9
This and the closely-related Management section contains a number of topics that cropped up on teaching/management courses.
It feels a bit fragmented but hopefully includes useful background to concepts and models one’s likely to encounter on similar courses or as part of “the syllabus”.
As ever the intention is to continuously improve the content and make 250 Textbooks even more coherent.
Teaching/Learning/Communication/Management/Therapy are all aspects of human interaction
Doceo Reflective Journal James Atherton
The state of medical education and practice GMC Oct 2011
Association for the study of medical education
Association for Medical Education in Europe
Centre for Medical Education Dundee
Roles and responsibilities of a teacher
Teacher Duties and Responsibilities ware.k12.ga.us
Roles, Responsibilities and Boundaries for Tutor thetutorpages.com
Attributes of a good teacher
What makes a good teacher? Highland learning and teaching
Being a better teacher Mahibur Rahman gpvts.info
Seven principles to guide teaching practice
Educational theories
Doceo Reflective Journal James Atherton
Possession of knowledge is no guarantee of the ability to pass it on.
There is a body of evidence, theories and guiding principles to ease the process.
Some of the more modern aspects may be deemed too prescriptive by experienced jobbing practitioners but awareness and training in these are prerequisites for the modern medical teacher – and they may well help in difficult or unaccustomed situations.
With respect to Medical Education / GP Education / Revalidation it might sometimes appear that the Authorities
– take ideas or contemporary mores willy-nilly, by-passing the critical discussions and evidence base of Real World practitioners and experts and sell on an inferior or incomplete version as something new and profound
-imbue them with more weight than the said Real World Teachers afford them
-pay more attention to bureaucratic and political aspects than genuine learning considerations
-lack behind contemporary thinking and developments – edupunk , eportfolios, WEb 2.0 learning etc
…by which we mean (and this is a recurring 250 Textbooks theme) the differences are minimal compared to the similarities – there is nothing particularly unique in fact about Adult Learning versus how kids learn, medical education versus other education, disease diagnosis, treatment or communication in say primary care versus secondary care etc. Politics, Ice Cream Wars and Empire Building may get in the way but the eternal truths still prevail
Adult learners
Pedagogical tutor centred/directed dispensing of learning/knowledge to passive learners
Andragogical the learner should be encouraged to learn from themselves in the way that suits them
RCGP/Appraisal approach may be viewed by some skeptics/reluctant learners as appearing to espouse androgeney whilst revealing a degree of pedagogy – we are here to encourage you to learn for yourselves but this is the way you should do it!
5 assumptions about Adult Learners
1 Adults are independent and self directing
2 They have accumulated a great deal of experience, which is a rich resource for learning
3 They value learning that integrates with the demands of their everyday life
4 They are more interested in immediate, problem centred approaches than in subject centred ones
5 They are more motivated to learn by internal drives than by external ones
Seven Principles of Adult learning
1 Establish an effective learning climate, where learners feel safe and comfortable expressing themselves
2 Involve learners in mutual planning of relevant methods and curricular content
3 Encourage learners to formulate their own learning objectives—this gives them more control of their learning
4 Encourage learners to identify resources and devise strategies for using the resources to achieve their objectives
5 Support learners in carrying out their learning plans
6 Involve learners in evaluating their own learning—this can develop their skills of critical reflection.
Didactic vs dialectic teaching
Both methods of promote thinking about ideas by asking questions
Didactic Teaching
Contemporary usage of the term didactic suggests authoritative, interaction-poor delivery of information to passive students eg in lecture setting
Classically this method involves mutual contemplation of a topic by teacher and student together examining both individual aspects then common themes to gain deeper understanding
Dialectic/Socratic Method
relentless pursuit of truth through unceasing questions
Ironic Stage
use questions to probe your student’s understanding–to find the inadequacies in his thoughts eg contradictions, insufficient definitions of terms, faulty logic hasty generalizations and reversal of cause and effect
Purpose: weaken student’s confidence in an inadequate understanding of reality
Maieutic stage
Continue with questions but with more suggestions to give birth to a more accurate understanding of reality
Metacognition
Modern applied educational theory not so far removed from certain contemporary mores but without the administration and beurocracy.
Identify and define your learning needs and objectives – so that of course your learning will be more focussed and productive – then just get on with it without diverting too much of your brain resources on the process.
What the heck is metacognition
Laird’s sensory theory 1985
Theories of learning Oxford Brookes
Learning is better the more senses are stimulated.
Lewin unfreeze change refreeze
Ideas and behaviours can become habituated entrenched and hardwired over time. Change is often resisted.
Lewin’s Change Management Model mindtools.com
This Experiential model was developed by Kolb into the learning cycle
http://www.youtube.com/watch?v=uHR8gw6derg
Kolb’s 4 phase learning cycle
Kolb Learning Styles simply psychology.org
1 Concrete Experience learning by doing
2 Observation & Reflection stepping back and thinking about what you’ve done
3 Abstract Conceptualising interpreting what’s happened and considering how to do differently
4 Active Experimentation redoing/refining in light of previous experiences & personal reflection
rinse & repeat as required
Why this matters —the theory suggests that without reflection people would continue to repeat their mistakes
Honey and Mumford learning styles 1986
Activist prefers doing and experiencing
Achiever keen embracers of stimulation & challenges and keeping busy
Pragmatist realist apply their learning logically to practical situations likes to ‘have a go’; try things out to see if they work
Theorist contemplator thinkers who research and contemplate options before acting wants to understand underlying reasons, concepts,relationships
Reflector observes and reflects
Logician even deeper thinkers who prefer tried and tested options
Why this matters
Again the teacher needs to to adopt their teaching style to the mix of their learners and also be wary of bringing imposing too much of their own learning style
Honey and Mumford built on Kolb’s work by connecting a learning style to each stage of the learning cycle
Depending on the preferred learning style, the learner will enter into the learning cycle at any of the four points.
Learning Styles learningandteaching.info
Honey Pond Mumford A (1986) The Learning Styles Questionnaire.
Kolb (1984) Experiential Learning: Experience as a Source of Learning and Development.
Rogers humanist facilitative learning
People are naturally keen to learn.
The teacher must be learner focussed, discover what the students want to learn and facilitate this.
Skinners behaviorist theory
Behaviorist theory of learning (Skinner) sil.org
Behaviour is a consequence of consequences.
Prompt feedback positive or negative will allow the learner to reinforce or adapt their behaviour.
