56
- Wheeless’ Textbook of Orthopaedics online
- American academy of orthopaedic surgeons aaos.org
- Orthopaedics Tulane University
- Shoulderdoc.co.uk
- world ortho.com
- orthopaedic weblinks.com
- Orthopaedics medmatrix.org
- Orthogate.org
- Orthopaedics Rural Health West au
- Sports Injuries Rural Health West au
MSK regional conditions
http://130.60.57.53/anatomy/Anatomy.html
Spinal anatomy
Cervical spine examination
- Cervical spine examination Rehabmanual.com
- Cervical spine examination Orthofracs.com
- youtu.be/vHQHrjMlOEU
- youtu.be/e3QXEjnxgyw
- youtu.be/YwR9EcKN_Jc
Thoracic spine examination
Lumbar spine examination
- Anatomy and Examination – UCSD
- Back Exam Patient UK
- youtu.be/jJIJ2sHVOoM
- youtu.be/bfrgN64ojRY
- youtu.be/ljzzYPeXOFk
- youtu.be/O49dwZ2CW5A
- youtu.be/a_ptmvfOe9c
Neck pain
Neck pain and sprains are common. Presentations include acute torticollis whiplash esp RTA, and degenerative disease in the middle aged and elderly. Whiplash can take up to 18m to settle but a positive approach from outset with rehabilitation advice can help reduce this.
Key Points
Accurate mechanism of injury
Follow Ottowa rules for management including Xray in acute Cspine injury. Refer immediately for neurological signs.
Beware central cord syndrome in elderly patient recieving blow to face
Examination
Undress patient to underwear to fully expose back
Inspect
symmetry swelling bruising muscle spasm asymmetry of posture
Feel/palpate
spinal processes for warmth & tenderness
percuss spinal processess with heel of hand
Test the following movements:
• Flexion (looking down at toes)
• Extension (looking up at ceiling)
• Lateral flexion (putting each ear onto the shoulder in tum)
• Lateral rotation (looking over each shoulder in tum).
Fix the shoulders when assessing flexion, to ensure that movement is occurring at the cervical spine rather than the shoulders.
Normal findings/ROM
(included to give an idea only while its difficult to be precise it is useful and more satisfying to be able to document findings objectively)
Flexion 50 degrees
Extension 75 degrees
Lateral Flexion 45 degrees
Rotation 70 degrees
Common conditions
Whiplash
Acute Torticollis ( young adults children, ?due to minor disc protusion – lasts few days (5-10)
OA
Investigations
C spine XRay for traumatic injuries (and immobilisation if) High velocity, age >65, paraesthesia in extremeties, immediate onset of pain, not moved since injury (not likely in WIC) midline Cspinne tendernes, inability to rotate neck to 45 degrees L+R, associated head injury
Acute neck sprain
Whiplash injury
Cervical spondylosis
- Cervical Spondylitis PUK
- Cervical radiculopathy BMJ 2009
- Cervical Sponylosis Medscape
- youtu.be/-9s28eQJcUE
- youtu.be/zUm6k1LJdk0
Cervical Disc
Cervical spine xrays
Thoracic spine pain
- Thoracic spine pain MD Gudelines
- Thoracic pain Richard Walker Pain Clinic
- Thoracic discogenic pain syndrome Medscape
- Thoracic disc injuries Medscape
- youtu.be/jxOUWyItTzw
- youtu.be/0OPL87ih7B4
- youtu.be/Tk8L2aF2cn4
Low back pain
Diagnosis
1. Is it mechanical backache or is there some underlying pathology?
(i) The older patient with possibilities of osteoarthrosis, osteoporosis, Paget’s disease and malignant deposits in the spine. In the elderly an Xray may be worthwhile
(ii) The young patient with low back pain and morning stiffness who may have ankylosing spondylitis
(iii) Referred pain – renal or gynaecological
(iv) Infection
(v) Depression can present as backache
Mechanical backache is likely to be episodic, related to posture, worse on movement and relieved by rest.
Back pain without these features, in the young « 20 years), in the elderly, that is progressive or continuous, or associated with systemic symptoms demands fuller investigation
2. If the pain is mechanical is it due to a prolapsed intervertebral disc? Practically this means, are there symptoms of nerve root compression?
Examination
Observe the curvature, feel where the tenderness is and test movement
Important part is the testing of straight leg raising (SLR) and the femoral stretch test (knee flexion when prone), the latter to detect higher (L 3/4) root pressure
A motor and sensory examination together with testing the reflexes is not likely to be a feature of the examination unless a disc prolapse is suspected
Much can be learnt from patient’s demeanour and posture and by simple enquiry (? sciatica, ? recent injury, ? occupation, etc.)
The rare central disc prolapse presents with urinary symptoms and severe weakness of the legs peripherally and requires an immediate referral for emergency surgery Red Flags in Low Back Pain Red flags such as bilateral or alternating leg symptoms, neurological disturbance, sphincter disturbance and history of malignancy help to identify those who need investigation.
Acute back pain is an exceedingly common complaint that affects up to 75% of all adults during their lifetime. Most causes are benign and recover within 2-3 weeks but serious etiologies must be considered. Patients with back pain typically experience difficulties with work and performing activities of daily living.
Red Flags
- Signs or symptoms of Cauda equine syndrome – Saddle anaesthesia, faecal incontinence poor anal tone pn PR – needs immediate referral to prevent permanaent disability
- Unexplained weight loss
- Unexplained fever
- Guarded movement
- Inability to bear weight or walk
- Night time pain or pain worse when recumbent
- Significant trauma
- Persistance
- Middle age and older
- AAA
Bowel or Bladder problems, bilateral lower limb paraesthesia or weakness, saddle anaesthesia in cauda equina syndrome
Age <20 >55
Thoracic Pain
Steroids
Weight Loss
H/O Cancer
AAA in elderly
Consider Vertebral Crush Fracture in osteoporotic elderly.
Physical exam for focal neurologic deficits
Analgesics
Rest until cause determined and pain controlled
Emergency transfer to facility with MRI and neurosurgical capabilities
Most causes of acute back pain are benign musculoskeletal or mechanical disorders but the clinician should be aware of more serious neurological, vascular and visceral causes.
Mechanical Back Pain
Acute strain or sprain of the back is often diagnosed by history alone. There is typically a preceding injury involving the lifting or moving of heavy objects. There may be no specific findings on physical exam, other than mild soft tissue tenderness.
Age related changes to the bony structure of the spine and discs lead to localized pain – especially common in the lumbar spine.
Compression fractures are often traumatic in nature and can be elicited on exam by midline tenderness. Atraumatic fractures may occur in the elderly.
Radiation of pain to the lateral or posterior leg is consistent with disc herniation and sciatica. Bilateral lower extremity pain is more likely the result of overall narrowing of the spinal canal known as spinal stenosis.
Muscle spasm of either upper or lower back musculature can readily be palpated during physical exam.
Non-mechanical Spinal Pain
Much less common causes of spinal pain include bony tumors, often from metastatic disease. These lesions typically cause unremitting, focal pain in the midline. Infections including spinal epidural abscess may cause more generalized pain and constitutional symptoms such as fever.
Intra-abdominal/Intra-thoracic Related Back Pain
A thorough exam of the heart, lungs, abdomen and bilateral pulses accompanied by a complete history is necessary if these diagnoses are a consideration.
Upper back pain may be attributed to radiation of pain from the thorax including thoracic aortic aneurysm, pulmonary embolus and pneumonia.
Lower back pain can be caused by abdominal aortic aneurysm, pelvic organ diseases, urinary tract infections, kidney stones and ectopic pregnancy.
Uncommonly, shingles may cause pain in a dermatomal region of the back prior to the appearance of the classic vesicular rash.
Treatments
NSAID’s or Paracetamol
Benzodiazepines or muscle relaxants
Opioid/analgesic combination – not shown to be more effective than NSAID’s but may provide short term relief.
Localized heat
Activity restriction
Patient education is important: recurrence of back pain is common. Demonstrate proper bending and lifting techniques.
Physical therapy
Massage; acupuncture; spinal manipulation
Return to work/activity as tolerated. No bed rest recommended.
Neurosurgery referral
Red flags in low back pain
Fracture
Major trauma (motor vehicle accident, fall from height)
Minor trauma or strenuous lifting in an older or osteoporotic patient
Tumor or infection
Age >50 years or <20 years
History of cancer
Constitutional symptoms (fever, chills, unexplained weight loss)
Recent bacterial infection
Intravenous drug use
Immunosuppression (corticosteroid use, transplant recipient, HIV infection)
Pain worse at night or in the supine position
Cauda equina syndrome
Saddle anesthesia
Recent onset of bladder dysfunction
Severe or progressive neurologic deficit in lower extremity
Diagnosis and management
Red Flags are symptoms and conditions that require urgent imaging, blood tests and referral. They include the following.
A past medical history of carcinoma, TB, drug abuse and HIV (cause of immunosuppression and infection).
Previous prescription drug use (e.g. steroids).
Symptoms of night sweats, fever and loss of weight.
A new structural deformity (e.g. kyphosis) suggestive of fracture.
Widespread neurology:
cauda equina symptoms these need immediate referral as there is a risk of permanent damage and incontinence. These symptoms include:
loss of sphincter control
bilateral neurological leg pain
saddle loss of sensation.
Low back pain
Low back pain is common and patients may present with acute or chronic problems.
Most is mechanical back pain following an acute strain or prolonged unaccustomed activity.
It requires reassurance simple analgesia and advice re staying mobile.
Radiation to the buttock or leg is common though true sciatica radiates below the knee.
Even acute disc prolapse usually settles within weeks with conservative treatment.
Examination is directed to confirm clinical impression exclude serious pathology or neurological emergency
Examination
Undress patient to underwear to fully expose back
Inspect
spinal profiles when upright and bending down – note curves and symmetry when upright and bending down (kyphosis lordosis scoliosis)
Feel/palpate
spinal processes for warmth & tenderness
percuss spinal processess with heel of hand
Move (active)
Test the following movements:
• Flexion (touching toes)
• Extension (leaning backwards)
• Lateral flexion (sliding the hand down the side of the right leg and then the left)
• Lateral rotation (twisting at the waist to the left and then the right).
Fix the pelvis when assessing lateral rotation. Do this by stabilising the pelvis with your hands, or performing the examination with the patient sat on the edge of the couch.
Special tests
Straight-leg raising
(for nerve root irritation)
Active and Passive
With the patient supine, use your arm to fix the patient’s pelvis at the anterior superior iliac spines.
The patient then attempts to flex the hip as far as possible with the knee fully extended – raise your straight leg towards the ceiling
Stretch test
(for sciatic nerve root irritation)
With the limit of straight-leg raising reached, allow the leg to lower slightly, then dorsiflex the foot (push the toes towards the head) quickly. If this causes severe pain the test is positive.
Test patella and achilles reflexes for weakness of ankle dorsiflexors and extensor hallucis (L4 L5 prolapse) weakness of the peroneal muscles toe flexors calf and tibialis posterior (L5 S1 prolapse)
Test function
Ask the patient to:
• put on a coat
• take off and put on their shoes.
