
- http://www.youtube.com/watch?v=WYvvXhrOVRw
- http://www.youtube.com/watch?v=EKuPJ4HNPIw
- Cholesteatoma earsurgery.org
- Cholesteatoma BMJ 2011
- Cholesteatoma medscape
Cholesteatoma = a ball of skin trapped in the middle ear
Grows as result of chronic inflammatory process and destroys structures (ossicles, inner ear, balance organ, facial nerve, brain)
Can lead to intracranial complications
Treatment = Mastoidectomy
Mastoid Cavity
Mastoid Cavity ENT Houston
http://youtu.be/_jFJz46y3Wc
Mack’s Ear dryer
Mastoiditis
- http://www.youtube.com/watch?v=hN-MJp9E1TM
- Mastoiditis medscape
- Mastoiditis PUK
- Acute Mastoiditis Biomed Central
Nose anatomy
Nose examination
Nasendoscopy
FB nose
FBs may be difficult to remove particularly if the patient is unable to co-operate.
Beads can sometimes be pushed further in by the wrong technique or instrument.
Broken nose
Nasal deformity is the important sign and radiology is early indicated.
ENT review for nasal deformity assessment should be when ST swelling is reducing at approx. day 4.
Septal haematoma requires evacuation ASAP.
Nose bleeds epistaxis
Local causes
Trauma, infection, foreign bodies, surgery, chemical irritants,
Benign neoplasms: juvenile NP angiofibroma
Malignant neoplasms
Systemic causes
Haematologic disorders:NSAID, Haemophilias, Leukaemias
Osler-Weber-Rendu disease
Management
Digital pressure on soft part of nose
Barrier creams/Naseptin
Cautery under L.A.
Packing
Bipolar diathermy under G.A.
Epistaxis first aid
- http://www.youtube.com/watch?v=_KezSoQHDcM
- http://www.youtube.com/watch?v=Mwf9JYYN2fk
- http://www.youtube.com/watch?v=6sJ_p5zNl3M
- http://www.youtube.com/watch?v=Dp_i-GJA7UI
Blocked nose
http://www.youtube.com/watch?v=pPPCqnCCxyQ
Adenoidal hypertrophy (children, teenagers)
Nasal polyps
Septal deformity
Choanal atresia
Deviated nasal septum
Nasal polyps
BSACI guidelines for the management of rhinosinusitis and nasal polyposis
Management
Nasal steroid sprays/drops
Systemic steroids
Surgery
Rare in children – Usually associated with cystic fibrosis
Bilateral
•Respiratory distress at birth
•Requires neonatal ventilation
•Opening of atresia at day 5-7
•Stenting for 3 months minimum
Unilateral
•May be undetected for years
•Unilateral nasal discharge ? FB
•Surgery age 3-5
Rhinitis
BSACI guidelines for the management of allergic and non-allergic rhinitis
Infective
Allergic
Vasomotor
Enlarged inferior and middle turbinates
Management
Identify cause and treat
Nasal steroid sprays
Saline nasal douches
Antibiotics if infective
Allergic rhinitis
- Rhinitis management guidelines British Society for Allergy and Clinical Immunology
- Allergic Rhinitis Lancet 22 Jul 2011
- http://www.youtube.com/watch?v=wQbyC5cpEQI
Asthma and rhinitis
Asthma and rhinitis usually co-exist, with symptoms of rhinitis found in 75–80% of patients with asthma
Rhinitis is a risk factor for the development of asthma
Treatment of rhinitis is associated with benefits for asthma
Rhinitis in pregnancy
Self-limiting condition affecting at least 20% of pregnancies. Can start at any time.
Regular nasal douching may be helpful
Most medications cross the placenta, and should only be prescribed when the apparent benefit is greater than the risk to the foetus
beclomethasone, fluticasone and budesonide appear to have good safety records as they are widely used in pregnant asthmatic women
cromoglicate may be helpful
chlorphenamine, loratidine and cetirizine may be added cautiously if additional treatment is needed but decongestants should be avoided
Some antihistamines may increase the risk of spontaneous abortion or congenital malformation
Topical corticosteroids have shown no evidence of harmful effects
BSACI guidelines for the management of allergic and non-allergic rhinitis. Clinical and Experimental Allergy 2008; 38:19–42
http://www.bsaci.org/index.php?option=com_content&task=view&id=117&Itemid=139
Acute sinusitis
Acute sinusitis DTB 2009;47:26–30
Organism S.pneumoniae
1st line Penicillin V 1g twice daily or 500mg four times daily for seven days.
2nd line Doxycycline 200mg stat and then 100mg daily for a total of seven days.