Kolb and Fry’s learning styles inventory
Kolb’s Theory of Experiential Learning scss.tcd.ie
Converger
Abstract conceptualization + active experimentation
Strong in practical application of ideas
can focus on hypo-deductive reasoning on specific problems
unemotional narrow interests
NERD
Diverger
Concrete experience + reflective observation
strong in imaginative ability
good at generating ideas and seeing things from different perspectives
good at generating ideas and
interested in people
broad cultural interests
Russel Brand
Assimilator
Abstract conceptualization + reflective observation
strong ability to create theoretical models
excels in inductive reasoning
prefers abstract concepts to people
Columbo
Accommodator
Concrete experience + active experimentation
doer, risk taker, thinks well on feet
solves problems intuitively
Crocodile Dundee
Learning Styles Myers Biggs
Sensory learning styles VAK
hacking-medschool/gardner-multiple-intelligence
VAK
Visual
Aural
Kinaesthetic
Why this matters
you should tailor your teaching to the learning styles of your learners
Individual learners may be a variable mix of all three styles and you may be teaching a group therefore mix/match and cover all bases
I hear I forget I see I remember I do I understand
Fleming 1987 Hand M
http://youtu.be/cX0teReijUk
Gagnés categories of learning 1965
Gagné Conditions of Learning psu.edu
Gagnés 5 categories of learning
Verbal Information
Intellectual Skills
Cognitive Strategies
Motor Skills
Attitudes
Why this matters
Each requires a different teaching/learning approach eg the opportunity to practice for motor skills versus discussion and reflection for attitudes
Gagne also describes 9 instructional stages together with the corresponding (meta)cognitive processes
1 gaining attention reception
2 informing learners of objectives expectancy
3 stimulating recall of prior learning retrieval
4 presenting the stimulus selective perception
5 providing learning guidance semantic encoding
6 eliciting performance responding
7 providing feedback reinforcing
8 assessing performance retrieval
9 enhancing retention & transfer generalisation
The Learning Cycle
Identifying needs & planning
Designing
Facilitating
Assessing
Evaluating
Heron’s six category intervention analysis
Six types of intervention a doctor, teacher, counsellor or therapist could use with a patient client or student
1 Authoritative Prescriptive
2 Informative
3 Confronting
4 Cathartic
5 Catalytic / Facilitative
6 Supportive
J Heron: Six Category Intervention Analysis scaling the heights.com
Heron’s Categories mindtools.com
Learning styles – multiple intelligences test
Personality tests @ Business Balls.com
Herman’s whole brain model
Howard Gardner’s multiple intelligence model
VAK learning styles test Business Balls
hacking-medschool/sensory-learning-styles-vak
Why this matters – People are happiest and most successful when they learn develop and work in ways that best use their natural intelligences (strengths/style/brain type)
Maslow’s hierarchy of needs (teaching)
Motivation – Maslow’s Hierarchy of Needs (1954)
hacking-medschool/maslow-management
Intrinsic motivation the learner just wants to learn
Extrinsic motivation the learner is driven by outside forces eg promotion
In any case the teacher should incorporate appreciation of the learners values drivers needs and motivations into their teaching
Intrinsic motivators for learning Malone and Lepper
Intrinsic Motivations for Learning Malone and Lepper Sarah Calandro.com
A taxonomy of motivation and game design instructionaldesignfusions.wordpress.com
Maintaining Student Engagement when Designing Online Activities 4cast.uiowa.edu
Curiosity
Indipendance
Imagination
Social Comparison
Interdependance
Esteem
Skills acquisition and development
unconscious incompetence not knowing that you don’t know how to do something competently
conscious incompetence aware of a gap in one’s competence
conscious competence able to perform a task with concerted effort an awareness eg following the instructions
through repeated practice one becomes
unconsciously competent tasks or skills can be performed effortlessly without thinking
Why this matters
learners/employees (ho hum) may be stuck at one of these levels unless they or their teachers/managers recognise and do something to remedy it (including in themselves)
Preparing to Teach in the Lifelong Learning Sector Ann Gravells
Four stage technique for practical skill teaching
Instructor Demonstrates at normal (realtime) speed
Instructor demonstrates slowly with commentary not just how but why including anatomy and physiology
Instructor demonstrates Trainees commentates
Trainee(s) demonstrates with commentary
Novice to expert Dreyfus
http://www.doceo.co.uk/background/expertise.htm
1 Novice
2 Advanced Beginner
3 Competent
4 Proficient
5 Expert
Becoming an expert 10 000 hrs
10 000 Hours
How To Become An Expert hunternuttall.com
Become an expert in only 10,000 hours daveswhiteboard.com
not just perserverance you need “talent” or a “bent” to begin with – i could spend 10 000 hrs playing darts or golf but wouldn’t be much better at the end. A business mind might succeed through ingenuity, guile, perseverence and good fortune, but hard work alone won’t cut it
the Peter Principle
Peter Principle for Skill Development – Stages of Competence – 1969
the Peter Principle – how stuff works
in evolution systems tend to develop up to the limit of their adaptive competence
The Peter Principle – Bureaucracy at Work envisionsoftware.com
Setting objectives and competencies
I’m not sure i agree with this stuff wholeheartedly
Knowledge and understanding must surely have future value beyond an immediate need for action or measurement, and quiet patient scholarship distributed learning might have even greater value
Whatever, these are the guidelines or should I say KEY LEARNING POINTS
Objectives should be behavioural ie what the learner/audience can do (not know or understand?)
– to what standard % precision quality safety time completeness
– under what conditions in the correct order within the timelimit
ie precise clear and easily measurable
Behavioural Verbs
write
draw
state
explain
demonstrate
identify
define
complete
select
solve
calculate
operate
Self directed learning vs core competencies
Self Directed Learning
http://www.selfdirectedlearning.com
Core Competencies
something from Helen Barrett
Bloom
http://www.youtube.com/watch?v=ZlESOh_MNdY&feature=related
Set dialogue closure
Set Dialogue Closure Scheme (ALSG)
Neat simple framework for any teaching situation – lecture, small group, 1-1 whatever – Keep It Simple Stupid
Set – environment atmosphere motivation objectives roles
Attention Interest Direction
welcome student(s) Introduce Yourself Claim Credibility
establish motivation
title and learning outcomes (slide)
student Involvement questions activities
Layout Equipment Temperature & lighting
Objectives housekeeping rules prompt start introduction credentials agenda expectations questions
Putting down markers makes you appear professional
Dialogue
main interaction between teacher & learners covering the essential subject matter including checking understanding
The main content and substance
Ensure a degree of vocal variety Voice Emphasis Pace Enthusiasm
Avoid verbal and postural tics
Interact with the audience
Effective use of questions
Closure
questions summary termination
Invite further questions
Repeat Questions for rest of audience and allow thinking time
Admit ignorance but promise to get back on difficult areas
Summarise what was covered
Review objectives and explain who they’ve been achieved
Take home messages 1-2 or max three
Presentation and platform skills checklist
source
Preparation
handouts presentation materials audiovisual aids
Location / Venue
environment equipment audience size and makeup
Practice
Equipment & Materials
materials handouts
prepare your bag
laptop memory stick email yourself take your own laptop
internet dongle
check arrangements
Set Up
equipment (test it)
room layout
flipcharts pens whiteboard duster
First and lasting Impressions
personal appearance
water
opening statement
meet & greet
breathe
check personal appearance
have a glass of water
silently practice your opening statement
meet & greet
appear confident and relaxed
breathe deeply
Intro
housekeeping agenda timetable
start promptly you are efficient
introduce yourself & you credentials/provenance
explain outcomes what the audience are going to get
run through the agenda
what is expected questions during or after
SMART aims & Objectives
Facilities
Tour of site
Health & safety
Hygeine factors
Course Qualifications Details & Dates
Expectations & Ground Rules
Break times
Assessment Details
Ground Rules
Icebreakers
Delivery
Posture
Stance
Hands
Eye Contact -lighthousing
Voice Projection – dance tone words
Presentation videos
Lesson plans PARR
Present Objectives & Tasks
Apply Learning Strategies
Reflect
Review
source?
Presentations – law of 3s
The Lost Art Of Oratory bbc.co.uk
Lectures / presentations
Unfairly maligned as an educational vehicle – the medium is alleged to be some kind of one way exposition of didactic facts directed towards passive recipients.
I’ve personally been greatly inspired by lectures/talks by great real life speakers and educationalists and televisual examples going back to the Royal Society Christmas Lectures as a child to now TED talks and infinite stuff courtesy of youtube et al – I can now be educated and inspired by “lectures” from Einstein, Feynman, Gell- Murray, Robert Anton Wilson etc. Go figure!
Textbooks are supposed to be bad/passive also – nevermind the generations of Nobel Prize Winners inspired by the Observer books of Birds or Astronomy, jumble sale copies of the Encyclopaedia Brittanica or the BBC’s World Service. What exactly Active Learning is I’m not sure – like many of my generation I was inspired to build my own microscope and make tin can telephones via Look and Learn Magazine but physics practicals went over my head. I had to fill in a “Homework Notebook” but thankfully didn’t have to include any reflections or do an audit to demonstrate learning.