Examine hip and knee as necessary
Normal findings
ROM Reflexes Myotomes Dermatomes MRC scale
Flexion 60 degrees
Extension 25 degrees
Lateral flexion 25 degrees
Rotation 30 degrees
Investigations
Consider ESR/PSA in elderley
Plain Xray unhelpful except to diagnose AS in young or vertebral collapse or malignancy in the elderly
MRI if nerve root symptoms persist >4 weeks.
Mechanical Back Pain
Mechanical Back Pain
Lumbar disc prolapse
Sciatica
Piriformis syndrome
Spondylosis OA spine
- Lumbar spondylosis Medscape
- spine health.com spondylosis what it means
- spinal disorders.com lumbar spondylosis
Spinal stenosis
- youtu.be/HpE9HU0i_bE
- youtu.be/YC62lgFb_yA
- Lumbar spinal stenosis JAMA 2010
- NICE IPG 365 2010 Interspinous distraction procedures for lumbar spinal stenosis
Spondylolisthesis
Sacroiliac syndrome and sacroiliitis
- youtu.be/1iwmcCw4bAw
- youtu.be/xxktB0kqIeY
- Sacroiliac Syndrome medscape
- Merck Manual seronegative spondyloarthropathies
- Reiters Medscape
Coccydynia
Lumbar spine manipulations
examples only – not yet organised
Lumbar spine Xrays
Shoulder anatomy
Shoulder conditions
rotator cuff disorder – inc tears, tendonitis and impingement syndromes
glenohumeral disorders – inc frozen shoulder and OA
acromioclavicular joint disorders
referred neck pain
myofascial conditions
Shoulder assessment
Red flags
history of, or suspicion of, cancer
possible unreduced dislocation
trauma plus acute disabling pain plus significant weakness suggesting acute rotator cuff tear
possible neurological lesion
referred pain – cardiac pain, gallbladder diaphragm, neck
Shoulder Exam
1. Introduction
The Shoulder Girdle is a sophisticated and complex unit that allows wide range of movement of the arm and hand free from the body but sacrifices some stability and is prone to acute an chronic injury as a result.
The shoulder joint proper is the glenohumeral joint – there are also acromioclavicular, sternoclavicular scapulothoracic and subacromial joints. When examining the shoulder girdle it is important to isolate the specific joints /movements.
Shoulder pain can be referrered from the neck. Common conditions are adhesive capsulitis (frozen shoulder) rotator cuff pathologies (eg supraspinatus tendinitis)
2. Red flags
Consider referred pain from C-spine or heart or diaphragm/abdomen. (MI, pneumonia, intra-abdominal pathology)
Anterior dislocation of shoulder usually obvious. Beware posterior dislocation in Epileptic fit/ electric shock
Suprsapinatus tear may need operative treatment in active young sportspeople – refer if unable to abduct actively.
3. Systematic Examination
Expose both knees adequately. Clarify main site of pain.
– Look
Observe the patients face and demeanor for signs of pain
Compare both sides front and back.
Observe for swelling redness bruising scars deformity
– Inspect/Look for – deformity of the clavicle or the AC joint, muscle wasting (deltoid, axillary nerve damage) asymmetry or loss of contour at the shoulder – a step in the deltoid contour or a gap below the acomium (subluxation or dislocation)
– Feel for areas of warmth (using back of hand)
swelling, crepitus, bony tenderness,
examine systematically from the
Sternoclavicular joint
along the clavicle
the acromioclavicular joint and
around the borders of the acromium
corocoid process (often tender in normal people)
head of humerus
spine and body of scapula
greater tuberosity of humerus (rotator cuff insertion & biceps tendon insertion)
Move
Active Motion
Abduction/Adduction With the elbow fully extended ask the patient to bring the arm away from the body until the fingertips point to the ceiling (abduction) and then swing the arm across the trunk (adduction)
With the elbow flexed at 90 degrees and tucked into the side ask the patient to turn the forearms outwards away from the body (external rotation) and then inwards towards the trunk (internal rotation)
Full internal rotation is blocked by the patients own torso. It can be assessed by asking the patient to see how far up between the shoulder-blades they can reach with the back of their hand behind the back.
Passive Motion
When testing passive abduction and adduction fix the scapula by grabbing the inferior angle to assess the degree of scapular rotation.
For passive internal rotation continue the movement behind the back of the patient.
Passive
test strength of active motion
abduction/adduction (0-170)
forward flexion (0-160)
backward extension( 0-60)
external rotation (put your hand on the back of your head)
internal rotation (put your hand behind your back to touch your shoulder blade
Note: crepitus on movement , restriction, pain (note painful arc – pain develops betwen 80-120 degrees then subsides)
and and weakness of particular movements test sensation over the deltoid (axillary nerve C5)
Special Tests
– Ask the patient to push against wall with flat of their palms and look for winging of the scapula (long thoracic nerve, serratus anterior)
– ask patient to abduct the shoulder against your hands with the thumbs pointing upwards (painful in supraspinatus tendinitis) (Tin Can Tests)
– ask patient to shrug the shoulder against your hands (spinal accesory nerve CN11)
– Scarf test ask patient to put hand on opposite shoulder then push against elbow (ellicits pain in AC joint pathology)
Tests for impingement
– Neers Impingement Test – fully abducting the straight arm will recreate symptoms
– Hawkings impingement test – hold arm at 90degees abduction and 90 degree elbow flexion rotation of the arm across the body will recreate symptoms
Functional Tests
Ask the patient to:
put their hands behind their head with elbows as far back as possible
scratch the centre of their back as far up as possible
put on a coat
Examine cervical spine as appropriate if shoulder examination does not reveal a cause for symptoms
Normal findings
abduction/adduction (0-170)
forward flexion (0-160)
backward extension( 0-60)
external lateral rotation ( 0-90 degrees)
internal medial rotation (0-70 degrees)
Common abnormalities and their significance
Clinical Pictures in Rotator Cuff Injuries
supraspinatus anterior deltoid abduction (painful arc)
infraspinatus posterior deltoid lateral rotation
subscapularis anterior/deltoid medial rotation /adduction
teres minor scapular lateral rotation
Common conditions
Frozen Shoulder
Rotator Cuff tears (often degenerative in middle age cf acute injury)
Impingement Syndrome
Fractured head of humerus in elderley
Shoulder exam
- hacking-medschool/shoulder-exam-2
- ucsd.edu/joints2
- youtu.be/VSrLbzZzJU8
- youtu.be/RsTObF8W9Ds
- youtu.be/WV1DJBpg2tc
- youtu.be/p60X8fADTeg
Shoulder special tests
- uwa.edu/shoulder
- usask.ca fmse
- youtu.be/rAmJccsG4uI
- youtu.be/f4hNiNGdP9A
- youtu.be/tdmRTQidaiI
- youtu.be/W0KnejfMtT0
- youtu.be/xVQy0qPU3Ho
- youtu.be/f9IoPmx-nfs
- youtu.be/Q3gIjMkg91k
- youtu.be/LPbc7HfHlAQ
- youtu.be/_8HB38Bx6WQ
Rotator cuff injury
S supraspinatus
I infraspinatus
T teres minor
S subscapularis
- Rotator Cuff Medscape
- youtu.be/Tg0eDAqaL-g
- youtu.be/i5vXk6u18dc
- youtu.be/e8NbW-dyxTY
- youtu.be/amonHbKwMec
- youtu.be/LmkEFLSpGGY
- youtu.be/xVQy0qPU3Ho
- youtu.be/WOabOI2Z4FA
- youtu.be/ZhN1_ZJyUnk
- youtu.be/uP4NYnycq4
Supraspinatus problems
Infraspinatus problems
- youtu.be/UfBLQqptUcg
- youtu.be/au-Sg0sMarw
- youtu.be/xVQy0qPU3Ho
- youtu.be/EzIZIwgCTQ4
- youtu.be/O6SL4SSBBmQ
Bicipital tendinitis
Subacromial bursitis
Acute subdeltoid bursitis – cyriax
- YT Functional examination shoulder – Cyriax orthopaedic medicine
- YT Cyriax transverse friction massage supraspinatus
- YT Cyriax transverse friction massage infraspinatus
- YT Intra-articular injection in the shoulder joint for arthritis, see www.cyriax.eu
- YT Mill’s manipulation, tennis elbow ; www.cyriax.eu
- YT Injection CTS
- YT Spinal lumbar stretch manipulation, www.cyriax.eu
- YTSpinal lumbar leg over manipulation, www.cyriax.eu
- YT Cyriax orthopaedic medicine thoracic manipulation
- YT Loose body manipulation Knee
Painful arc shoulder
- youtu.be/wU-ppPL0JpQ
- youtu.be/3LU1xsUrKV4
- youtu.be/N_Y3UoDsum4
- youtu.be/u1vhSwBgfxA
- Shoulder pain PUK
- Shoulder pain Medscape
Frozen shoulder
Lennard Funk 2008
Frozen shoulder is an extremely disabling condition, presenting with and remitting shoulder pain and stiffness.
This was well defined by Codman in 1934, who described the first and best classical diagnostic criteria still used to this day:
1. Global restriction of shoulder movement.
2. Idiopathic etiology.
3. Usually painful at the outset.
4. Normal x-ray.
5. Limitation of external rotation and elevation.
This is a distinct pathological condition identified by global limitation of glenohumeral motion, with a loss of compliance of the shoulder capsule, with no specific underlying cause found.
A secondary stiff shoulder or secondary frozen shoulder, typically presents after injury or surgery.
It may also follow an accompanying condition, such as subacromial impingement or a rotator cuff tear.
Diagnosis: The diagnosis of a primary Idiopathic frozen shoulder is made on the basis of:
1. Age: Typically occurring in females more common than males, in the 4th and 5th decade.
2. Pain: The pain is of a constant nature, severe, affecting sleep. There is often a toothache pain at rest, with sharp pains with forceful movements.
3. Loss of external rotation: The typical loss of external rotation is such that passive external rotation is <60 degrees from the sagittal plane. A secondary frozen shoulder usually has restriction of external rotation, which is beyond 0 degrees (i.e. external rotation of 10 degrees as opposed to -10 degrees with a primary frozen shoulder).
Natural History: The natural history of a frozen shoulder has typically been described as passing through 3 stages over 2 years.
Stage
Duration
Symptoms
Freezing
3m
pain+ and global restriction of function
Frozen
3-9 m
pain at extreme range of movement and marked stiffness
Thawing
9-18 m
usually painless and the stiffness starts to gradual resolve at this stage
Aetiology: The frozen shoulder has been found to be more common in association with the following conditions:
1. Diabetes (10-20% association). There is a 2-4 times increased risk for diabetics of developing frozen shoulder. Insulin-dependent diabetics have a 36% chance of developing it, 10% bilaterally and the condition is more severe in diabetics.
2. Cardiac/lipid problems.
3. Epilepsy.
4. Endocrine abnormalities, particularly hypothyroidism.
5. Trauma.
6. Drugs MMPI.
Pathology: The microscopic appearance is that of thickening of the anterior capsule, particularly the middle glenohumeral ligament. There is villonodular synovitis within the rotator interval with thickening and contracture of the coracohumeral ligament. There is a reduced glenohumeral joint volume.
Coracohumeral ligament (circled) in the rotator interval, which becomes thickened and limits external rotation.
Microscopically there are 4 stages:
1. Inflammatory synovitis with capsule unaffected.
2. Proliferative synovitis, which is hypertrophic.
3. Maturation of the capsule, with reduced vascularity.
4. Burnt out synovium with a dense scar appearance.
Tim Bunker in 1995 has shown the pathology to be similar to Dupuytren’s disease with increased collagen, myofibroblast and fibroplasia.
