20
| Paeds vital signs | ||||
|---|---|---|---|---|
| Age | RR | HR | Weight | BP |
| 1-12w Newborn | 100-220 | 3.5 kg | ||
| 0-1y infant | 30–60 | 6m 7.5 kg1 Year 10kg | >60 | |
| 1-3y toddler | 24–40 | 90-150 | >70 | |
| 3-6y preschool | 22–34 | 80-140 | 5 Years 20kg | >75 |
| 6-12y school age | 18–30 | 70-120 | 10 Years 35kg | >80 |
| 12–16y adolescent | 12-18 | 60-100 | >90 | |
| Wt = (age+4)*2 |
| SBP = 80 + 2 X years of age |
Pulse rates for a child who is sleeping may be 10 percent lower than the low rate listed.
In infants and children aged three years or younger, the presence of a strong central pulse should be substituted for a blood pressure reading
hacking-medschool/paeds-vital-signs
| GCS children under 4 | |
|---|---|
| Eye Opening | |
| Spontaneously | 4 |
| To verbal stimuli | 3 |
| To pain | 2 |
| No response to pain | 1 |
| Best motor response | |
| Spontaneous or obeys verbal command | 6 |
| Localises to pain or withdraws to touch | 5 |
| Withdraws from pain | 4 |
| Abnormal flexion to pain (decorticate) | 3 |
| Abnormal extension to pain (decerebrate) | 2 |
| No response to pain | 1 |
| Best verbal response | |
| Alert, babbles, coos, words to usual ability | 5 |
| Less than usual words, spontaneous irritable cry | 4 |
| Cries only to pain | 3 |
| Moans to pain | 2 |
| No response | 1 |
| Conscious level AVPU | |
|---|---|
| A | Alert |
| V | Responds to Voice commands |
| P | Responds to Pain |
| U | Unresponsive |
| PEWS | |||
|---|---|---|---|
| Behaviour | CVS | Resps | |
| lethargic confused or reduced pain response | grey CRT>5 tachycardia +30 or bradycardia | 5 below normal with retractions +/- >50% FiO2 | 3 |
| irritable agitated and inconsolable | CRT 4 tachycardia + 20 | >20 above normal using accessory muscles 40-49% FiO2 or >3 LPM | 2 |
| sleeping or irritable and consolable | pale or CRT 3s | >10 above normal using accessory muscles 24-40% FiO2 or >2 LPM any initiation of O2 | 1 |
| playing appropraite | Pink CRT 1-2s | WNL for age no retractions | 0 |
| Add 2 pts for frequent interventions (suction, positioning, O2 changes or multiple IV attempts>7 assess every 30m6 assess every hr5 assess every 1-2 hrs0-4 asses every 4 hrsParental concern should be an automatic call to RRTchoa.org/PEWS | |||
Babycheck pamphlet for parents
General assessment
Observe the child from a distance whilst obtaining the history.
The child’s interest/trust can be gained and information obtained by giving them a toy, tongue depressor whatever whilst talking to the parents
Children who are truly sick tend to be preoccupied, uninterested and unsmiling, and usually the parent/guardian will have noticed these changes
If you (with the parent) decide that such changes are very marked, then they alone could be sufficient criteria for urgent referral
In most circumstances there will be accompanying signs and these should be sought. Examination should cover the child’s airway and breathing, circulation
and neurological signs together with some assessment of the child’s general appearance. It is particularly important to check for features suggesting very
serious illness (preterminal signs).
It is also important to recognise that if a child is clearly ill, but you can find no abnormality of airway, breathing, circulation or conscious level, referral for a second opinion is still appropriate although it may be less urgent. (source?)
Airways and breathing
Check for features of altered respiratory work
recession/use of accessory muscles
flaring of alae nasae
grunting
stridor/wheeze
positioning, eg ‘tripod position’ to splint the chest wall
increased respiratory rate
exhaustion (this is a preterminal sign).
Assess the efficiency of breathing. – using stethoscope and pulse oximeter.
A silent chest is a pre-terminal sign.
Look for the effects of respiratory failure on other organs
cyanosis (another pre-terminal sign)
tachycardia
bradycardia (preterminal sign)
agitation, confusion or drowsiness.
Circulation
Check HR, pulse volume and capillary refill (press on the skin over the sternum for 5 seconds – in a healthy child the blanched area will re-perfuse in less than 2 seconds).
BP drops late in most conditions and, in itself, is of limited value as other signs should be present. Hypotension is a pre-terminal sign.
Look for the effects of circulatory failure on other organs
tachypnoea without recession
pallor
agitation then drowsiness
profuse sweating.
Posture and tone – normal / floppy / increased tone.
Features of meningitis such as neck stiffness or irritability (a child may be upset by being handled).
Abnormal movements.
Pupils particularly reaction to light.
Skin and mucous membranes
Look for changes in the skin and mucous membranes
petechial or purpuric rash
bruising
oedema
signs of dehydration
| Paeds fluid and electrolyte requirements | ||
|---|---|---|
| Daily Requirement | 2500 ml/day | c 35ml/kg/day 100ml/kg first 10kg plus 50ml/kg/day next 10 kg plus 20ml/kg/day beyond |
| urine losses | 800-1500 ml | |
| stool losses | 250 ml | |
| insensible loss | 600-900 ml | increased by 10% for each degree of fever decreased on ventilator |
| Na | ||
| Total Daily Maintenance Requirements | |
|---|---|
| up to 10kg body weight | 100 mL/kg/day |
| plus from 11 to 20kg | 50 mL/kg/day |
| plus from 21 to 70kg | 20 mL/kg/day |
| Dehydration | |
|---|---|
| mild | 3-5% of body wt. = 30 -50ml/kg |
| moderate | 6-9% of body wt. = 60 90ml/kg |
| severe | 10-15% of body wt = 100-150ml/kg |
| Oral rehydration |
|---|
| eg dioralyte 120-150ml/kg/day (2-2.5oz./lb/day) maintenance plus replace deficits. |
| Give in small, very frequent amounts. Emphasise importance of fluid replacement to parents |
Paeds BLS
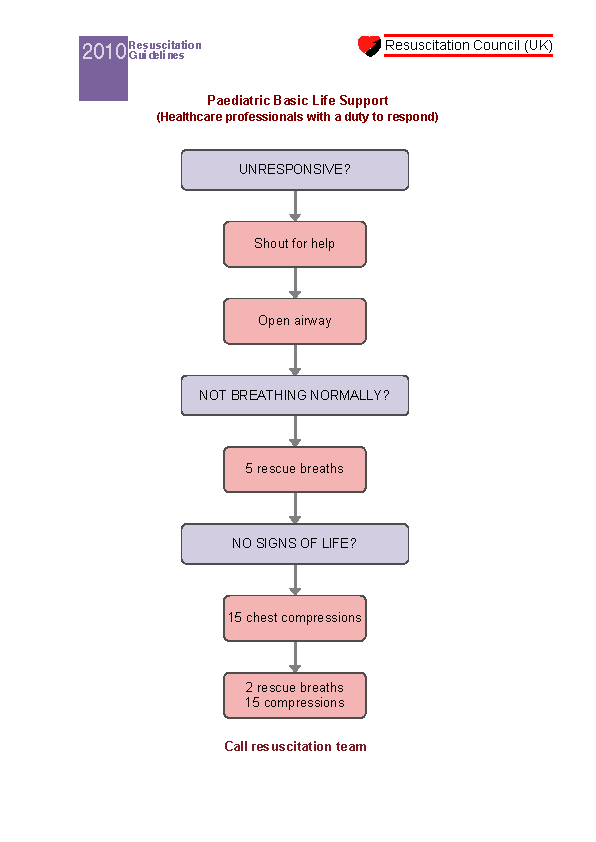
How to rescuscitate a child NHS Choices
http://www.cprdude.com/default.shtml
Palpating brachial artery in kids
Paediatric Nursing Procedures Google books
Paeds chin lift
Paeds ALS
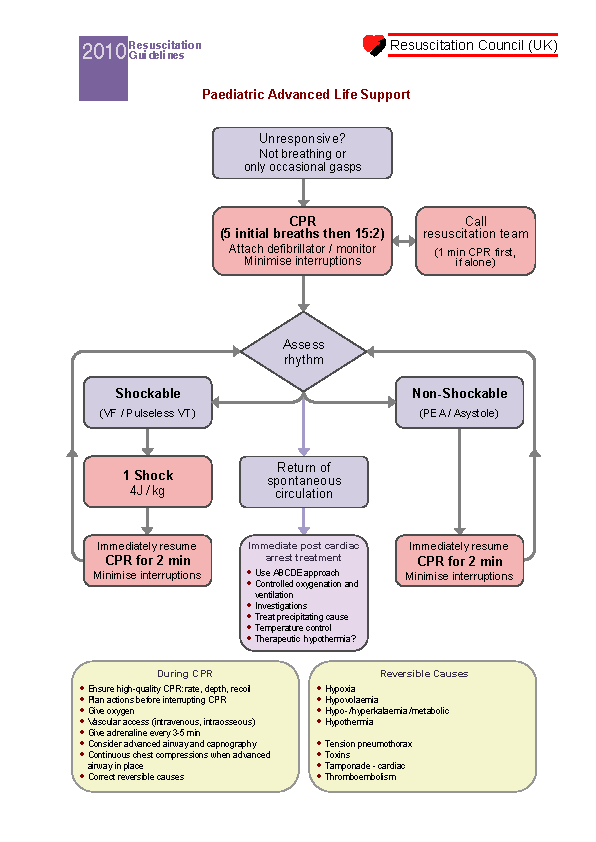
Paeds ET tubes and laryngoscopes
Anaphylaxis Treatment Algorithm for Children
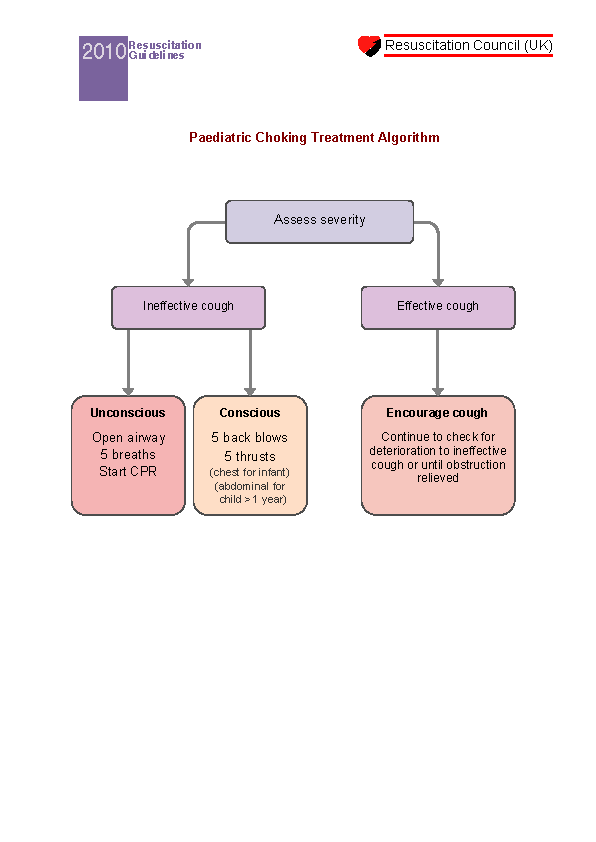
Choking child and infant
Drowning child
| Paeds doses (APLSG) | ||
|---|---|---|
| Age | mean weight (kg) | % adult dose |
| Newborn | 3.5 | 12.5% |
| 2 month | 4.5 | |
| 3 months | 6 | |
| 4 month | 6.5 | 20% |
| 6 months | 8 | |
| 9 months | 9 | |
| 1 year | 10 | 25% |
| 2 years | 12 | |
| 3 years | 15 | 33.3% |
| 4 years | 16 | |
| 6 years | 20 | |
| 7 years | 23 | 50% |
| 8 years | 25 | |
| 10 | 30 | 60% |
| 12 | 40 | 75% |
| 14 | 50 | 80% |
| 16 | 60 | 90% |
| Adult | 70 | 100% |
| Paediatric Weight = (age+4)*2 |
Paeds acute severe asthma
For Children admission should be arranged when there is:
• Failure to respond or early deterioration following bronchodilator (Peak flow < 50% expected 10 mins after Rx),
• GP request for admission,
• Severe breathlessness or tiredness,
• or difficulty at home with Rx.
