18
Case
Age: 18-year-old man
Reason for referral to ophthalmology: Double vision
Past medical history: None
Past ocular history: None
Medications: None
Habits: Non-smoker and occasional drinker (less than 1 glass per day)
HPI: He was recently admitted to college and made the football team as a wide received. Since the beginning of the season, he noticed that he could only run routes well to the left since he developed double vision when looking to the right. When he sees double, objects are separated vertically and this resolves when he covers either eye. He discussed this with his team physician and a neuro-ophthalmology consultation was requested.
Ophthalmological examination:
Blood pressure: 118/81, heart rate 71
Visual acuity: 20/20 OD, 20/20 OS
Pupils are equal sizes and reactive to light, there was no RAPD
Color vision: 14/14 OD and 14/14 OS correct Ishihara plates
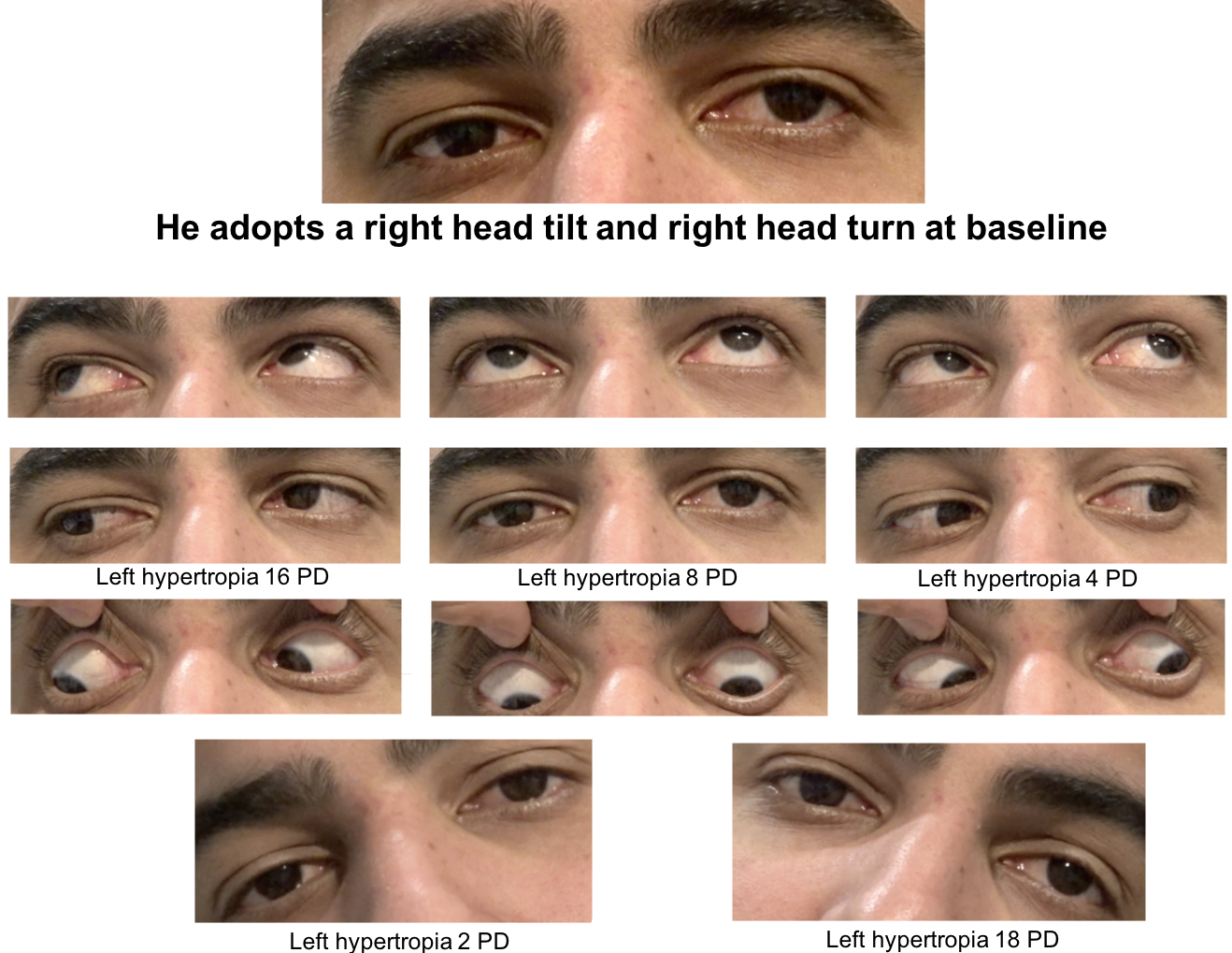
Ocular motility and alignment are shown below
Slit lamp examination is normal
Neurological examination is normal
1. What would the patient see if a Maddox rod was placed over the right eye in primary position?
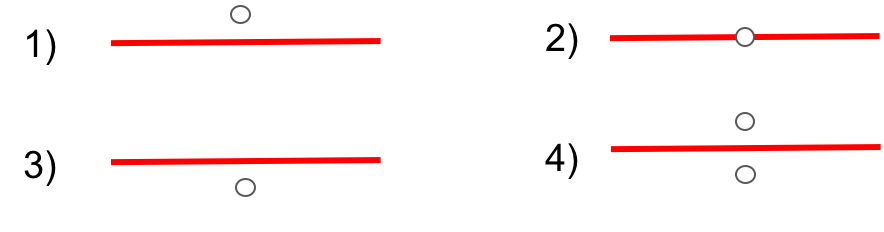
1. What would the patient see if a Maddox rod was placed over the right eye in primary position?
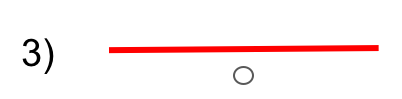
The Maddox rod consists of a series of parallel cylinders that are oriented perpendicularly to the line that the patient sees (the cylinders should be oriented vertically to test a patient with a vertical strabismus). The Maddox rod is typically placed over the right eye and the patient sees a red line with the right eye and a fixation light with the left eye. Since the left eye is at a higher position than the right eye, the light will appear lower than the red horizontal line (remember that the eye that is higher sees an object that is lower and vice versa).
2. What conditions should be considered in the differential diagnosis of vertical binocular diplopia?
- 3rd nerve palsy
- 4th nerve palsy
- Thyroid eye disease
- Ocular myasthenia gravis
- Skew deviation
- All of the above
2. What conditions should be considered in the differential diagnosis of vertical binocular diplopia? 6. All of the above
In a patient with vertical binocular diplopia the differential diagnosis includes a 3rd nerve palsy, 4th nerve palsy, thyroid eye disease, ocular myasthenia gravis, skew deviation, Brown syndrome, and degenerative changes in the orbit such as that seen in heavy eye syndrome and sagging eye syndrome. The presence of other signs such as a head tilt, ptosis, proptosis, fatigability, and nystagmus can help in differentiating these conditions.