(The more I write this the more my uninformed self wonders just how far a certain Educational Hegemony of new-thought and power is crushing the opportunity for genuine thought in the young. The intelligent digital natives will escape some but not all of this damage – some but by no means all will presumably (hopefully) still be able to satisfy subvert and circumvent the requirements of Schooling but it still adds up to a great waste of time for the academically keen and gifted and a continued failure for the rest – same as it ever was)
Said to be Good for
disseminating information
reducing ambiguity
stimulating learner interest
introducing learners to content/tasks before other instructional methods
Drawbacks
not good for teaching skills
limited attention span of audience 20-40 mins?
Structure
Set
Dialogue
Closure
3 is the magic number
Break down into sections each geared to achieving one of the initial objectives
tell a story – organise and reveal facts in an ordered manner to reveal that story justifying why along the way
Slides Powerpoint rule of sevens
videos interesting but advise audience in advance what to look out for
Things not to do
Annoy
Bore
Confuse
Distract
Exhaust
Assessment
Avoid powerpoint completely
Visual Meetings : How Graphics, Sticky notes & Idea Mapping Can Transform Group Productivity
Making a successful presentation Dr Mahibur Rahman gpvts.info
source Franklin Covey Presentation Course
Aims objectives SMART
Aims Versus Objectives (groan)
SPECIFIC
Objectives should specify what they need to achieve – percieved wisdom suggests a specific objective is more likely to be achieved.
To set a specific objective you need to answer the SIX “w” Questions
Who: Who is involved?
What: What do i wish to accomplish?
Where: identify a location
When: establish a timeframe
Which: identify requirements and constraints
Why: specific reasons purpose or benefits of accomplishing the goal
Specific means that the objective is concrete, detailed, focused and well-defined.
The objective must be straight forward and emphasize action and the required outcome.
Specific also means that it is results and action-orientated.
Objectives need to be straight-forward and to communicate what you would like to see happen.
To help set specific objectives It helps to ask:
What am going to do? This are best written using strong action verbs such as conduct, develop, build, plan, execute, etc.
This helps your objective to be action-orientated and focuses on priorities
Why is this important for me to do?
Whois going to do what?
Whoelse need to be involved?
When do I want this to be completed?
How am I going to do this?
Measureable means that the measurement technique is identified and we are able to track the actions as we progress towards the objective.
It’s important to have measures that will encourage and motivate you on the way as you see the change happening – this may require interim measures.
Objectives (unlike say, aspirations or visions) need to be achievable
If the objective is too far in the future, you may find it difficult to keep motivated
Objectives need to stretch you, but not so far that you become frustrated and lose motivation.
Measurable
You should be able to measure whether you are meeting the objectives or not
Estabablish concrete criteria for measuring progress toward the attainment of the set objectives.
When you measure your progress, you stay on track, reach your target dates, and experience the feeling of achievement.
Attainable
When you identify objectives that are most important to you, you begin to figure out ways you can make them come true.
The objective needs to be attainable by you based on the skills you have and the constraints imposed.
What do I warn: to accomplish?
Where: Identify location
When: Establish a time frame.
Which: ldentify requirements and constraints
Why: Specify results, purpose or beneflts of accomplishing the objectives
To determine your objectives measurable, ask How much? How many? How will I know when it is accomplished?
Realistic
Can you realistically achieve the objectives with the resources available?
To be realistic, It must represent an objective toward which you are both willing and able to work,
An objective can be both hard and realistic – you are the only one who can decide just how hard it should be.
Your objectives probably realistic if you truly believe that it can be accomplished.
Additional ways to know if your objective is realistic is to consider if you have accomplished anything similar in the past or ask yourself what conditions would have to established to accomplish this objective.
Objectives that are achievable, may not be realistic – realistic: does not mean easy rather that you have the resources to do it
Achievement of an objective needs resources eg skills, money, equipment, support etc
Whilst keeping objectives realistic, ensure that they stretch you.
Most objectives are achievable but, may require adlanQ’e 11″1 your pnontles to make them happen.
Time-bound
set deadlines for the achievement of the objective. Deadlines need to be both achievable and realistic.
Not setting a deadline reduces the motivation and urgency required to execute the tasks.
• Do you have the resources available to achieve this objective?
• Do I need to revisit pnontles ~ my I~e to make this happen?
• Is it possible to achieve this objective
• When will this objective be accomplished? ls there a stated deadline?
When do you want to achieve the set objectives?
Tangible
T also stands for tangible -A goal is tangible when you can experience it with one of the senses, that is, taste, touch, smell, sight or hearing.
When your goal is tangible you’ll have a better chance of making it specific and measureable and thus attainable.
Diagnostic Questions
What exactly are we going to do, with or for whom?
What strategies will be used?
Is the objective well understood?
Is It clear who is involved?
Is the objective described with action verbs?
Is It clear where this will happen?
Is it clear what needs to happen?
Is the outcome clear?
Will this objective lead to the desired results?
How will I know that the mange has occurred?
Can these measurements be obtained?
Can we get it done within the proposed time-frame?
Do I understand the limltations and constraints?
·can we do this with the resources we have?
·has anyone else done this successfully?
·is this possible?
Problem based learning PBL
Problem-based learning Study Guides.net
Problem based learning sfsu.edu
Problem based learning maricopa.edu
Problem based learning ntlf.com
Micro-teaching
What Is Microteaching? Harvard.edu
Micro-teaching bhmed-emanual.org
Micro-teaching Bhim Chandra Mondal slideshare.net
Facilitated discussions and workshops
Facilitating learning and change in groups and group sessions infed.org
EPIC Model for Facilitation
Simplified four-part model that is distilled from Brockbank & McGill (1998); Gregory (2002); and Heron (1999).
ENVIRONMENT for enquiry
PRESENCE and attention
INTERVENING thoughtfully
CHECKING progress
Role play and scenarios
Role-play for medical students learning about communication: Guidelines for maximising benefits
Role playing in education Adam Blatner
Group dynamics Tuckman 1965
Forming group comes together
Storming members vie for status leadership etc
Norming tacit process of agreeing standards of behaviour
Performing group gets on with its task
(5 Adjourning)
Group development learning and teaching
Peer observation
Teachers Observing Teachers educationworld.com
Teachers Observing Teachers learnnc.org
DOPS and COTS
Disruptions and difficult students
Disruptions in the Classroom: Dealing with a Difficult Student usask.ca
Positive Behaviour Management Sue Cowley.co.uk
Communication skills in teaching
Communication Skills For Teachers communication skills world.com
Communication Skills for Teachers Dilip Barad slideshare.net
Listening skills
Listening Skills infoplease.com
Active Listening mindtools.com
Mentoring and coaching
hacking-medschool/mentoring-clinical-supervision
Mentoring in general practice gp-training.net
Assessment – formative and summative
Formative
Used to check progress understanding and give feedback at points along the course.
Doesn’t count towards final mark.
Summative
Final tests or assignments to be passed.
