10
Case
Age: 45-year-old white woman
Reason for referral to ophthalmology: Unilateral optic disc edema
Past medical history: None
Past ocular history: None
Medications: None
Habits: Non-smoker and does not drink alcohol
HPI: She went to see an optometrist for a routine eye exam. She was found to have slightly reduced visual acuity and optic disc edema in the right eye. An urgent ophthalmology consultation was requested. She is asymptomatic.
Ophthalmological examination:
Blood pressure: 118/80, heart rate 74
Visual acuity: 20/30 OD, 20/20 OS
Pupils are equal sizes and reactive to light, there is no RAPD
Color vision: 14/14 OD and 14/14 OS correct Ishihara plates
Ocular motility and alignment are normal
Slit lamp examination is normal
Neurological examination is normal
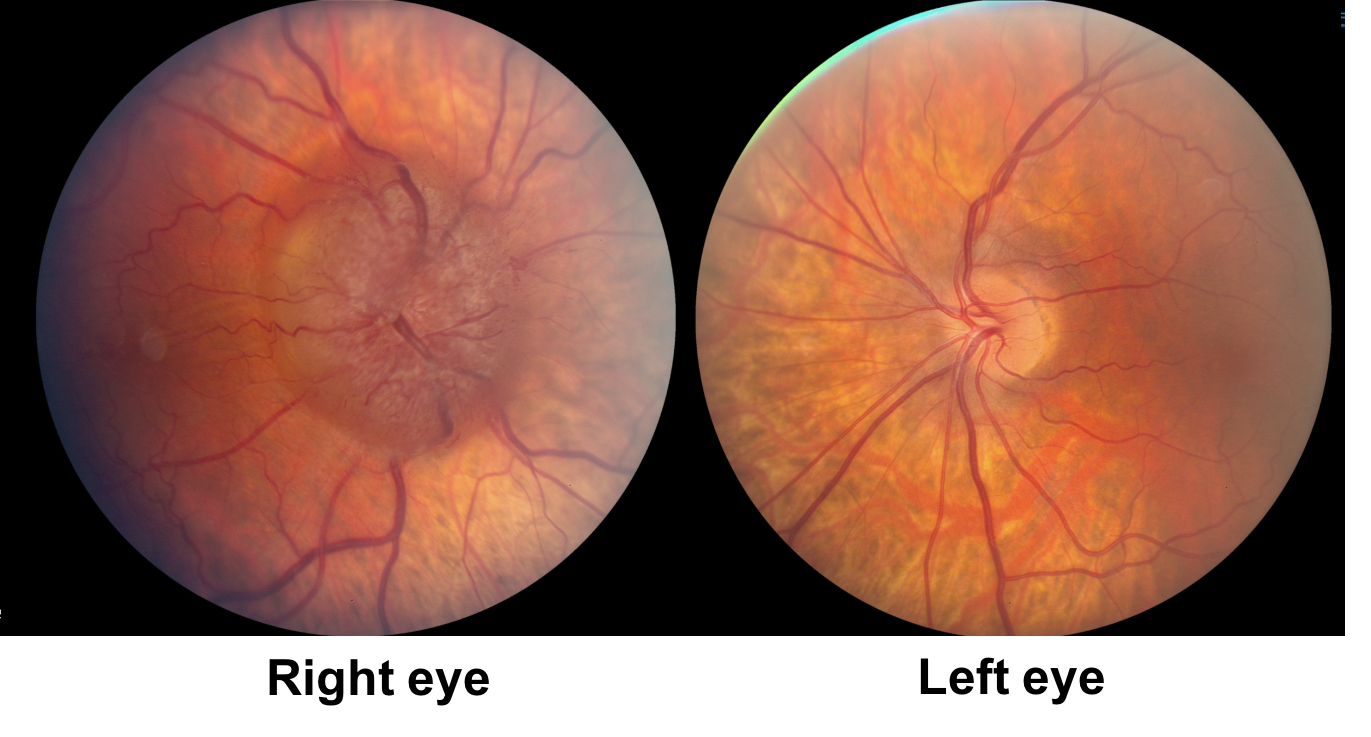
1. How would you describe the appearance of the right optic nerve?
- Optic disc elevation with visible drusen
- Optic disc edema and a choroidal neovascular membrane
- Optic disc edema and retinal folds
- Normal appearance
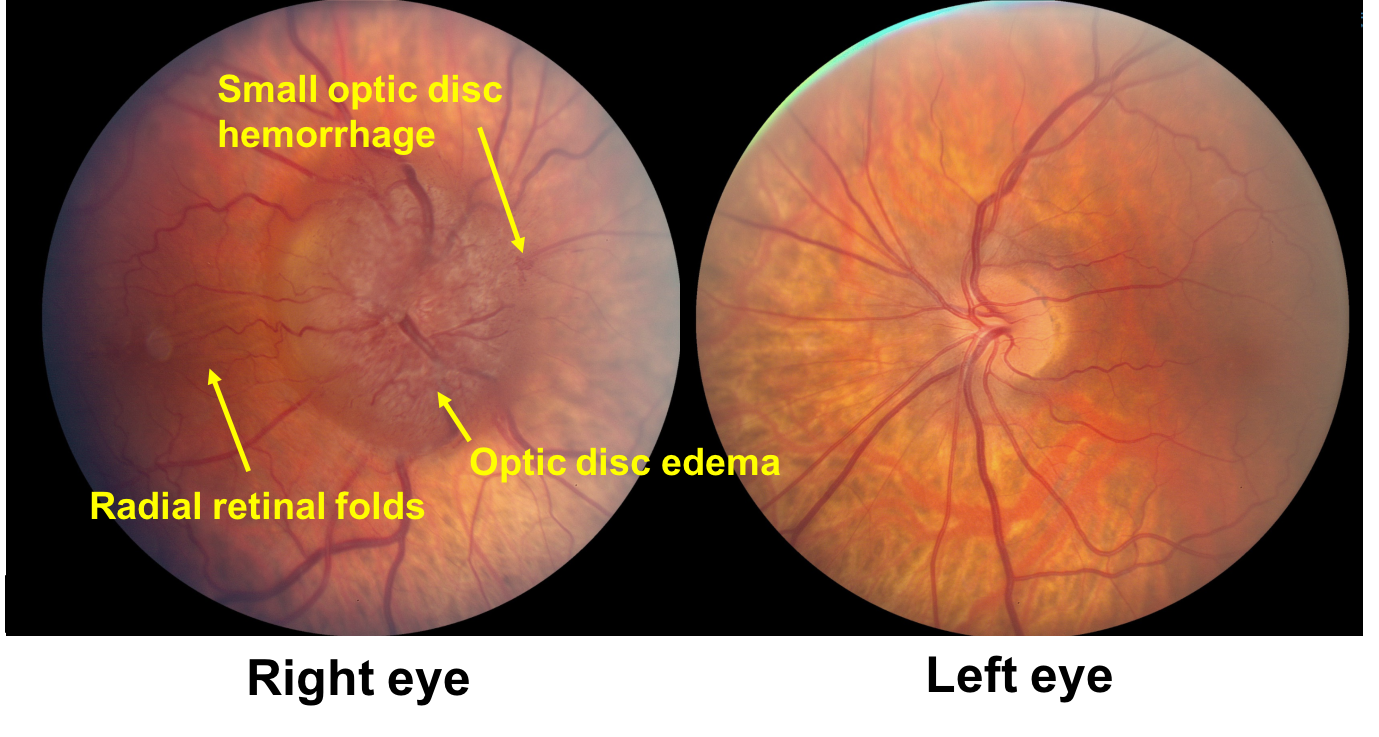
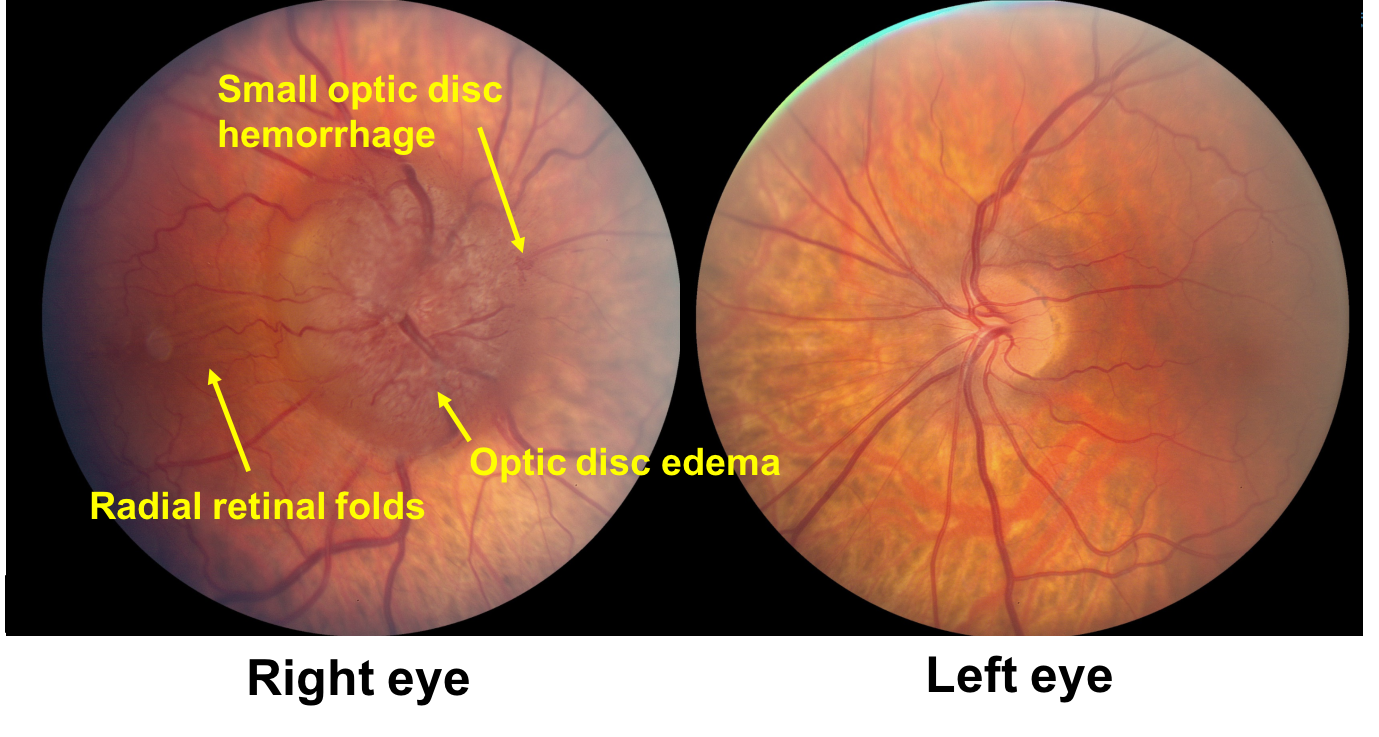
1. How would you describe the appearance of the right optic nerve? 3. Optic disc edema and retinal folds
The right optic nerve has disc edema and radial retinal folds as illustrated in the diagram below. Retinal folds are intraretinal undulations that may have various orientations (radial, horizontal or oblique). They can be differentiated from choroidal folds, which have deeper retinal pigment epithelial striations.
2. The left optic nerve can be described as:
- Large physiologic cup
- Small crowded optic nerve with absent cup
- Visible optic nerve drusen
- Mild optic disc edema
2. The left optic nerve can be described as: 2. Small crowded optic nerve with absent cup
The patient’s left optic nerve is small, crowded and without an physiologic cup. This is called a “disc-at-risk” and is a pre-requisite for developing NAION, although only a small percentage of patients with a disc-at-risk develop NAION.