Acute asthma paeds under 2
Assessment of acute asthma in early childhood can be difficult. Intermittent wheezing attacks are usually due to viral infection and the response to asthma medication is inconsistent. Wheeze frequently occurs in the absence of a prior diagnosis of asthma and may be due to viral infections, bronchiolitis, asthma, aspiration pneumonitis, pneumonia, tracheomalacia or complications of underlying conditions such as cystic fibrosis or congenital anomalies
Management
Moderate Severe Life threatening
Give: b2 agonist up to 10 puffs via spacer ± face mask or nebuliser
If known asthmatic add prednisolone 10mg daily
While awaiting transfer give: Oxygen via facemask ?2 agonist up to10 puffs via spacer ± face mask or nebulised salbutamol 2.5mg or terbutaline 5mg
Refer urgently (???) if: SpO2 is known to be <92% pre-treatment
the child deteriorates and
has features of life threatening or severe asthma
you are concerned about the parent’s ability to recognise deterioration and/or manage care at home
If poor response add nebulised ipratropium 250micrograms
If not referred advise the parents on what to do if the child deteriorates and review the child regularly
Acute asthma paeds over 5
| Moderate | Severe | Life-threatening | |
|---|---|---|---|
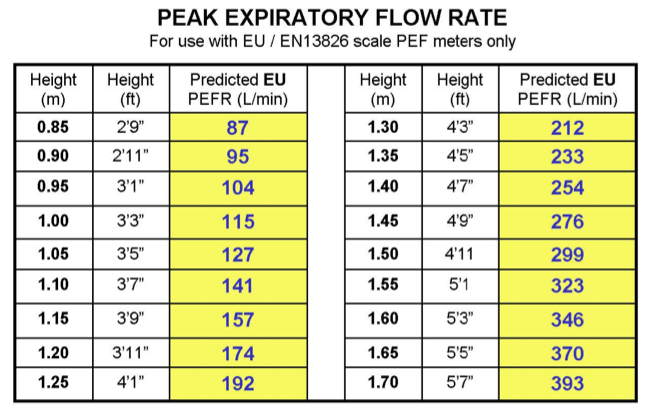
| PEF | >50% | 33-50% | <33% |
| Speech | Normal | cant complete sentences | Silent chest, cyanosis poor respiratory effort |
| Pulse | <110 bpm | >110 bpm | Bradycardia, dysrhythmia, or hypotension |
| Respiratory rate | <25/min | >25/min | Exhaustion, confusion, or coma |
| SpO2 | >92% | <92% | <92% |
When measuring PEF use best or predicted value
Moderate
Give: a ?2 agonist 2-4 puffs via spacer ± face mask
Consider soluble prednisolone 30- 40mg
Increase ?2 agonist dose by 2 puffs every 2 minutes up to 10 puffs according to response
If poor response refer to hospital urgently (???)
Severe
Give: oxygen via face mask
?2 agonist 10 puffs via spacer ± face mask or nebulised salbutamol 2.5-5mg, or terbutaline 5-10mg AND soluble prednisolone 30-40mg
Assess response to treatment 15minutes after ?2 agonist
If poor response repeat ?2 agonist and refer to hospital immediately (????)
Life threatening
Refer to hospital immediately (????).
While awaiting transfer give: oxygen via face mask
AND nebulised (preferably on oxygen) salbutamol 5mg or terbutaline 10mg AND nebulised ipratropium 250micrograms
AND soluble prednisolone 30-40mg or IV hydrocortisone 100mg
Repeat ?2 agonist via oxygen driven nebuliser
If good response continue up to 10 puffs of nebulised ?2 agonist as needed (up to 4 hourly).
If symptoms are not controlled repeat ?2 agonist and refer to hospital urgently (???)
Continue prednisolone for up to 3 days
Arrange follow-up visit to clinic
Nebuliser vs MDI + Spacer
Table 1.1 Peak expiratory flow normal values in children. Normal PEF values in children correlate best with height; with increasing age, larger differences occur between the sexes. These predicted values are based on the formulae given in Cotes JE and Leathart GL (1993) Lung Function (4e) Blackwell, Oxford, adapted for EU scale
MiniWright peak flow meters by Clement Clarke
Adults and children over 5 years with PEF greater than 75% of expected value:
give usual inhaled bronchodilator. Check PEF afterwards check inhaler technique consider commencing inhaled beclometasone, or ensure that the patient is taking an adequate dose of inhaled
corticosteroid .
asthma specialists may consider adding a longacting betaagonist (LABA)
consider prescribing peak flow meter if patient does not aIready have one
recommend recording the results on a chart
advise the patient to seek further help from the most appropriate NHS agency if the asthma worsens despite the increase in treatment
follow up in asthma clinic after 12 weeks for review of longterm treatment
Children 5 years and younger with mild symptoms
try usual bronchodilator or, if uncooperative, nebulised salbutamol 2.5 mg
observe, assess effect, listen to the chest again
consider commencing inhaled beclometasone, or ensure that the patient is taking an adequate dose of inhaled corticosteroid
continue inhaled bronchodilator, but ensure adequate technique
if inadequate, consider changing the inhaler delivery system, e.g. using an Aerochamber or changing to a breathactuated device
advise parents to seek further medical help if the asthma worsens: child more distressed, breathing faster, wheezing more, recession
review in asthma clinic after 1-7 days depending on severity and parental confidence in dealing with asthma
Stridor
| Croup | Epiglottitis |
|---|---|
| 6 months-3 years | 2-7 year |
| Parainfluenza virus | Haemophilus influenzae |
| Often mild or no fever | > 38C |
| May not look too ill | looks ill, toxic, tachycardic |
| Sometimes can eat/drink | drooling saliva |
| Parainfluenza virus | Child prefers sitting upright |
| Often preceded by a prodromal coryzal illness in hours | Rapid course progressing in hourssore throat |
| loud | muffled quieter than croup(unfinished) |
NEVER examine the throat of a child with stridor – if epiglottitis, may precipitate complete airways obstruction
3. Assess the degree of respiratory obstruction. Signs of severity are:
(i) Cyanosis-an emergency
(ii) Generalized restlessness or drowsiness
(iii) Tachycardia
(iv) Intercostal recession and accessory muscle respiration
(v) Continuous stridor
4. Refer urgently a child with signs of obstruction epiglottitis is one instance where the GP should accompany the child to Casualty.
Inhaled foreign body may cause immediate obstruction with acute sudden onset stridor with no prior illness necessitating an emergency tracheostomy -make sure you know how to do one
Treatment
1. Treatment of croup is steam inhalation, sitting the child in a bathroom full of steam or boiling a kettle in the bedroom. Instruct the parents when to call for a revisit if the child’s condition deteriorates – viral croup itself can cause sufficient respiratory obstruction to merit referral
Rx oral dexamethasone
2. Admit all cases where there is any suspicion of epiglottitis as an emergency
3 See / visit all children with stridor
| Croup score | ||||
|---|---|---|---|---|
| Conscious level | normal 0 | disoriented 5 | ||
| Cyanosis | none 0 | c agitation 4 | at rest 5 | |
| Stridor | none 0 | c agitation 1 | at rest 2 | |
| Air Entry | normal 0 | decreased 1 | marked 2 | |
| Retraction | none 0 | mild 1 | mod 2 | severe 3 |
| Total Score Less than 4 mild 4-6 moderate 7 or more Severe mdcalc croup score NCEMI Croup Score |
||||
Pneumonia (paeds)
Tachycardia and low oxygen saturations are the best predictors of pneumonia in children ADC 2011
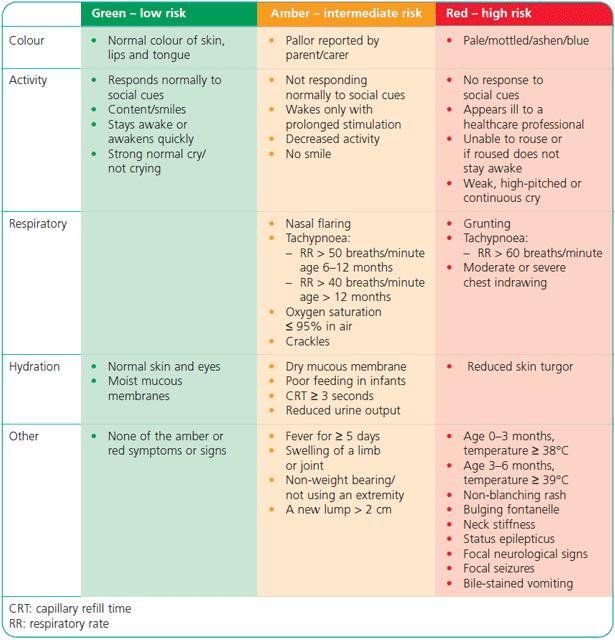
Fever in children NICE traffic lights
NICE CG47 Feverish illness in children May 2007
Ill and Feverish Child Patient UK
Measure and record
Temperature
Heart rate
Respiratory rate
Capillary refill time
Assess for signs of dehydration
Prolonged capillary refill time
Abnormal skin turgor
Abnormal respiratory pattern
Weak pulse
Cool extremities
Febrile convulsions
Around 3% of children between the age of 6 months and 5 years will have at least one convulsion triggered by fever rather than any underlying neurological pathology. Convulsions usually occur at the beginning of the febrile illness and are more likely if the temperature rise is rapid. Fits, which
are mainly generalised tonicclonic, usually last no longer than 20 minutes and are selflimiting with complete recovery within an hour.
Underlying causes
Viral infection (eg upper respiratory tract infection, nonspecific viral illness, roseola, chickenpox etc), otitis media and tonsillitis are the underlying cause of 8590% of presentations. Other possible causes include urinary tract infection, gastroenteritis, lower respiratory tract infection, meningitis, and immunisation.
Management
If the parent or carer telephones, advise them to keep the child lying on his or her side in order to prevent inhalation of vomit.
If the fit lasts longer than 10 minutes give diazepam, preferably as a rectal solution
1 month2 years Diazepam rectal solution 5 mg
212 years 510mg
If the fit is not controlled in 5 minutes, repeat the dose of diazepam. If a child receives multiple doses of diazepam, monitor for respiratory depression.
As soon as is feasible attempt to lower core body temperature
Assessment
The following issues need to be addressed as soon as possible:
What is the likely cause of the fever? It is particularly important to check for the possibility of acute bacterial meningitis, UTI or septicaemia.
Does the febrile illness require treatment in its own right?
Could the fit be the result of some other condition requiring urgent treatment such as hypoglycaemia (check BM), drug overdose, encephalitis or head injury?
Does the child have neurological impairment or developmental delay?
Referral advice
A child should be transferred immediately (????) to hospital if:
? fits are uncontrolled despite 2 doses of diazepam
? breathing/airway is compromised.
A child should be transferred to hospital urgently (???) in any of the following cases. If:
? it is the first fit and they are aged under 18 months
? the fits have atypical features, for example focal seizures
? the fit has lasted longer than 20 minutes
? there is incomplete recovery within one hour
? meningitis is suspected or you are not confident it can be excluded
? the fit is symptomatic of some other disorder requiring admission in its own right, for example hypoglycaemia or trauma
? you are uncertain about the cause of the pyrexia
? this is the second or subsequent fit recurring during the same illness
? there is concern over the ability of the parents to manage the child at home.
In general, a child in supportive circumstances who has a single febrile convulsion can be managed at home. Parents should be advised how to
manage seizures in the event of further fits, ie lowering core body temperature, lying the child on his or her side and administering diazepam.
1. Introduction
These occur in around 3% of children between 6m and 5 years and are triggered by a fever rather than any underling neurological illness such as epilepsy. They typically occur at the outset of the fever, particularly when rising rapidly or spiking. They are tonic clonic lasting up to 20m with full recovery within 1hour. 15% of cases will have further seizures within the same illness.
95% of cases are caused by common infections such as viral URTIs and illness, chicken pox, otitis media, and tonsillitis.
Witnessing a child have a seizure can be frightening for a parent, reassurance and education will help alleviate some of the parents concerns.
Red Flag Warnings
Seizure lasting for more than 15 minutes
More than one seizure a day
Focal seizure
Abnormal neurologic status present preceding the seizure (for example, cerebral palsy)
Less than one year old
Positive family history for epilepsy
Immediate Care Considerations
Maintain / protect airway during seizure
Administer oxygen
Protect from injury during seizure
Take measures to cool the child down
Remove excess clothing
Transfer Hospital
Care for Fitting Child:
Do not restrain them or put anything in their mouth
Note the exact time the seizure started and continue to monitor the duration of the seizure
For prolonged or repetitive seizures administer rectal or intravenous anticonvulsant drugs as prescribed, Once the seizure has finished, place the child in the recovery position to prevent a hypotonic tongue from blocking the airway
Febrile seizures are very common in children, occurring in 3% of under 5s.They tend to be generalized, brief (lasting usually less than 5 minutes and typically triggered by viral-like infections of the ear, pharynx, urinary or gastro-intestinal tract. Febrile seizures that are more complex, demonstrating focal signs or may recur within 24 hours are typically triggered by more serious causes like infections of the central nervous system such as meningitis or encephalitis.
Children who present with a febrile seizure and a family history of epilepsy or underlying neurological conditions such as cerebal palsy should be further investigated as the cause of the seizure may not be the fever, as these children are more likely to have recurrent seizures or epilepsy.
The vast majority of children recover completely even if they have more than one febrile seizure.
Carefully observe and record all aspects of the seizure:
How did it start?
Which part of the body was affected first?
Was more than one area of the body affected at one time?
What kind of movements occurred? Did these movements change?
How long did the seizure last?
Check for signs of dehydration or other signs of compromised health:
Prolonged capillary refill time
Abnormal skin turgor
Abnormal respiratory pattern
Weak pulse
Cool extremities
Tepid sponging is not recommended for the treatment of fever.
Children with fever should not be underdressed or over-wrapped.
The use of antipyretic agents should be considered in children with fever who appear distressed or unwell. Antipyretic agents should not routinely be used with the sole aim of reducing body temperature in children with fever who are otherwise well. The views and wishes of parents and carers should be taken into consideration.
Either paracetamol or ibuprofen can be used to reduce temperature in children with fever. It is no longer recommended they are given together
Antipyretic agents do not prevent febrile convulsions and should not be used specifically for this purpose.
Care for Seizing Child:
Gently lower the child to the floor and place on their side if possible
Do not restrain them or put anything in their mouth
A child should not be left unattended whilst having a seizure
Note the exact time the seizure started and continue to monitor the duration of the seizure
Remove any objects in the nearby area that the child may injure themselves
Talk calmly and reassuringly to the child during and after the seizure
For prolonged or repetitive seizues administer rectal anticonvulsant drugs as prescribed, Once the seizure has finished, place the child on their side
An other wise well child over 18m may who has made a full recovery after a first febrile seizure may be managed at home if parents are happy and there are no worrying features.