This in association with Trisomy 7 & 8, 58% of patients who had a primary idiopathic frozen shoulder had Dupuytren’s disease elsewhere.
The inflammatory drivers for Dupuytren’s disease and frozen shoulder are similar, these being TGF-beta and PDGF.
Arthroscopy of the shoulder, showing villonodular synovitis in the rotator interval.
Treatments: The natural history of frozen shoulder is not necessarily that of complete resolution.
The original quotation that most recover from frozen shoulder originates from Codman in 1934.
However, he stated that most frozen shoulders recover compared to tuberculosis.
Many studies have shown frozen shoulder not to be an entirely self limiting condition and most patients still have some restriction of shoulder movement on resolution of the frozen shoulder but no functional disability (Grey JBJSA 1962, Shaffer JBJSA 1992, Bunker JBJSB 1995, Miller Orthopaedics 1996).
The treatment options range from:
1. Nothing.
2. Physiotherapy.
3. Distention injections.
4. Locally acting steroid injections.
5. Manipulation under anaesthetics.
6. Open/Arthroscopic capsular release.
Non-Operative Treatment: Studies on non-operative treatments for frozen shoulder have shown that physiotherapy improves range of movement but not necessarily pain relief. Steroid injections have a benefit for short-term pain relief only but no long-term pain relief
(Ryan’s Rheumatology 2005, Haslan and Celiker Rheumatol int 2001, Bulgnann Ragum Dis 1984).
Hydrodilatation has become increasingly popular recently. The procedure is performed under local anaesthetic, takes about 15 minutes to complete and the patient goes home immediately afterwards. The procedure appears to be safe with transient pain during and after the procedure being the most common complaint. Most have included corticosteroid as part of the procedure but it is not known if this is necessary. It is also not known whether arthrographic distension using steroid and saline is better than intra-articular steroid injection alone. There is some evidence that arthrographic distension provides short-term benefits in pain, range of movement and function in Frozen Shoulder. It is uncertain whether this is better than alternative interventions.
Surgery: Early surgery has been shown to be of significant benefit for a faster recovery of pain, quicker recovery of function and earlier return to work (Hill Orthopaedics 1988, Doddonhoff JSES 2000). Arthroscopic capsular release has been shown to avoid the complications of manipulation under anaesthetic. It has the advantage of being able to identify any other associated pathologies. Numerous studies have demonstrated the benefit of capsular release, although no study that we are aware of randomises patients directly comparing MUA to arthroscopic release. Our own study of 48 patients undergoing capsular release followed for 18 months, demonstrated significant improvement by 5 months postoperatively for resistant frozen shoulders. The Constant score improved from 14 preoperatively to 66 postoperatively, with 80% satisfaction. Range of movement improved significantly by 5 months (Boutros, Snow and Funk 2006).
Arthroscopic release of contracted (red) middle glenohumeral ligament.
Treatment Algorhythm. Treatment algorhythm is based on the ability of patients to cope and the significance to cope with the pain and stiffness during the stages of frozen shoulder and not based on the stage itself.
Primary idiopathic frozen shoulder is an extremely disabling condition, which does pass through a typical 3 stage progression. However, full recovery at the conclusion of the 3 phases is not common. Early surgical intervention has significant benefits for those patients that are unable to cope with non-operative treatment.
For more information see: www.shoulderdoc.co.uk
Glenohumeral instability
Dislocated shoulder
- Dislocated Shoulder Medscape
- Dislocated Shoulder Medscape
- Dislocated Shoulder Medscape
- youtu.be/CGvy6sA2OD4
- youtu.be/xDePRKeB4kc
- youtu.be/a5YRjLRz0Lo
- youtu.be/2wiIlT6_YLM
- youtu.be/jIVjVRXo79w
- youtu.be/LSW2apXq-cU
Acromioclavicular subluxation / dislocation
Thoracic outlet syndrome
Reflex sympathetic dystrophy
Elbow anatomy
Elbow conditions
Elbow examination
- hacking-medschool/elbow-examination
- ucsd.edu/joints4
- youtu.be/wRUkpGoiUZ8
- youtu.be/v=3s_kzqQMmNE
- youtu.be/4M_lNVlpKCQ
- youtu.be/96EMB7SWF0I
- youtu.be/zH5z3bpyuuI
Elbow assessment
Elbow & Forearm
The Elbow joint consists of the main radio-humeral hinge joint plus the ulnar-humeral and superior radio-ulnar joints which allow pronation and supination of the wrist. ( see”ottowa” elbow rules). Fractures are common but sometimes difficult to detect even on xray. Refer significant pain swelling or loss of function especially children. Myositis Ossificans not uncommon at elbow – encourage early mobilistation
Look
for injury/deformity/swelling (bony, soft tissue, fluid) redness old injury or scars skin changes (psoriasis) due to joint or other disease signs of infection or inflammation (olecramon bursitis)
Feel
Gently palpate around the elbow joint including the bony landmarks .Feel for temperature swelling tenderness bony abnormalities
Move
Quickly rule out shoulder dysfunction by asking the patient to put the hands behind the back of the head with the elbows well back.
Active Movements
The Wrist is a simple hinge joint (like the knee) and can move in one plane only.
Ask patient to bend arm as fully as possible (flexion) then straighten them out (extension) Note whether patient can extend fully.
(Note supination and pronation occurs at the superior radioulnar joint and the wrist)
Passive Movements
Repeat the above movements moving elbow yourself.
Tests of function
Ask patient to pour and drink a glass of water
Put a cardigan or coat on
Normal findings/ROM
flexion 0-140 degrees
extension 0 degrees
pronation/supination 0-180 degrees
Common abnormalities
Tennis Elbow
Golfers Elbow
Olecranon Bursitis
Pulled elbow in Children
Tennis elbow lateral epicondylitis
Tenderness at lateral epicondyle
Pain maximal on resisted wrist extension
Recovery can take weeks to months
Golfer’s elbow (medial epicondylitis)
Similar self-limiting condition with management as above.
Occasionally associated with ulnar neuropathy.
Olecranon bursitis
Ulnar neuritis
Elbow fractures and dislocations
(a) Supracondylar Fractures. Admit all Supracondylar fractures for Neurovascular observation.
Collar and Cuff sling +/backslab.
Never use a completed LA-POP in these patients.
(b) Radial Head Fractures. Displaced fractures may need internal fixation. Obtain orthol_paedic advice. Undisplaced # may not be visible. You should look for a + Fat-pad sign indicating Haemarthrosis.
Treat with sling. Review # Clinic 2 weeks.
(c) Pulled Elbow. e.g. Small child pulled by arm axially (e.g. in a shop).
X-Ray often unhelpful.
Reduce by pronation \ supination of elbow flexed to 90 degrees with axial compression. Normal function should return within 5¬10 mins. No review necessary.
Monteggia fracture
Colles fracture
Wrist anatomy
Wrist pain & injury
The wrist joint comprises 2 rows of 4 small carpal bones sitting in a shallow cup formed by the with radius and ulnar above and articulating with the metacarpal bones of the thumb and fingers distally. The joint allows flexion extension abduction and adductio. Pronation and supination of the wrist occur at the inferior radioulnar joint.
The wrist is vulnerable to falls on the outstretched hand, overuse injuries together with inflammatory or degenerative conditions (Rheumatoid arthritis,
Osteoarthritis, gout) and conditions peculiar to the
area conditions and other specific entities such as Carpal Tunnel Syndrome and DeQuervains Tenosynovitis
Red Flags
Grss deformity or exposure of underlying structures such as bone, nerves, tendons
Weakness or inability to move wrist, hand or fingers
Significant swelling
Pallor, coldness, numbness, or decreased pulses and capillary refill
Uncontrolled bleeding
Signs of shock
Beware Missed Scaphoid Fracture
Cervical Sponylosis can refer pain to the wrist.
Soft tissue injuries
Soft-tissue injuries of the wrist consist of sprains, strains, or dislocations. Sprains and strains are a common injury to the wrist and typically are caused by falling forward, pushing on heavy objects, or sports injuries.
Dislocation is an injury to the ligaments that surround the joint which results in separation of the aritcular surface of the joint. Dislocations to the wrist are typically caused by falls, sports injuries, or motor vehicle accidents and require immediate reduction to prevent neurovascular compromise.
Fractures
Falls on a hyper extended wrist and motor vehicle accidents cause most wrist fractures. Wrist fractures are complex because of the small size and large number of the carpal bones. The two most common fractures of the wrist are Colles fractures and fractures of the scaphoid bone. Colles fracture includes injury to the distal radius and ulna, usually caused by a fall on an outstretched hand. Scaphoid fractures are often difficult to appreciate on x-ray, therefore any “snuffbox” tenderness along with history of injury should be enough reason to apply a thumb spica splint and provide orthopedic follow-up.
Lacerations
Cuts that occur over a joint may not heal well without suturing due to the constant movement of the joint. Lacerations to the wrist should warrant assessment for nerve or tendon damange which would be identified by inability to move fingers . If assessment is positive for potential nerve or tendon damage, a referral for a hand surgeon should be arranged.
Tenosynovitis of Wrist
De Quervains Stensoing Tenovaginitis
The tendon sheath of EPB and APL of the thumb become inflamed due to overuse leading to pain and swelling on the radial side of the wrist. Resisted Abduction of the thumb is positive. (Finkelsteins test)
The wrist may be involved in OA particularly if previously damaged by fracture involving the joint surface or complications of scaphoid or lunate fractures. Active RhA may involve the wrist causing pain swelling deformity and instability and may also cause rupture of the extensor tendons at the wrist.
Hand and wrist examination
- hacking-medschool/wrist-hand
- youtu.be/65mjCLGrGTE
- youtu.be/Yw2b-c2shWE
- youtu.be/yDPt842bdic
- youtu.be/SqpPvJLNYE
- youtu.be/lYq2YihhIg
- youtu.be/dUwpNf1QSA0
- youtu.be/UFIqkMZ_l0c
- youtu.be/bovmH1-gT68
Wrist and hand injuries are common, as are infections, involvement in inflammatory or degenerative conditions (Rheumatoid arthritis, Osteoarthritis, gout) and conditions peculiar to the area (deQuervains stenosing tenovaginitis, paratendinitis crepitans, Carpal Tunnel Syndrome).
Be sure to examine all of the movements of all of the joints of the fingers and thumb
Red flags
Digital Nerve injuries often missed any alteration or difference in sensation needs referral (pencil test)
Apparently superficial injury may hide deeper damage to tendons and nerves.
Beware missing collateral and volar plate injrie to IP jointsligament
Again test sensation, explore wounds fully, and check full strength movement against resistance.
Scaphoid Injuries are still missed . Possible fractures should be referred/ sent back for review.