3. What is the primary action of the superior oblique muscle?
- Depression
- Elevation
- Incyclotorsion
- Excyclotorsion
3. What is the primary action of the superior oblique muscle? 3. Incyclotorsion
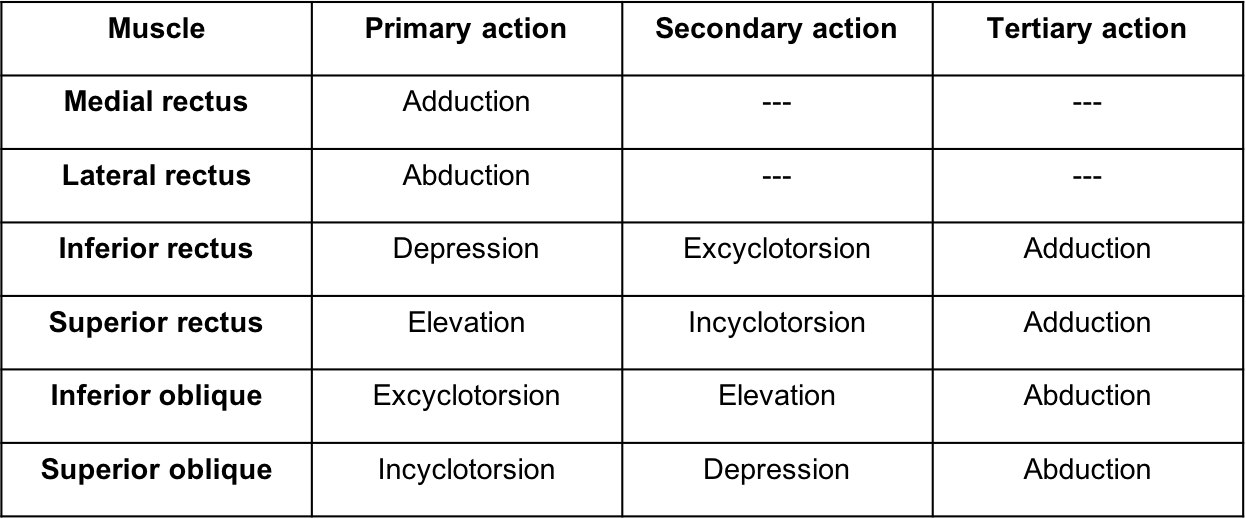
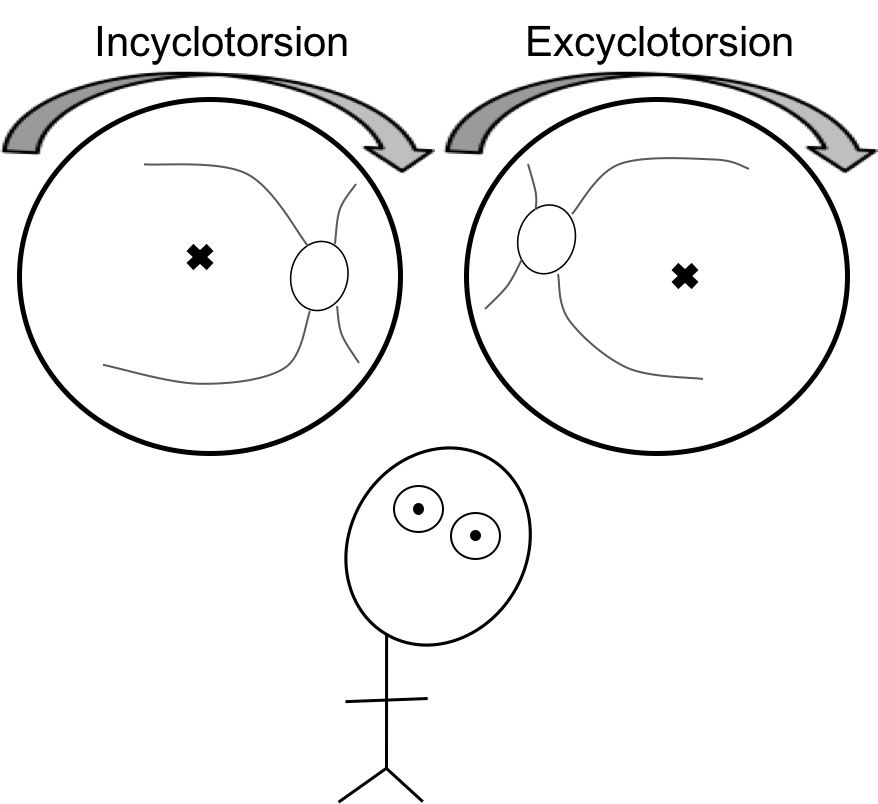
Because the oblique muscles are inclined 51 degrees to the visual axis, their primary action is torsion. The primary action of the superior oblique is incyclotorsion (rotation of the superior pole of the eye towards the nose) and the primary action of the inferior oblique is excylotorsion (rotation of the superior pole of the eye towards the ear). The actions of the extraocular muscles are summarized below.
4. What is the most likely diagnosis in this patient?
- Left 3rd nerve palsy
- Left 4th nerve palsy
- Left 6th nerve palsy
- Orbital bone fracture with entrapment
4. What is the most likely diagnosis in this patient? 2. Left 4th nerve palsy
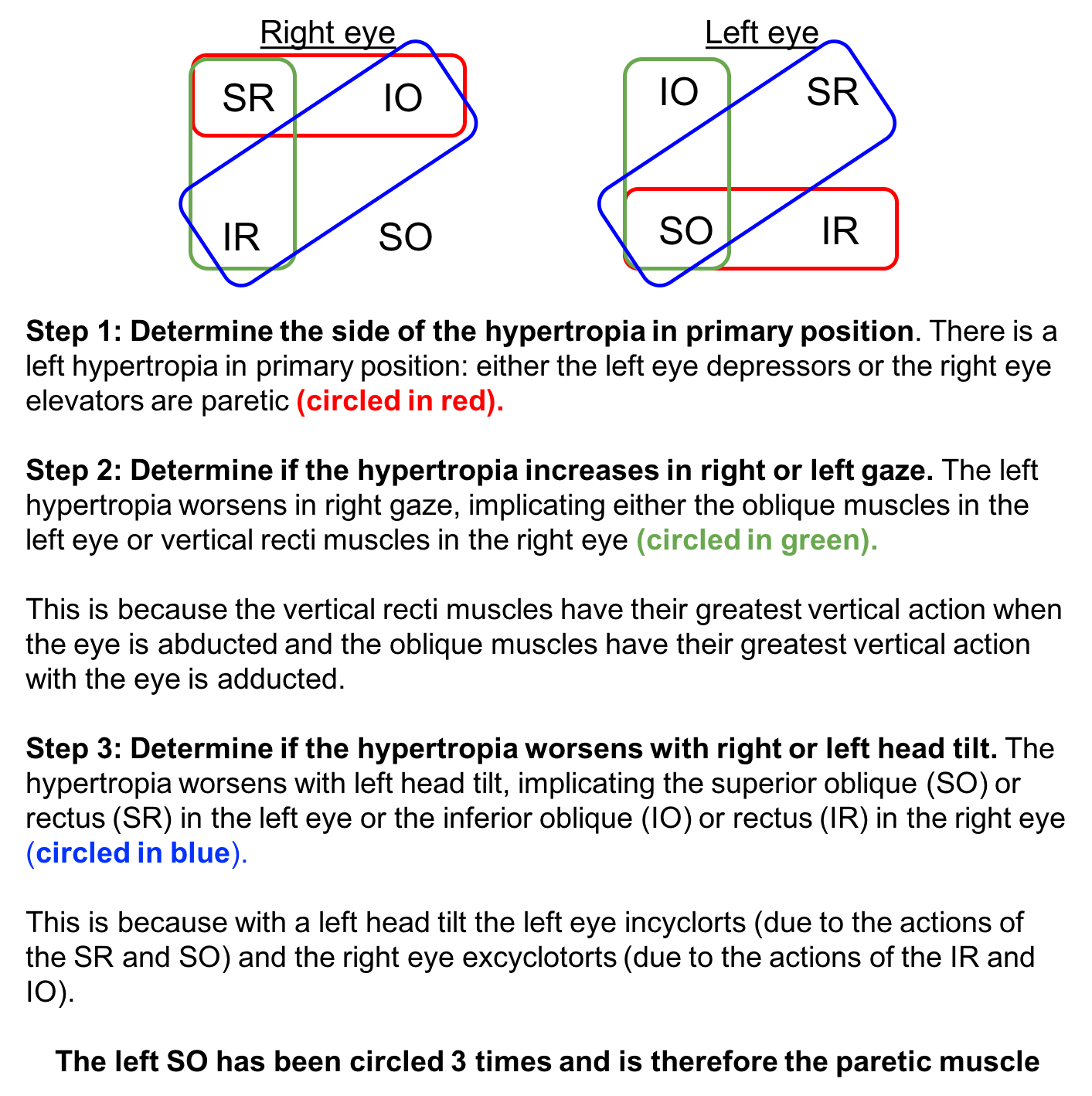
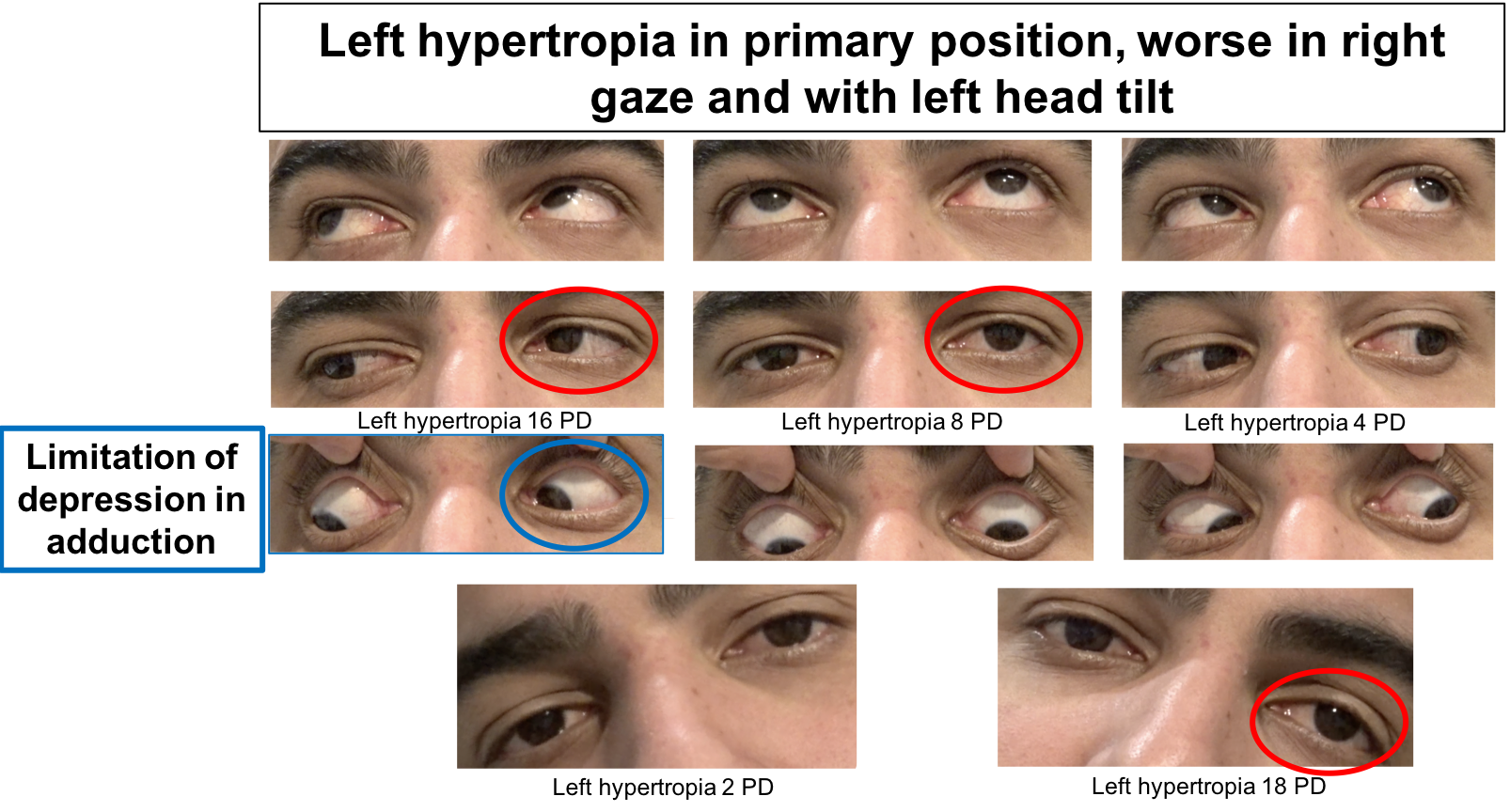
The patient has a left hypertropia that follows the Parks-Bielschowsky three-step test that is used in the diagnosis of 4th nerve palsies. The Parks-Bielschowsky three-step test is demonstrated below. A left 4th nerve palsy will cause a left hypertropia in primary position that increases on right gaze and left head tilt. You can also see that he has limitation of depression in adduction, which is seen in 4th nerve palsies since the maximal depression caused by the superior oblique occurs in adduction.
Clinical Pearl
A left 4th nerve palsy will have a:
-
- Left hypertropia in primary position
- Left hypertropia worse in right gaze
- Left hypertropia worse with left head tilt
*Remember left-right-left for a left 4th nerve palsy
5. Why does the hypertropia increase with left head tilt?
- Compensatory activation of the left superior rectus
- Excess incyclotorsion by the left superior oblique muscle
- Compensatory activation of the left inferior oblique muscle
- Excess incyclotorsion of the right superior oblique muscle
5. Why does the hypertropia increase in left head tilt? 1. Compensatory activation of the left superior rectus
When the patient tilts his head to the left, the left eye normally incyclotorts and the right eye excyclotorts. The incyclotorters of the left eye are the superior oblique (primary action) and the superior rectus (secondary action). Since the left superior oblique is paretic, the superior rectus compensates, but also elevates the eye since this is its primary action.