3. What is included in the differential diagnosis for this patient?
- Right optic nerve sheath meningioma
- Unilateral papilledema
- Right incipient NAION
- All of the above
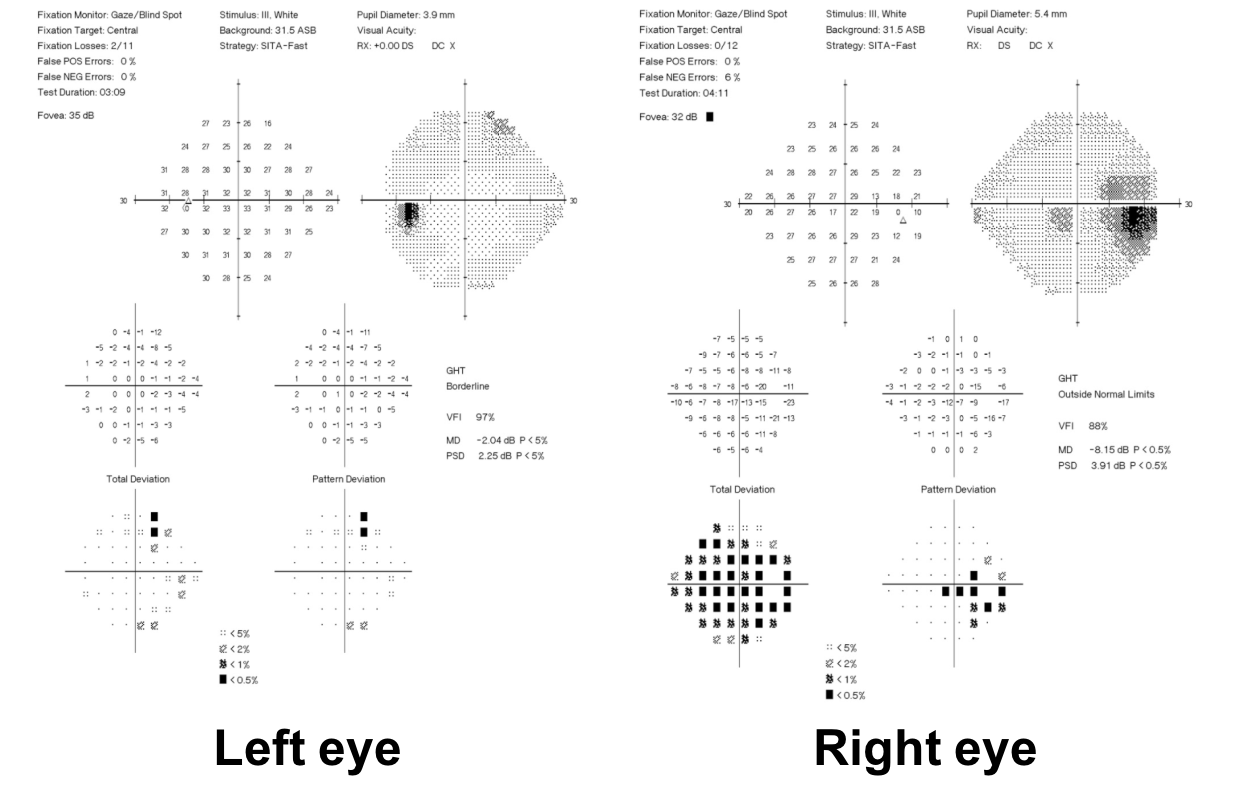
3. What is included in the differential diagnosis for this patient? 4. All of the above
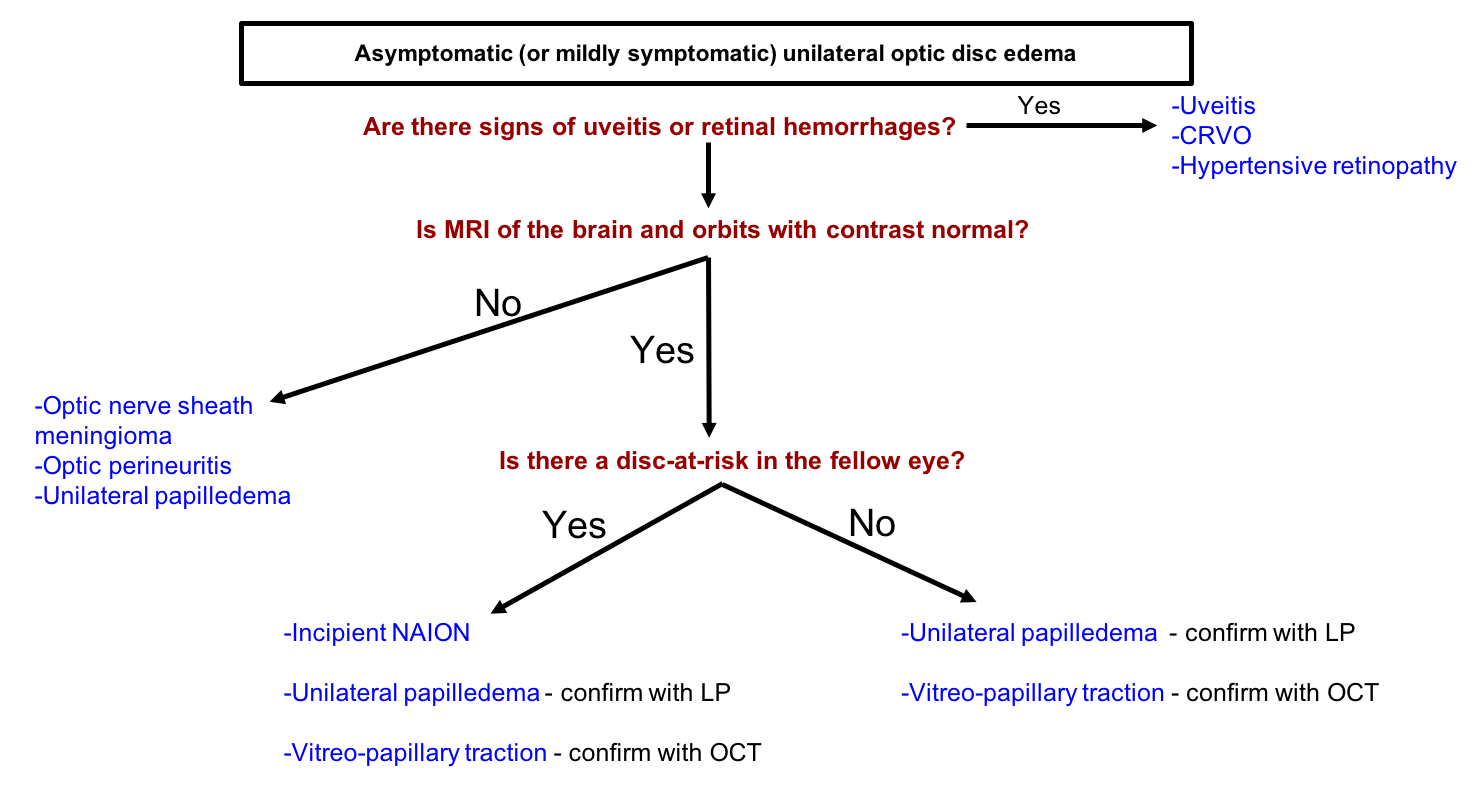
This patient has asymptomatic or “pauci-symptomatic” unilateral optic disc edema. The differential diagnosis is summarized below and includes optic nerve sheath meningioma or other retrobulbar masses, unilateral papilledema from various causes including idiopathic intracranial hypertension, vitreopapillary traction and right incipient NAION, which is a diagnosis of exclusion in a patient with a disc-at-risk. It is first important to ensure that there is true optic disc edema, since anomalous optic nerves and buried optic disc drusen may appear similar to optic disc edema.