Grease Gun Injuries
Palm space Infections
Examination
Look for injury/deformity/swelling (bony, soft tissue, fluid) redness/ wasting of the thenar or hypothenar eminence/ old injury scarring or contracture, nail changes due to joint or other disease
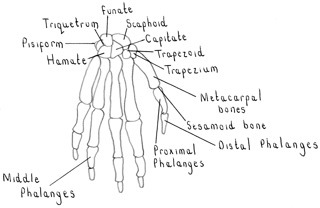
Feel Palpate around wrist and small joints of the hand: carpal bones, carpometacarpal, metacarpophalangeal, proximal interphalangeal, distal interphalangeal, as well as IP joint in the thumb palpate carefully within the anatomical snuffbox in wrist injury to not miss the scaphoid(Small bones of the wrist – Scaphoid Capitate Trapezuim Trapezoid Triquetral Lunate Hamate Pisiform)
Feel for temperature swelling tenderness bony abnormalities
Squeeze across the MCP joints to detect pain +/- tenderness.
Move
Wrist Movements
With the elbows flexed at 90 degrees and held pinned to the patients side
Ask the patient to turn their palms towards the floor (pronation)
and then towards the sky (supination)
Ask the patient to adopt the prayer position (palms together – flexion)
then the inverse prayer position (backs of hands together – extension)
With the arms still tucked firmly by the sides ask the patient to move the hands apart (abduction) then together (adduction)
Movements of the thumb
Place the back of the hand on the desk (or pillow) and fix the wrist to prevent interference with movement.
Ask the patient to curl their thumb (flexion) then straighten it out (extension)
Keeping the thumb straight (uncurled) ask the patient to move the thumb away from the palm (abduction) then to the palm (adduction) then touch tips of each finger in that hand with the tip of the thumb (opposition)
Finger Movements
Ask a patient to make a fist (flexion) then open it out (extension)
Wth the palms on the desk ask the patient to spread their fingers apart (abduction) and then back together (adduction) – both movements ulnar nerve ( T1?)
PAD Palmar interossei ADDUCT
DAB Dorsal intereossei ABDUCT
Grip Strength – ask patient to squeeze your finger tightly
Passive Movements
Repeat the above movements moving the hand or digit yourself
Tests for Tendon Function and Integrity
-with the hand on the desk palm upwards, and the PIP held in extension by the examiner get the patient to actively flex the fingertip at the DIP (flexor digitorum profundus)
-next test flexor digitorum superficialis by by asking patient to actively flex each finger at the PIP whilst holding the other 3 fingers in extension
test again agains resistance if any doubt re the strenght / integrity of the tendons
Special Tests
Tinels Test – tap the flexor surface of the wrist repeatedly for 30secs to attemprt to ellicit the synptoms of CTS
Phalens – put the wrists in inverse prayer position for 60 secs to try to reproduce the symptoms of CTS
Test for the presence of myotonia by asking the patient to make a fist and
then open it quickly. A patient with myotonia will not be able to pertorm this action quickly.
Test sensation
Test the modalities of light touch, pain, vibration sense and joint position sense in both penpheral nerve and dermatome distnbutions.
Peripheral nerve distnbutions are tested as follows:
• Radial nerve: touch in the anatomical snuffbox on the dorsal aspect.
• Ulnar nerve: touch over tile medial one and a half lingers on the palm (little linger, and medial half of ring finger).
• Median nerve: touch over the lateral three and a hall fingers on the palm (lateral hall of ring linger, middle finger, Index finger and thumb).
Assess pulses
Palpate the radial and ulnar pulses. You may also wish to pertorm Allan’s test of perfusion of the hand.
Allan’s Test • Ask the patient to make a fist. • Occlude both the radial and ulnar arteries by pressing over them.
• Press for 5 seconds. • Ask the patient to open the palm and release the pressure on each artery in turn and watch the colour of the palm.
• It should change tram pale to pink as blood flow Is re-established.
Froment’s sign
To do this, ask the patient to hold a piece of paper/card between the thumbs and the radial aspect of the index finger. Then pull the paper away and ask the patient to stop it. With paralysIs ot adductor pollicis, the thumb will flex at the interphaiangeal joint.
Finklestein’s test
Ask the patient to flex their thumb. Now, ulnar deviate the wrist. Pain is indicative of De Quervain’s tenosynovitis.
Types of Grip
precision grip – roll a coin between finger and thumb
ball grip – pick up a tennis ball
flat pinch hold a key between forefinger and thumb
writing – holding a pen
hook grip carrying a suitcase
unscrewing – the lid of a jar
Other Tests Of Function
ask patient to write name
fasten and unfasten a button
pour and drink a glass of water
Normal findings – ROM hand & wrist + dermatomes +/- myotomes and reflexes
Wrist :
Flexion 0-80 degrees
Extension 0-70 degrees
Abduction 0-20 degrees (radial deviation)
Adduction 0-30 degrees (ulnar deviation)
Carpometacarpal joint of thumb:
Flexion 0-15
Ext 0-20
Abduction 0-70
Plus MCP joints
Flex 0-50 thumb 0-90 fingers
Ext 0 thumb 0-20 fingers
IP joints
Flexion ip thumb 0-65 pip fingers 0-100 DIP 0-70
Extension 0-20 degrees 0 degrees 0 degrees
Common abnormalities
Osteooarthritis of the hands may produce bony swellings at the DIP (Heberdens) and the PIPs (Bouchards).
RhA produces radial deviation at the wrist, ulnar deviation of the fingers Zshaped thumbs Boutonniere and swan-neck deformity of the fingers
Dupuytrens
CTS
DeQuervains
Tenosynovitis wrist
acute tenosynovitis/tendovaginitis
Ganglion
Subcutaneous cystic swelling on the dorsum of wrist (occasionally foot and ankle).
Carpal Tunnel Syndrome
Due to median nerve compression beneath the anterior carpal ligament (flexor retinaculum) at the wrist – causing burning, tingling or pain to the forearm, hand, wrist, and fingers (thumb, index, middle and half of the ring finger) worse at night.
There may be weakness of thumb abduction and opposition and wasting of the thenar eminence. Diagnosis supported by reproduction of symptoms in positive Phalens test (wrists fully palmar flexed for 1 minute) or Tinels Test (tapping the nerve over the tunnel at the wrist).
Risk factors include RHA pregnancy hypothyroidism menopause, gout, acromegaly. Treatment is via splinting or surgery.
Painful tingling of hands due to compression of median nerve at wrist.
May be weakness/wasting of small muscles of hand and thumb – eg opponens polliciand abductor pollicis brevis – with sensory loss over palmar aspect of thumb index middle and radial half of the ring finger.
Causes- idiopathic, pregnancy, premenstrual oedema, RhA, hypothyroidism, trauma, amyloid.
- http://orthoinfo.aaos.org/topic.cfm?topic=a00005
- DTB 2009;47:86–89
- youtu.be/u5dWTGYQ6PU
- youtu.be/xuCjuLOSFK8
- youtu.be/gLYsnD3JHfA
- youtu.be/xoeJbyR7k4Q
Scaphoid fracture
Perilunate subluxation
Perilunate subluxation capitate
Hand anatomy
- Hand anatomy Medscape
- eatonhand.com
- youtu.be/ztUdLyuYc2Q
- youtu.be/7NsRPttX2Uo
- youtu.be/P22ajLcv-h4
- youtu.be/CDKI46yPmJw
- youtu.be/vlwAoKpSI7s
Hand examination
- hacking-medschool/wrist-hand
- ucsd.edu/joints3
- youtu.be/QR151fDUQN4
- youtu.be/ysWOHe4dfpI
- youtu.be/65mjCLGrGTE
- youtu.be/bovmH1-gT68
- youtu.be/iXu8v1S__Ds
- youtu.be/REn2dlFQBzA
- youtu.be/jjofSxoCL0Q
- youtu.be/_SqpPvJLNYE
Hand injuries
- youtu.be/8MovgvhWmwg
- youtu.be/pDrAgTXEgNg
- Soft Tissue Hand Injury Medscape
- Hand Injuries PUK
- Hand Injuries I AAFP 2004
- Hand Injuries II AAFP 2004
Hand Injuries and conditions
Always record the mechanism of injury and examine and record the function of underlying flexor and extensor tendons and digital nerves.
X-Ray all wounds caused by glass to exclude the presence of retained foreign bodies. Remember that wounds caused by glass and by knife blades often extend through all soft tissues to bone.
Warn patient about jump Conduction (a completely divided nerve may continue to conduct for up to 48 hours until the distal portion degenerates). Warn also about the possibility of Delayed tendon rupture ( A partly divided tendon may later rupture when subjected to force.
Nail bed injuries These should be repaired so as to leave a flat surface, otherwise nail dystrophy will result.
Finger tip infection Paronycheal infection and pulp space infection should be drained to decompress.
Extensor avulsion Mallet & Boutonniere injuries should be treated by splintage.
Tendon Injury. Injury to tendons should be identified & treated early to minimise complications and disability.
Digital Nerve Injury
Digital Nerve injury can be referred to Plastic Surgery; consult with the on-call Plastic Surgeon in the Ulster Hospital Dundonald. For injuries to Extensor tendons or flexor injuries other than in the hand or wrist, you should seek the assistance of the Orthopaedic team here.
Arterial bleeding
Arterial bleeding emanating from the hand (or elsewhere) should be controlled by firm direct pressure with elevation. The hand should be assessed for signs of nerve injury (which is often associated) and tendon damage. If you are unfamiliar with exploration of hand wounds you should seek the help of the Surgical or Orthopaedic SHO. Bleeding should be brought under control before any transfer (e.g. to Plastic Surgery) is contemplated, but you should avoid blind application of artery forceps into the depths of a bleeding wound as this is likely to compound any neurovascular damage.
Volar Plate Avulsion Injury.
Hyperextension of a Proximal IP joint may result in tearing of the volar condensation of the joint capsule (on palmar surface). This can be accompanied by a small avulsion fracture from palmar base of middle phalynx. The injury is a significant one which will result in a haemarthrosis and can result in permanent swelling and stiffness of PIP. Irrespective of presence of # treat with Zimmer splint and review at 10 days to commence mobilisation.
High pressure jet injury.
Occurs with pressurised paint or oil sprays and will result in small puncture of finger tip with extensive spreading of irritant chemicals etc. into soft tissues and tendon sheath in hand. This injury will at first appear innocuous but will subsequently result in serious inflammation within teMon sheaths and may result in ischaemia, necrosis, dense adhesion formation and significant anatomical and functional disturbances. Admit for exploration.
Hand Splintage.
Hands should be splinted in a position of MCP flexion, lP extension using Zimmer splint (preferably on one surface only) or POP slab. Immobilise the joint on each side of the injury. Use a high sling and adequate analgesia.
Hand Injuries
Carpal
These occur with falls onto the hand. Scaphoid fracture
Diagnose clinically by tenderness in ASB and over palmar scaphoid tubercle. An X-ray should be performed to exclude other injuries and abnormalities. Apply Scaphoid POP and arrange fracture clinic referral.
Most other carpal fractures are rare, except for avulsion of dorsal aspect (with forced wrist flexion) Treat these in neutral POP
Beware Lunnate dislocation and trans-scaphoid perilunar wrist dislocation.
Hand conditions
Metacarpal fractures
Boxers fracture (5th MC neck) Scrapping x 2 weeks Refer to fracture clinic. Warn patient about residual deformity.
Displaced # I1-IV Manipulate, check X-ray, Refer # clinic. Where there is more than one fracture POP/ Vol. r slab would be appropriate.
Bennetts # These are often displaced and because of the pull of long tendons may be difficult to reduce. If so internal fixation may be appropriate
OA hands
OA thumb
OA at the base of the thumb BMJ Nov 2011
Dupuytrens contracture
Palpable thickening, fibrosis and contracture of palmar fascial aponeurosis and tendons causing flexion deformities of MCP joints espescially ring and middle fingers.