Inflammatory process involving lining of paranasal sinuses
Initially viral rhinosinusitis then Secondary bacterial infection -Streptococci, Staphylococci H.Influenza
Other causes: Dental infections, facial trauma, immotile cilia syndrome, neoplasia
Treatment
-Broad spectrum antibiotic (Amoxycillin+/-Clavulanic Ac.) for 2/52
-Analgesia
-Topical/systemic decongestants
-Decongestant pack in MM/sinus puncture
Complications of acute sinusitis
•Cranial (osteomyelitis)
•Orbital (cellulitis, abscess, endophthalmitis)
•Intracranial (cavernous sinus thrombosis, brain abscess)
Diagnosing sinus tenderness (Murtagh)
http://youtu.be/8Lo3bENDqzs
Eliciting sinus tenderness is important in the diagnosis and follow-up of sinusitis.
Firm pressure over any facial bone, particularly in the patient with an upper respiratory infection, may cause pain. It is important to differentiate sinus tenderness from non-sinus bone tenderness
Method
1. This is best done by palpating a non-sinus area first and last, systematically exerting pressure over the temporal bones (T), then
the frontal (F), ethmoid (E) and maxillary (M) sinuses, and finally zygomas (2), or vice versa.
2. Differential tenderness both identifies and localises the main sites of infection.
Diagnosis of unilateral sinusitis
A simple way to assess the presence or absence of fluid in the frontal sinus, and in the maxillary sinus (in particular), is the use of transillumination.
It works best when one symptomatic side can be compared with an asymptomatic side.
It is necessary to have the patient in a darkened room and to use a small, narrow-beam torch.
Frontal sinuses
Shine the torch above the eye in the roof of the orbit and also directly over the frontal sinuses, and compare the illuminations.
Maxillary sinuses
Remove dentures (if any). Shine the light inside the mouth, on either side of the hard palate, pointed at the base of the orbit. A dull glow seen
below the orbit indicates that the antrum is airfilled.
Diminished illumination on the symptomatic side indicates sinusitis.
Snoring
Obstructive sleep apnoea
Obstructive sleep apnoea in adults BMJ 2009;338:b1165
Throat anatomy
Throat anatomy
Throat examination
Throat examination
Cervical lymphadenopathy
Swollen glands / enlarged cervical lymph nodes / Cervical Lymphadenopathy
http://hacking-medschool.com/lymphadenopathy-lymph-node-examination
http://www.youtube.com/watch?v=aAdB0A42qas
Causes of generalized lymphadenopathy
ALL AML
Lymphoma
Infections – glandular fever, secondary syphilis, miliary TB.
CTD – SLE, Still’s, rheumatoid Arthritis
Sarcoid
Sore throat
http://hacking-medschool.com/sore-throat-kids
http://www.cks.nhs.uk/sore_throat_acute/evidence/references
Sore throats MeReC 2006;17(3)
History
duration
fever/malaise
recurrent problems
immunocompromised
on medication which may cause agranulocytosis, e.g. carbimazole, mirtazapine
Examination
examine throat asking the patient to yawn or pant may improve the view.
Consider using a tongue depressor if the back of throat is not visible (but beware of epiglottitis)
assess inflammation of pharynx
look for exudates on tonsils
check neck for lymphadenopathy
look for a macular rash (small red flat patches)
Tests
FBC and Paul Bunnell for glandular fever, if symptoms persist for longer than a week
Urgent FBC should be requested if patient on drugs causing agranulocytosis
Action
antibiotics are of marginal benefit in most cases, and at best will only shorten the illness by 24 h.
Give antibiotics if immunocompromised, or if severe malaise or macular rash (scarlatina) present
Avoid amoxicillin if glandular fever a possiblity
Prescription
symptomatic treatment for most patients – ibuprofen or paracetamol, benzydamine spray
if an antibiotic is indicated in adults and children aged 10 years and over, give penicillin V for 10 days
if an antibiotic is indicated in children under 10 years, Rx amoxicillin suspension for 7 days. Although it is more likely to cause side-effects than penicillin V, in our experience young children find the taste of penicillin V suspension unpleasant and often refuse to take it
if allergic to penicillin, use erythromycin /clarithromycin
Refer immediately if:
child very sick, drooling, cannot swallow (possible epiglottitis, do not examine throat)
large swelling around one tonsil (possible quinsy, may need surgery)
on drugs that can cause agranulocytosis
Tonsillitis
SIGN 117 QRG Sore Throat/Tonsillectomy Jun 10
Penicillin is recommended by the American Academy of Paediatrics and American Heart Association as first-line therapy for GABHS infections;
erythromycin is recommended for those allergic to penicillin.
Treatment duration with penicillin should be 10 days to optimize cure in GABHS infections.