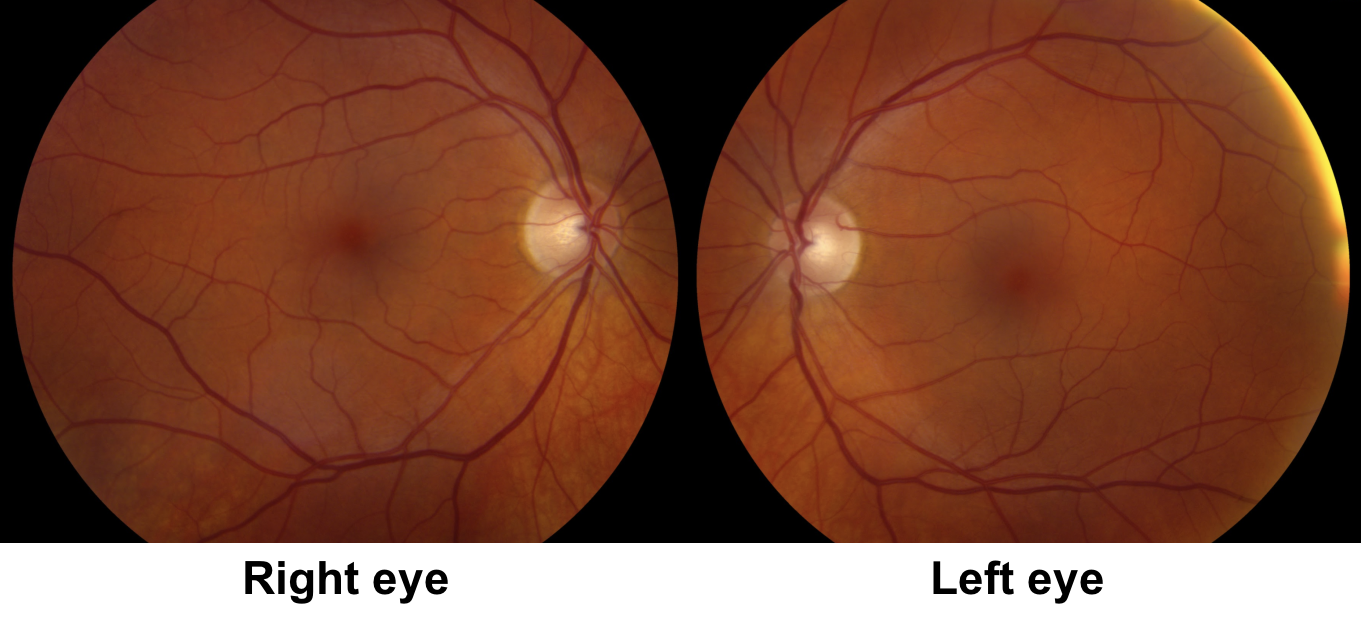
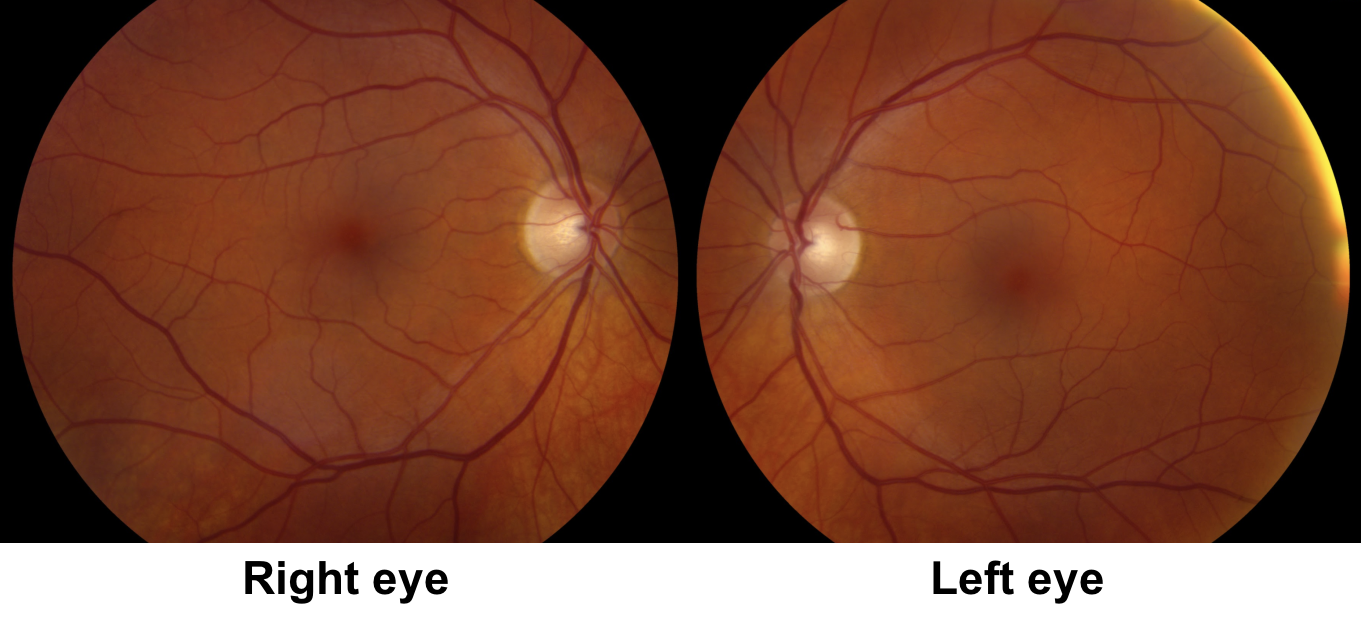
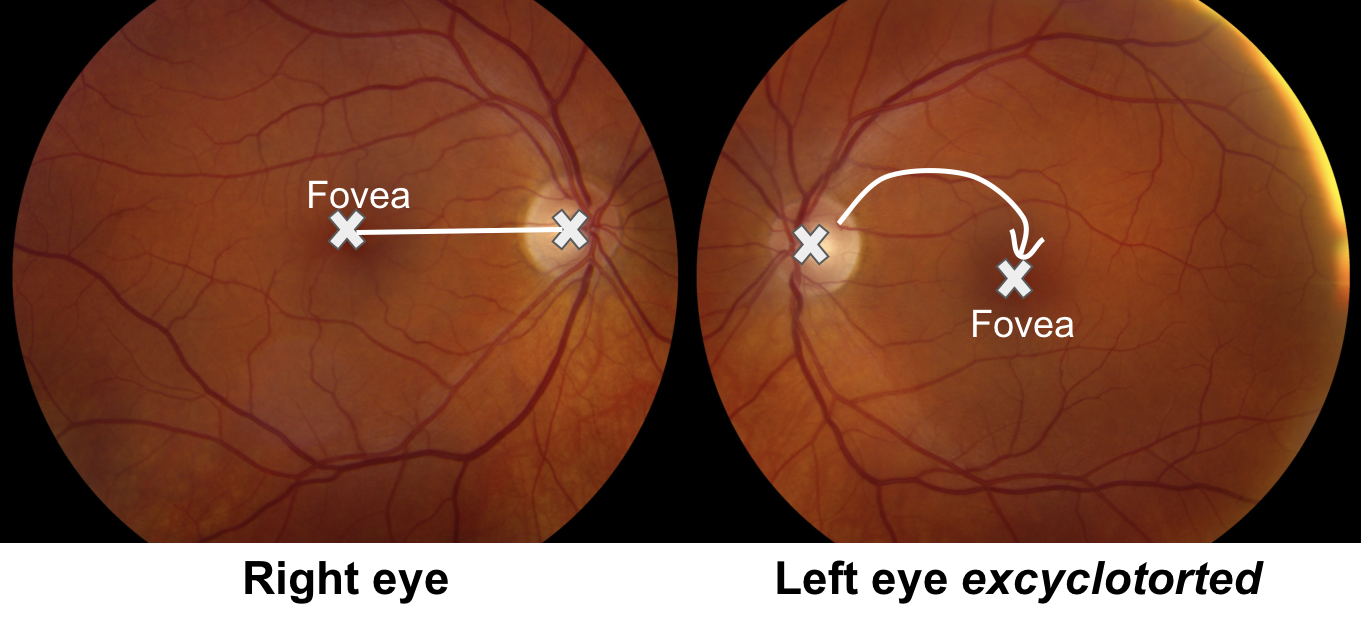
6. What is the most pertinent finding in this patient’s fundus photos?
- Left fundus is incyclotorted
- Left fundus is excyclotorted
- Left fundus has more tortuous vessels
- Left fundus has choroidal folds
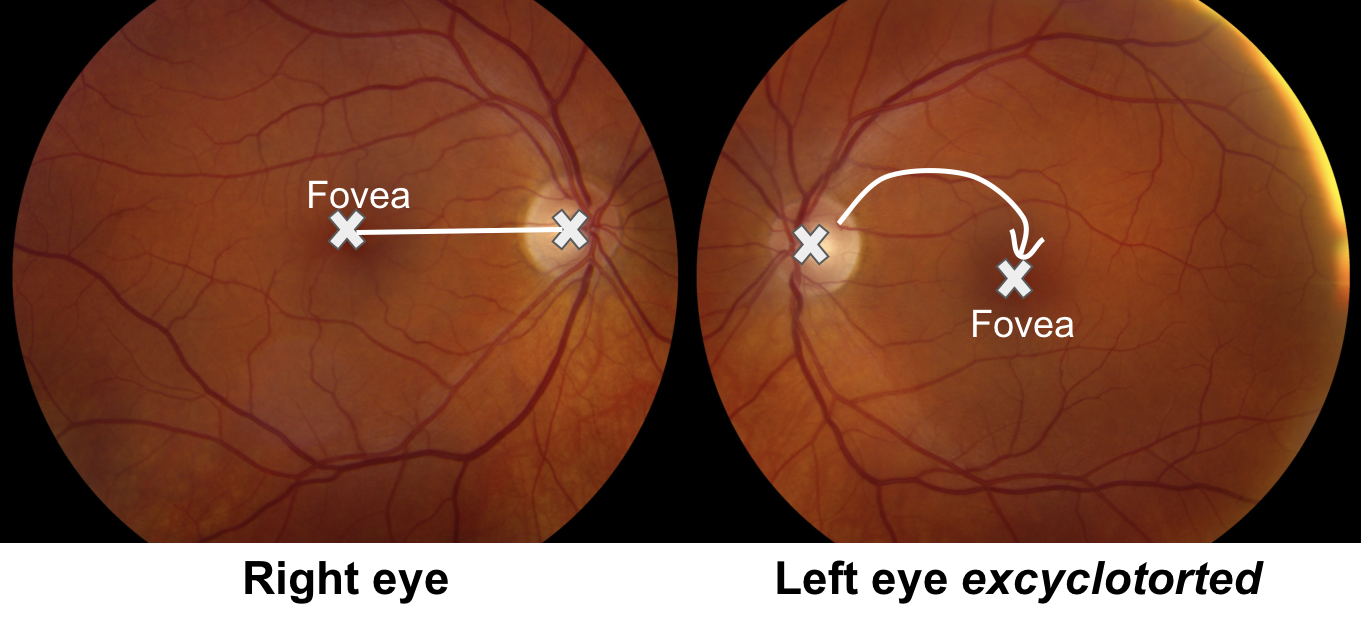
6. What is the most pertinent finding in the fundus photos? 2. Left fundus is excyclotorted
Since the primary action of the superior oblique muscle is incyclotorsion, the left fundus should appear excylotorted since the superior oblique muscle is paretic. An excylotorted fundus can be assessed by judging the position of the optic disc in relation to the foveal center. The fovea is normally just slightly lower than the middle of the optic disc by about 6 degrees. In an incyclotorted fundus, the fovea will be at a higher position compared to the middle of the optic disc and in an excyclotorted fundus, the fovea will be at a lower position compared to the middle of the optic disc. This patient has a left excyclotorted fundus consistent with his left 4th nerve palsy.