Causes
Idiopathic and familial
Traumatic/Occupational – gardeners – vibrating machines
Epilepsy
RhA
Liver disease espescially portal hypertension
Xiapex (clostridium histolyticum)
Trigger finger/thumb
Idiopathic thickening – with nodule formation – of fibrous flexor sheath at base of finger (or thumb). The thickened tendon or nodule becomes stuck in the tendon sheath when the finger is flexed – and the finger has to be released by passively extending the digit using the other hand.
Volkmanns ischaemic contracture
Finger injuries
Injuries to the fingers occur frequently during sports activities and within a variety of occupational settings. The most common injuries include fractures, dislocations and lacerations. Proper evaluation, treatment and referral are necessary to prevent improper healing and loss of function of the digits.
Red Flags
Amputation
Signs/symptoms of shock
Signs of neurovascular compromise – pallor, loss of sensation, cold digit
Missed Collateral ligament rupture
Traumatic finger injuries include lacerations, dislocations, tendon/ligament disruptions and fractures. The most common injuries will be discussed below.
Key anatomy of the fingers include the bones: proximal, middle, and distal phalanges (the thumb has only proximal and distal); and the three joints of the fingers: the metacarpophalangeal (MCP) is the knuckle of the hand; the proximal interphalangeal (PIP) joint and the distal interphalangeal (DIP) joint.
Extensor tendons are located on the dorsal aspect of the hand whereas the flexor tendons are located on the palmar or volar aspect.
Lacerations
Lacerations involving the digits occur frequently and may be simple or complex. Wounds must be copiously irrigated and explored in a bloodless field (use a tourniquet if necessary but always ensure this is removed!) and the affected finger moved through full range of motion to evaluate for tendon, ligament, muscle or bone injury.
Simple lacerations may be closed using proper techniques.
Complex lacerations involving underlying structures require consultation with a hand surgeon for immediate or delayed repair. Lacerations involving the fingernail may involve the nail bed. Such injury may require nail removal and repair of the nail bed injury.
Dislocations
Dislocations of the PIP joint are common – often from a ball striking the end of an extended digit. Most can be reduced by traction. Athletes may present with history of dislocation that was reduced by the player or coach. These still need to be X-rayed and splinted even if the gross appearance of the digit is normal. DIP joint dislocations are uncommon and often are accompanied by significant fracture around the joint, requiring evaluation by hand surgery.
Tendon and ligament disruptions
One of the most common tendon injuries to the digits is known as mallet finger. The patient will present with the tip of the finger in flexion, with inability to straighten at the DIP joint. This often occurs when a ball strikes the tip of a flexed finger. X-rays and splinting the finger in full extension is necessary with close orthopedic follow up.
Skier’s or gamekeeper’s thumb occurs when the thumb is bent backward (acutely abducted) during a fall and injures the ulnar collateral ligament – a ligament running along the base of the thumb. These injuries must be x-rayed, placed in a spica splint and sent for orthopedic referral.
Fractures
Fractures of the fingers occur from a variety of forces including crush injuries and hyperextension/flexion of the interphalangeal(IP) joints. Avulsion fractures are common at the IP joints and may be difficult to detect on X-rays. Distal phalanx or “tuft” fractures that do not involve the joint and phalangeal shaft fractures may be managed by splinting alone. Fractures involving large avulsions at the joint or the joint itself mandate splinting and orthopedic referral.
Other Injuries
Subungual hematoma is bleeding under the fingernail, usually secondary to crush injury. If the patient presents within a few hours of injury, the blood can be drained from under the nail by means of an electro-cautery device or by boring an 18 gauge needle through the nail until blood spontaneously drains from the opening.
Paronychia is an infection along the border of the fingernail. This occurs more frequently in patients who bite their nails. Treatment includes incision and drainage of the infected space, warm soaks and antibiotics.
Felon is an infection of the finger pad, or the distal fleshy aspect of the finger opposite of the fingernail. This is often caused by a puncture wound which becomes secondarily infected. Incision, drainage and antibiotics with close follow up for re-evaluation are crucial aspects of care.
Test full range of motion of affected digit, compare to opposite hand
Neurovascular exam – including 2 point discrimination (use a paper clip – normal range for fingertip is 2-5mm); extending wrist and fingers (radial nerve); spreading fingers against resistance (ulnar nerve); opposing the thumb against resistance (median nerve); capillary refill and radial/ulnar pulses.
X-ray – before and after reduction
Finger fracture
Check for rotational deformity which is particularily likely in fractures of proximal phalynx. Following reduction check X-Ray in splint. Splint hands with MCP Flexion and IP Extension. If reduction is unstable or not possible (eg due to interposition of soft tissues) get orthopaedic advice re? admission for internal fixation. See section on Hand Injuries
Finger tip injury
In Children treat these conservatively with Steristrips and Occlusive dressings (e.g. Flammazine). Suturing is normally not necessary.
In adults use Digital Nerve Block to ensure wound is cleaned thoroughly. Where bone is protruding this would usually require trimming to obtain soft-tissue cover.
Mallet finger
These should be kept in extension in a mallet splint for 6 weeks with 4 weeks night splintage thereafter if successful. Instruct patient to keep splint on and dry. Refer to fracture clinic.
Ring removal
Removal of a ring from a digit may be necessary if a patient is unable to remove the ring and has impending or existing swelling of the digit or surrounding area or is developing numbness or impaired circulation to the digit. A ring which becomes too tight can cause sufficient pressure on the digit arteries to cut off the circulation to the digit distal to the ring and in extreme circumstances this could lead to loss of the digit.
Digit swelling may be secondary to trauma to the digit itself or to a more proximal part of the extremity, or as a result of soft tissue swelling such as in congestive heart failure, fluid retention in pregnancy or inflammatory processes such as arthritis.
Key Issues
Red Flag Warnings
Pallor, numbness, coldness, decrease or absent pulses in the digit
Decreased capillary refill
Severe pain
More proximal swelling which could extent to the digit over time
Immediate Care Considerations
Assess neurovascular status of the digit
Capillary refill
Digital pulses
Sensation
Elevate affected area
Ice affected area
Stabilize and immobilize affected area if trauma suspected
Background Information
Timely removal of a ring is important. It is better to remove a ring before it has become too tight than to wait for this to happen. This could prevent a trip to A&E during the night!
Many injuries cause swelling and even if the injury is not to the digit itself, the digits may swell secondarily. The same applies to swelling arising for other reasons. If a ring becomes tight this can lead to nerve or vascular injury with impairment of sensation of circulation and in extreme cases loss of the digit as a result. Neurovascular status of the digit should be assessed before and after removing the ring.
When assessing neurovascular compromise keep in mind the 5 P’s
pain,
pallor,
pulses,
paraesthesia,
and paralysis.
Follow your own departmental policy on obtaining signed consent for removal of the ring and documentation of the ring being returned to the patient.
Ring Removal Techniques
There are various techniques for ring removal.
The more commonly used are 1) ring cutting and 2) string wrap or pull technique.
When preparing to remove a ring keep in mind the urgency of the situation. If the patient’s circulation is compromised the first priority is the well being of the patient not the integrity of the ring. If the patient is not compromised in any way you can then take into account the value of the ring.
Ring cutting is typically used if the ring is thin and metal. This ring cutting tool has a special blade guard but the operator should be familiar with how to set up and use the tool ensuring that the guard is aligned properly so it will not cut/abrade the skin. Some ring cutters are manually operated while others may have an electric motor. Ring cutting kits sometimes include different blades for different metals, and if so it is important to ask the patient what type of metal their ring is made from and to use the correct blade. If the ring is loose enough for you to be able to identify the metal hall mark, the patient may appreciate you avoiding cutting through this as it will help retain the value of the ring. Be sensitive to the emotional connotations of cutting through a ring such as a wedding ring. Advise the patient of the consequences of non removal and reassure the likelihood of invisible repair.
The string technique is performed as follows:
Slip a piece of string under the ring while moving the ring toward the hand
The remainder of the string is then wound around the swollen part of the finger distal to the ring a number of times ((and soap applied ?))
The string is now unwound from the hand side pushing the ring forwards towards the tip of the finger
Repeat this process gradually easing the ring towards the finger tip to complete removal
Investigations
X-ray according to nature of any trauma or examination findings.
Treatments
Rest, ice, and elevate – while in the department and at home afterwards
Pain relief as required
Consider antihistamine (for swelling associated with insect bite/stings)
Consider the need for tetanus immunization if skin integrity is breeched
Discharge and Follow Up Considerations
Advise the patient to report any changes in sensation, color, temperature, or any increase in pain.
Hip / groin exam
- hacking-medschool/groin-exam
- ucsd.edu/joints5
- youtu.be/VuHsa4kxT0s
- youtu.be/4IYgyXMpfik
- youtu.be/5LNYdJIrWYo
- youtu.be/FyFFnW5_qms
Hip Thigh Pelvis
The hip is a stable ball and socket joint surrounded and stablised by a large muscle mass. Injuries include FNOF in elderly, Hamstring tears and haematomas.
Common atraumatic conditions are OA hip, trochanteric bursitis.
Red flags
Hip pathology may present with knee pain as they share obturator and femoral nerve supply.
Beware Child with spontaneous limp – often transient synovitis of hip but sometimes SUFE (teenager) or Perthes (5-9 years)
Beware quads/patellar injury after minor injury or stumble in elderly – refer if cant SLR.
Examination
Undress patient down to underwear. Use blanket for modesty. Patient standing initially.
Inspect
front and back – deformity, scars, soft tissue or bony swelling, level of iliac crests, raised gluteal folds
Examine gait pattern, use of walking aid, stride length, pain.
Palpate
Bony landmarks ASIS Ischial spine greater trochanter
Move
With the patient supine
Fix the pelvis by placing your hand on the opposite iliac crest – so that movements are indeed from the hip and not the pelvis
Flexion – ask the patient to bring the heel up to the bottom
Abduction – ask the patient to move the straight leg away from the midline
Adduction – ask the patient to move the straight leg across the midline
Ask the patient to roll over so they are now prone
then raise each leg off the bed
ask the patient to keep the knees together and rotate the ankles outwards then inwards
Repeat Active Movements
Special tests
Trendelenburg test
• Observe the patient from behind.
Ask them to support their weight on the right hip only (ie ask them to lift the left leg off the ground by bending the knee).
• Watch the pelvis, and note the direction of tilt. (In nonmal individuals, the pelvis will rise on the side of the leg that has been lifted. With instability, the pelvis may drop on the side of the leg that has been lifted.) Repeat the test, with the patient standing on the other leg.
Thomas’ test
• Put your left hand (palm upwards) beneath the lumbar spine to ensure that the lumbar spine remains flattened during the test.
• With the other hand, passively flex one hip.
• While you are flexing this hip, observe the movement of the other leg – in the event of a fixed flexion deformity (common in hip osteoarthritis), the opposite leg flexes too. Repeat other side.
Test function
Gait Should have been assessed earlier in your examination.
Normal findings/ROM
flexion 0-120 degrees
ext 0-20 degrees
abduction 0-45 degrees
adduction 0-30 degrees
medial rotat 0-35 degrees
lateral rotat 0-35 degrees
Groin Exam — hernia scrotum
Thigh Exam
Femur + surrounding muscles + soft tissues -Quadriceps anteriorly and hamstrings posteriorly
Soft tissue injuries.