4. Why may elevated intracranial pressure manifest as asymmetric or unilateral papilledema?
- It cannot since papilledema is always symmetrical
- The patient has had previous ocular surgery on the side with more optic disc edema
- The patient has an exophoria, which places traction on the optic nerve sheath
- There is reduced transmission of CSF pressure on the side with less optic disc edema, which may be due to a smaller optic canal size
4. Why may elevated intracranial pressure manifest as asymmetric or unilateral papilledema? 4. There is reduced transmission of CSF pressure on the side with less optic disc edema, which may be due to a smaller optic canal size
Papilledema, which is optic disc edema from elevated intracranial pressure, is usually symmetric, but may be asymmetric and even unilateral. This is because of compartmentalization of the peri-optic subarachnoid space from the suprasellar cisternal spaces on the side with less optic disc edema. A previous study found that the bony optic canal was consistently smaller on the side with less papilledema and resulted in decreased transmission of the CSF pressure to the optic nerve head.
5. What is the next most appropriate test to arrange for this patient?
- Intravenous fluorescein angiogram
- Lumbar puncture
- MRI brain and orbits with contrast
- CT angiogram of the head and neck
5. What is the next most appropriate test to arrange for this patient? 3. MRI brain and orbits with contrast
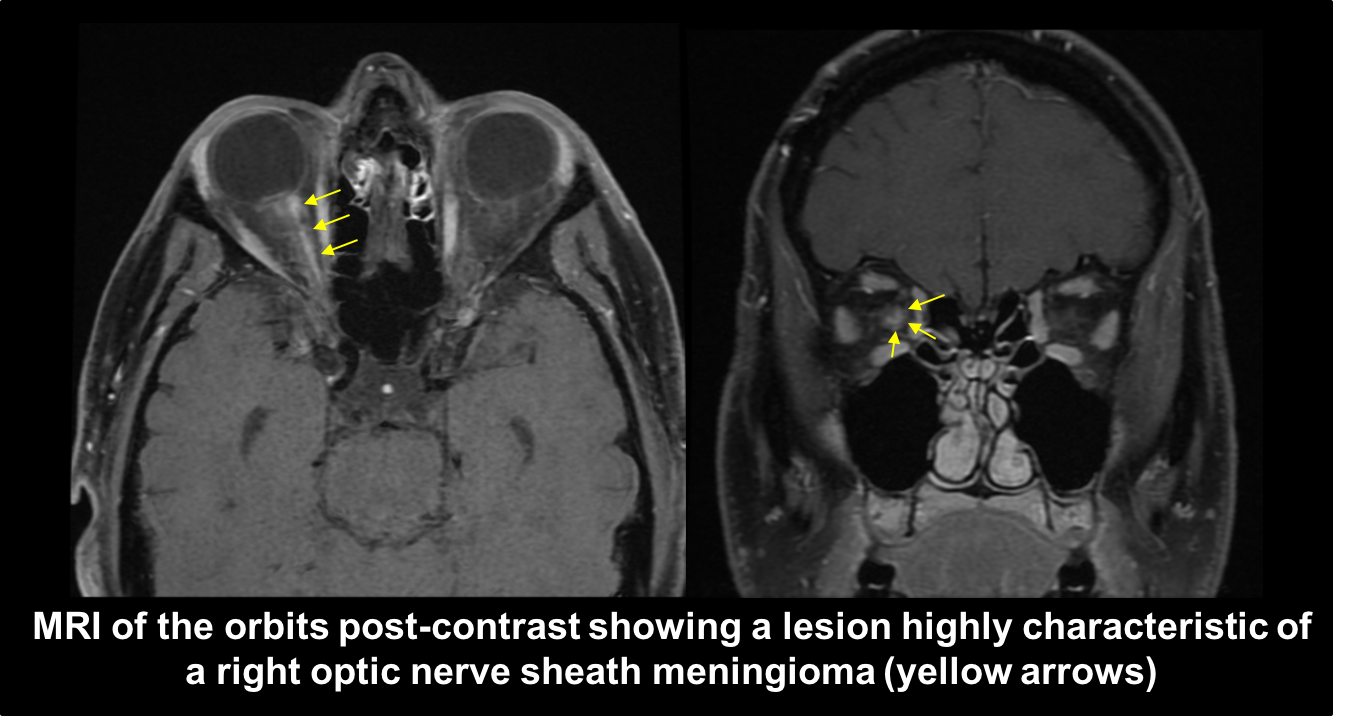
The differential diagnosis for this patient includes a right retrobulbar mass such as an optic nerve sheath meningioma and unilateral papilledema. An MRI of the orbits with contrast will be able to assess for any orbital pathology and MRI of the brain will be able to look for signs of chronically raised intracranial pressure (partially empty sella, flattening of the posterior sclera, cerebellar tonsillar ectopia, etc.) and any intracranial process that may be causing papilledema. An MRV of the head may also be considered to look for narrowing of the distal transverse sinuses, which is seen in patients with intracranial hypertension and IIH.