Burns rule of nines (child)
Thermal Burns: Initial Assessments and Management Tips @ Firerescue.com
Safeguarding children / child protection
MPS Factsheet Safeguarding Children
NICE PH28 Looked-after children and young people Oct 2010
https://www.education.gov.uk/publications/standard/Childrenandfamilies/Page2/DCSF-00305-2010
http://www.corelearningunit.nhs.uk/SignIn.aspx
Paeds approach to the patient
History
Past medical history
Birth history
Immunisations
Developmental history
Feeding/diet
Family history
Drug history
Social history Family and siblings
School
Red-flags
Developmental delay, poor growth/weight gain
Child protection issues, abuse/neglect
Examination
Plot on centile charts: height, weight, head circumference
Alert, responsiveness, hydration
Uncooperative child and anxious parent/grandparent
Wrapping in a blanket
In an emergency, such as cement inside the lids. if necessary wrap the child up in a blanket to prevent struggling, the arms should be separate inside the layers of blanket and. with an assistant steadying the head ‘and body, lay the child supine on a couch or the floor.
It may be difficult to separate the eyelids. and Casualty Departments should have a pair of curved wire lid speculae for this purpose, as well as sterile saline for irrigation by means of an I.V. giving set. or an undine, after liberal instillation of local anaesthetic drops.
While the child is restrained there will be an opportunity to check the cornea for abrasions or foreign bodies; treatment for this may be given immediately. or if necessary deferred in favour of a general anaesthetic later
Tongue depressor trick
Paeds examining the throat
Paeds examining the Ear
Child health surveillance
hacking-medschool/child-health-surveillance-2
Health promotion (inc Immunisation), screening, and early intervention
Newborn
General physical examination with emphasis on heart, eyes and hips.
Administration of vitamin K, BCG and hep B in high-risk babies
5-6 days – Blood spot test for hypothyroidism and phenylketonuria. Sickle cell, cystic fibrosis, MCAD
Newbirth visit 12 days
Assessment of family’s needs plus family given personal child health record and ‘Birth to Five’ guide HV or MW
6-8 weeks Physical examination and administration of first set of immunisations: polio, diphtheria, tetanus, whooping cough, Hib and meningitis C
3 months Second set of immunisations.
4 months Third set of immunisations
12 months Further developmental assessment.
Around 13m MMR immunisation
2-3 years Health visitor performs further developmental assessment
3-5 years MMR, polio, diphtheria, tetanus and whooping cough boosters
4-5 years School entry review (SN). Foundation stage profile (teacher) physical, emotional, social creative development language and literacy.
10-14 years Tetanus, BCG vaccination given to those who require it.diphtheria and polio boosters (age 1318 years)
Childhood developmental milestones
4-6 w smiles responsively
6-7 m sits unsupported
9m gets to a sitting position
10m pincer grip
12m 2-3 words
15m walks indpendantly
18m tower of blocks
24m 3 word sentances
30m dry by day
| Developmental Red flags (Palmer & Boeckx notes for MRCGP) | |
|---|---|
| Age (months) | Red Flag |
| 2 | absent smile fails to vocalise |
| 4 | persistant fist clenching no laugh |
| 6 | fails to localise voice head lag |
| 9 | fails to sit unsupported fails to say mama or dada non-specifically |
| 12 | fails to stand alone for 2 seconds |
| 15 | fails to walk alone |
| 18 | fewer than 20 words no scribble |
| 24 | fails to kick a ball |
| Developmental Milestones to 6m | |
|---|---|
| 1 m | Lifts head when lying on tummy Responds to sound Stares at faces Follows objects briefly with eyes Vocalizes: oohs and aahs Can see black-and-white patterns Smiles, laughs Holds head at 45-degree angle |
| 2 m | Vocalizes: gurgles and coos Follows objects across field of vision Notices his hands Holds head up for short periods Smiles, laughs Holds head at 45-degree angle Makes smoother movements Holds head steady Can bear weight on legs Lifts head and shoulders when lying on tummy (mini-pushup) |
| 3 m | Recognizes your face and scent Holds head steady Visually tracks moving objects Squeals, gurgles, coos Blows bubbles Recognizes your voice Does mini-pushup Rolls over, from tummy to back Turns toward loud sounds Can bring hands together, bats at toys |
| 4 m | Smiles, laughs Can bear weight on legs Coos when you talk to him Can grasp a toy Rolls over, from tummy to back Imitates sounds: “baba,” “dada” Cuts first tooth May be ready for solid foods |
| 5 m | Distinguishes between bold colors Plays with his hands and feet Recognizes own name Turns toward new sounds Rolls over in both directions Sits momentarily without support Mouths objects Separation anxiety may begin |
| 6 m | Turns toward sounds and voices Imitates sounds Rolls over in both directions Is ready for solid foods Sits without support Mouths objects Passes objects from hand to hand Lunges forward or starts crawling Jabbers or combines syllables Drags objects toward himself |
Neonatal Examination / Newborn Babycheck
Record details of pregnancy & delivery
FH. Heredity diseaese and health of siblings.
APGAR at 1 min and 5 min.
Skull & Spine
Limbs & Gestation.
Birthweight.
Placenta. Cord Vessels.
Head Circ
Ht
Wt
Temp
Pulse
Resps
Facies
Skull
Palate
Fontanelles
Eyes Red Reflex
Ears
Lungs
Heart Sounds
Femoral pulses
Abdomen
Genitalia
Anus
Skeletal Symmetry
Hips
Skin
Muscle Tone
Reflexes
6 week baby check
Start by asking some open questions to elicit any concerns about development/feeding/sleeping
Specifically ask about social smile, are they moving their eyes to follow things and startling to loud noises?
Talk through what you’re doing and be very reassuring about all the normal findings, try not to give too much detail which might be alarming (“I’m just checking for congenital heart disease” may not go down well!)
Explain about the hip check (“I’m going to check their hips now, sometimes they don’t like this bit very much but it doesn’t hurt them so try and bear with me” or similar)
This is a good opportunity to observe the parent and baby interacting, it’s usually mum who brings them so be aware of PND and ask some screening/open questions to check this out.
Examination
It’s a systematic check but you can do the component parts in any order, as with all paediatric examinations auscultate the heart while they’re settled, before undressing if necessary.
Wash Hands
Observe:
Alertness/dysmorphia/tone when handled by parent/smile/response to noise.
Ears and palms (? dysmorphia/palmar crease)
Check:
Weight, length, head circumference
Heart sounds (ASAP!)
Fontanelle
Eyes red reflex/co-ordinated movement to follow things
Abdomen palpate, check the umbilicus is ok
Head control/tone – Head lag still present but can hold level momentarily in ventral suspension Prone may just transiently lift head off the couch
Mora reflex should be symmetrical
Hips- Barlow=test for dislocatable hip
Ortolani=test for dislocated hip
Nappy off be quick!
Femoral pulses, testis, genitalia (hypospadias)
Nappy back on
Spine dimples/hairy patches and ventral suspension (observing tone again)
wash hands again and check palate
Motor
Hearing does baby respond/ quieten to sound?
Vision eyes can fixate and follow through 90 degrees from midline (when supine)
Socialising baby smiling?
Document findings in the red book and make an appropriate follow up plan if there are any areas you have been unable to assess/findings you are unsure of/definite abnormal findings which require referral.
Reassure parent/carer if all is well and offer further review if they have any concerns.
Kate Eve Bradford VTS
Developmental dysplasia of the hip CDH
6Fs
foetal actors (multiple pregnancies, oligohydramnos, caesarean delivery)
firstborn
female
family history
floppy/hypotonic
feet first (breech)
postural deformities of the feet
asymmetrical leg creases
Barlows test for dislocataBle hip. Hip flexed to 90 degrees and addicted.femoral head is then pushed posteriorly while Inge ally rotating – a dislocataBle hip will clunk as it slips over the rim of the acetabulum.
Ortolanis test for hip that is already dislocated the hips and knees are flexed with examiners middle finger over the greater trochanter and thumb along the medial femur. Pull the hip gently forward while abducting
Barlow’s Backwards
Ortilani’s Outwards
(mnemonics for medical students Khan)
DDH Paediatric Orthopaedics.com
Neonatal screening
newbornbloodspot.screening.nhs.uk
Pulse Oximetry Screening for CHD in neonates Lancet Aug 2011
MCADD
medium chain acylcoenzyme A dehydrogenase deficiency
Rare, life-threatening autosomal recessive condition.
Neonatal jaundice
NICE CG98 Neonatal Jaundice May 10
British Society of Paediatric Gastroenterology Hepatology and Nutrition
Causes for jaundice in infants
physiological jaundice
breast milk jaundice
liver disease
haemolysis
infection
hypothyroidism
Urine and stool colour
urine normally colourless – persistently yellow urine which stains the nappy can be a sign of liver disease
stools normally green or yellow – persistently pale or clay coloured stools may indicate liver disease
If the stools and urine in a jaundiced baby are abnormal in colour, the baby should be referred to paeds immediately
First visit of midwife and/or health visitor
Every baby should be checked for jaundice by looking at the sclera of the eyes
The presence of jaundice in an infant should always be recorded when transferring a baby from the midwife to the health visitor
If the baby is jaundiced, however mild, stools and urine should be checked and seen by either the health visitor and/or midwife
Prolonged jaundice
beyond two weeks in term babies and three weeks in preterm babies (whether or not the baby has pale stools)
if the baby unwell and/or not progressing normally then refer paeds
Assessment
feeding history including whether breast or bottlefed
weight
document stool and urine colour
inform parents of reason for blood tests
Blood tests
serum total bilirubin
split bilirubin – conjugated (direct) bilirubin level and the unconjugated (indirect) bilirubin levels
– in all babies with prolonged jaundice be given a split bilirubin test
– in breastfed babies (an unconjugated hyperbilirubinaemia)
Causes of unconjugated hyperbilirubinaemia
prolonged physiological jaundice
breast milk jaundice
Crigler Najjar Syndrome
haemolysis (red cell breakdown)
If the conjugated bilirubin is >20% of the total bilirubin, the baby should be referred for immediate investigation by a paediatrician
If the conjugated bilirubin is <20% of the total and the total bilirubin is less than 200 micromoles/l, the parent(s)/guardian(s) should be reassured and weekly serum bilirubin levels checked until it returns to normal
Where the total bilirubin is very high (> 200 micromoles/l) and the conjugated fraction is <20%, healthcare professionals are advised to contact a paediatrician.
Other tests
LFTs
albumin
aspartate and alanine transaminases (AST, ALT)
alkaline phosphatase (ALP)
gamma glutamyltransferase (GGT)
blood glucose
coagulation tests
prothrombin time (PT)
partial thrombin time (PPT)
Coagulation may be prolonged secondary to vitamin K deficiency, particularly in breastfed babies not given vitamin K at birth. All babies with suspected liver disease must be given vitamin K orally if INR is normal or intravenous/intramuscular if abnormal
Liver disease in infants
Neonatal rashes
pedclerk.bsd.uchicago.edu Neonatal Skin
stephen-a-christensen.suite101.com/benign skin rashes in infants
Birthmarks in newborns and children
newborns.stanford.edu/Port Wine
newborns.stanford.edu/Slate Grey
Nappy rash
pee-sac
psoriasis
eczema
excoriation – diarrhoea acid stools disaccharide intolerance
seborrhoeic dermatitis
ammonical dermatitis
candidiasis
Red, shiny, wet-looking rash of the skin in the nappy area of babies. Caused by prolonged exposure to urine and faeces. Usually mild and can be treated with a simple skincare:
frequent nappy changes
leaving nappies off for part of the day
and zinc and castor oil cream as a barrier.
anti-candida treatment
- Differential diagnosis
Primary bacterial infections
Impetigo
Perianal streptococcal dermatitis
Infantile seborrhoeic dermatitis
Atopic eczema
Eczema herpeticum
Psoriasis.
Allergic contact dermatitis
Rare causes of nappy rash
Zinc deficiency may present with nappy rash that fails to respond to normal treatments. It is more common in premature infants and is associated with dermatitis around the mouth and erosive lesions of the nails and palmar creases.
Langerhans’ cell histiocytosis commonly presents in the third month of life with persistent intertrigo. Initially small, yellow papules develop which become confluent and subsequently ulcerate.
Bacterial infection — marked redness with exudate, and vesicular and pustular lesions.
Candidal infection — sharply marginated redness around the perianal skin, which may involve the perineum. Confluent zones of papules and pustules involving the skin creases. Satellite lesions are characteristic of candida infection.
Check for oral candidiasis — if present, it increases the likelihood of nappy rash with candidal colonization
Treatments
The area should be cleaned regularly with warm water.
Aqueous cream or similar emollients can be used as a soap substitute.
Soap, talcum powder or perfumed nappy wipes should not be used.
Nappies should be changed as soon as possible after wetting or soiling.
The nappy should remain off for as long as possible each day and allow the baby’s bottom to air dry as much as possible.
Make sure that the baby’s bottom is completely dry before putting on a new nappy.
A water repellent emollient or barrier preparation should be used with each nappy change; a pharmacist can advise about suitable nappy rash creams.
Apply/administer antibiotic medicine as ordered
If disposable nappies are used, choose those that are made with materials that lock wetness inside the nappy and away from the skin.
Advice to reduce exposure to irritants:
Leave nappies off for as long as possible
Consider using nappies with a high absorbency factor
Clean and change the child as soon as possible after wetting or soiling
Use water, or fragrance and alcohol-free baby wipes
Avoid vigorous rubbing after cleaning
Do not use soap, bubble bath, or lotions
Avoid excessive bathing (such as more than twice a day) which can be drying to the skin
Nappy rash Rx
Barrier preparations
Age under 6 years
Zinc oxide ointment BP
Zinc ointment
Apply to the affected area after each nappy change.
Supply 100 grams.
Age: under 6 years
NHS cost: £0.88
Licensed use: yes
Patient information: Change nappies frequently and whenever possible leave the affected area exposed to the air.