The groups of muscles located in the back of the thigh are the hamstrings and are commonly sprained or strained in athletes or sports injury. A hamstring injury typically occurs when the knee is extended and the hip flexed as the person falls forward.
The anterior groups of thigh muscles are the quadriceps. The rectus femorus muscle tear and groin strain are the two most common injuries with the quadriceps. Clinical manifestations of strains and sprains are similar and most are self-limiting with full function restored in 3 to 6 weeks.
Blunt Injury/Lacerations
Lacerations that occur to the thigh may be minor cuts or abrasions or major penetrating injuries such as gunshots, knife wounds, or foreign bodies such as tree branches from a fall or glass. When these types of injuries occur the depth of the injury as well as possible damage to the underlying structures (arteries, nerves, tendons, and ligaments) should be considered.
Thigh Adductors
Observe three ducks pecking grass
Obturator, three adductors (longus, brevis, magnus) Pectineus Gracilus (Obturator, femoral plus sciatic nerves)
Hamstrings (posterior compartment)
Big fat swotty Samantha ate my hamsters pens (Khalid Khan Mnemonics & Study Tips For Medical Students)
Biceps femoris, Semitendinosous Semimembranous Adductor Muscle Hamstring Portion
Say Grace Before Tea
Sartorious & Gracilis Before Semitendinosus
Hip and groin conditions
- Medscape Groin injuries
- Medscape Hip Tendonitis and Bursitis
- Medscape Ilopsoas Tendinosis
- Medscape Adductor Strain
- Medscape Hip Pointers
- Osteitis Pubis
- hipandgroinclinic.ie hip arthroscopy
- london hip arthroscopy centre hip-and-groin-conditions-labrum
- cjsmblog.com hip and groin conditions
- manchester hip arthroscopy.com hip-conditions
Lower limb injuries
Tibia
Tibial fractures should normally be admitted after consultation with the staff of the Orthopaedic Unit. Immobilisation prior to fixation may be achieved with a Frac Pac or POP slab.
Ankle
Minor fractures can be managed with Wool/Crepe bandaging and NWB with crutches. Encourage elevation.
For Displaced/ Bilateral/ Subtalar joint injury admit for elevation as these invariably swell considerably. Do not apply POP initially. With os calcis fractures ensure that your examination excludes fractures of the proximal skeleton e.g.. Knee, hip, spine
Pelvis
Admit pelvic fractures.
For high velocity injuries remember the possibility of urethral and vascular injury. Pelvic injuries may be masked in patients with other painful injuries and in those with multiple injuries.
In serious trauma a pelvic X-Ray should be done as a routine as pelvic injury may be concealed, is common, and can result in considerable concealed blood loss.
Ankle Pilon Fracture
Fractures Os Calcis?
FNOF Hip Fracture
Fractured Femur
OA hip
Elderly patient with slowly progressive pain and stiffness in hip, groin, anterior thigh (and often knee). Worse on movement relieved by rest.
- OA PUK
- AO AR UK
- Hip OA Orthopaedic weblinks
- youtu.be/om7y1IZIiPU
- youtu.be/8qcBKF-Jo4M
- youtu.be/r8mS4y0EmAw
OA hip management
Femoral acetabular impingement
- youtu.be/R4_3Fem4bM0
- youtu.be/JOqKKe-euIY
- youtu.be/Ggx7H58DI6k
- youtu.be/_BIko1erlCA
- youtu.be/7N0Zrd-F42Q
- youtu.be/k9BduZUbrXY
- youtu.be/nGA5Tpp77hk
- youtu.be/Rtp4oz0_3YY
Lateral hip pain trochanteric bursitis
Ischial Bursitis
- physioadvisor.com.au ischial bursitis
- Bursitis Medscape
- Bursitis in Emergency Medicine Medscape
- youtu.be/4uyOVvdlKdU
Piriformis
hacking-medschoo/piriformis-syndrome
Meralgia paraesthetica
Pins and needles and numbness along the lat side of the thigh due the entrapment of the lat cutaneous nerve of the thigh between the two fibres of the inguinal lig at the ant sup iliac spine (ASIS).
Rx: steroid injection and if it fails then operation
Usually pregnant or otherwise gaining weight
Thigh Pain Lateral thigh pain:
DD – trochanteric bursitis and meralgia paraesthetica
Trochanteric bursitis: pt c/o pain around the hip area but more pointing towards the upper lat aspect of the thigh, unable to lie on the effected side, pain on walking and getting up, may mimic hip arthritis.
Inv: none – clinical diagnosis mainly
Rx: nsaid, capsaicin cream and steroid injection which might need to be repeated.
Hamstring injury
Knee anatomy
Knee examination
The knee is a major weight bearing joint which relies on dynamic muscle contraction and intact ligaments for its stability.
Knee injuries injuries are common, and can often be correctly diagnosed by detailed attention to the history.
If there is full movement and the patient can weight bear the likely diagnosis is a simple sprain or contusion.
Rapid onset of swelling, locking + giving way (loose body) , inability to extend fully or weight bear are suggestive of more serious pathology.
Red flags
Beware Pain referred from hip and lower back
Rupture of Quadriceps tendon / patella tendon – always SLR
All effusions are significant and should be reviewed.
Meniscal and anterior cruciate ligament injuries are often missed at first presentation.
Examination
Expose both knees adequately. Clarify main site of pain.
Look
Observe gait
On the couch inspect in close detail for scars, small volumes of fluid, cysts, quadriceps muscle wasting (especillly medially) deformity/swelling (bony, soft tissue, fluid) redness or heat ( gout , prepaellar bursitis, septic arthritis) Q angle
Compare alignment and contours of knees
Feel
Palpate for heat and warmth swelling tenderness bony abnormality
palpate along the the quadriceps tendon, patella and patellar tendon
Palpate along the joint line (ask the patient to bend the knee slightly to identify this)
Palpate the patellofemoral joint, including beneath the patella for crepitus
Palpate the medial and collateral ligaments
Medial and lateral menisci
Milk bursa and patellar tap or bulge sign
Test for the presence of a joint effusion, using either the bulge test (if a little fluid is present) or the patellar tap test (for a larger volume of fluid).
Bulge test
Using the curve formed between your extended thumb and Index finger, milk down any fluid from above the knee.
Using your index and middle fingers together as a unit, sweep any fluid along the medial aspect of the knee. Then sweep along the lateral side of the knee, and watch to see if a bulge occurs on the opposite side
Move
Active Movements
Flexion Ask the patient to bend their knee to their buttock
Extension Ask the patient to straighten their leg fully
Passive Movements
Repeat the above movements moving the knee yourself.
Special Tests
Collateral ligaments
Lateral Collateral – flex knee to 30 degrees Support the medial aspect of the thigh, and push medially on the lower leg Medial Collateralhen – support the lateral aspect of the thigh, and push laterally on the lower leg
Excessive movement indicates ligament damage.
Cruciate ligaments
Anterior and posterior drawer tests
With the patient supine and relaxed on the couch. ask them to flex their knee to about 15 degrees
Palpate the bulk of the quadriceps muscles to ensure that the patient is relaxed.
Stabilise patients foot by sitting on it on couch ( make sure not painful!)
With the fingers of both hands round the back of the knee, keeping the thumbs in front over the patella. Position the thumbs so they point directly towards the ceiling.
Pull/push the unit you have formed with your hands forward and backward to test the anterior and posterior cruciates
Excessive movement indicates ligament damage.
Meniscal Tests (Apley’s grinding test)
Ask the patient to lie prone (face down) with the knee flexed to 90 degrees.
Use your left hand to stabilise the lower leg behind the knee and with the right hand grip the heel of the foot.
Twist the foot in a ‘grinding motion’.
A grinding sensation or pain indicates meniscal damage.
Tests of ligament integrity
Adduction stress test (medial collateral ligament)
Abduction stress test (lateral collateral ligament)
Anterior draw test (anterior cruciate)
Posterior draw test posterior cruciate
McMurrys (rotation of tibia on menisci at 90 degrees) or Aspleys grind and distraction tests
Rotation of foot
Normal findings – ROM
flexion 0-140 degrees
extension 0 degree
Common abnormalities/conditions
Chondromalacia
OA
Prepatellar Bursitis
Septic Arthritis
Gout
Meniscal Injury – follows sudden forced rotation of the upper leg (ie tibia) on a fixed lower limb tearing the meniscus sitting on the tibia
ACL – as above with associated high velocity impact to the side of the knee (loud pop, inability to weight bear immediately, immediate swelling within minutes- 1hr)
Investigations
Traumatic injuries may need referral for Xray if:
age>55, isolated patellar tenderness, tenderness over head of fibula, inability to flex to 90 degrees, inability to weight bear at time of injury and at examination.
WCC/ESR/CRP Rheumatoid screen again depending on clinical history and finding
- youtube.com/watch?v=eRPvoNe9Aho
- youtu.be/W5T42dFYaOg
- youtu.be/W5T42dFYaOg
- youtu.be/Irg3Cb4JaE8
- youtu.be/bHytLhg-1vM
- youtu.be/yQdBrr3Mmj0
- youtu.be/28mJFyHMXHo
- www.youtu.be/i-nFGqwr_VE
- www.youtu.be/fxKCDkOiJs
- www.youtu.be/ubP-1WaFeEc
Knee Special Tests
- youtu.be/vvebjHOjiLc
- youtu.be/dH_jnTy1rNk
- youtu.be/yOztSsiL2ng
- youtu.be/fkt1TOn1UfI
- youtu.be/w57I1cYXlCA
Calf Examination
Knee pain and injuries
Knee mechanisms of injury
Ottowa knee rule
Fractured Patella
youtu.be/Qe6VNxxOJaw
Fractured tibial plateau
Cruciate ligament Injuries
xxx
Osteochondritis dissecans
- Osteochondritis dissicans Medscape
- youtu.be/kPpLEfQBJfQ
- youtu.be/tAYvkMVr9Sk
- youtu.be/cjJz91R9Yg0
- youtu.be/l5rBhmgnCds
Anterior knee pain
Causes
chondromalacia patella (patellofemoral overload)
jumper’s knee,
prepatellar bursitis
PFD
Often teenage girls or athletes, c/o pain over the front of the knee or underneath the knee-cap, may be triggered by simple injury, pain is always worse on climbing up and down the stairs or when standing up after prolonged sitting, knee may give way or swells up, it sometimes catches but there is no true locking and it is often bilateral.
The knee may look normal but careful examination may reveal misalignment and quads wasting. Patella will be tender at the edges and Clark test (sharp pain when patella is forcibly pressed against femur and pt contracts the quad muscle suddenly) is +ve.
Rx – quad drill(stretching) exercises and physio usually cure the problem but remind the patient that it will take time. Refer to ortho if conservative Rx fails.
Infrapatellar bursitis may need aspiration and steroid injection
Q angle
OA Knee
Slowly progressive pain and stiffness precipitated both by activity and restriction of movement (cinema sign).