Summative and formative assessment studentvoice.com
Formative and Summative Assessment education.com
Understanding Medical Education: Evidence, Theory and Practice Tim Swanwick
Methods of Assesment
Validity & Reliability
Making Assessment decisions
Giving feedback – agenda led outcome based -ALOBA
http://hacking-medschool.com/giving-feedback
http://hacking-medschool.com/giving-feedback-2
Teaching Communication Skills skillscascade.com
Foundation Programme assessment tools:
Teachers toolkit London Deanery.ac.uk
http://vimeo.com/album/1537329
http://vimeo.com/album/1537045
Giving feedback 3 approaches
Positive Sandwich
Tell them what they did well
Tell them what they could improve
Reiterate what they did well, ending on a positive note
Reflective Model
Ask student what they felt went well or were pleased about
Respond and tell them what you think went well
Ask what they would like to improve
Tell them what you think they could do differently
Narrative Approach
Start at the beginning of the experience and talk it through logically with the student
Constantly seek learners memory of the event feelings and responses
Focus on strengths as well as highlighting ways to improve
Progress Records Standardisation QA
Giving feedback (teaching)
http://hacking-medschool.com/giving-feedback-mangement
Responsive
Objective
Subjective
focus on the behaviour not the person
be specific
how to change
own i felt
direct feedback to the individual
positive good points
constructive identify change required and how to achieve it
www.rch.org.au/emplibrary/jms/ende_paper_feedback_in_clinical_medical_education.pdf
Giving feedback Pendletons rules
Pendletons Consultation Models
Receiving feedback
Performance Feedback – 7 Tips For Receiving Feedback Gracefully – Management for the rest of us.com
Johari window
Joseph Luft & Harry Ingham
Johari Window noogenesis.com
Johari window BusinessBalls.com
known to self not known to self
known to others open blind
not know to others hidden unknown
Reflection
Two definitions from Davis & Forrest How to Teach CME
1 Active persistent and careful consideration of any belief or supposed form of knowledge in the light of the grounds that support it and further conclusions to which it leads…..it includes a conscious and voluntary effort to establish belief upon a firm basis of evidence and rationality Dewey
2 A deliberate act to develop a critique of the presuppositions on which our beliefs have been built Mezirow
Reflection in action not reflection on action. So true deep reflection is a tough and rigorous process and not just about feelings.
Not perhaps for the fainthearted then, but and understanding of this may appeal to those put off by the idea of reflection as fashionable Ivory Tower Imposed touchy-feely introspection or educational fascism.
One could of course just do an occasional Audit SEA and (eventually) put learn to appear reflective in one’s CPD log.
However one might then miss the opportunity to correct rather than continue to replicate shortfallings in ones knowledge and practice.
Reflective practice Donald Schon
Gibbs reflective cycle
Gibbs – Learning by Doing: a guide to teaching and learning methods 1988
Reflective model widely used within the health professions. Said to be good for emotionally charged cases
Description / Context
Who was there?
Why were you there?
What was happening?
Feelings thoughts /self awareness
How did you feel?
How did the others around you feel?
How did you feel about the outcome of the event?
Evaluation / Judgements
What went well, what not so well.
What was good and not so good about your experience
Analysis
Break down the event and explore each part separately
Conclusion / synthesis
Explore what you could have done differently.
Action plan
What you would do differently next time – would you act differently or do the same?
SRTs (teaching)
Structured reflective templates
hacking-medschool/srts-cpd-appraisal
Teaching communication
Teaching Communication Skills edo.med.miami.edu
Calgary Cambridge (teaching)
250textbooks/calgary-cambridge
Shared Understanding
Doctor understands the patient’s ideas and views
Patient understands the medical aspects and effects of treatment options
Curriculum models
Arisotle’s categories of knowledge
theoretical
productive
practical
1 Curriculum = syllabus – canon of knowledge or syllabus to be transmitted
2 Curriculum = product or outcome – heavily dependent on the setting of behavioural objectives. The curriculum, essentially, is a set of documents for implementation
3 Curriculum = process the interaction of teachers, students and knowledge
4 Curriculum = praxis as above plus consideration collective human well-being and to the emancipation of the human spirit
1: Diagnosis of need
2: Formulation of objectives
3: Selection of content
4: Organization of content
5: Selection of learning experiences
6: Organization of learning experiences
7: Determination of how and what to evaluate
Principles of interprofessional learning London Deanery infed.org
Stenhouse curriculum model 1975
Stenhouse @ Psychologist at large blogspot
Curriculum Design – Problems @ Crumpton UCE Birmingham
Stenhouse Research Model @ GED 550
Medical education resources
Preparing to Teach in the lifelong Learning Sector Ann Gravells 3rd ed 2008
ABC of learning and teaching in medicine Applying educational theory in practice David M Kaufman
ABC of learning and teaching in medicine BMJ
How to teach continuing medical education Forrest and Davis
The changing face of medical education Cavenagh Leinster and Mile
Understanding Medical Education Tim Swanwick
Learning needs assessment Janet Grant
General Education Blogs and links
http://dangerouslyirrelevant.org/
http://whatedsaid.wordpress.com/
Doceo Reflective Journal James Atherton
Teaching videos
http://www.youtube.com/watch?v=vpxTNV2iXv8&feature=related
Interprofesional / intraprofessional Learning
Principles of interprofessional learning londondeanery.ac.uk
Undergraduate FY1 ST Training
Undergraduate Medical Curriculum bgs.org.uk
Tooke Report consultant medical interview.com
Speciality training rcpe.ac.uk
Essays
How to write an essay UK essays.com
GP training sites
National gp recruitment office
Irish College of General Practitioners
Courses
why after the hamster wheel and massive expense of school and med school entry onto a shitty GP training course in preparation for a career in salaried GP serfdom should be yet another thing that requires even more coaching and even more expense for the nations finest youngest minds is puzzling and should really incite some kind of rebellion
Whatever – these courses are good – and it’s not their fault – or is it?
emedica.co.uk
medical-interviews.co.uk
GP training
Practice based small group learning (PBSGL)
Practice Based Small Group Learning NHS Education Scotland
WPBA Case Based Discussion Bradford VTS
http://vimeo.com/album/1534750
WPBA Case Based CEXs Bradford VTS
http://vimeo.com/album/1535465
WPBA COT Bradford VTS
http://vimeo.com/album/1535473
WPBA DOPs Bradford VTS
http://vimeo.com/album/1535468
Mentoring and clinical supervision
http://hacking-medschool.com/mentoring
Clinical supervision London deanery.ac.uk
http://vimeo.com/album/1521296
Identifying learning needs
Learning needs = discrepancy between the starting point (where are you now) and end point (where you want to be) (Kaufman and English, 1979).
identifies 46 formal and informal methods of needs assessment (yawn) including:
Personal review
Personal reading, internet and media, lectures and meetings, further study and research
Formal testing, e.g. quizzes in medical magazines; PEP CDs; BMJ learning modules; SWOT analysis; and Manchester Rating Scales.
Reflection on challenging consultations or interactions (what happened; why did it happen; what can I do differently next time to alter the outcome
COT/ Videos of consultations I joint surgeries: actual performance is reviewed by the doctor or by a peer to see if the desired behaviours are present, e.g. did the doctor demonstrate empathy.
Clinical Practice
Audit
SEA
Patient Feedback
Patient Feedback
Patient Satisfaction Survey
PUNS (patients asking questions Dr cant answer)
Complaints
Colleague/Staff Feedback
Informal – practice Meeting
360 degree feedback
Appraisal
PACT
Guidelines
Individual learning plan
aka PDP next page
SMART learning objectives based on the needs you identified learning needs
How the learning objectives relate to your organisation’s goals and/or values
How the learning will be carried out
How much it will cost this is optional, but might be useful in giving you an understanding of the true cost of learning, including the hidden cost of time
When the learning will be completed
What happens after the learning – how it will be applied and evaluated.
1: What do you hope to achieve from the learning activity?
2: What organisational value or goal does this relate to?
3. Which of the skills in the skills framework does it relate to?
4: How will the learning activity be carried out?
5: When will it be completed?
6: How much will it cost?