A five day regimen is advised for azithromycin (a macrolide).
Prevention of rheumatic fever is the primary objective for antibiotic therapy of GABHS infections
Tonsillitis/Pharyngitis/Acute Sore Throat
Average length of illness 1 week. Consider delayed antibiotic strategy.
75% of infections are viral not bacterial, both may have exudate.
If 3 or 4 centor criteria (fever, purulent tonsils, cervical lymphademopathy, no cough) or history of otitis media then antibiotics may be of more benefit.
Organism S.pyogenes, beta-haemolytic Strep
Samples Clinically suspicious of glandular fever, consider laboratory investigation.
1st line Penicillin V 1g twice daily or 500mg four times daily ten days
Clarithromycin 500mg twice daily for 10 days in penicillin allergic patients.
Quinsy – peritonsillar abcess
Unilateral Tonsillar Swelling
Recurrent acute infection
Peritonsillar abscess
Neoplasia
–Lymphoma (children)
–Salivary gland tumours
–SCC (adults)
Parapharyngeal space mass
Tonsillar Cancer
Glandular fever
http://hacking-medschool.com/glandular-fever-ebv-monospot
Glandular Fever (Epstein –Barr virus tonsillitis)
Transmission through infected saliva
Oral secretions transmit for up to 6 months
Petechiae at junction of soft–hard palate
FBC: monocytosis with 10% atypical monocytes
Serologic studies may be negative for 2 weeks
Management
Cephalosporins to avoid bacterial infection
Steroids
Avoid ampicillin
Avoid contact sports for 2 months – hepatosplenomegaly
Look for thrombocytopenia
Complications
Meningoencephalitis
Guillain-Barre Syndrome
Bell’s Palsy
Pneumonitis
Pericarditis, Myocarditis
Syndrome of inappropriate Antidiuretic Hormone (SIADH)
Splenic rupture (days 4-21): 0.1-0.2%
Airway Obstruction
Strep Pharyngitis
Tonsillectomy
- youtube.com/watch?v=LP7Os8m0Nc4
- youtube.com/watch?v=RTFUpoqhbHo
- youtube.com/watch?v=X9MKgoTwTIo
- youtube.com/watch?v=4WN0aTfXMs4
•Recurrent acute tonsillitis
•Peritonsillar abscess
•Suspected malignancy
•OSA
Adenoidectomy
Obstruction:
•Chronic nasal obstruction or obligate mouth breathing
•OSA
•Dysphagia
•Speech problems
Infection:
•Recurrent/chronic adenoiditis (3 or more episodes/year)
•Recurrent/chronic OME
FB Throat
Foreign Bodies in the Ear, Nose, and Throat AAFP 2007
Neck lumps
http://hacking-medschool.com/thyroid-exam
Midline
Thyroglossal cyst
Midline dermoid
Anterior triangle (anterior to sternomastoid)
Thyroid
Branchial cysts
Pharyngeal pouch
Salivary gland swellings
Lymph nodes
Carotid body tumour
Cervical rib
Posterior (posterior to sternomastoid)
lymphadenopathy
Goitre
Any swelling of thyroid gland
Croup epiglottitis stridor
- hacking-medschool/viral-croup
- hacking-medschool/croup-score
- hacking-medschool/stridor
- hacking-medschool/stridor-1
Hoarseness
Dysphagia (ENT)
- http://hacking-medschool.com/dysphagia-general-surgery
- SALT assessment Nursing Times
- youtu.be/1YfO11Pry6Y
Parotid and salivary gland disorders (ENT)
- http://hacking-medschool.com/salivary-gland-disease
- medlineplus salivary gland disorders
- ent associates.com salivary glands
- Salivary gland tumours medscape
Warthins
Warthins
Pleomorphic adenoma
Pleomorphic Adenoma
Head and neck cancer
Thyroid Cancer
- Papillary
- Follicular
- Anaplastic
- Medullary
- Lymphoma
ENT Prescribing
Otitis externa
Betnesol® drops (betamethasone 0.1%)
Dose: Ear, apply 2-3 drops every 2-3 hours, reduce frequency when relief obtained.
Gentisone-HC® drops (gentamicin 0.3%/hydrocortisone 1%)
Dose: Apply 2-4 drops into the ear 3 to 4 times daily and at night.
Locorten-Vioform® drops (flumetasone pivalate 0.02%/clioquinol 1%)
Dose: Apply 2-3 drops into the ear twice daily.
These preparations should be used for no longer than 7 days to prevent fungal overgrowth. Preparations containing aminoglycosides or polymyxin should not be used if the eardrum is perforated.