7. How do you assess for a 4th nerve palsy in the presence of a complete 3rd nerve palsy?
-
- It cannot be assessed
- Assessing for torsion of the eye during depression in abduction
- Assessing the position of the eyelid
- Assessing for eyelid retraction
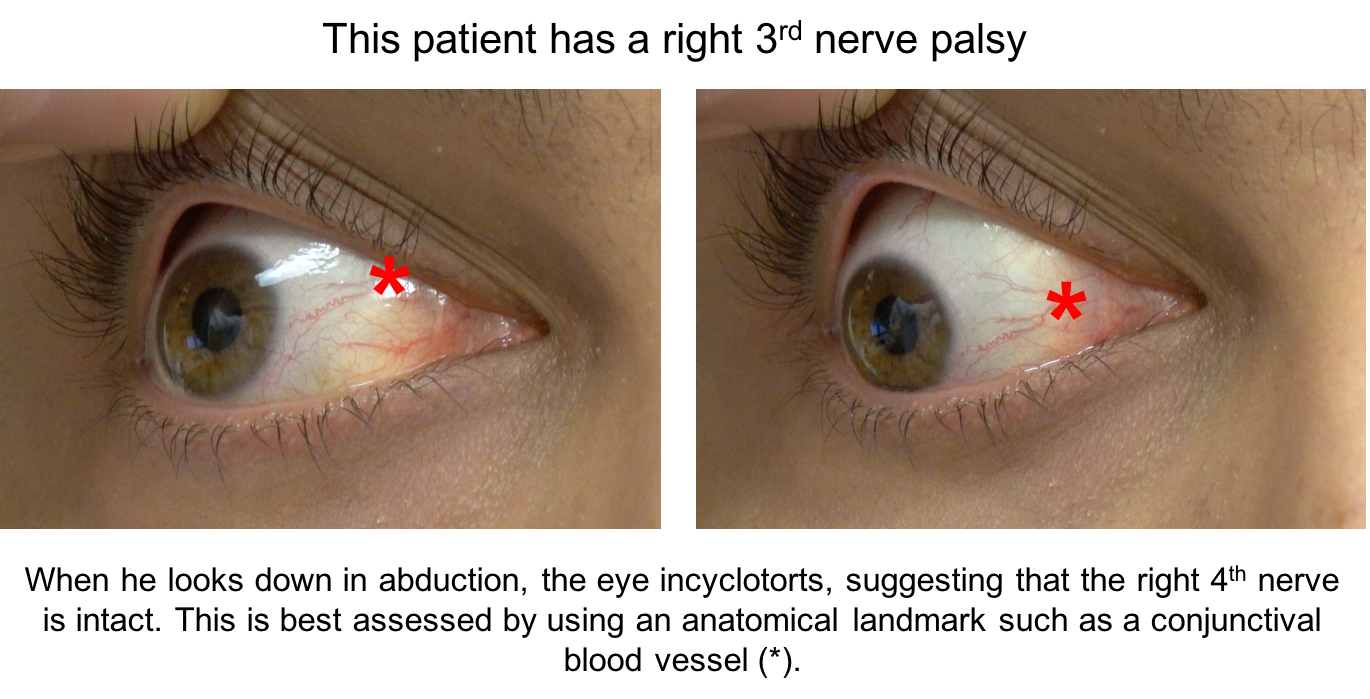
7. How do you assess for a 4th nerve palsy in the presence of a complete 3rd nerve palsy? 2. Assessing for torsion of the eye during depression in abduction
A 4th nerve palsy may occur in conjunction with a 3rd nerve palsy since the 3rd and 4th nerves are in close anatomical proximity in the cavernous sinus. Since the eye cannot adduct in a 3rd nerve palsy, the limitation of depression in adduction that is normally seen in a 4th nerve palsy cannot be assessed. The patient should be asked to abduct the eye and look down, if there is incyclorsion of the eye when looking down, then the 4th nerve is intact. Incyclotorsion can be assessed by using an anatomical landmark such as a conjunctival blood vessel.
8. How can you differentiate a congenital decompensated 4th nerve palsy from an acquired etiology?
- Look for incyclotorsion of the fundus
- Parks-Bielschowsky three-step test
- Vertical fusional amplitudes
- Fatigability
8. How can you differentiate a congenital decompensated 4th nerve palsy from an acquired etiology? 3. Vertical fusional amplitudes
The most common cause of a 4th nerve palsy is congenital; other common causes are trauma and microvascular ischemia. Congenital 4th nerve palsies may decompensate with minor head trauma or without any antecedent event. Signs of a congenital 4th nerve palsy include facial asymmetry, a head tilt seen on old photographs, lack of subjective excylotorsion, and large vertical fusional amplitudes. Normal vertical fusional amplitudes are small, around 1-2 prism diopters, but patients with congenital 4th nerve palsies may have vertical fusional amplitudes up to 10-25 prism diopters. It has also recently been suggested that congenital 4th nerve palsies have a hypertropia greater in upgaze than downgaze or equal in upgaze and downgaze.
Clinical Pearl
Signs suggestive of a congenital 4th nerve palsy:
-
- Longstanding head tilt
- Large vertical fusional amplitudes (> 2 PD)
- Facial asymmetry
9. How can you differentiate a bilateral from unilateral 4th nerve palsy?
- Cannot be differentiated
- History of trauma
- MRI of the brain with contrast
- Double Maddox rod testing
9. How can you differentiate a bilateral from unilateral 4th nerve palsy? 4. Double Maddox rod testing
Bilateral 4th nerve palsies should be considered whenever a unilateral 4th nerve palsy is diagnosed. Patients with bilateral 4th nerve palsies have a crossed hypertropia (right eye higher on left gaze and left eye higher on right gaze), excyclotorsion of 10o or greater that is best measured with a double Maddox rod, and a large V-pattern esotropia (> 25 prism diopters), which may cause a habitual chin-down position.