Zinc and castor oil ointment BP (contains peanut oil)
Zinc and Castor oil ointment
Apply to the affected area after each nappy change.
Supply 100 grams.
Age: under 6 years
NHS cost: £0.57
Licensed use: yes
Patient information: Change nappies frequently and whenever possible leave the affected area exposed to the air. Tell your doctor if you or your baby are allergic to nuts.
Titanium ointment (Metanium®)
Titanium ointment
Apply to the affected area after each nappy change.
Supply 30 grams.
Age: under 6 years
NHS cost: £2.01
Licensed use: yes
Patient information: Change nappies frequently and whenever possible leave the affected area exposed to the air.
White soft paraffin BP
White soft paraffin solid
Apply to the affected area after each nappy change.
Supply 500 grams.
Age: under 6 years
Licensed use: no – off-label indication
Patient information: Change nappies frequently and whenever possible leave the affected area exposed to the air.
Dexpanthenol 5% ointment (Bepanthen®)
Dexpanthenol 5% ointment
Apply to the affected area after each nappy change.
Supply 30 grams.
Age: under 6 years
NHS cost: £2.1
OTC cost: £3.22
Licensed use: no
Topical imidazole (nappy rash)
Age under 6 years
Clotrimazole 1% cream: apply two to three times a day
Clotrimazole 1% cream
Apply to the affected area 2 to 3 times a day. Continue for at least 2 weeks after the affected area has healed.
Supply 20 grams.
Age: under 6 years
NHS cost: £1.92
OTC cost: £3.38
Licensed use: yes
Econazole 1% cream: apply twice a day
Econazole 1% cream
Apply to the affected area twice a day. Continue for 2 to 3 days after the affected area has healed.
Supply 30 grams.
Age: under 6 years
NHS cost: £2.75
OTC cost: £4.85
Licensed use: yes
Ketoconazole 2% cream: apply once or twice a day
Ketoconazole 2% cream
Apply to the affected area(s) once or twice a day. Continue for a few days after the affected area has healed.
Supply 30 grams.
Age: under 6 years
NHS cost: £3.54
Licensed use: yes
Miconazole 2% cream: apply twice a day
Miconazole 2% cream
Apply to the affected area twice a day. Continue for 10 days after the affected area has healed.
Supply 30 grams.
Age: under 6 years
NHS cost: £1.93
Licensed use: yes
Sulconazole 1% cream: apply once or twice a day
Sulconazole 1% cream
Apply to the affected area once or twice a day. Continue for at least 2 weeks after the affected area has healed.
Supply 30 grams.
Age: under 6 years
NHS cost: £3.9
OTC cost: £6.87
Licensed use: yes
Topical corticosteroid
Age from 1 month to 6 years
Hydrocortisone 0.5% cream
Hydrocortisone 0.5% cream
Apply thinly to the affected area once or twice a day. If there is no improvement after 7 days return to your doctor; if there is an improvement, continue using this cream for up to 14 days.
Supply 15 grams.
Age: from 1 month to 6 years
NHS cost: £2.65
Licensed use: yes
Hydrocortisone 1% cream
Hydrocortisone 1% cream
Apply thinly to the affected area once or twice a day. If there is no improvement after 7 days return to your doctor; if there is an improvement, continue using this cream for up to 14 days.
Supply 15 grams.
Age: from 1 month to 6 years
NHS cost: £2.19
Licensed use: yes
Topical anticandidal + hydrocortisone
Age from 1 month to 6 years
Clotrimazole 1% + hydrocortisone 1% cream
Clotrimazole 1% / Hydrocortisone 1% cream
Apply thinly to the affected area once or twice a day. If there is no improvement after 7 days return to your doctor; if there is an improvement, continue using this cream for up to 14 days.
Supply 30 grams.
Age: from 1 month to 6 years
NHS cost: £2.42
Licensed use: yes
Miconazole 2% + hydrocortisone 1% cream
Miconazole 2% / Hydrocortisone 1% cream
Apply thinly to the affected area once or twice a day. If there is no improvement after 7 days return to your doctor; if there is an improvement, continue using this cream for up to 14 days.
Supply 30 grams.
Age: from 1 month to 6 years
NHS cost: £2.08
Licensed use: yes
Nystaform HC cream (contains nystatin and hydrocortisone 0.5%)
Nystaform HC cream
Apply thinly to the affected area once or twice a day. If there is no improvement after 7 days return to your doctor; if there is an improvement, continue using this cream for up to 14 days.
Supply 30 grams.
Age: from 1 month to 6 years
NHS cost: £2.66
Licensed use: yes
Patient information: Wash hands after applying cream. This cream only needs to be applied thinly. Measure ONE ‘fingertip unit’ by squeezing the cream in a line from the tip of an adult’s index finger to the first crease in the finger. ONE fingertip unit is enough to cover an area that is twice the size of a flat adult hand.
Timodine cream (contains nystatin + hydrocortisone 0.5%)
Timodine cream
Apply thinly to the affected area once or twice a day. If there is no improvement after 7 days return to your doctor; if there is an improvement, continue using this cream for up to 14 days.
Supply 30 grams.
Age: from 1 month to 6 years
NHS cost: £2.38
Licensed use: yes
Oral flucloxacillin (nappy rash)
Age under 1 month
Flucloxacillin oral solution: neonate under 7 days
Flucloxacillin 125mg/5ml oral solution
*WEIGHT REQUIRED* Give 25mg per kg bodyweight TWICE a day for 7 days.
Supply 100 ml.
Age: under 1 month
NHS cost: £2.94
Licensed use: yes
Flucloxacillin oral solution: neonate 7-20 days
Flucloxacillin 125mg/5ml oral solution
*WEIGHT REQUIRED* Give 25mg per kg bodyweight THREE times a day for 7 days.
Supply 100 ml.
Age: under 1 month
NHS cost: £2.94
Licensed use: yes
Flucloxacillin oral solution: neonate 21-28 days
Flucloxacillin 125mg/5ml oral solution
*WEIGHT REQUIRED* Give 25mg per kg bodyweight FOUR times a day for 7 days.
Supply 100 ml.
Age: under 1 month
NHS cost: £2.94
Licensed use: yes
Age from 1 month to 1 year 11 months
Flucloxacillin oral solution: 62.5mg four times a day
Flucloxacillin 125mg/5ml oral solution
Take 2.5ml four times a day for 7 days.
Supply 100 ml.
Age: from 1 month to 1 year 11 months
NHS cost: £5.03
Licensed use: yes
Age from 2 to 6 years
Flucloxacillin oral solution: 125mg four times a day
Flucloxacillin 125mg/5ml oral solution
Take one 5ml spoonful four times a day for 7 days.
Supply 200 ml.
Age: from 2 years to 6 years
NHS cost: £10.06
Licensed use: yes
Penicillin allergy: oral erythromycin or clarithromycin (nappy rash)
Age under 1 month
Erythromycin s/f suspension: 12.5mg/kg four times a day
Erythromycin ethyl succinate 125mg/5ml oral suspension sugar free
*WEIGHT REQUIRED* Give 12.5mg per kg bodyweight FOUR times a day for 7 days.
Supply 100 ml.
Age: under 1 month
NHS cost: £1.71
Licensed use: yes
Clarithromycin suspension: child less than 1 month old
Clarithromycin 125mg/5ml oral suspension
*WEIGHT REQUIRED* Give 7.5mg per kg bodyweight TWICE a day for 7 days.
Supply 70 ml.
Age: under 1 month
NHS cost: £5.58
Licensed use: yes
Age from 1 month to 1 year 11 months
Erythromycin s/f suspension: 125mg four times a day
Erythromycin ethyl succinate 125mg/5ml oral suspension sugar free
Take one 5ml spoonful four times a day for 7 days.
Supply 200 ml.
Age: from 1 month to 1 year 11 months
NHS cost: £5.46
Licensed use: yes
Age from 1 month to 3 years
Clarithromycin suspension: child weighs 7.9kg or less
Clarithromycin 125mg/5ml oral suspension
*WEIGHT REQUIRED* Give 7.5mg per kg bodyweight TWICE a day for 7 days.
Supply 70 ml.
Age: from 1 month to 3 years
NHS cost: £5.58
Licensed use: yes
Age from 1 year to 2 years 11 months
Clarithromycin suspension: child weighs 8kg to 11.9kg
Clarithromycin 125mg/5ml oral suspension
Take 2.5ml twice a day for 7 days.
Supply 70 ml.
Age: from 1 year to 2 years 11 months
NHS cost: £5.58
Licensed use: yes
Age from 2 to 6 years
Erythromycin s/f suspension: 250mg four times a day
Erythromycin ethyl succinate 250mg/5ml oral suspension sugar free
Take one 5ml spoonful four times a day for 7 days.
Supply 200 ml.
Age: from 2 years to 6 years
NHS cost: £5.42
Licensed use: yes
Age from 3 to 6 years
Clarithromycin suspension: child weighs 12kg to 19.9kg
Clarithromycin 125mg/5ml oral suspension
Take one 5ml spoonful twice a day for 7 days.
Supply 70 ml.
Age: from 3 years to 6 years
NHS cost: £5.58
Licensed use: yes
Perianal streptococcal dermatitis
Perianal Streptococcal Dermatitis BMJ
Perianal Streptococcal Dermatitis AAFP Jan 2000
Perianal streptococcal dermatitis Dermnet.nz
Bright red, sharply demarcated rash that is commonly misdiagnosed and treated as a fungal infection.
It occurs most commonly in children 3–4 years of age. It remains unresponsive to treatment with topical steroids and antifungal creams.
Perianal pain and itching are common and blood-streaked stools occur in up to a third of cases.
Cradle cap seborrhoeic dermatitis
hacking-medschool/seborrhoeic-dermatitis
Cradle Cap @ Web MD
Greasy yellow scale + erythema on the scalp and forehead. Nappy areas and limb flexures may also be affected.
Mainly infants under 3 months of age – usually disappears by 12m.
Caused by a disorder in the production of sebum from glands in the skin of the scalp eyebrows, ears, and nasolabial folds.
Unlike atopic eczema, not itchy or painful.
Not contagious nor an indicator of poor care.
If severe or refractory swabbing may help exclude secondary bacterial infection or thrush
Will generally clear on its own with mild emollient therapy such as an emollient bath daily and a light emollient cream +/- antifungal if indicated.
Thick crusts on a baby’s scalp can be removed by soaking them with baby oil for 20-30 minutes every day.
The hairy area of the scalp is then washed with zinc pyrithione shampoo.
Do not to remove adherent scales by picking – as this may result in hair loss or introduce infection
However baby oil can be applied to the scalp and gently massaged in to loosen the scales and encourage them to separate The oil can be left in for 30 minutes to overnight, depending on the severity of the cradle cap
A mild infant shampoo can be used to remove the oil
A soft baby brush can then be used to gently remove the loosened scales
Infant feeding
Feeding problems
mayoclinic.com feeding problems
nationwide childrens.org feeding disorders
Breast feeding (paeds)
Breast feeding babycentre.co.uk
Bottle Feeding
Daily Requirements 150mls/kg in 4-6 feeds (1oz = 30 mls)
dh.gov.uk Guide to bottle feeding
Types of milk
Vitamins for kids
weight loss resources.co.uk children/nutrition/calorie needs
Nice PH 11 Maternal and child nutrition Mar 2008
Infantile colic
A systematic approach to the differential diagnosis and management of infant colic
Working Party – Marks, Archbold, Augstburger, Clayton, Lord, Kanabar, Majid & Morgan
INFANTILE COLIC
Usually beginning ill the first few weeks of life resolving by 4 months
Attacks tend to occur in the early everling when, without any clear reason, the child begins to cry inconsolably, bends the knees and pulls the legs up towards the abdomen, seems to be in pain, and may pass wind.
trial of treatment
– with hypoallergenic formula 2 weeks
– for reflux oesophagitis
Excessive crying vs normal crying- rule of threes
crying/whimpering for at least 3 hours a day
at least 3 days a week,
for a minimum of 3 weeks
By 4 months, most infants’ crying has dropped to a normal level.
GORD infants
Gastro-oesophageal reflux in infants DTB 2009, Vol 47 (12)
childrenshospital.org aug 07/reflux in infants
Weaning
Lactose intolerance / cows milk allergy
Lactose Intolerance NHS choices
cows milk intolerance expert babycentre.co.uk
Primary: due to a physiological decline in lactase concentrations at the time of weaning
Secondary: commonly due to temporary injury to the intestinal mucosa due to infection
Reduced intestinal lactase results in malabsorption of lactose, which is then metabolised by colonic bacteria to produce gas and fatty acids, abdo cramps, bloating, diarrhoea and flatulence
Failure to thrive
Inadequate wt gain and linear growth in infancy
Short stature and growth disorders
- RETARD HEIGHT
Rickets
Endocrine (cretinism, hypopituitarism, Cushing’s)
Turner syndrome
Achondroplasia
Respiratory (suppurative lung disease)
Down syndrome
Hereditary
Environmental (post-radiation, postinfectious)
IUGR
GI (malabsorption)
Heart (congenital heart disease)
Tilted back (scoliosis)
Growth disorders Health Direct au
Crying baby
A babies only way of communicating and usually an expression of unmet need – hunger thirst discomfort or need for more physical contact.
If feeding weight gain and overall health OK parents can be reassured wil settle at 3-4 months.
Hunger
Prem babies may need larger volumes at 2-3 hours
Demand feeding generally preferable to 4 hourly
Sleeping through the night occurs roughly when bay eaches 5kg
Thirst
Increased in pyrexia or hot weather. Offer fluids between feeds if baby remains unsettled.