Removal of ear wax
Almond or Olive Oil
Dose: This patient should lie with the affected ear uppermost for 5 to 10 minutes after a generous amount of oil has been introduced into the ear. Oils should be warned (e.g. by pouring onto a warmed teaspoon) before administration.
Sodium Bicarbonate drops 5%
If the wax is hard and impacted drops may be used twice daily for several days before syringing (up to 10 days may be required); otherwise the wax may be softened on the day of syringing. Cerumol drops have not been included due to the relatively frequent occurrence of allergic reactions.
Antifungal preparations
Clotrimazole solution 1%
Dose: Apply 2-3 drops daily continuing for at least 14 days after disappearance of infection.
Nasal Allergy
Beclometasone aqueous nasal spray 50micrograms/metered spray
Dose: 100micrograms (2 sprays) into each nostril twice daily; max. total 400micrograms (8 sprays) daily; when symptoms controlled, dose reduced to 50micrograms (1 spray) into each nostril twice daily.
Fluticasone furoate nasal spray ?27.5micrograms/metered spray
Dose: 55micrograms (2 sprays) into each nostril once daily; when control achieved reduce to 27.5micrograms (1 spray) into each nostril once daily.
In seasonal allergic rhinitis (eg hay fever), treatment should begin 2 to 3 weeks before the season commences and may have to be continued for several months.
Corticosteroid nasal preparations should be avoided in the presence of untreated nasal infections, and also after nasal surgery (until healing has occurred); they should also be avoided in pulmonary tuberculosis. Systemic side effects of nasally administered corticosteroids are rare and there are no advantages in using the significantly more expensive fluticasone nasal spray. Many patients using beclometasone can be controlled on once daily dosing.
Topical nasal decongestants
Xylometazoline nasal drops 0.1%
Dose: Instil 2-3 drops into each nostril, 2 to 3 times daily when required; max. duration 7 days; not recommended for children under 12 years.
Topical nasal decongestants often cause rebound congestion and should be used for no longer than 7 days. Sympathomimetics, such as xylometazoline, should be avoided in patients taking monoamine oxidase inhibitors (MAOIs).
Sodium Chloride 0.9% given as nasal drops may relieve nasal congestion by helping to liquefy mucous secretions and may be useful for infants under 3 months.
Anti-infective nasal preparations
Naseptin® (chlorhexidine 0.1%/neomycin) cream
Dose: For eradication of nasal carriage of staphylococci,apply to nostrils 4 times daily for 10 days; for preventing nasal carriage of staphylococci, apply to nostril twice daily.
Mupirocin nasal ointment is reserved for resistant cases. In hospitals, mupirocin nasal ointment should be reserved for the eradication of nasal carriage of MRSA
Oral ulceration and inflammation
Benzydamine oral rinse 0.15%, spray 0.15%
Dose: Oral rinse, rinse or gargle, using 15ml (diluted with water if stinging occurs), every 1½ to 3 hours as required, usually for not more than 7 days; not suitable for children aged 12 years or under. Spray, adult, 4-8 sprays onto affected area every 1½-3 hours.
Triamcinolone acetonide oral paste 0.1%
Dose: Apply a thin layer 2-4 times daily; do not rub in; use limited to 5 days for children and short-term use also advised for elderly.
Benzydamine is effective at relieving oral discomfort and for irradiation mucositis. If the full strength mouthwash causes some stinging, it may be diluted with an equal volume of water. See also PRODIGY Guidance – Sore throat – acute
Oropharyngeal fungal infections
Nystatin suspension 100,000units/ml
Dose: 100,000 units 4 times daily after food usually for 7 days (continued for 48 hours after lesions have resolved). Higher doses may be needed for immunosuppressed patients (eg 500,000 units 4 times daily).
Miconazole oral gel 24mg/ml
Dose: Place 5-10ml in the mouth after food and retain near lesions, 4 times daily. Treatment continued for 48 hours after lesions have resolved. Localised lesions, smear small amount on affected area with clean finger 4 times daily (dental prostheses should be removed at night and brushed with gel).
If candidal infections fail to respond to 1 to 2 weeks of treatment with anticandidal drugs the patient should be sent for investigation to eliminate the possibility of underlying disease.
Mouthwashes
Chlorhexidine mouthwash 0.2%
Dose: Oral hygiene and plaque inhibition, rinse the mouth with 10ml for about 1 minute twice daily. Denture stomatitis, cleanse and soak dentures in mouthwash solution for 15 minutes twice daily.
Chlorhexidine mouthwash causes a reversible brown staining of the teeth. Chlorhexidine gluconate may be incompatible with some ingredients in toothpaste; leave an interval of at least 30 minutes between using mouthwash and toothpaste.
Grazax for hay fever DTB 2010;48:54