7: After the learning activity have you learned what you set out to learn (1) how has it changed your performance, and helped you contribute to the values or goals in (2)
Appraisal / revalidation
CPD CME
Continuing professional development cycle: 5 stages (yawn)
1 assessment of individual and organizational needs
2 making personal development plans
3 implementation
4 reinforcement and dissemination
5 review of the effectiveness of the CPD intervention
http://www.gpvts.info/cme1.htm
PDP professional / personal development plan
Content and praxis largely dictated by requirements for Appraisal and Revalidation (Form 4) – essentially a PDP should contain
1. what the planned CPD activity is
2. its intended date of completion
3. how the educational need was identified
4. the changes to practice that will occur on completion of the CPD
5. the dates for completion of the changes detailed in (4)
CPD log
http://hacking-medschool.com/cpd-tag
Domain 1 Knowledge, Skills and Performance
attribute 1.1 professional performance
attribute 1.2 knowledge and experience
attribute 1.3 records
Domain 2 Safety & Quality
attribute 2.1 Patient protection & improved care
attribute 2.2 risk management
attribute 2.3 own health
Domain 3 Communication Partnership & Teamwork
attribute 3.1 communication
attribute 3.2 colleagues & delegation
attribute 3.3 patient partnerships
Domain 4 Maintaining Trust
attribute 4.1 respect for patients
attribute 4.2 fairness
attribute 4.3 honesty/integrity
250 Credits tags categories taxonomies
Appraisal Checklist
Professional Details
PDP – review of last year
CPD Credits
PDP – agree this year
Complaints
Audit
SEA
Patient Feedback
360 Feedback
Health
Probity
Additional Evidence
CPR
Child Protection
SIGN OFF
GMC Attributes
1 Knowledge Skills Performance / Maintaining Performance /Knowledge & Experience / Records
2 Safety & Quality /Patient Safety & Improved Care /Risk Management / Own Health
3 Effective Communication /Teamwork & Delegation / Patient Partnership
4 Maintaining Trust / Respect for patients / Equality & Fairness /Honesty & Integrity
Professional Performance,Knowledge & Experience,Good Records,Safety & Quality Improvement,Effective Communication,Collaboration & Delegation,Partnership With Patients,Risk Management,Attention to Own Health, Respect for Patients,Fairness Patients/Colleagues, Honesty/Integrity
1 Good clinical care
2 Maintaining good medical practice
3 Relationships with patients
4 Working with colleagues
5 Teaching training appraisal
6 Probity
7 Colleague Health & performance
Why Chosen
Opportunistic / Serendipitous
Personal Interest/Ambition
PDP
Core Knowledge
In-service Training
PUNS DENS Newly Identified Need
Other
Impact
Self
Patients
Practice
Locality
Wider
RCGP curriculum
1 Being a GP,2 Consultation/Clinical Examination/Communication,3.1 Clinical Governance,3.2 Patient Safety,3.3 Ethics Values Medicolegal,3.4 Equality & Diversity,3.5 EBM,3.6 Research/ Academic,3.7 Teaching/Mentoring,4.1 Management & Leadership,4.1l Managemen & Leadership,4.1 NHS,4.1 Practice Management,4.2 Commissioning,4.2 IM&T,5 Health Promotion/DP,6 Genetics,7 Acute Care,8 Children/Young People,9 Older People,10.1 Women’s Health,10.2 Men’s Health,11 Sexual Health,12 Cancer & Palliative Care,13Mental Health,14 Learning Disabilities,15.1 CVS,15.2 GIT,15.3 Drugs/Alcohol,15.4 ENT/Facial,15.5 Eyes,15.6 Metabolic Problems,15.7 Neurology,15.8 Respiratory,15.9 MSK/Trauma,15.10 Dermatology,15.11 Renal,15.12 Haematology,15.13 Immunology15.14 Infectious Diseases,15.15 Travel Health,15.16 Occupational Health,15.17 General Surgery,16 Prescribing,17 Normal Values & Tests,18 Anatomy
Learning Activity
Book Reading,Journal Reading,Email Bulletin,Internet Research,Online Module,Case Reflection,Small Group Discussion,In-House Meeting,Service Development,Evening/Lunchtime Meeting,Lecture,Workshop,Study Day/Half-Day,Conference,Exhibition,Taught Course,MSc Module,Residential Course,,Hands On Training,In-Service Training,Distance Learning,Research,Teaching,Presentation,Interview Preparation,Writing,Guideline Protocol Development,Prescribing Review,Audit,SEA,PUNS/DENS/OLNS,Observed Practice,Consultation Audit,Patient Feedback,MultiSource Feedback,Complaint
Book Reading
Journal Reading
Email Bulletin
Internet Research
Online Module
Case Reflection
Small Group Discussion
In House Meeting
Service Development
Evening/Lunchtime Meeting
Lecture
Workshop
Study Day / Half-Day
Conference
Exhibition
Taught Course
MSc Module
Residential Course
Hands On Training
In-Service Training
Distance Learning
Research
Teaching
Presentation
Interview Preparation
Writing
Guideline Protocol Development
Prescribing Review
Audit
SEA
PUNS/DENS/OLNS
Observed Practice
Consultation Audit
Patient Feedback
MultiSource Feedback
Complaint
Opportunistic / Serendipitous
Personal Interest/Ambition
PDP
Core Knowledge
In-service Training
PUNS DENS Newly Identified Need
Other
for rapid redeployment of various incarnations of my cpd log / eportfolio databases.
in fact I’m likely to settle on using one of the RCGP/ BMA or other online tools through expediency – even though i feel they’re still not as good as my original prototypes.
my own view is the portfolio should suit ones own personal approach and ideally be something one can use as the centre of ones CPD not just for the collection of evidence and not locked-into /walled-in-by local transient personal political or administrative aspects
i can/might probably try to turn 250 textbooks into my CPD log too using custom fields (probably visible to myself only) and tags/categories such as those above
again this will entail a small ammount of importing into an official approved products – but this has proved relatively easy using my previous cpd vehicles – the recording of cpd activities, reflections , demonstration of learning etc along the way is the important/hard thing – spending a couple of hours tidying it up once a year (or however often one chooses) has not proved particularly burdensome
PUNS DENS OLNs
1 Record some patient identification so you can remember the consultation eg Computer I.D., Age, Sex
2 Describe the PUN Patient Unmet Need
Identified by doctor during or at the end of consultation by reflecting on difficulties, knowledge gaps or areas for improvement “How could I have done better?”
3 Define the DEN Doctors Educational Need – the area for improvement, development or change
4 Classify into relevant areas: (Original “tags” Knowledge clinical/ Knowledge non-clinical/ Skill /Attitude now superceded by domains of GMC/Appraisal)
Identify PUNs that can be easily solved by chatting to colleagues or by delegating to practice staff.
GPs can’t possibly be omni-competent and so PUNs may be met without fulfilling a DEN, for example, by delegation.
PUNs that require some time spent on them form DENs that by definition need addressing – so-called “DEN fulfilment” (groan)
Sometimes PUNs will be met not by individual doctors but by changes elsewhere in the practice administration or managerial development.
…clearly useful and necessary aspect of CPD and identifying and prioritising knowledge gaps but can be a little bit itsy and f in its execution
OLNs Other Learning Needs
because knowledge gaps don’t all come directly from patient encounters
Patient Unmet Need
identified from consultation (or otherwise)
– clinical knowledge
– non-clinical knowledge
– skill
– attitude
Doctors Educational Need
defined by the above
– learning
– delegation
– change in practice management
NOE
naturally occurring evidesce
Personal Reflection
the real value of these to me may be in not only identifying the original problem but also reducing recurring knowledge gaps – “I meant to look that up last time” or I did but I didnt record it somewhere accessible ( even something stupid like passwords) what a waste of energy and efficiency and learning to look up the same thing over and over again – see metacognition.