Colic
Evenings 5-10pm till 3-4m. Baby cries and draws up legs
Wind
Excessive air swallowing may be due to blocked teat or excesive milk secretion in first few minutes.
Try expressing some milk before starting feeding and nursing upright after feeding.
Underfeeding
Overfeeding
Colics
Sleep problems in babies
Sleep problems in childhood
Incidence
about 10% of pre-school children are considered to be poor sleepers by their parents
Aetiology:
Possible causes of childhood sleep disturbance include:
a child may have become “trained to stay awake”
separation anxiety
depression
nightmares
child wakes terrified; remembers the dream
age 8-10 years
night terrrors
child half-wakes terrified; still dreaming; cannot remember the dream when he wakes in the morning
sleep walking
very rare condition
occurs generally between 11-14 years of age
child wakes half-awake and calm; child had no memory of the event on waking the following morning
childhood illness
Management:
A common cause of sleep disturbance in a child is that the child has been “trained to stay awake”. A child may have been ‘rewarded’ for waking or crying at night e.g. with a cuddle, drink or being taken into his parents’ bed.
Methods that might help with “training to sleep” include:
attending to the crying child but limiting the attention to excluding physical problems such as a wet, sodden nappy
not attending to a child as soon as he wakes but instead waiting until he cries. Children will often wake transiently at night
gradually increasing the time a child is left to cry before attending
not providing ‘rewards’ for waking e.g. cuddles, drinks
use of sedative medication (e.g. a sedative antihistamine such as Vallergan (R)) is a last resort used on a short-term basis. Parents should be encouraged to modify their own pattern behaviour so as to encourage good sleeping habits when the sedative medication is withdrawn. Specialist review may be required if the problem persists melatonin may be indicated in the management of childhood sleep disorders
Advice from the book Toddler Taming by Dr Christopher Green
Children with poor sleep patterns have an immense impact on the whole family as well as the child themselves and up to 1/3 of children between the ages of 1-4 wake at least once every night.
Sedatives can be used as a short-term measure, but they don’t solve the problem in the long run and often they can have the side-effects of making the child drowsy the following day or have the paradoxical effect of making them hyperactive. Possible advice that you could give to a parent with a child who has sleep problem to try to train and modify their sleep patters are:-
Follow a regular routine leading up to bedtime and put the child to bed at a consistent time.
Calm them down before bedtime. i.e. don’t wind them up and get them excited such as fighting, chasing, running, playing wild games with them. Instead ease them down by giving them bath, talking to them quietly and gently, tucking them in bed, giving them a cuddle, reading a bed time story.
Once it is time to leave do it decisively, say goodnight and mean it. Don’t rise to any request that have no purpose except to procrastinate e.g. needing a drink, wanting to go to the toilet, for you to lie down with them etc.
If the child gets out of bed, you must return them at once. Be firm, take charge, do it without any questions or fuss. Keep repeating this process each time the child reappears and make sure both parents do the same to show a united front.
Alternatively you can choose to sit quietly at the bedside of the child until they start to fall asleep. Your there to offer your presence, not act as bedtime entertainment. If they lie quietly then you stay, but once they start to climb out of bed or question then leave decisively.
Children who get up in the middle of the night and cry, often do it for attention. It has been shown that in children who wake in the middle of the night where comfort is not readily available, generally decide it is easier to settle themselves back to sleep without making much of a fuss. Dr Green in his book suggests the controlled crying technique as follows:
Decide on a length of time to leave the child crying for before you attend to them and the length of time depends on how tolerant the parent is and how genuinely upset the child becomes. The aim is to not let them get too hysterical or afraid. (on average 5mins, 10mins if tough and 2mins if they’re feeling weak).
After the allotted time has passed then go to the toddler room, lift, cuddle and comfort until the loud upset crying turns to sobs and eventually sniffles. This is the sign to then put them down and walk away. The child may be quite taken aback that the parents has dared to leave and likely will immediately start to cry again in protest. This time leave the child to cry 2mins longer than the last time and repeat the same procedure and continue adding on 2mins and increasing the time you take attend to the child. Follow the same routine each night and after a couple of days to weeks , they should soon notice a different. However, you have to encourage the parents to persevere and be strong in their resolve.
In this method the child knows that the comfort is always there and they are not left to cry for hours in fear alone, but they soon learn that it is not readily available and you won’t rush to their every whimper and demand and that it isn’t worth all the effort.
Abdo pain kids
http://www.patient.co.uk/doctor/Recurrent-Abdominal-Pain-in-Children.htm
Constipation
NICE CG99 2010 Constipation in children and young people
Normal frequency varies 3x day -1 every 3 days
Quantity and frequency of defaecation depend first of all on the
quality and quantity of food and fluid consumed. Food with little
plant-based fibre provides only minimal undigested matter in the
colon, which means the capacity of the intestinal contents to absorb
water is very small. This results in faeces consisting primarily of dead
bacteria, so that, even if enough water is consumed, a small, dry mass
is produced. Because this mass does not expand in the colon, there
are minimal propulsive contractions, and transit is slow.
Normally, the faecal material is retained in the rectum and colon until
sufficient stimuli are present to relax the upper anal sphincter. As
the faeces enter the anal canal, there is an urge to defaecate. In
addition, the external anal sphincter contracts to prevent undesired
evacuation. Defaecation is only possible after this sphincter has been
relaxed consciously.
This normal process can become disrupted due to anatomical,
functional and psychological factors. In childhood, 90% of
constipation is functional. Organic causes are usually discovered
before the child’s third year. The various aetiologies of constipation
vary according to the child’s age.
In infants up to 5 months old, constipation is usually related to the composition of the milk. Breast-feeding can result in relatively
infrequent, hard faeces. Incorrectly prepared bottle formula (too
much milk powder per unit of water) can also lead to constipation,
and small anal fissures may aggravate the situation.
Rare causes – Hirschsprung’s disease and meconium ileus.
Between 2 and 5 months of age a baby may simply have difficulty
evacuating the faeces (its face turns red). The faeces are visible at the
anal opening, but are not easily passed. Incomplete coordination of
the various motor reflexes seems to be the cause. This ‘problem’
disappears spontaneously.
In children of pre-school age, constipation is usually caused by
emotional or behavioural factors, although changes in diet and
potty training may be relevant. Chronic constipation in children
under 2 years of age, a constantly bloated abdomen and an empty
rectum during a digital rectal examination, strongly suggest the
diagnosis of Hirschsprung’s disease. Early diabetes, lead intoxication,
hypercalcaemia and various renal and metabolic disorders can also
be the cause.
In school-age children, constipation usually presents as stomach
ache. Only on inquiry is slow, infrequent defaecation reported.
Peculiar dietary patterns, sometimes involving the entire family,
are often found. Acute painful constipation may also be related to
irritable bowel syndrome (lBS). Extreme cases of faecal soiling and
encopresis, both usually the result of long-term overfilling of the
colon and rectum, require a great deal of attention. The assistance
of a paediatrician and/or a child psychologist may be valuable.
In puberty, most constipation results from an imbalanced diet.
Anorexia nervosa can also playa role at this age: the resistance to
food and the desire to lose weight can lead to minimal food intake,
constipation and laxative use.
Some children may experience pain during defaecation, and the fear of this can cause them to suppress the mge to defaecate, thereby
aggravating the problem. In severe chronic constipation, symptoms may include a lack of
appetite and general malaise. Recurring stomach aches, urinary tract infections or ‘paradoxical’
diarrhoea can also be symptoms of constipation.
TREATMENT
For infants, provide dietary advice: if bottle-feeding, add more water, possibly with a few teaspoons of orange juice or juice from
soaked prunes an alternative is a lactose-rich milk formula; in those on solids, vegetables, h’uit (not too finely chopped) and
brown bread should be encouraged. Children who consume a lot of milk and juice often have less appetite for solid foods with the
necessary fibre.
Bristol stool chart

Stool form scale as a useful guide to intestinal transit time Lewis and Heaton 1997
Encoporesis and soiling
Encoporesis and Soiling PubMed 2009
Encoporesis.com Commercial Site
Gastroenteritis in infants
| Management of feeding during rehydration and maintenance phases | |
|---|---|
| Breast Fed | Continue breast-feeding throughout rehydration and maintenance phase |
| Formula fed | Restart feeding at full strength as soon as rehydration is complete (ideally after 4 hours) |
| Weaned children | Give the child normal fluids and solids after rehydration. Avoid fatty foods or foods high in simple sugar |
Toddlers Diarrhoea PUK
Lactose intolerance PUK
E Coli 157 Common and potentially serious cause of admission with diarrhoea
Rotavirus causes one third of all hospital admissions for diarrhoea and leads to about 600 000
deaths per year / 6% ofdeaths in the under fives. In the UK, 1 in 40 children are admitted to hospital
for rotavirus infection in their first 5 years.
Rotavirus vaccination
Diarrhoea and Vomitting (babies/children)
Gastroenteritis in kids
NICE CG84 Diarrhoea and vomiting in children under 5 Apr 2009
1. Assessment of the state of hydration examine the child to exclude other diagnoses and to provide some indication of the state of hydration.
Remember that a baby who is seriously dehydrated may continue to feed well, so feeding itself should not be used as an indication of well being. Signs of dehydration are not usually present until there is a weight loss of about 3%.
Minimal
(Less than 3%)
MildModerate (3-8%)
Severe
(9% or more)
Decreased skin turgo
Tachycardia
Decreased urine outpu
Mouth dryness
Eye signs (sunkenness)
Level of consciousness
Clinical features
r +/ +++
– +/ + + +
t + + + + + +
+/(moist) + (dry) +++ (very dry)
(normal) + +(sunken) + + + (very sunken & dry)
(well, alert) +/(restless, irritable) + + +(lethargic, unconscious,floppy)
2. Rehydration For those with 3% or more dehydration give oral rehydration solution (eg dioralyte or electrolade) over 4 hours.
Mild to moderate dehydration (3-8% weight loss) 30-80mL/kg in 4 hours
Severe dehydration (weight loss of 9% or more) Refer to hospital immediately (????)
Give fluid little and often. If the child is vomiting, reduce the volume and give the fluid more frequently.
3. Maintenance Once rehydration has been achieved ensure that the child receives their normal fluid requirements. These can be calculated according
to the summative table below. Remember to compensate for ongoing fluid losses, such as watery stools or vomiting, by giving an additional 10mL/kg per vomit or stool.
Fluid requirement per day
First 10kg 100mL/kg
Second 10kg 50mL/kg
Subsequent kg 20mL/kg
For example: A 25kg child would require 1000 + 500 +100 = 1600mL/day
Management of feeding during rehydration and maintenance phases
Breast Fed
Continue breast-feeding throughout rehydration and maintenance phase
Formula fed
Restart feeding at full strength as soon as rehydration is complete(ideally after 4 hours)
Weaned children
Give the child normal fluids and solids after rehydration. Avoid fatty foods or foods high in simple sugar
Remember to advise the parent(s) or carer about what they should do to prevent spread of gastroenteritis (meticulous hand washing and hygiene). In
general, children can go back to school/nursery as soon as they are symptom-free, and have maintained a satisfactory fluid intake, for around 24 hrs.
Stool microscopy/culture – this is necessary when the child
has frank blood in the stool
has recently returned from abroad
has a history suggestive of food poisoning
appears systemically unwell or has severe or prolonged diarrhoea
is taking, or has recently taken, a broad spectrum antibiotic (request Clostridium difficile toxin detection).
Referral advice
Any child who is 9% or more dehydrated, or showing signs of shock, should be transferred to hospital immediately (????).
Children should be transferred to hospital urgently (???) if:
they will not take, or tolerate, sufficient fluids orally to maintain adequate hydration/urine output
they appear systemically unwell
there is a suspicion that the symptoms might be due to a cause other than acute gastroenteritis.