Patient may be obese and/or have history of previous injury/surgery/ or inflammatory arthritis some years previously
Exercises OA knee
Surgery for OA Knee
- youtu.be/MyO_eJLmZ5g
- youtu.be/uoL35NJz86w
- youtu.be/fyxDS9eCvVA
- youtu.be/dCBeGDCYVNk
- youtu.be/XwSa_hoCazs
NZ joint replacement criteria
Table NZ Priority criteria for major joint replacement (maximum score 100)
Pain (40%)
Degree (patient must be on maximum medical therapy at time of rating):
None 0
Mild: slight or occasional pain; patient has not altered patterns of activity or work 4
Mild-moderate: moderate or frequent pain; patient has not altered patterns of activity or work 6
Moderate: patient is active but has had to modify or give up some activities because of pain 9
Moderate-severe: fairly severe pain with substantially limited activities 14
Severe:major pain and serious limitation 20
Occurrence:
None or with first steps only 0
Only after long walks (30 minutes) 4
With all walking, mostly day pain 10
Significant, regular night pain 20
Functional activity (20%)
Time walked:
Unlimited 0
31-60 minutes (eg longer shopping trips to mall) 2
11-30minutes (eg gardening, grocery shopping) 4
2-10 minutes (eg trip to letter box) 6
<2 minutes or indoors only (more or less house bound) 8
Unable to walk 10
Other functional limitations (eg putting on shoes, managing stairs, sitting to standing, sexual activity, recreation or hobbies, walking aids needed):
None 0
Mild 2
Moderate 4
Severe 10
Movement and deformity (20%)
Pain on examination (overall results are both active and passive range of motion):
None 0
Mild 2
Moderate 5
Severe 10
Other abnormal findings (limited to orthopaedic problems eg reduced range of motion, deformity, limp, instability, progressive x ray findings):
None 0
Mild 2
Moderate 5
Severe 10
Other factors (20%)
Multiple joint disease:
No, single joint 0
Yes, each affected joint mild: moderate in severity 4
Yes, severe involvement (eg severe rheumatoid arthritis) 10
Ability to work, give care to dependants, live independently (difficulty must be related to affected joint):
Not threatened or difficult 0
Not threatened but more difficult 4
Threatened but not immediately 6
Immediately threatened 10
Total score (> 70 = priority for joint replacement)
The New Zealand priority criteria scoring system for hip and knee replacement is used by many PCTs to triage those patients who may require joint replacement.
A score > 70 makes the patient a priority for joint replacement
BMJ 1997;314:131 (11 January) The New Zealand priority criteria project.
Bow legs and knock knees
Occurs due to changes in the tibiofemoral angle during growth.
Often, a varus or valgus position isaccentuated by internal or external rotation of the tibiae, respectively.
This rotation is due to the uneven growth of the tibia and fibula, and disappears spontaneously during normal development.
A varus position during a child’s first 2 years is normal (distance between the knees of 10 cm or less),
At 7 years of age, the intermalleolar distance is normally less than 2.5 cm, with a maximum of 8 cm. A larger distance indicates a valgus position, which may require treatment.
Abnormal knee positions can be caused by physiological variation, rickets and Blount disease.
Less likely causes are endocrine and metabolic bone disorders, epiphyseal dysplasia, treponematosis, post-traumatic, post-radiation or post-infection abnormalities, local congenital defects, tumours and abnormalities resulting from paralysis.
Calf strain / tennis leg
Caused by a (partial) rupture of the gastrocnemius muscle.
Characterized by a sudden, severe pain in the calf accompanied by difficulty in walking, usually occurring during sports or when walking, but also sometimes when standing still.
The gastrocnemius muscle is particularly vulnerable to injury because it covers two joints. When active plantar flexion of the foot and passive stretching by extension of the knee occur at the same time, the muscle is stretched to its maximum, and so may rupture eg when serving on the tennis court or in volleyball
PRESENTATION
The patient presents with a typical story. For example, while serving on the tennis court, the patient thought he was hit hard in the calf by a ball from another court, or, while running, by a stone. He may have even heard a ‘snap’. Immediately after, he is unable to walk because of the searing pain in his calf. Some patients even collapse from the
pain. Several hours or days after the injury, the patient attends with a typical clinical picture: he walks on the toes of one foot or limps, the foot on the injured side is in a twisted position, and it is impossible to put the foot on the ground in the normal position, as this aggravates the pain.
EXAMINATION
Calf muscles will usually be slightly swollen.
The injury sometimes gives the impression of an indentation, almost always just above the transition from the Achilles tendon to the medial muscle belly of the gastrocnemius muscle. (cf lower/distal indentation in achiles tendon rupture)
This site is very tender on palpation.
Plantar flexion of the ankle is possible, especially passively, but passive dorsiflexion is very painful. Plantar
flexion against resistance is nearly impossible because of the pain.
A haematoma is often visible one or several days after the injury occurs (distal from the injury).
Exclude complete Achilles tendon rupture:
Thompson’s test: the GP firmly squeezes the lateral and medial calf muscle groups while the patient is lying on his stomach or kneeling on a chair. If there is a total rupture of the Achilles tendon, no plantar flexion of the foot will occur.
Hoffmams/Homas Test
Doppler assessment if deep vein thrombosis is suspected.
TREATMENT
Ice and rest to limit bleeding and tissue damage
NSAIDS
In the absence of complications, the patient can begin walking and light stretching exercises after a week. Once the normal walking pattern has been restored, the patient may carefully start sport and stretching exercises. Complete recovery will occur after an averageof 4-6 weeks.
Differential Diagnosis
Ruptured Achilles Tendon
Compartment syndrome
2 different entities – acute post trauma/surgery and chronic exhertional
Achilles tendon
Ruptured achilles
- youtu.be/HC7jf4W0
- youtu.be/MLT5-Wnu594
- youtu.be/lfQ_E6mDDU8
- youtu.be/AmDi08rlR3I
- youtu.be/wQbEJrcmGpQ
- youtu.be/7YK_qLk1alw
Ankle ligament anatomy
Tom Dick and Harry
Tibialis Posterior
Flexor Digitorum Profundus
Posterior Tibial Artery
Flexor hallucis Longus
@@@ Ankle and foot examination
hacking-medschool/ankle-foot-examination
Ankle & Foot including Tendon and Calf
Ankle injuries particularly sprains of the lateral ligament complex are common. It is important to detect and refer bony injuries but also to give appropriate advice re rehabilitation (proproceptive exercise, physio) and arrange follow up for sprains as these can be associated with prolonged recovery, reinjury , and development of chronic instability
Red flags
Compartment syndrome – severe unremitting pain lower leg following trauma.
Complete lateral ligament rupture
Inferior Syndesmosis disruption
Achilles tendon rupture (Sudden sharp pain in achilles palpable defect – Simmonds negative – active plantar flexion does not exclude achilles rupture)
Tibia fractures of children hard to diagnose – suspect if non weight bearing after minor twisting injury.
Examination
LOOK/INSPECT
With the patient walking (if possible)
Inspect the patient’s gait as they walk to the other side of the room, turn, and come back. Observe first with the patient wearing footwear, then barefoot (as shoes may hide some abnormalities).
Inspect the ankles and feet close up for fine details, such as scars, callosities or ulcers.
Inspect the longitudinal and transverse foot arches ; pes cavus (high arched foot) or pes plantus (flat foot)
Inspect and compare ankle, heel, dorsal, and plantar aspects of foot toes observe for injury swelling redness and deformity
Inspect the toes for ingrowing toenails. atrophic toenails, mallet toe, hammer toe (usually 2nd toe). bunion (1st metatarso-phalangeal [MTP] joint). bunionette (5th MTP joint) or clawing.
FEEL/PALPATE
Ask patient to indicate site of maximum pain and inform of any pain/tenderness during assessment
The patient should remain on the bed. Feel for:
• temperature – feel over the main joints with the dorsum of your hand
paraesthesia
• bony prominences/asymmetry – anterior and posterior aspects of lateral and medial malleoli, MTP joints, interphalangeal (IP) joints and heel;
Identify and palpate cuboid and navicular bones
Squeeze across metatarsal joints and note any pain. Palpate individual metatarsals and toes.
• Achilles’ tendon – feel for a palpable gap in the tendon indicating a rupture
• spurs – press deep into the sole of the foot to feel for spurs.
Measure
If necessary measure the ‘calf girth’ on both sides, in order to obtain an objective measure of any muscle wasting or hypertrophy.
Active movements
Movements take place at the ankle joint, subtarsal joint, mid-tarsal joint, MTP and IP joints. Movements should be performed while the patient is sitting on the edge of the bed, with the legs hanging over the edge (knees flexed and lower leg relaxed).
Dorsiflexion Ask the patient to point the toes towards their head.
Plantar flexion Ask the patient to point the toes towards the floor.
Inversion Fix the calcaneum with your hand, and ask the patient to tum the sole in towards the midline.
Eversion Fix the calcaneum with your hand, and ask the patient to tum the sole away from the midline.
Toe flexion Ask the patient to curl their toes.
Toe extension Ask the patient to straighten their toes.
Toe abduction Ask the patient to fan the toes.
Toe adduction Ask the patient to try to hold a piece of paper between the toes.
Passive movements
Repeat as above with you the examiner performing the movements – dorsiflex plantarflex inversion eversion
rather than asking the patient to perform them. Be cul not to cause pain.
Resisted Movement test strength through resisted movement
Special tests (if indicated)
Simmond’s (squeeze) test (to test for rupture of the Achilles’ tendon)
Ask the patient to kneel on a chair with their feet hanging over the edge, holding the back of the chair for steadiness. Squeeze the gastrocnemius muscle gently. Normally, the foot will plantar-flex. If the Achilles tendon is ruptured, no plantar flexion will occur.
Assess knee and hip as necessary
Normal findings/ROM/Dermatomes
Dorsiflex 0-20 degrees
Plantar flex 0-50 degrees
Inversion 0-30 degrees
Eversion 0-20 degrees
First MTP
flexion 0-20
extension 0-80 degrees
Common abnormalities
Ankle Sprain
Achilles Tendinitis (tendinosis)
Ruptured Achilles Tendon
Ankle fractures
Fractured base 5th metatarsals
March Fracture
IGTN
Subungal Haematoma
Mortons Neuroma
Hallux Valgus
Hallux Rigidus
Gout
OA
Plantar fasciitis
Severs
Investigations
Xray may be indicated (ottawa rules) in acute injury if : age> 45, unable to weight bear (ie take 5 steps), posterior malleolus tenderness, tendernessover base 5th metatarsal, tenderness over navicular.
Xray/MRI/Standard blood tests via GP or Secondary Care according as clinically indicated.
- youtu.be/7IbutxdhB7U
- youtu.be/tLxgqG5uBVM
- youtu.be/AegHwX8Y3AM
- youtu.be/97KSvgipIW0
- youtu.be/uxjKEHXKwr0
- youtu.be/NyR1zs6Yg78
- youtu.be/0R4zRSE_-40
- youtu.be/YIwAMtdYcg8
- youtu.be/kdGSGofCa9I
Ankle injuries and sprains
- FastRehab
- HEM Rehab
- youtu.be/I8Z0obhpew
- youtu.be/c60mihBxCM8
- youtu.be/X6qCBPBoTnU
- youtu.be/dzaS0UG8jMA
- youtu.be/KjJi_FCRhl0
Ankle and foot injuries and conditions
Foot and ankle injuries are extremely common and may include sprains, strains, fractures, blisters, infections and foreign bodies . Assessment should include a detailed history of mechanism of injury and thorough examination. It is part of the musculoskeletal system which consists of bones, muscles, tendons, and ligaments. The foot is composed of many small bones making fractures common. Foot injuries are common and can include Some foot injuries can interfere with activities of daily living.