PUNs and DENs: discovering learning needs in general practice Oxford Radcliffe
Richard Eve 2003 Clifton Lodge Surgery Taunton Somerset
NOE naturally occuring evidence
stuff that just crops up (sometimes/often uninvited)
Naturally Occurring Evidence in ePortfolio Yorkshire and Humberside
Appraisal
NHS Clinical Governance Support
| Appraisal forms | |
|---|---|
| Form 1 | Current curriculum vita |
| Form 2 | brief and factual description of his or her current medical activities |
| Form 3 | documentation in line with GMP 7 |
| Form 3A | Good clinical careMaintenance of core clinical competencies Doctor patient communication Premises Patient access to services Integrity of medical records Use of equipment Appropriate use of investigations Prescribing Structured approaches for the management of chronic diseases Emergency care |
| Form 3B | Maintaining good medical practice: Keeping up to date Personal and practice development planning Audit Significant event analysis Awareness of local and national health related initiatives Health & safety regulations and employment matters. |
| Form 3C | Relationships with patients information about services consent to treatment Confidentiality Discrimination and prejudice against patients Complaints and formal enquiries. |
| Form 3D | Working with colleagues Communication within the practice Teamwork and staff development Defined roles and responsibilities Referrals. |
| Form 3E | Teaching and training, appraising and assessinghonesty and objectivity in appraisal and assessment of colleagues. Those involved in teaching have an obligation to maintain and develop their skills |
| Form 3F | Probity and HealthAccuracy of published information about services Honesty in writing reports and signing documents Integrity of research Financial and commercial dealings Conflicts of interest Doctors are requested to consider whether or not aspects of their own health influence their ability to care for others. |
| Form 3G | An opportunity is provided for the doctor to share his or her insights to reflect on the achievements of the appraisal period, to consider present developmental needs and to identify constraints to progress. Completion of necessary paperwork prior to the appraisal discussion is an essential prerequisite for constructive dialogue between the doctor and appraisal facilitator. Description of activities should be succinct and accurate. There is no need for exhaustive detail though necessary supportive documentation should be included. The appraisal discussion will provide an opportunity for explanation and fuller account |
| Form 4 | This document provides an accurate summary of both the appraisal submission and issues identified in discussion. An outline of the doctor’s learning and developmental strategy over the subsequent twelve months will be included. The doctor and the appraiser will each retain a copy of Form 4. Form 5 Declaration that the annual appraisal has been satisfactorily completed. The appraisal facilitator will send a copy of the signed document, to the central Appraisal Office |
GP Appraisal Step by Step Guide NHS Sheffield
Appraisal Checklist
Professional Details
PDP – review of last year
CPD Credits
PDP – agree this year
Complaints
Audit
SEA
Patient Feedback
360 Feedback
Health
Probity
Additional Evidence
CPR
Child Protection
SIGN OFF
From Salford GP Learning Hub – Dr G Wong
Evidence with asterisks (*) are essential for Revalidation (RCGP Aug 2009) while those in italics are considered good practice.
Learning credits could be obtained from all sections not just under GMP.
General
Statement of all roles* (paid or unpaid)
Good Clinical Care
Clinical Audits*
Significant Event Audits*
PUNS & DENS
Use of evidence-based protocols
Prescribing data
QOF data
Referral log, data or outcomes
Patient access (e.g. appointments, extended hours)
PBC data
Supporting self-care
Feedback (e.g. hospital, PCT)
Structured case review
Maintaining Good Medical Practice
Personal Development Plan*
50 learning credits*
Competence in other roles* (e.g. GPwSI, appraisers, OOH)
Reflective learning log
Learning needs analysis (e.g. nPEP)
Range of learning topics
Range of learning methods
Resuscitation training
Child protection training
Relationship with patients
Personal patient survey with reflection*
Complaints (if any) with reflection*
Cards/letters from patients
Consultation training
Complaints procedure
Confidentiality policy
Up to date practice leaflet/website
Working with colleagues
Multisource feedback with reflection*
PHCT meetings
PHCT initiatives (e.g. away days, buddy scheme)
Practice Development Plan
Contacts with other GPs
Contacts with secondary care colleagues
Teaching and Training
Feedback from learners
Reflection of teaching sessions
Educational material produce (e.g. handouts)
Activities to maintain competence
Learning needs analysis
Peer review of teaching
Postgraduate qualifications
Probity
Any GMC restriction/GMC certificate*
Ongoing investigation by regulatory bodies*
Indemnity cover*
Practice agreement
Employment contract
Audited accounts
Chaperone policy
Gift policy
Consent policy
Case discussion of ethical dilemma
Issues of conflict of interest
Self declaration
Management
Practice, PCT, LMC, PBC, BMA, GPwSI etc
Reflection of roles and responsibilities
Learning needs analysis
Research
Research governance
Health
Declaration of health issues*
Hepatitis B status
Registered with a GP
Work life balance
Appraisal form 1 background details (CV)
Dr Shitty Shitter
Shitside Health Centre
Shits Green Green
M30 8AR
DrX@mac.com
Dr.X@nhs.net
12 X Street
Xchester
MX 4XX
X7x57X8X6X
Salaried GP (PCT) 37.5 hrs Aug 2009
MB ChB 1988
MRCGP 1994
Postgraduate Diploma Sports & Exercise Injury Management 2004
GMC X2X031 19X9 Full
JCTCGP 01/12/1993
Salford PCT Performers List
Other Current/Recent Positions
GP Advisor Clinical Solutions Decision Support 2010
GP Advisor Northwest eHealth 2009-2010
Sessional GP Oldham WIC Cumbria Health On Call 2008-2009
GP Principal, Huddersfield University Health Centre 1996 – 2009
Other Details Describing Current Medical Practice
Salford PCT LNC
In House Acupuncture +/- MSK
Appraisal form 2 current medical activities
1 Salaried GP Clinical Lead PCT FT 37.5 hrs 1 yr
Performers List
Accreditation
Clinical Governance
Appraisal
CPD
Clinical Supervision
Job Description
Person Specification
Induction & Training
Daily meetings Weekly Clinical with Admin Input
General GP
Contraception but not IUD/Implants
Sexual Health
Antenatal Care
Postnatal Care
Child Health
Minor Surgery
Teaching
Management
Governance
Child Protection
PB Commissioning
Clinical Assistant
Urgent Care / WIC
2 GP Advisor Medical IS and GP Rep for JNC Project
See “Why did i get sacked (again)?” Structured Reflective Template
Appraisal form 3 questionnaire
Form 3 Report
1 Good Clinical Care
2 Maintaining Good Medical Practice
3 Patients
4 Colleagues
Good Points
Widely experienced. Generally good communication skills and bedside manner.
Patient centred, caring and tenacious with management – don?t like to say nothing more we can do.
Genuinely committed to continuous quality improvement for patients, staff and the organisation.
Bad Points
Lacking confidence with CDM and other aspects of General Medical Practice having been in a specialist practice for some years.
Communication can deteriorate into idiosyncratic style not always to everyone?s liking – if deviate too much from communication framework.
Talk to fast mumble and repeat myself too much
Sometimes lack of confidence with young babies, disgruntled punters and 3rd parties –
Sometimes confuse personal tendency towards openness with organisational needs for discretion.
Genuinely committed to CQI and lifelong learning.
Understand the problem more than most (I think) and wish to help others with this problem.
Understand the privilege of being a Doctor and the responsibilities that entails wrt to specialist knowledge and skills – particularly when that knowledge is so precarious and vicariously available to the (expert) patients themseves.