Most children can be managed at home but will need to be re-assessed regularly. Frequency of assessment will depend on the age of the child and
whether losses continue. Warn parents that stools may take several days (sometimes up to two weeks) to return to normal. If diarrhoea recurs once the child has returned to a normal, or near-normal, diet consider lactose or other intolerance, particularly if there is failure to thrive
Diarrhoea and Vomitting Under 5 NICE
Causes include:
1. Tonsillitis and otitis media
2. Intussusception
3. Meningitismay be atypical in infants
4. Pneumonia
5. Urinary tract infection
6. Gastroenteritis
Parents’ history may not be exact and vomiting may be a nonspecific symptom of an ill baby. Hence vital to examine fully every infant with diarrhoea and/or vomiting’
Management
If serious disease suspected, refer
1. If a simple gastroenteritis, assess dehydration from the length of the history, the frequency of the diarrhoea and vomiting, and the signs
2. Signs of dehydration (occur when baby is> 5% dehydrated)
(i) Loss of skin elasticity doughy skin
(ii) Weight loss
(iii) Oliguria, Le. fewer wet nappies
(iv) Tachycardia and tachypnoea
(v) Sunken eyes with no tears
(vi) Sunken fontanelle
(vii) Dry mouth
(viii) Irritability or lethargy
IF THERE ARE SIGNS OF DEHYDRATION, ADMIT
Management of simple gastroenteritis in infants is:
(i) Advice-no milk or solid food for 24-48 h
(ii) Clear fluids to be given-the ideal is a glucose electrolyte solution, e.g. Dioralyte sachets. Advise small sips often-intake should be about one to one-and-a-half times the usual feed volume
(iii) Review the next day, within 24 h. Tell the parents to contact you earlier if the infant refuses all fluid, the vomiting increases, the infant’s condition deteriorates or other complications develop
(iv) On review, if infant still vomiting or signs of dehydration evident, admit. If child improving, continue Dioralyte and then begin, as symptoms settle, to regrade through % strength to Y2 strength and finally to full strength feeds in 1224-h steps according to progress
(v) Recurrence of diarrhoea occasionally due to lactose intolerance-if so try a soya milk, e.g. Wysoy, for a month
(vi) Social circumstances and parental attitudes obviously important in determining management
(vii) A written advice sheet is helpful
(viii) If breast-fed the baby can continue-giving little and often, supplemented with Dioralyte
DIARRHOEA AND VOMITING IN OLDER CHILDREN
Much more likely to be just a simple gastroenteritis rather than a manifestation of other illness, but remember appendicitis
Diarrhoea and vomiting caused by gastroenteritis: diagnosis, assessment and management in children younger than 5 years NICE C
Perform stool microbiological investigations if:
you suspect septicaemia or there is blood and/or mucus in the stool or the child is immunocompromised
Assessing dehydration and shock
Use table below to detect clinical dehydration and shock
Fluid management
In children with gastroenteritis but without clinical dehydration:
continue breastfeeding and other milk feeds
encourage fluid intake
discourage the drinking of fruit juices and carbonated drinks, especially in those at increased risk of dehydration (see below)
offer oral rehydration salt (ORS) solution as supplemental fluid to those at increased risk of dehydration (see below)
In children with clinical dehydration, including hypernatraemic dehydration:
use low-osmolarity ORS solution (240–250 mOsm/l)* for oral rehydration therapy
give 50 ml/kg for fluid deficit replacement over 4 hours as well as maintenance fluid
give the ORS solution frequently and in small amounts
consider supplementation with their usual fluids (including milk feeds or water, but not fruit juices or carbonated drinks) if they refuse to take sufficient quantities of ORS solution and do not have red flag symptoms or signs (see below)
consider giving the ORS solution via a nasogastric tube if they are unable to drink it or if they vomit persistently
monitor the response to oral rehydration therapy by regular clinical assessment
Use intravenous fluid therapy for clinical dehydration if:
shock is suspected or confirmed
a child with red flag symptoms or signs (see table below) shows clinical evidence of deterioration despite oral rehydration therapy
a child persistently vomits the ORS solution, given orally or via a nasogastric tube
If intravenous fluid therapy is required for rehydration (and the child is not hypernatraemic at presentation):
use an isotonic solution, such as 0.9% sodium chloride, or 0.9% sodium chloride with 5% glucose, for both fluid deficit replacement and maintenance
for those who required initial rapid intravenous fluid boluses for suspected or confirmed shock, add 100 ml/kg for fluid deficit replacement to maintenance fluid requirements, and monitor the clinical response
for those who were not shocked at presentation, add 50 ml/kg for fluid deficit replacement to maintenance fluid requirements, and monitor the clinical response
measure plasma Na, K urea, creatinine and glucose at the outset, monitor regularly, and alter the fluid composition or rate of administration if necessary
consider providing intravenous potassium supplementation once the plasma potassium level is known
Nutritional management
After rehydration:
give full-strength milk straight away
reintroduce the child’s usual solid food
avoid giving fruit juices and carbonated drinks until the diarrhoea has stopped
Information and advice for parents and carers
Advise parents, carers and children that:†
washing hands with soap (liquid if possible) in warm running water and careful drying are the most important factors in preventing the spread of gastroenteritis
hands should be washed after going to the toilet (children) or changing nappies (parents/carers) and before preparing, serving or eating food
towels used by infected children should not be shared
children should not attend any school or other childcare facility while they have diarrhoea or vomiting caused by gastroenteritis
children should not go back to their school or other childcare facility until at least 48 hours after the last episode of diarrhoea or vomiting
children should not swim in swimming pools for 2 weeks after the last episode of diarrhoea
Assessing dehydration
These children are at increased risk of dehydration:
children younger than 1 year, especially those younger than 6 months
infants who were of low birth weight
children who have passed six or more diarrhoeal stools in the past 24 hours
children who have vomited three times or more in the past 24 hours
children who have not been offered or have not been able to tolerate supplementary fluids before presentation
infants who have stopped breastfeeding during the illness
children with signs of malnutrition
Symptoms and signs of clinical dehydration and shock
—————————————————————————————————————————————————————-›
No clinically detectable dehydration Clinical dehydration Clinical shock
Symptoms (remote and FTF assessments)
Appears well Appears to be unwell or deteriorating
Alert and responsive irritable, lethargic Decreased LOC
Normal urine output Decreased urine output
Skin colour unchanged Skin colour unchanged Pale or mottled skin
Warm extremities Warm extremities Cold extremities
Signs (remote and FTF assessments)
Alert and responsive irritable, lethargic Decreased level of consciousness
Skin colour unchanged Skin colour unchanged Pale or mottled skin
Warm extremities Warm extremities Cold extremities
Eyes not sunken Sunken eyes
Moist mucous membranes (except after a drink) Dry mucous membranes (except for ‘mouth breather’)
Normal heart rate Tachycardia Tachycardia
Normal breathing pattern Tachypnoea Tachypnoea
Normal peripheral pulses Normal peripheral pulses Weak peripheral pulses
Normal capillary refill time Normal capillary refill time Prolonged capillary refill time
Normal skin turgor Reduced skin turgor
Normal blood pressure Normal blood pressure Hypotension
Umbilical problems
Umbilical hernia
Will usually resolve within first year – 2 years. surgical intervention is not advised before the third year, unless the neck of the hernia is larger than 2 cm at the time of the child’s first birthday, in which case spontaneous closure is very unlikely.
Paraumbilical hernia rarely resolve and will need surgical correction after the age of 2-3 years
Undescended testes
Undescended Testes @ Patient UK
Breast buds
Neonatal vaginal discharge and bleeding
Maternal oestrogens and progestogens from the placenta cross over into the foetal blood system causing development of the foetal endometrium.
Abrupt withdrawal of these hormones after birth causes atrophy and shedding of the mucosa causing a mucus / bloodstained discharge
source GPCSG
Hormonal Effects in Newborns medicine online.com
Pyloric stenosis
<a href=”http://emedicine.medscape.com/article/803489-overview>Pyloric stenosis Medscape
Pyloric Stenosis information for parents GOSH
Intussusception
Circumcision
Enuresis
Failure to voluntarily control micturition. Can be diurnal or nocturnal.
http://guidance.nice.org.uk/CG111
Most children are dry at night by 4 years.
Age % wetting
5 11
10 5
15 2
Ten per cent of 5-year-olds wet their beds.
Treatment is justified after the age of 4 years
History
1. Primary or secondary? Secondary may be emotional or organic
2. Other symptoms, e.g. dysuria, abdominal pain
3. Family history
4. Is the child developing normally, both mentally and physically
5. Family stress
6. Parental expectations
Examination
1. Examine the back and lower limbs for anatomical anomalies or lesions of the lower spinal cord
2. Palpate the abdomen for kidneys and bladder and examine the external genitalia of boys
Tests
MSU and dipstick urine if appropriate
Management
With no anomalies, neuropathic bladder or UTI, the management is:
1. Advice, e.g. lifting the child before going to sleep
2. Star charts, rewarding the child for engaging in pocess not for success! dry nights and reviewing the chart to encourage success
3. Enuresis alarms cure 80% in 6 months and are the treatment of choice. Relapse responds to restarting the alarm. Best for the 6+
age group, as a little frightening at 5 years old.
Health visitors ideally suited to educating parents and following up children with enuresis.
4. Drugs eg desmomelts
UTI in children
NICE CG54 Urinary tract infection in children Aug 2007
Pre and Post-treatment samples essential.
Refer if < 3 months or after first proven urinary tract infection.
| UTI Children | |||
|---|---|---|---|
| Acute Cystitis | E. coli | Trimethoprim | Then treat as per culture. |
| Recurrent cystitis | E. coli | recurring UTI requires prophylaxis as does first attack for children < 1 yr | |
| Pyelonephritis | E. coli | Ceftriaxone | Then oral therapy as per culture. |
Urinary tract infections (UTIs) occur in at least 3% of boys and 5% of girls and account for 5% of fevers in infants and toddlers. In early infancy it is more common in boys but from six months is more common in girls. Re-infection is particularly likely in girls; in boys re-infection is uncommon unless there are severe underlying urinary tract anomalies. If not treated promptly, UTIs can lead to renal scarring which in some patients can result in hypertension, renal failure and complications of pregnancy. A UTI may mimic many of the common childhood illnesses and should be considered in any child with a fever.
Clinical features
In children under 2 years, a UTI may present with non-specific symptoms such as fever, feeding problems, malaise, vomiting, diarrhoea, abdominal
distension, febrile convulsions and failure to thrive.
In a child aged 2-3 years, more specific urinary features may be detected but this is unlikely if the child is still wearing nappies.
Older children may have signs of cystitis or acute pyelonephritis ) but often present with non-specific symptoms as described above.
Assessment
Assess the level of hydration
Look for evidence of sepsis (eg fever, tachycardia and malaise)
Inspect the external genitalia to look for alternative causes of urinary symptoms such as phimosis or perineal soreness
Examine the abdomen to check for suprapubic or loin tenderness and for an enlarged bladder or abdominal mass
Inspect the spine for evidence of dysraphism.
Management
1. Ensure that the parent/carer understands the need to establish whether or not the child has a UTI and the importance of treating it.
2. Collect urine to test for evidence of infection. The best urine samples are clean catch samples’where fresh urine is collected directly into a sterile
container. However, this is sometimes difficult or impossible in a sick infant or toddler. For them, urine can be collected into an adhesive plastic
bag ‘bag sample’ or into a specially designed ‘pad’ which can be placed inside the nappy. Samples from potty-trained toddlers can be collected
successfully from plastic potties thoroughly washed with hot water and washing-up liquid.
3. Use a dipstick to test for the presence of nitrite, leucocyte esterase, blood and/or protein. If any of these are positive send a urine sample for culture.
The sample should be transferred to the lab as soon as possible but can be stored overnight in the fridge at home, or in the surgery, if necessary.
4. If the dipstick test is positive for nitrites and/or leucocytes, or you strongly suspect a UTI, then start an antibiotic such as trimethoprim (4mg/kg twice a day for 5 days). The choice of antibiotic should reflect local sensitivity patterns. Reassess the child in around 48 hours and review the choice on antibiotic depending on the lab results.
5. Any child with a first UTI should undergo further investigation by ultrasound. Those under 5 years old should be given prophylaxis with
trimethoprim (1-2mg/kg) or nitrofurantoin (1mg/kg) at night, until the results of investigation are available and a long-term plan agreed.
Referral advice
Children should be transferred to hospital immediately (????) if they are more than 9% dehydrated (see page 73).
Children should be transferred to hospital urgently (???) if they:
are ‘septic’
have severe vomiting
have evidence of a UTI and are under 6 months old.
Children with recurrent episodes of acute pyelonephritis should be referred to be seen within a month (??).
Children should be referred to a paediatrician (?) if they:
need further investigation that cannot be undertaken in primary care.
This may include ultrasound, dimercaptosuccinic acid (DMSA) scan for children under 5 years, or micturating cystourethrogram (MCUG) in
children under 1 year
have frequently recurring UTIs and/or breakthrough infection while taking prophylaxis
have evidence of underlying renal disease such as an abnormal ultrasound, proteinuria, raised creatinine (adjusted for age) or hypertension.
Obtaining a Urine specimen in young children
InfoPOEMS Posterior Urethral Valves and CKD in Boys
1. Introduction
A urinary tract infection (UTI) occurs when there is infection in any part of the urinary system (kidneys, ureters, bladder or urethra)
Key Issues
Red Flag Warnings
Where an unexplained fever of 38° C is present in an infant or young child consider UTI
Diagnosed renal abnormality
Dysfunctional voiding
History of recurring UTI
Family history of vesicoureteric reflux (VUX) or other renal pathology
Constipation
Poor growth
High blood pressure
Spinal lesion
Enlarged bladder
Abdominal mass
Presenting symptoms may include
Fever
Vomiting
Lethargy
Irritability
Poor feeding history
Failure to thrive
Abdominal pain
Jaundice
Haematuria
Offensive urine odor
Loin tenderness
Frequency
Dysuria
Changes to continence
Loin tenderness
Immediate Care Considerations
Assess airway, breathing and circulation (ABC’s)
Record temperature, heart rate, respiratory rate and capillary refill
Urinalysis
<3 months – 3 years request urgent paediatric evaluation/admission
Paracetamol or ibuprofen for comfort measures (do not administer together but consider use of the alternative medicine if no response to the first)
2. Background Information
A urinary tract infection (UTI) occurs when micro-organisms enter the urinary system.
Urinary tract infections are categorised into two types, upper UTI and lower UTI.
Lower UTI is classified into cystitis where there is inflammation of the bladder or urethritis where there is inflammation of the urethra.
Upper UTI is classified as pyelitis where there is inflammation of the pelvis of the kidney, or pyelonephritis where there is inflammation of both the pelvis of the kidney and the actual kidney itself.
A UTI is considered undifferentiated when it is not possible to determine whether it is upper or lower in origin.
The most common organisms that cause a UTI are;
Escherichia coli
Klebsiella
Proteus mirabilis
Staphylococus saprophyticus
Less common organisms include;
Proteus vulgaris
Enterobacter species
Citrobacter species
Serritica species
Staphylococcus aureus
Rare organisms include;
Candida albicans
Urinary tract infections can occur on more than one occasion and are defined as recurrent when there have been 2 or more episodes of upper UTI; 1 episode of upper UTI plus one or more lower UTI; or 3 or more occurrences of a lower UTI.
UTIs can be a contributing factor in the development of Vesicoururetetic reflux (VUR) or can be diagnosed following a UTI in infants and young children where urine remains static in the bladder creating an ideal medium for bacteria to grow. Primary VUR occurs when;
A infant is born with an impaired valve where the bladder meets the urethra
The ureter has not grown long enough during fetal development
The valve fails to close causing urine to reflux from the bladder to the ureters and eventually to the kidneys
In instances of primary VUR as the child grows and the ureters lengthen the outcomes usually improve with greater valve efficiency.