10. Why is there a large V-pattern esotropia seen in patients with bilateral 4th nerve palsies?
- Tertiary action of the superior oblique is abduction, which is limited
- Tertiary action of the superior oblique is depression, which is limited
- Tertiary action of the inferior oblique is depression, which is overactive
- Tertiary action of the inferior oblique is abduction, which is limited
10. Why is there a large V-pattern esotropia seen in patients with bilateral 4th nerve palsies? 1. Tertiary action of the superior oblique is abduction, which is limited
A V-pattern means that the eyes are closer together in downgaze compared to upgaze. The superior oblique depresses the eye maximally in downgaze and its tertiary action is abduction (remember oBliques aBduct). Since both superior oblique muscles are paretic in bilateral 4th nerve palsies, there is less abduction in downgaze and the eyes are closer together, leading to a V-pattern.
11. A patient has a small bleed in the midbrain in the region of the right 4th nerve nucleus. This will manifest as a:
- Right 4th nerve palsy
- Left 4th nerve palsy
- Bilateral 4th nerve palsy
- Right 6th nerve palsy
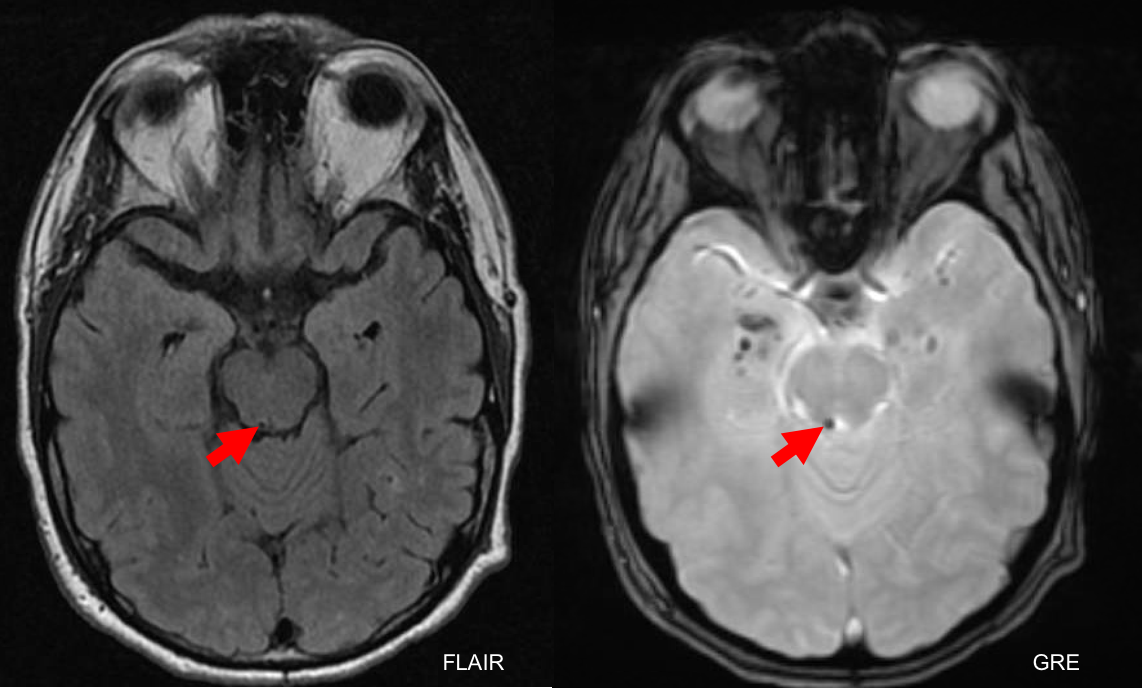
11. A patient has a small bleed in the midbrain in the region of the right 4th nerve nucleus. This will manifest as a: 2. Left 4th nerve palsy
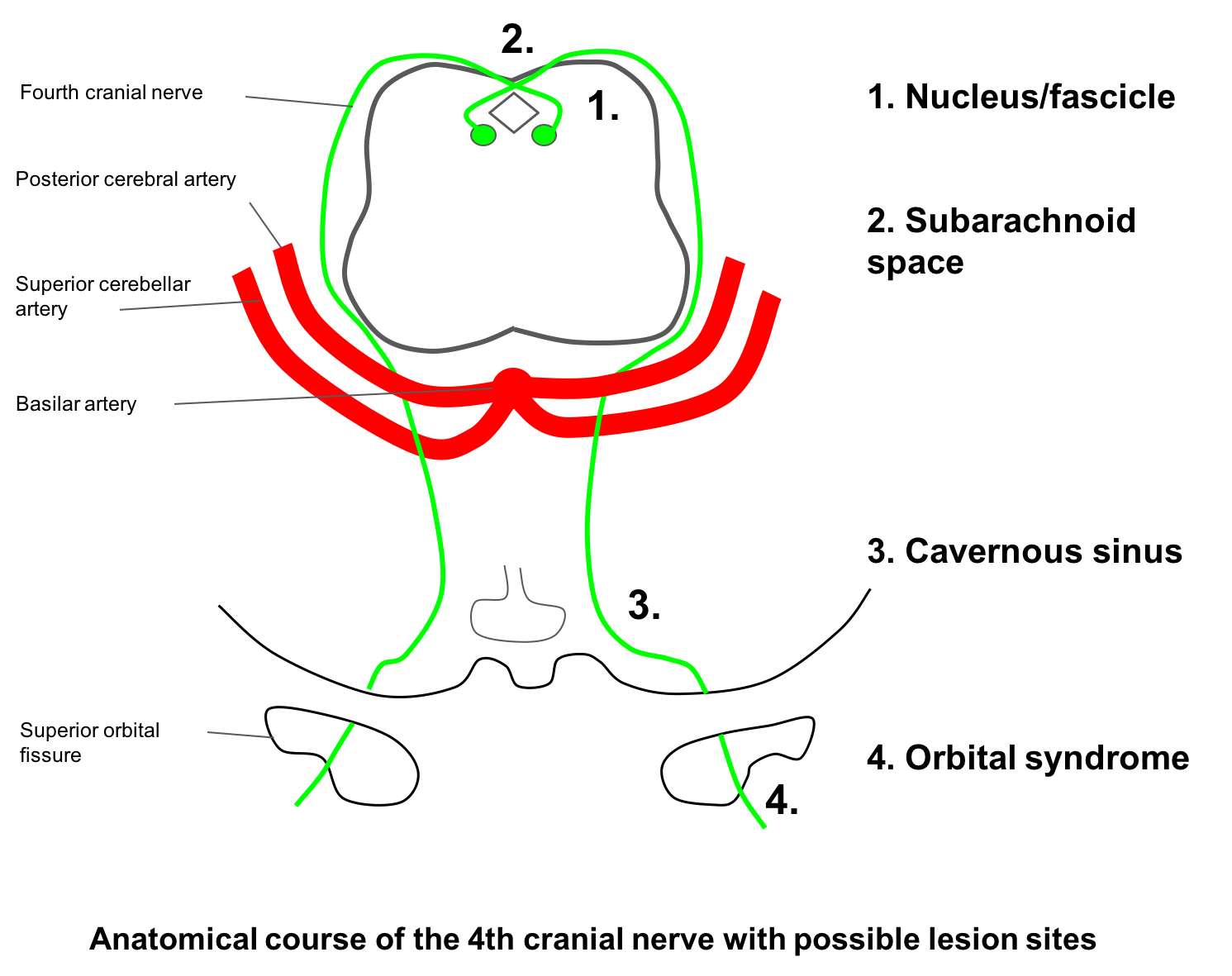
The 4th cranial nerve nucleus is located in the midbrain at the level of the inferior colliculus and the 4th nerve exits the brainstem dorsally and innervates the contralateral superior oblique muscle. Because the 4th nerve fascicle travels a very short distance before exiting the brainstem, it is very difficult to differentiate a nuclear and fascicular lesion. The course of the 4th cranial nerve is illustrated in the diagram below.
12. What additional finding on examination suggests damage to the 4th nerve fascicle in the midbrain?
- Ipsilateral homonymous hemianopia
- Tortuous retinal venules
- Contralateral Horner’s syndrome
- Tonic pupil
12. What additional finding on examination suggests damage to the 4th nerve fascicle in the midbrain? 3. Contralateral Horner’s syndrome
The descending sympathetic tracts are in close proximity to the 4th nerve nucleus and fascicle and therefore a lesion involving the 4th nerve nucleus or its fascicle before decussation in the anterior medullary velum may also affect descending sympathetic fibers and cause a Horner’s syndrome. Since the descending sympathetic fibers do not cross, the Horner’s syndrome will be ipsilateral to the lesion and the 4th nerve palsy will be contralateral.