See CPD Log & Documents
Very positive feedback from previous patient surveys.
Generic patient satisfaction 99.9% in current working environment.
(survey introduced by myself but other attempts at feedback and information giving — website , practice leaflet etc limited by PCT constraints)
One complaint over last appraisal period.
Statement Exceptional Circumstances
Form 3 Questionnaire
Appraisal form 4 PDP
1 Core Clinical Knowledge
What development needs do I have ? – explain the need
Improve knowledge and skills in core clinical knowledge
Continuing need for systematic coverage of current medical and basic clinical knowledge
How Will I address this Need – explain how you will take action and what resources you will need
Attend GP NB medical update course and provide evidence of reflection
Date By Which I plan to Achieve the development goal (agreed with appraiser)Aug 2011
Outcome – how will your practice change as a result of the development activity?
Patients will benefit from up to date care
Completion – agreement with Appraiser (next year) that development need has been met
2. Improve knowledge and skills in field of medical management and leadership
Embark on RCGP SPED course and provide evidence of reflection August 2011
Will Refine & Broaden Skill Base
Build on in-house and broader opportunities for formal management experience
– service development – bids – governance and structures – Inhouse opportunities – involvement commissioning – SE
3 Improve and Update Skills in field of Family Planning (Certifications)
Attend FP update and arrange implant training August 2011
Update skills, knowledge and cerification in family planning/ sexual health, minor surgery and CHS Formal refreshers in Minor Surgery /Family planning and Child health as required for needs of certification
Patients will have up to date care.
Personal and practice Governance requirements will be satisfied.
Others
Health Informatics -Msc University Leeds
Refresher training in MSK – GPSI Training Bradford — if can find tutor
Own Self Learning in Database and Medical App Development
Urgent Care
Complaints template
1 Description Of Events
2 Complainants Concerns
3 Assessment of Complaint
4 Actions Arising
5 Outcome
6 Lessons Learnt Changes Made Implications
(Reflections on complaint wrt – KSP – safety & quality – communication partnership teamwork – maintaining trust)
Be sure to follow practice/organisation complaints procedure esp wrt timely respones and informing complainant of said procedures.
SEA template
1 Title of incident
2 Date of Incident
3 Date of SEA
4 Who Present at SEA
5 Good Points
6 Bad Points
7 Reflection – knowledge skills performance – safety and quality – communication partnership teamwork – maintaining trust
8 Changes agreed – for Dr personally – for the team
Clinical audit template
1 Title
2 Reason Chosen
3 Dates of first data collection & re-audit
4 Criteria Standards set with justification (ref to guidelines etc)
5 Results of 1st Data Collection wrt standards
6 Summary Discussion Changes Agreed
7 Changes Implemented
8 Results of 2nd data collection versus standards
9 Quality Improvement Achieved
10 Reflections on Audit wrt – KSP – safety & quality – communication partnership teamwork – maintaining trust
SRTs (cpd/appraisal)
Structured reflective templates (cpd/appraisal)
hacking-medschool/srts-teaching
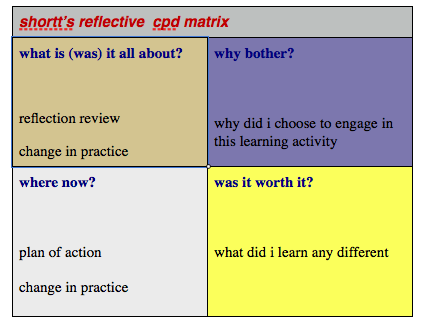
What / So What /Now What
Neat simple template but no less sophisticated or effective for that.
Can be used for (reflective) recording of Learning Activities and as generic analytic framework for other educational/work situations and scenarios.
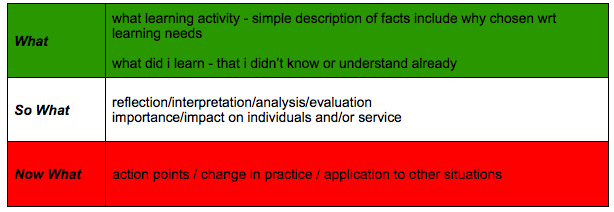
| What So What Now What | ||
|---|---|---|
| What | the facts | describe the situation/event/what happened |
| So What | analysis/reflection/ interpretation | why this matters |
| Now what | action | formulate action plan – what will learner(s)/participants do differently? how can this be applied to other situations? |
“What? So What? Now What?” experiential reflection rubric (Eyler & Giles, 1999 – via Dr. Stephanie Y. Evans)
Reflection in Higher Education Service-Learning Conors and Seifer September 2005
Eyler and Giles 1999 Where’s the Learning in Service-Learning?
http://www.energizeinc.com/art/abres.html
http://www.inquiry.net/adult/trainer/reflection.htm
Bloom’s Question Types (terms in orange – Knowledge, Comprehension, Analysis, Application, Synthesis, & Evaluation).
Basic Reporter’s Questions (terms in blue – Who? What? When? Where? Why? How?)
| Reporters Questions 5 Ws and 1 H |
|---|
| What |
| When |
| Why |
| Where |
| Who |
| How |
Core Question
What information do I need access to in order to learn through this expereince?
Cue Questions
Description of experience
Phenomenen Describe the “here and now” experience
Causal What essential factors contributed to the experience?
Context What are the significant background factors to this expereince?
Clarifying What are the key porcesses for reflection in this expereince?
Reflection
What was I trying to achieve?
Why did I intervene as I did?
What were the consequences of my action for myself / patient / team / organisation?
How did I feel about the expereince as it was happening?
How did patient / others feel?
How do I know what patient / others felt?
Influencing factors
What internal factors influenced my decion making?
What external factors influenced my decion making?
What sources of knowledge did / should have influenced my decioin making?
Could I have dealt better with the situation?
What other choices did I have?
What would be the consequences of these choices?
Learning
How do I feel about the expereince now?
How have I made sense of this expereince in the light of past expereince and future practice?
Has this expereince changed my ways of knowing, thinking, doing or me personally?
By combining the core questions in this model with the questions on identifying your further needs and developing an action plan to address them you will begin to write more reflectively.
Kent Surrey Sussex Guide To Reflective Writing
Experiential Learning Cycles Overview of 9 Experiential Learning Cycle Models
SRT Gibbs
Aims Versus Objectives (groan)
| SMART goals/aims/objectives | |
|---|---|
| Specific | Think about exactly what needs to be done. For example if wanting to eat less fat, start with small steps like using semi skimmed milk, butter substitutes or even just spreading butter more thinly on bread and using low fat & low cal food options |
| Measurable | A way of assessing the achievement of goals; for example eating five fruit and vegetables each day, or no more than three portions of fat per day or the 10,000 step a day challenge |
| Achievable | Is the goal something that can be realistically achieved? Aim for something that is achievable and then gradually work towards what might be desired. For example if needing to reduce snacks, start by cutting down the frequency and quantity gradually, rather than suddenly stopping |
| Relevant | Is the smaller goal helping towards achieving the larger goal? For example, if the aim is to reduce fat intake, then need to focus specifically on eating foods low in fat |
| Time specific | Setting a realistic time frame by which goals will be achieved. For example next week, next month, three months time |
SPECIFIC
Objectives should specify what they need to achieve – percieved wisdom suggests a specific objective is more likely to be achieved.
To set a specific objective you need to answer the SIX “w” Questions
Who: Who is involved?
What: What do i wish to accomplish?
Where: identify a location
When: establish a timeframe
Which: identify requirements and constraints
Why: specific reasons purpose or benefits of accomplishing the goal
Specific means that the objective is concrete, detailed, focused and well-defined.
The objective must be straight forward and emphasize action and the required outcome.