Soft tissue injuries
Soft-tissue injuries consist of sprains, strains, dislocations and subluxation. The common causes of a sprained or strained foot are running, missing a step, stepping onto uneven ground or sports injury. A sprain is an injury to the ligaments surrounding a joint causing stretching of a muscle and its fascial sheath.
Sprains are typically accompanied by bleeding beneath the skin and the formation of ecchymosis and swelling. Sprains can be further classified according to the amount of ligament fibers torn. A first degree sprain involves a few ligaments, with mild tenderness and swelling. A second degree sprains involves the tearing of more ligaments with partial disruption of involved tissue, and increased swelling and tenderness is present. A third degree sprain is the complete tearing of the ligament and typically very painful. Sprains and strains are more painful with motion and sprains may also be painful at rest due to the swelling.
Ankle Ligament Injury very common and due to a twisting and inversion of the foot causing a partial tear to fibres of the lateral ligament. Occassionally there is a complete tear causing joint subluxation. Treatment involves 24hrs RICE then early mobilization. Complete tears may be treated in a POP or by surgery. Long term problems include instability, joint adhesions recurrent strains.
Dislocation is a injury to the ligaments that surround the joint which results in separation of the aritcular surface of the joint, subluxation is a partial displacement of the joint and less severe. Dislocations are not common in the feet but may occur with a stubbed toe.
Ankle Fractures
The distal tibia and two malleoli make up a mortice in which the talus bone fits snuggly. If the talus is twisted withenough force then one or both malleoli can be fractured – -one is pushed off by the talus fracturing in an oblique pattern whilst the other is broken transversely by the pulling off of the collateral ligaments.
High ankle fractures may also cause tearing of the tibiofibular syndesmosis ligament causing widening (diastasis) of the joint and instability.
Overuse Injury
Stress fractures of the 2nd or 3rd metatarsals occur after excessive unaccustomed exercise (Soldiers March Fracture) or as overuse injury in commonly seen in runners or athletes. Initial Xray may be negative but a prepeat Xray after 2-3 weeks may show callus formation around the area of the stress fracture. Treatment is usually conservative though a plaster cast may be used for pain relief for 2-3 weeeks.
Plantar fasciitis is due to chronic strain of the plantar feascia where it attatches to the inner under surface of the heel and presents with heel pain.
Foreign bodies
When individuals walk without protection to the feet they are at greater risk of stepping on sharp objects such as glass, wood, or nails. These injuries vary depending on the cause and depth of penetration. Risk of nerve or tendon damage is possible as well as infection.
Diabetics and elderly are at greater risk for developing complications associated with foreign bodies in the foot due to poor circulation and decreased sensation in lower extremities caused by underlying medical conditions and pathophisoloigcal changes in the eldery. Clinicians should encourage diabetics to inspect their feet daily for injury or sores and seek treatment immediately for impaired skin integrity to assist in the prevention of complications. When left untreated, foreign bodies can cause infection that potentially lead to osteomyelitis, which requires surgical treatment.
Blisters are common when improperly fitting shoes are worn. Many injuries to the feet can be prevented just through proper foot wear.
Investigations
X-ray as needed for bony tenderness according to Ottowa Rules.
Orthopedic/podiatry/physiotherapy referral
Stiffness is a major problem in all ankle injuries ao advice re mobilization, rehabilitation +/- physiotherapy to restore stability and proprioception. Apply ice using a barrier to protect skin for the first 24-48 hours
Rest and immobilize the injured area
Elevate the injured area for 48-72 hours
Instruct on signs of poor circulation and to call if pain worsens
Ankle fractures
Ottowa ankle rules
X-Ray particularly where there is tenderness over malleoli, or where the patient is over 55 yrs.
(a) Mild Strains & Sprains require only support bandaging or strapping for 10 days.
Encourage stretching exercises and normal gait. Review not normally necessary.
Advise: Rest Icepacks Compression & Elevation
(b) Moderate sprains: Consider discussion with Physiotherapist re: Haematoma dispersal, proprioceptive re-education etc. Strapping + crutches. Review may be necessary after 10-14 days
(c) Partial Ligamentous Rupture: SL POP with heel + Crutches; Refer to Fracture Clinic.
(d) Complete Ligamentous Rupture: Discuss with Orthopaedic SHO re: admission for repair.
(e) Fracture: If undisplaced malleolar # SL-POP Non-weight bearing, Refer # clinic 2 Wks. Malleolar tip fractures may weight bear when the POP is set. If you wish the patient to have a walking heel applied to their POP on their Day 1 POP check, please record this in the notes.
(f) Displaced Fractures: These require reduction and should be admitted for this and for elevation.
Foot anatomy
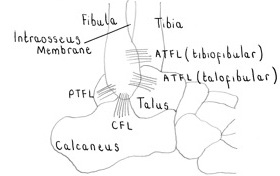
Foot conditions
Heel pain
Achilles tendonitis pain and diffuse swelling of the tendon worse on dorsi/plantar flexion
Achilles bursitis localised tender swelling at the bottom of the TA often due to ill-fitting shoes.
Retrocalcaneal bursitis tenderness anterior to TA more directly on the bone.
Haglund’s Retrocalcaneal exostosis
Pump Bumps exostosis on the back of the heel
Plantar Fasciitisworse in the morning, usually unilateral but if bilateral consider RhA, gout or SLE.
Plantar fasciitis
Crawford E Plantar heel pain (including plantar fasciitis). Clin Evid 2002;7: 1091-100.
Dailey JM. Differential diagnosis and treatment of heel pain. Clin Podiatr Med Surg 1991 ;8: 153-66.
Painful 1st MTP and gout
Sudden onset of painful 1st MTPJ without any trauma. Most likely to be gout but can be OA.
Serum urate may be normal in an acute attack, so it needs to be repeated about 1 month afterwards to confirm gout. Swollen joints can be aspirated for crystals during the acute phase to confirm a diagnosis if the serum urate is normal.
Rx There are three stages in the management of gout
1. Treating the acute attack: NSAIDs are the preferred treatment in acute gout. The most important determinant of therapeutic success is not which NSAID is chosen, but rather how soon NSAID therapy is initiated. You can also use colchicine or oral prednisolone. Acute painful joint can be injected with steroid.
2. Lowering excess stores of uric acid to prevent flares of gouty arthritis to prevent crystal deposition uricosuric agents like probenacid
3. Prophylaxis – allopurinol (needs ‘covering’ for 1 – 3 months to prevent flare up) or low dose colchicine.
Common pitfalls:
1. Blood uric acid level may be normal in acute attacks.
2. Don’t stop allopurinol on gouty patients during their acute attacks.
3. Remember there are alternatives to nsaids such as oral prednisolone (35mg a day for 5 days) or colchicine for acute attacks.
4. Don’t start allopurinol around the time on an acute attack, as it can increase crystal deposition and make pain worse.
5. Start allopurinol 100mg od and uptitrate slowly with nsaids or colchicine cover until the serum urate is in the lower half of the normal range.
6. Allopurinol usually needs to be continued lifelong.
7. People with very high uric acid are likely to suffer from gouty arthritis more often.
Forefoot pain metatarsalgia
Causes
Stress #
Morton’s neuroma
flat feet
synovitis of the MTPs
Flat feet
– usually accompanied by valgus deformity of the foot and pronation at the subtalar-midtarsal complex. They usually need biomechanical assessment before Rx, hence appropriate referral to the chiropodist is necessary.
Synovitis
may present with similar s/s of morton’s metatarsalgia. Tenderness is present on both dorsal and plantar aspect of the MTPJs. Rx steroid injection and chiropodist referral for shoe adjustment.
Metatarsalgia
Mortons neuroma
Usually women, c/o sharp pain in the forefoot radiating to the toes. Tender interdigital space. Diagnosis is usually confirmed by USS. Rx usually needs excision but pain can be relieved by steroid inj.
Metatarsal fractures
Stress #
usually of the 2nd or 3rd MT mainly in young people or osteoporotic patients. No direct injury. Very tender base of the MT. X-ray confirms the diagnosis but may be normal. A bone scan may be necessary if the X-ray is normal. If you suspect it, refer to orthopaedics.
For a single # use strapping and a metatarsal pad. For multiple fractures use POP. Avulsion fractures of the 5th Metatarsal base may require POP slab, depending on extent of discomfort. Refer MT fractures to # clinic. Fractured
Digital nerve block
This procedure can be used to provide anesthesia for nail removal, burns, incision and drainage, fractures, dislocations and laceration repairs to the fingers and toes.
DO NOT use epinephrine/adrenaline containing anesthetics in digital nerve blocks or at other vulnerable sites
Remove rings from affected digits
Caution in fingers with significant swelling – additional swelling from injected anesthetic may contribute to decreased blood flow
Digital blockade of fingers or toes is achieved by fully anaesthetizing each of four nerves which surround the digit – a ventral nerve and a dorsal nerve each side each.
Caution in fingers with significant swelling – where even more swelling produced from injected anesthetic may contribute to decreased blood flow.
Caution also in the toes where the smaller subcutaneous tissue space that may make anaesthetic infiltration difficult.
Equipment/Supplies: alcohol or betadine prep pad; exam gloves; 5mL syringe filled with 1% or 2% lidocaine with or without 0.5% bupivicaine; 3.75cm (1.5in) 25 or 27g needle.
1. Aseptic preparation – have the patient place their palm down on the exam table and prepare the dorsal surface of the finger by cleaning the area from the knuckle to just beyond the web space.
2. Two injections are necessary for the dorsal approach. Begin on one side by piercing the skin ajacent to the bone in the web space. Create a wheal in the subcutaneous tissue (essentially when the needle contacts bone) with 0.5-1mL of anesthetic.
3. Then advance the needle until it begins to tent the skin on the palmar side of the finger. Withdraw the needle 1mm then aspirate to ensure it is not in a vein or artery. Inject 0.5-1.5mL of anesthesia slowly and then withdraw the needle. If resistance to infiltration is significant, slowly reposition the needle, aspirate, and attempt again.
4. Repeat same procedure on the opposite side of the digit
5. Massage area for 15-30 seconds to promote infiltration of anesthetic
Educate patient that anesthesia may last 4-8 hours. Patient should return for increased pain, if the digit becomes/remains pale or if swelling worsens.
Hammer toes
Hammer proximal flexion deformity then mallet distal deformity in alphabetical order
Hallux valgus
Slowly progressive lateral deviation of great toe at MTP joint with associated medial deviation of 1st metatarsal (in fact other way round with strict anatomical nomenclature wrt foot?). Affects mainly middle aged and elderly femalse due to tight pointy shoes but often hereditary. Leads to bursa formation over protruding head of 1st metatarsal head (the bunion) +/- MTP joint OA.
Corns and calluses
Flat Feet
Lower Limb Biomechanics
- youtu.be/h_tlBZe25oU
- youtu.be/6inEpxTxWnM
- youtu.be/YIwAMtdYcg8
- youtu.be/pODcT55_7zA
- youtu.be/0R4zRSE_-40
Physiotherapy techniques videos (Pulse)
Pulse – Pulse – Clinical skills videos – Physiotherapy techniques