Clinical Pearl
MRI of the brain and orbits with contrast is required in any patient with unilateral asymptomatic optic disc edema.
6. What is the next most appropriate step in the diagnosis of this patient’s optic nerve lesion?
- Biopsy and histopathological analysis
- Lumbar puncture for cytology and flow cytometry
- Metastatic survey
- No further diagnostic tests are required
6. What is the next most appropriate step in the diagnosis of this patient’s optic nerve lesion? 4. No further diagnostic tests are required
Neuroimaging studies, particularly MRI of the orbits, have obviated the need for tissue biopsy in most cases since optic nerve sheath meningiomas show highly characteristic radiological features. A biopsy confers a very high risk of permanent vision loss and would not be recommended in this patient with good vision. Biopsy would only be considered when there is an unusual clinical course or atypical MRI findings in a patient with severe vision loss.
7. Optic nerve sheath meningiomas originate from what layer of the meninges?
- Dura mater
- Arachnoid mater
- Pia mater
- None of the above
7. Optic nerve sheath meningiomas originate from what layer of the meninges? 2. Arachnoid mater
Optic nerve sheath meningiomas originate from arachnoid cap cells within the dural sheath surrounding the intraorbital or less commonly, the intracanalicular optic nerve. The optic nerve sheath may secondarily become affected by an intracranial meningioma on or near the planum sphenoidale that spreads anteriorly. As the optic nerve sheath meningioma spreads, it compromises the function of the optic nerve by interfering with blood flow or impairing axonal transport.
8. Which of the following is true regarding the optic nerve appearance of patients with optic nerve sheath meningiomas at presentation?
- There may be optic disc edema
- The optic nerve may appear pale
- The optic nerve may appear normal
- All of the above
8. Which of the following is true regarding the optic nerve appearance of patients with optic nerve sheath meningiomas at presentation? 4. All of the above
Examination of the optic disc may reveal optic disc edema, atrophy or may even appear normal at first presentation. The presence of optic nerve swelling suggests that the tumor is located closer to the globe and is less commonly seen with tumors located more posteriorly near the optic canal. Some degree of optic atrophy and edema may also be seen together at the same time. A previous study found that 98% of patients will show some degree of optic disc edema or pallor at initial presentation.
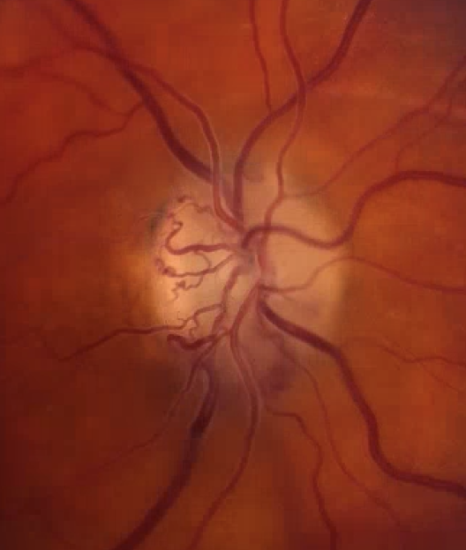
9. A patient presents with longstanding vision loss in the right eye. The optic disc has the following appearance.
What is included in the differential diagnosis?