Specific also means that it is results and action-orientated.
Objectives need to be straight-forward and to communicate what you would like to see happen.
To help set specific objectives It helps to ask:
What am going to do? This are best written using strong action verbs such as conduct, develop, build, plan, execute, etc.
This helps your objective to be action-orientated and focuses on priorities
Why is this important for me to do?
Whois going to do what?
Whoelse need to be involved?
When do I want this to be completed?
How am I going to do this?
Measureable means that the measurement technique is identified and we are able to track the actions as we progress towards the objective.
It’s important to have measures that will encourage and motivate you on the way as you see the change happening – this may require interim measures.
Objectives (unlike say, aspirations or visions) need to be achievable
If the objective is too far in the future, you may find it difficult to keep motivated
Objectives need to stretch you, but not so far that you become frustrated and lose motivation.
Measurable
You should be able to measure whether you are meeting the objectives or not
Estabablish concrete criteria for measuring progress toward the attainment of the set objectives.
When you measure your progress, you stay on track, reach your target dates, and experience the feeling of achievement.
Attainable
When you identify objectives that are most important to you, you begin to figure out ways you can make them come true.
The objective needs to be attainable by you based on the skills you have and the constraints imposed.
What do I warn: to accomplish?
Where: Identify location
When: Establish a time frame.
Which: ldentify requirements and constraints
Why: Specify results, purpose or beneflts of accomplishing the objectives
To determine your objectives measurable, ask How much? How many? How will I know when it is accomplished?
Realistic
Can you realistically achieve the objectives with the resources available?
To be realistic, It must represent an objective toward which you are both willing and able to work,
An objective can be both hard and realistic – you are the only one who can decide just how hard it should be.
Your objectives probably realistic if you truly believe that it can be accomplished.
Additional ways to know if your objective is realistic is to consider if you have accomplished anything similar in the past or ask yourself what conditions would have to established to accomplish this objective.
Objectives that are achievable, may not be realistlc – realistic: does not mean easy rather that you have the resources to do it
Achievement of an objective needs resources eg skills, money, equipment, support etc
Whilst keeping objectives realistic, ensure that they stretch you.
Most objectives are achievable but, may require adlanQ’e 11″1 your pnontles to make them happen.
Time-bound
set deadlines for the achievement of the objective. Deadlines need to be both achievable and realistic.
Not setting a deadline reduces the motivation and urgency required to execute the tasks.
• Do you have the resources available to achieve this objective?
• Do I need to revisit pnontles ~ my I~e to make this happen?
• Is it possible to achieve this objective
• When will this objective be accomplished? ls there a stated deadline?
When do you want to achieve the set objectives?
Tangible
T also stands for tangible -A goal is tangible when you can experience it with one of the senses, that is, taste, touch, smell, sight or hearing.
When your goal is tangible you’ll have a better chance of making it specific and measureable and thus attainable.
Creating SMART Goals
Diagnostic Questions
What exactly are we going to do, with or for whom?
What strategies will be used?
Is the objective well understood?
Is It clear who is involved?
Is the objective described with action verbs?
Is It clear where this will happen?
Is it clear what needs to happen?
Is the outcome clear?
Will this objective lead to the desired results?
How will I know that the mange has occurred?
Can these measurements be obtained?
Can we get it done within the proposed time-frame?
Do I understand the limltations and constraints?
·can we do this with the resources we have?
·has anyone else done this successfully?
·is this possible?
MSF 360 degree
360 Degree Feedback: The Good, the Bad, and the Ugly About.com
Factors associated with variability in the assessment of UK doctors’ professionalism BMJ Nov 2011
Revalidation appraisal toolkit ATK and eportfolios
Appraisal Revalidation Newsletter Jan 2012 NHS Salford www.salfordgp-learninghub.org
Gen Wong (gwong@nhs.net) Alan Berry, (Alan.Berry@salford.nhs.uk) Yvonne Kelly (Yvonne.Kelly@salford.nhs.uk)
According to latest GMC guidance, Revalidation is still pencilled to start at the latter part of 2012. The plan is to Revalidate all doctors in a local area within 3 years of the starting date. This is done by revalidating a third of the doctors per year; hence completing the proc-ess in 3 years.
The GMC and RCGP will continue to guide us to be “revalidation ready”. How-ever, a few issues are worth bearing in mind now: You need to set up a GMC online account before Revalidation starts. Set this up at www.gmc-uk.org Appraisals remain the core component for Revali-dation. Annual appraisals is the professional responsibil-ity of the individual doctor. GPs need to ensure they have arranged their appraisal date in good time and give at least 2 weeks for the ap-praiser to assess their ap-praisal folder before the discussion.
Appraisal and Revalidation electronic platforms
NHS Salford has paid for all GPs to use the Clarity Ap-praisal Toolkit (ATK) until 30/10/2012. This version of the ATK was not made for Revalidation. Clarity has now come out with a new version of the ATK, Ap-praisal Toolkit 2011, which is “revalidation-ready”. Ap-praisal Toolkit 2011 will eventually replace the “old” ATK. The other existing workable system which is “revalidation-ready” is the RCGP ePortfolio.
However, GPs need to be aware of future costing for these systems. The RCGP system, currently free, will be chargeable from April 2012 for non-RCGP mem-bers. There may be an initial discount for 2012/2013 (not confirmed), from £120 to £22 but eventually non-members will still need to pay about £120 per year. Appraisal Toolkit 2011 is free to all Salford GPs until 30/10/12. However, there is no guarantee of funding
from the PCT beyond that date. Annual cost for this system is about £60 per GP.
The RCGP cost includes local (i.e. PCT) admin sup-port. Unfortunately, the Clarity cost does not include this function.
GPs will need only one elec-tronic system for Revalida-tion. They need to decide which system suit them best based on their circum-stances.
Clarity Appraisal Toolkit 2011
All existing users of the Ap-praisal toolkit (ATK) will eventually need to move to the new version called Ap-praisal Toolkit 2011. Yvonne Kelly will work with Clarity to migrate all users to the new system. Previous completed apprais-als and supporting docu-ments will automatically move across in this process. Once migration is complete, users will get an email from Clarity asking them to up-date their details.
All GPs who have already completed their appraisal by 31/01/12 will be migrated to the new Toolkit. Yvonne Kelly will perform the mi-gration and these GPs do not need to take any action. When the process is done, they will receive confirma-tion from Clarity to update their details for the new Toolkit. They could then prepare for next year’s ap-praisal (appraisal year 2012/2013) on the new Toolkit. GPs, whose com-
appraisal (appraisal year 2011/2012) and is using the old toolkit should finish this appraisal using the old tool-kit. Once their appraisal is completed, Yvonne Kelly will migrate them over to the new Toolkit. They could then prepare for next year’s appraisal (appraisal year 2012/2013) on the new Tool
Registration for RCGP Revalidation ePortfolio
RCGP Members or Ex-Members
1. Visit https://gpeportfolio.rcgp.org.uk
2. Login using your RCGP website ID and password
3. The first time you login, you will be asked to enter NHS Salford Unique Password, which is SaL01mjj12
4. You will also be asked to enter your Personal Identification Pin. Please contact Yvonne Kelly (Yvonne.Kelly@salford.nhs.uk or 2124416) for your individual Pin details
Non-Members
1. Visit https://integra.rcgp.org.uk/membersarea and register with the website
2. Within 2 hours of registration, you will receive an email from Integra@rcgp.org.uk. Follow the link within this email where you will be asked to enter the password provided in the email
3. Log in to the RCGP self-service area, click Non-Member Services from the menu on the left and follow the steps to sub-scribe to the Revalidation ePortfolio
4. Follow the Member steps as above