Secondary VUR occurs when there is a blockage anywhere in the urinary system. In UTI the resulting inflammation causes a blockage and in turn causes reflux of urine to the kidneys.
Symptoms of VUR include
Urinary tract infection
Bedwetting (enuresis)
High blood pressure
Proteinuria
Kidney failure
Clinical features of obstruction to the urinary tract include poor urine flow, fever of uncertain origin, enlarged bladder, abdominal mass, poor growth and high blood pressure. Key features to be noted in the patient medical history and examination are ante-natal diagnosis of any renal abnormality, any spinal, ano-rectal or genitor-urinary abnormality.
Treatment of urinary tract infection is through the administration of antibiotics via a route that can be suitability tolerated by the infant/child.
For most infants and children the prognosis for recovery after antibiotic treatment is excellent. However UTI can reoccur and long term complications include renal scarring, hypertension, renal insufficiency and failure.
If the infant is <3 months old and has a possible UTI a referral to a paediatrician should be made immediately.
3. Investigations
Where an infant or child has possible symptoms of a UTI:
Test urine using clean catch methods (consider urine collection pads/catheter sample if unable to collect via clean catch). If supra pubic aspiration is required an ultra sound must be used to check for presence of urine in the bladder before using this urine collection method.
Dipstick test
i. Leucocyte esterase and nitrates positive: regard as UTI
ii. Leucocyte esterase negative and nitrates positive: commence antibiotics and send for culture
iii. Leucocyte esterase positive and nitrates negative: send urine for cultue, do not commence antibiotics unless good clinical evidence of UTI
iv. Leucocyte esterase and nitrates negative: Not a UTI, explore other potential causes of illness
Send urine for urgent microscopy and culture
If atypical UTI an ultrasound should be performed during the acute stages of the infection to identify whether there are any structural abnormalities
Infants under 3/12 treatment managed by a paediatrician
Children >3 months and older
Upper Urinary tract infection –
Treat with oral antibiotic therapy (Cephalosporin or co-amoxuclave)
If oral antibiotics not tolerated consider intravenous or intramuscular injection if this is not possible.
Lower Urinary tract infection
Use local trust guidelines (consider Trimethoprim, Nitrofurantoin, Cephalosporin) for 3 days
Encourage adequate oral fluid intake in all age groups
To address any dysfunctional elimination syndromes, encourage the child not to delay voiding of urine, for example if delaying due to be involved in play
Management of constipation
Advice re access to clean toilets, personal hygiene after defecation in girls.
Only if the child has had recurrent UTI consider prophylaxis
Ultrasound within first 6 weeks if <6 months old or if there have been recurrent UTI in any age group
| Trimethoprim Doses UTI Kids | |
|---|---|
| Age | Trimethoprim dose |
| 2-5 months | 25mg twice daily for seven days |
| 6m – 5 years | Trimethoprim 50mg twice daily for seven days |
| 6-12 years | Trimethoprim 100mg twice daily for seven days |
RTIs children
NICE CG69 RTIs> NICE CG69 July 08
Sore throat children
hacking-medschool/sore-throat-ent
Organisms
•Viruses: most common
–Adenovirus, influenza, entero-, rhinoviruses, coxsackie, herpes simplex, EBV
•Bacteria
–Group B a-haemolytic Streptococcus
–S. pneumoniae
–Haemophilus influenza
–Moraxella catarrhalis
–Other: N. gonorrhoea, Syphilis, diphtheria, Vincent’s angina
Bacterial tonsillitis
•Group B a-haemolytic streptococcus
–M surface proteins (serotyping), streptolysin O
–Positive cultures + negative ASO= carrier state
•N. gonorrhoea: common in male homosexuals
•Vincent’s angina (trench mouth): Pharyngitis and ulcerative gingivitis: synergistic infection of the anaerobic Fusobacterium fusiformisand the spirochaete Borrelia vincentii
Complications of acute tonsillitis
•Local
–Upper airway obstruction
–Abscess (peritonsillar, parapharyngeal, retropharyngeal)
•General
–Septicaemia
–Meningitis
–Acute rheumatic fever
–Acute glomerulonephritis
Treatment of Acute Bacterial Tonsillitis
•Analgesia
•Penicillin 500 mg qds 1/52
•?steroids: Prednisolone 40mg od 4-5 days
•Local anaesthetic spray/gargles
•If dysphagia to fluids refer to hospital for IV treatment and fluids
Centor score
Tonsils and adenoids
hacking-medschool/tonsillectomy-2
Grommets
Cough in children
Bronchiolitis and viral croup
Viral croup is a disorder of young children that involves shortness of breath, inspiratory stridor and a barking cough resulting from an infection of the mucosa of the larynx and trachea.
The disorder is viralusually the parainfluenza virus, but other causes include influenza A virus, influenza B virus, adenovirus and respiratory syncytial virus.
The interior wall of the larynx swells up, particularly in the mucosal folds just under the vocal cords. Because of the cartilage rings, the swelling can only expand in the lumen of the larynx, and not to the periphery. This narrowing high up in the airway causes the shortness of breath, cough and the often very audible inhalation. Mucus accumulation may also be present, in addition to the inflammation of the mucous membrane. The child’s agitation only serves to make the shortness of breath worse. Viral
croup is usually a harmless disordel: However, rarely, the lumen can become entirely occluded in a relatively short time.
PRESENTATION
There is a typical pattern to the presentation. The GP is often calledin the evening. The parent reports that the child played normally during the day, but had a bit of a cold. The child then went to bed atthe normal time, but after sleeping an hour or more, woke up with shortness of breath and a cough like a seal’s bark. Anyone who has
ever heard this will recognize it easily, even over the phone. Parents who have never heard it before are often very worried.
EPIDEMIOLOGY
Viral croup is a disorder that usually occurs in young children aged 3 months to 3 years. It occurs very occasionally in children of schoolage. The incidence is 0.7-3.5 per 1000 children under 6 years old per year. It is more common in boys than girls. As for the typical seasonal peaks of virus infections, viral croup occurs more often when there is an ‘R’ in the month especially in the autumn.
HISTORY
The GP asks:
when the child began experiencing shortness of breath
if there were symptoms earlier (during the day)
whether the child makes noises when breathing
whether fever is present (there may or may not be fever with viral croup, but it would be unlikely to produce a temperature above 40°C)
whether the child has (previously) had asthmatic symptoms
if there is any possibility of a foreign body.
EXAMINATION
Auscultation usually reveals nothing apart from the conduction of the inspiratory stridor. Rhonchi can be heard if tracheobronchitis is present, in which case the child’s temperature is usually higher. An important differential is epiglottitis. In such a case, the onset is sudden, and the child is older, sicker, paler and calmer than a child
with pseudo-croup. Usually, the child is unable to lie down and (characteristically) drools because he cannot swallow. If epiglottitis is suspected, the throat should not be examined.
TREATMENT
In the first (telephone) contact, the GP recommends that the parents sit with the child in a steamy bathroom or shower. It is important that the child sees the parents are calm agitation will aggravate the problem. The parents usually accept that this will help settle the situation. It is unclear what part of this treatment is the most
effective: the steam or the ‘calm’. If the parents are satisfied with this reassuring advice, the GP asks them to call back to inform him about the child’s progress.
However, if the parents remain anxious, or there is any diagnostic doubt, the GP should arrange to see the child to assess further. In rare cases, viral croup can cause significant airways obstruction, for which hospitalization and even intubation may sometimesbe necessary.
Treatment with steam has not been scientifically evaluated, although it is not harmfuland in daily practice, steaming has often already been started by the parents before they call the GP It is not known if it is in spite of, or thanks to, steaming that less than 5% of children with croup have to be referred to hospital. The effect of treatment with (inhaled) steroids has only been evaluated in selected populations.
The guideline Acute Coughing from the Dutch College of General Practitioners advises, for more severe croup with stridor and tachypnoea, a once-only dose of steroid (e.g. 5 to 10 puffs with fluticasone via a spacer). UPDATE THIS
PREVENTION AND ADDITIONAL INFORMATION
When giving information to the parents, emphasize the good prognosis of viral croup and the value of the most frequently recommended remedies steam and rest.
Key points
Viral croup is a disorder of young children that involves shortness of breath, inspiratory stridor and a barking cough resulting from an infection of the mucosa of the larynx and trachea.
The barking cough is instantly recognizable, even over the phone, but it may worry parents if they have never heard it before.
An important differential diagnosis is epiglottitis.
In rare cases, viral croup can cause significant airways obstruction.
Human metapneumovirus (hMPV), first isolated in 2001, is an important new virus in young children. Over a 25 year period, 20% of children, mean age 12 months, with a lower
respiratory infection tested positive for hMPV It usually presented as bronchiolitis, but also as croup and exacerbations of asthma.
Stridor
(A) Stridor
? inspiratory stridor only (partial airway obstruction at the larynx or above), both inspiratory and
expiratory stridor (partial tracheal obstruction), or expiratory stridor only (partial airway obstruction below
the carina).
? croup?, epiglottitis?, F.B.?, bacterial tracheitis?, peritonsillar abscess?/tonsillitis/pre-existing tonsillar
hypertrophy?, retropharyngeal abscess?, allergic reaction/angioedema? ? all seven may result in upper
airway obstruction. Do not agitate the child, leave them in a position of respiratory comfort.
? Bag and mask with 100% O2 prn.
? Intubation? Use an ET tube 1-2mm smaller than usual prn (with adequate lubricant, e.g. xylocaine jelly).
A small ET tube will suffice, at least temporarily. Consult anesthesia if time permits.
? Epiglottitis?, direct the ET tube through the “eye of the cherry.”
Aspiration of F.B. into tracheal-bronchial system?, esophagus?, unilateral wheezing? ? do bilateral decubitus
expiration views prn, or an upright expiratory film if the patient can cooperate (the side with the F.B. may
demonstrate ar trapping).
(B) Croup
? viral?, bacterial?, spasmodic?
The Gist of Emergency Medicine?
(C) Epiglottitis
? the child is sitting in the “sniffing position” ? toxic, fever, muffled voice, dysphagia/drooling, ± cyanosis.
? L ABC’s, position of respiratory comfort, humidified 100% O2, racemic epinephrine aerosol prn (0.5cc
2.25% with 4.5cc saline/100% O2), portable x-ray?, bag and mask with 100% O2 prn, intubate in the OR
prn, and claforan® 100mg/kg/I.V./day. The patient may require immediate intubation in the ER. The
presence of pharyngitis does not rule out epiglottitis. Bacterial tracheitis presents and is managed similarly
to epiglottitis.
Epiglottitis prophylaxis: L rifampin
? adults 600mg of rifampin bid X 4 days
? 1 month to 12 years of age, 10mg/kg bid X 4 days
? less than 1 month, 5mg/kg bid X 4 days
(D) Retropharyngeal or peritonsillar abscess
? tonsillitis/pre-existing tonsillar hypertrophy?
L ABC’s, position of respiratory comfort, humidified 100% O2 prn, intubate prn, penicillin G 100,000
units/kg/day/I.V., incision and drainage in the OR prn.
gist
ABs in LRTIs in children
1. Pneumonia
Lobar pneumonia Strep. pneumoniae
Haemophilus influenzae
Staph. aureus (< 1 yr) Amoxicillin > 1 year
or co-amoxiclav
< 1 year
Atypical pneumonia Mycoplasma pneumoniae and others Erythromycin (iv) or clarithromycin (oral)
Post-operative aspiration/hospital acquired pneumonia
Strep. pneumoniae
Haemophilus influenzae
Staph, aureus
Anaerobes
Co-amoxiclav
Post-viral pneumonia Staph. aureus
Haemophilus influenzae Co-amoxiclav
2. Bronchitis/Bronchiolitis
Children < 1 year RSV Ribavirin If NPA positive and clinical criteria apply, only on Consultants’ instructions (see Bronchiolitis Protocol 1994)
Exacerbation of cystic fibrosis (bronchiectasis)
Pseudomonas aeruginosa
Staph. aureus
Ceftazidime plus gentamicin Then treat as per culture
Upper Respiratory Tract Infections
Clinical conditions Pathogen(s) Antibiotic(s) Comments
Tonsillitis Virus (75%)
Strep. pyogenes
Nil
Penicillin V Clarithromycin if allergic to penicillin. Avoid amoxicillin or ampicillin. 10 days therapy required to prevent sequelae.