13. What physiologic adaptation would you expect to see if a normal individual was rotated to the left (in the roll plane) as shown below:
- Left eye incyclotorsion
- Right eye excyclotorsion
- Left eye upward rotation
- Right head tilt
- All of the above
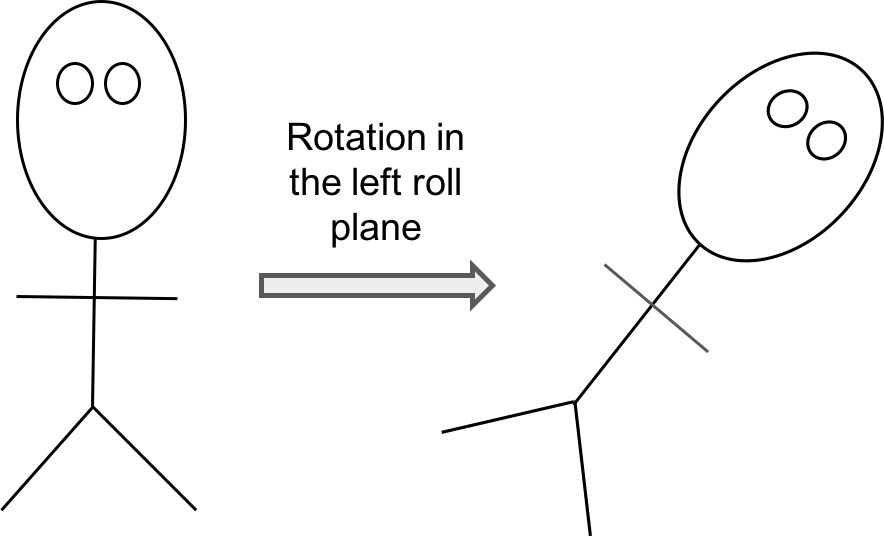
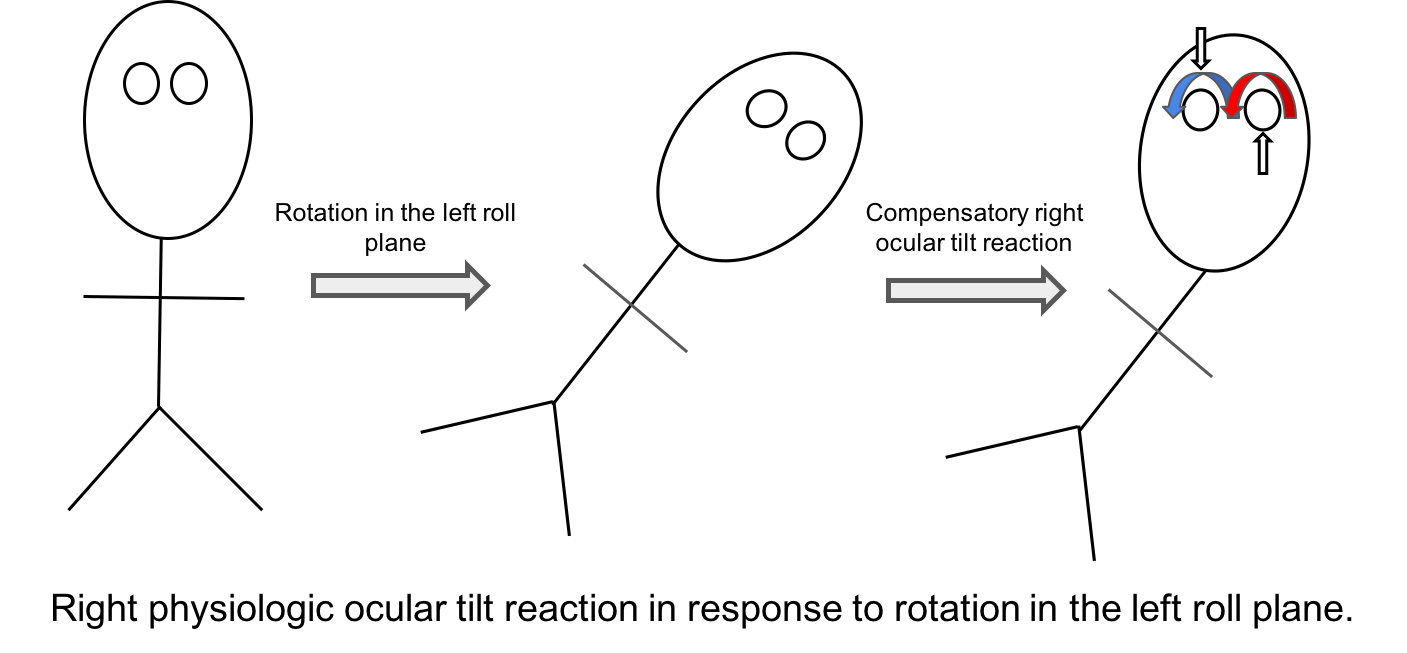
13. What physiologic adaptation would you expect to see if a normal individual was rotated to the left (in the roll plane) as shown below: 5. All of the above
The vestibulocular system receives input from the semi-circular canals and otoliths and plays an important role in maintaining eye position and fixation in response to changes in body position. When this individual is rolled to the left, a right compensatory ocular tilt reaction is initiated: there is incyclotorsion of the left eye, excylotorsion of the right eye, a right head tilt, an upward rotation of the left eye and a downward rotation of the right eye. This is an adaptive mechanism to realign the visual axis with the gravitation vertical plane.
Clinical Pearl
An ocular tilt reaction consists of:
-
- Head tilt
- Ocular torsion
- Skew deviation
14. A patient presents with a left head tilt and has a right hypertropia in primary position. Dilated fundus examination shows right eye incyclotorsion and left eye excyclotorsion. What is the diagnosis?
- Pathologic ocular tilt reaction
- Right 4th nerve palsy
- Left 3rd nerve palsy
- Thyroid eye disease
14. A patient presents with a left head tilt and has a right hypertropia in primary position. Dilated fundus examination shows right eye incyclotorsion and left eye excyclotorsion. What is the diagnosis? 1. Pathologic ocular tilt reaction
A pathologic ocular tilt reaction is caused by a lesion in the vestibular pathways and results in asymmetric vestibular input to the central nervous system and mimics a change in body position in the roll plane. This patient is acting as if her body was rolled to the right and has a left ocular tilt reaction. Note that the hypertropic eye is incyclotorted in this case, whereas it would be expected to be excyclotorted in a 4th nerve palsy (since the superior oblique muscle is an incyclotorter).
Clinical Pearl
The hypertropic eye is excyclotorted in a 4th nerve palsy and incyclotorted in a skew deviation.
15. What other signs may help differentiate a skew deviation from a 4th nerve palsy?
- Presence of nystagmus
- Presence of an internuclear ophthalmoplegia
- Cerebellar findings
- All of the above
15. What other signs may help differentiate a skew deviation from a 4th nerve palsy? 4. All of the above
Sometimes a skew deviation mimics a 4th nerve palsy and it can be difficult to differentiate the two conditions. A skew deviation may also have other associated neurological signs such as gaze-evoked nystagmus, gaze palsy, Horner’s syndrome, or cerebellar signs. Since the utrical pathway synapses in the vestibular nuclei, then crosses the midline and ascends in the medial longitudinal fasciculus to the vertically acting oculomotor and trochlear nuclei, an internuclear ophthalmoplegia may also be seen in a patient with a skew deviation.
Case Summary
He has had longstanding vertical binocular diplopia when looking to the right. He was found to have a left hypertropia that followed the Parks-Bielschowsky three-step test, implicating the left superior oblique muscle. There was limited depression of the left eye in adduction and the left fundus was excyclotorted, confirming the diagnosis of a 4th nerve palsy. He was found to have a longstanding right head tilt on old photographs and had an enlarged vertical fusional amplitude of 12 PD, consistent with a left congenital 4th nerve palsy. He was treated with prism glasses and his double vision essentially resolved.
Further reading:
-
Peragallo JH, Pineles SL, Demer JL. Recent advances clarifying the etiologies of strabismus. J Neuroophthalmol 2015;35(2):185-193. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4437883/
-
Guy J, Day AL, Mickel JP, Schatz NJ. Contralateral trochlear nerve paresis and ipsilateral Horner’s syndrome. Am J Ophthalmol 1989;107(1):73-76. https://www.ncbi.nlm.nih.gov/pubmed/2912120
-
Brodsky MC, Donahue SP, Vaphiades M, Brandt T. Skew deviation revisited. Surv Ophthalmol 2006;21(2):105-128. https://www.ncbi.nlm.nih.gov/pubmed/16500212