Epiglottitis/acute bacterial tracheitis ALTB Haemophilus influenzae
Staph. aureus Ceftriaxone (for epiglottitis) add flucloxacillin iv for other patients
Acute otitis media Strep. pneumoniae H influenzae Amoxicillin
Mastoiditis As above but wider spectrum of causes Co-amoxiclav
Pertussis B. pertussis Clarithromycin (oral) or erythromycin (iv)
Cough mixtures
NEJM 2009 357;23
Wheezy child – preschool viral wheeze
asthma
viral or bacterial infection
anatomical anomalies (including laryngeal problems),
inhaled foreign body
cystic fibrosis
bronchiolitis
Various entities labelled, e.g. ‘wheezy bronchitic’, but they are largely academic as below the age of 2, where attacks of wheeze
can be brought on by infection, bronchodilators are generally ineffective. A proportion of ‘wheezy bronchitics’ will develop asthma
Consider asthma in the child with recurrent cough, especially nocturnal cough, and in those with dyspnoea on exertion
Preschool Viral Wheeze
THE CHILD WITH A COUGH
Commonly due to simple respiratory tract infections but if persistent think of:
1. Pertussis see chapter on Infectious diseases
2. Asthma
3. Inhaled foreign body
4. Chronic respiratory infection secondary to a postnasal drip from infected sinuses or adenoids
5. Anatomical anomalies
6. Immune disorders
7. Hiatus hernia with gastro-oesophageal reflux
8. Cystic fibrosis-associated with failure to thrive ~ malabsorption
9. Psychogenic cough-a well-recognized entity
Children with a persistent cough or a recurrent cough need therefore a good assessment including a history, chest and ENT examination and, as appropriate, CXR, RAST test, FBC and peak flows. Asthma is very common and a trial of bronchodilator is worthwhile, especially for those with recurrent coughs
Asthma in children
hacking-medschool/acute-asthma-children-under-2
hacking-medschool/acute-asthma-children-over-5
NICE TA10 2000 Inhalers Spacers and Masks in under 5s
asthma.org.uk advice for parents
Cystic fibrosis
Bronchiectasis in children
hacking-medschool/bronchiectasis
Bronchiectasis in Childrenmedscape
Allergies in childhood
NICE CG 116 Feb 11 Food allergies in children
Fighting food allergies among schoolchildren NICE Sep 2011
eGuidelines presentation June 2011 (Phadia)
Pyrexia in Kids – Nice traffic lights
hacking-medschool/child-with-fever-nice-traffic-lights-cg47-2007
Antipyretics in Children
Thermofocus Non-Touch Thermometer
Paracetamol ibuprofen in Kids
hacking-medschool/ibuprofen-paracetamol
Updated advice on paracetamol dosing in children NPC/MeReC Rapid Review Jun 2011
Paracetamol prescribing in primary care: Too little and too much?
Infant paracetamol suspension (120 mg/5ml)
3 – 6 months 2.5 ml Four times
6 – 24 months 5 ml Four times
2 – 4 years 7.5 ml Four times
4 – 6 years 10 ml Four times
Paracetamol six plus suspension (240/250 mg/5ml)
Age Dose How often (in 24 hours)
6 – 8 years 5 ml Four times
8 – 10 years 7.5 ml Four times
10 – 12 years 10 ml Four times
Paracetamol and asthma BMJ 2010;341:c4616
Febrile convulsions
newcastle-hospitals.org.uk febrile-convulsions
Paeds antibiotic doses (emergencies)
hacking-medschool/paeds-ab-doses-infections
hacking-medschool/abs-children
Neonatal conjunctivitis
Neonatal Conjunctivitis Medscape/emedicine
Epilepsy in children
NICE CG20 CG20 Epilepsy in children and young people Mar 2010
Epilepsy Society Epilepsy and you
Headaches and migraine in children
rcgp gps help with school headaches
Faints funny turns in Kids
Breatholding Attacks Sidney Childrens Hospital
Henoch schoenlein purpura HSP
? acute vasculitis of small vessels with frequent multisystem involvement.
? etiology unknown, but believed to result from immune complex reactions to various antigenic stimuli.
? pathognomonic skin lesions ? erythematous progressing to purpuric, predominately on the buttocks and
lower extremities (feet and ankles in adults).
? GI, renal, pulmonary, CNS, and arthritic manifestations.
L ABC’s, supportive care, corticosteroids prn, consult pediatrics.
Haemolytic uraemic syndrome HUS
? usually follows an episode of gastroenteritis or respiratory infection.
? may result from eating undercooked hamburger meat contaminated with E. Coli.
? nephropathy, hemolytic anemia, and thrombocytopenia.
? seizures, hypertension, petechiae, acute renal failure.
L ABC’s and supportive care (e.g. L seizures, hypertension, hyperkalemia/renal failure, anemia,
thrombocytopenia), consult pediatrics, admit ICU prn.
HUS VS TPP
Petechiae in well children
Arch Disease Children 2010;95:518-20
Less than 4 isolaed lesions in a well afebrile child no need to investigate further.
Kawasaki disease (paeds)
250textbooks/kawasaki-disease-2
Childhood murmurs
Congenital heart disease in children
Cyanotic
Acyanotic
VSD
PS
ASD
PDA
Coartation of the aorta
Six S’s of an innocent murmur
Symptom free
Systolic
Split 2nd heart sound
Sternal edge (left) side
Small part of pulmonary area only
Signs otherwise normal
Murmers bhf factfile Oct 2001 pdf
Childhood Murmers
Flow Murmers
ASD
Small VSD
Bicuspid aortic Valve
Venous Hum
VSD
Pulmonary Stenosis
Aortic Stenosis
Mitral Regurgitation
Behavioural problems in toddlers
Is a long way from being a helpless baby to becoming a relatively independent 3 or 4 year old ready to go to play group or nursery. It can be an exciting journey of discovery but it can also seem a very bumpy ride for both you and your child.
As your child moves through his second year he will be wanting to take part in what is going on around him through exploring and playing, watching and imitating others and using his first words. He now feels he is a person in an interesting world of people and he wants to join in.
But he also has to discover all sorts of things he can’t yet do or mustn’t do and feelings that he can’t yet manage by himself without tears or tantrums.
Young children react very differently to the triumphs and set backs of their second and third year and need different kinds of support from their parents.
Some children can’t bear to feel little and helpless. They refuse to accept that there are things they can’t yet manage. Being bossy can be a way of covering this up and trying to make others feel small.
This can be so convincing that sometimes as parents we may come to believe they don’t need us or feel so irritated we want to cut them down to size. But bossy 2 year olds really need someone to offer them love and care even when they don’t seem to want it.
BEING FUSSY…
Many children of 2 or 3 develop all sorts of fads and rituals which they will absolutely insist on.
From a parent’s point of view it can seem silly and tyrannical but how does it look to a small child?
Everyone is expecting her to give up being a baby and become more independent. But she may feel as if the grown-ups are always interfering and bossing her around. When she insists on wearing something strange or doing things in a particular order she may be trying to get others to recognise her choices and preferences. It’s probably helpful to give in gracefully sometimes over things which don’t really matter. That way she will get the chance to learn what it is to back down.
And, of course, there are going to be plenty of times when she wants something impossible or dangerous. So there will still be opportunities for her to learn about “no” and for you to learn to cope with her tears.
‘I’D RATHER BE SMALL’
A child who is clingy and fearful can be very trying in a different way.
As parents we need the reassurance of seeing things move in the right general direction. So babyish’ behaviour is hard to bear because it makes us worry that things are going backwards.
NEW SITUATIONS CAN BE FRIGHTENING
Children of 2 or 3 sometimes feel quite scared about new situations, especially if they think it means being left with other people.
It is worth being truthful about new situations or child minding arrangements so that they don’t feel taken by surprise or tricked.
Allow plenty of time for settling in and a certain amount of fussing. And be prepared to take it seriously if your child really feels he isn’t ready for a new step forward.
BUT SOME OF THE FRIGHTENING THINGS ARE INSIDE HIM
A 2 or 3 year old is having to wage a constant battle with his own passionate wants, hopes and fears. He is still struggling to sort out who he is and what he feels about those who care for him why he loves them one moment and hates then the next.
Far a parent it’s very exhausting not knowing of you’ve got a baby or a big boy on your hands. When you feel you can’t get it right the chances are your child is feeling in a tremendous muddle too.
HAVING WORRIES….
Sometimes fussiness is to do with worries which your child can’t name or tell you about.
Then, his determination to avoid certain objects or situations may be his way of controlling his fears.
What’s worrying him may not have any obvious connection with the things he’s making a fuss about but it’s easier to control what you let your mum put on your plate than to control anxieties you don’t understand.
These sorts of fears tend to come and go but if his behaviour becomes especially difficult it is worth wondering if he’s under some particular stress.
NIGHTMARES
It is at this age that children first complain of bad dreams.
Sometimes the dreams seem to be connected with worrying events which happened during the day but quite often they seem to grow from feelings within the child.
You may never really know what’s troubling him, but it’s very comforting for a child who can’t yet understand himself if he feels that a grown up is trying to do the understanding for him.
TEMPER TANTRUMS
Your child is coping with strong feelings all day long. If he’s managing to keep on a reasonably even keel he’s doing wall but there are bound to be times when he can’t cope.
DOES IT REALLY MATTER IF I SCREAM BACK?”
In the heat of the moment it is easy to become as angry as your child.
As parents we feel helpless, embarrassed or exposed if our children have tantrums if public.
Even at home there are going to be times when they drive us too far.
But children learn by example so if they never see us struggling to cope with our frustration or worry how can they ever learn that is possible to be distressed or angry without throwing a tantrum?
‘SO WHY DOES SHE HAVE TANTRUMS?”
Isn’t she just wanting attention?
When your child throws a temper tantrum what she is doing is showing you what it feels like inside her when she can no longer cope.
She can’t tell you in words. She screams and throws herself around because she feels her big girl self has exploded.
She doesn’t just ask for your help but messes you around with contradictory demands because that’s how helpless and confused she feels.
She is probably scared as well as angry because her rage seems so powerful and dangerous and she has lost her picture of Mum and Dad as helpful or friendly.
She doesn’t need you to come up with a solution or to buy her off with treats (though everyone has done that at times).
She needs to see that you can feel upset and helpless and still take care of both you and go on loving her.
BUT WHAT ABOUT DISCIPLINE?
Firmness is important but so are understanding and tolerance. Simply telling a child to behave better doesn’t give them the strength to control their feelings. They can only learn slowly how to share, wit and accept “no”. And they learn this by example.
This doesn’t mean being perfect parents but it does mean parents who are trying expect more of themselves than their child.
SOME HELPFUL PRACTICAL TIPS
Unless she’s doing something dangerous count to 10 before taking any action at all.
Try not to get drawn into an argument about exactly what started it. She really is beyond reasoning with.
Don’t ask more of her than she can manage.
Coping with her temper doesn’t mean trying to stop her being angry, it means coping with how angry she makes you feel.
Try to avoid saying things just to hurt her backespecially threats of leaving home or having her put away. You may not mean it but she doesn’t know that.
Don’t worry that she’s growing up to be a monster. The temper tantrums of a 2 and 3 year old will start to tail off but only slowly. It will take 2 or 3 years.
Try to remember that through her tempers she’s learning important lessons about herself and both of you are practising for when she’s a teenager!
‘I’M AT THE END OF MY TETHER.’
Sometimes parents feel they are no longer able to keep going. They may become frightened that they will injure their child physically or emotionally.
If you feel this is happening to you for the sake of your child and yourself, you should seek help to sort out what’s wrong.
You may feel you don’t have enough help and support. You may have too many worries on your plate. You may feel depressed or unwell.
Your Health Visitor or GP are probably the best people to talk to first.
They will help you decide whether to seek help from a Social Services Department or Child Guidance Clinic or Hospital Department.
‘BUT MY CHILD’S TEMPERS ARE NOT JUST ORDINARY TANTRUMS.’
Sometimes parents feel that their child’s temper tantrums are not just the sort they will grow out of. Perhaps they feel that their child has never really got going with talking or doesn’t enjoy playing or being with other people. He may be restless and destructive as if he can’t take pleasure in anything. And most painful of all, parents in this situation feel there is a barrier between themselves and their child.
If you have concerns of this sort it is important to seek specialist advice. It is not a good idea to just leave things in the hope that they will sort themselves out.
If you feel you need help, please contact your GP or Health Visitor .
Published by The Child Psychotherapy Trust, 21 Maresfield Gardens, London, NW3 5SH.
Night terrors
Night terrors and nightmares are nightly sleep disturbances that usually occur in childhood. In a night terrolrs the child is incompletely
aroused from deep, slow-wave sleep. The child is not completely awake, and seems confused. He may make random movements with
his arms and legs, does not respond when spoken to, and does not remember anything about the episode the next day. These attacks
rarely last longer than 15 minutes.
Nightmares are frightening dreams that wake the child from sleep, and which are not accompanied by motor agitation. The child is
woken by the dream and can still remember it.
AETIOLOGY/PATHOGENESIS
Night terrors occur due to a sudden arousal from deep (non-REM sleep), generally at the beginning of the night. An episode usually
begins with a loud, penetrating scream, followed immediately by random movements of the arms and legs, and sometimes the entire
body, with the tendency to sit bolt upright in bed. Characteristically, the child will have an intensely frightened facial expression (with
bulging, wide-open eyes), and sometimes heavy perspiration with rapid heartbeat and breathing. After a few minutes, the severity
of the symptoms decreases, but the child remains confused for several minutes before falling asleep again. There is a familial predisposition, possibly in combination with sleepwalking and nocturnal enuresis. Upper respiratory disorders that disrupt sleep can aggravate the problem.
Nightmares are very frightening dreams that wake the patient from REM sleep, usually in the second half of the night. These are
GMC Guidance for dealing with children & Young People
Paediatrics is concerned with patients from 0 to 18 years. Guidance for all doctors can be found at www.gmc-uk.org/.
This is the first publication from the GMC issuing guidance on children. It outlines roles and expectations and may
help in making decisions that are in the best interest of the child/young person, assess capacity and consider consent issues.
Child Protection & Safeguarding Children
Child protection
In 2007 there were 27900 children under a Child Protection Plan (CPP). These
children are on a child protection register because they are at risk of ongoing
abuse. Such abuse could be physical, sexual (this includes contact and noncontact),
neglect and emotional illtreatment.
Following the Victoria Climbie trial there has been renewed effort to keep us
all informed on child protection issues and Working to Safeguard Children was
published. As GPs we are not expected to be trained in forensics, but we should
remain vigilant, keep good records, be prepared to set investigations in motion
through the child protection agency and maintain close contact with other health
professionals and the family. This is often tricky in that, although the welfare of
the child must be placed above all other considerations, usually all members of
the family are under our care and often at the start ofan investigative process you
may be reporting only suspicions.
….Sections missing