- Glaucoma
- Optic nerve sheath meningioma
- Chronic papilledema
- Central retinal vein occlusion (CRVO)
- All of the above
9. What is included in the differential diagnosis? 5. All of the above
The optic disc shown above has optociliary shunt vessels, also known as retinochoroidal collaterals. These are pre-existing venous channels that dilate in response to chronically elevated central retinal vein obstruction. They occur in approximately 30% of patients with optic nerve sheath meningiomas and may also be seen in patients with optic nerve gliomas, CRVO, glaucoma, and chronic papilledema.
Clinical Pearls
The differential diagnosis of optociliary shunt vessels includes:
- Optic nerve sheath meningioma
- Optic nerve glioma
- Central retinal vein occlusion
- Glaucoma
- Chronic papilledema
10. What other examination finding may be seen in patients with optic nerve sheath meningiomas?
- Proptosis
- Anterior segment inflammation
- Eyelid retraction
- Aberrant regeneration
10. What other examination finding may be seen in patients with optic nerve sheath meningiomas? 1. Proptosis
Proptosis is a common finding in patients with optic nerve sheath meningiomas and has been reported in 142 of 241 (59%) of patients at presentation. It is usually mild to moderate and slowly progressive. Other external changes that may be seen include a limitation of ocular motility, which is due to stiffening of the optic nerve and mechanical restriction of the extraocular muscles.
11. Which of the following is true regarding the epidemiology of optic nerve sheath meningiomas?
- They occur more commonly in women
- They occur more commonly in patients in their 7th and 8th decade of life
- They are more common in black patients
- They are never bilateral
11. Which of the following is true regarding the epidemiology of optic nerve sheath meningiomas? 1. They occur more commonly in women
Meningiomas in general tend to occur more frequently in women with a female to male ratio of two to three to one. This is also true for optic nerve sheath meningiomas and a review of cases reported in the literature showed a female predominance (61%). The mean age of presentation was 40.8 years but may occur at almost any age. Although unilateral presentation is the norm, they may rarely be bilateral at presentation.
12. What is the treatment of choice for optic nerve sheath meningiomas?
- Estrogen antagonist
- Stereotactic fractionated radiotherapy only after the diagnosis is confirmed with biopsy
- Surgical excision
- Stereotactic fractionated radiotherapy
12. What is the treatment of choice for optic nerve sheath meningiomas? 4. Stereotactic fractionated radiotherapy
Stereotactic fractionated radiotherapy is the treatment of choice for optic nerve sheath meningiomas and has been reported to stabilize vision or improve vision in 94.3% of cases. There is still some debate as to whether treatment should be initiated immediately after diagnosis or only after progression since some patients may remain stable for years. With improved technology and radiation techniques, however, the risk of radiation retinopathy and pituitary dysfunction are very small. Surgery or biopsy is usually not recommended due to the high risk of permanent vision loss.
13. What is the most common primary tumor of the optic nerve?
- Optic nerve glioma
- Optic nerve sheath meningioma
- Metastases to the optic nerve
- Retinoblastoma
13. What is the most common primary tumor of the optic nerve? 1. Optic nerve glioma
Gliomas are the most common optic nerve tumors followed by optic nerve sheath meningiomas. Most optic pathway gliomas are detected during the first two decades of life (approximately 90%) and there is a strong association with neurofibromatosis I with an incidence of up to 70%. Optic nerve gliomas diagnosed later in life tend to have a worse prognosis.
14. Which radiological feature is more characteristic of optic nerve gliomas compared to optic nerve sheath meningiomas?
- Kinking or buckling of the optic nerve
- Calcification of the optic nerve sheath
- Optic nerve sheath thickening and enhancement with relative sparing of the optic nerve substance
- Extradural tumor extension
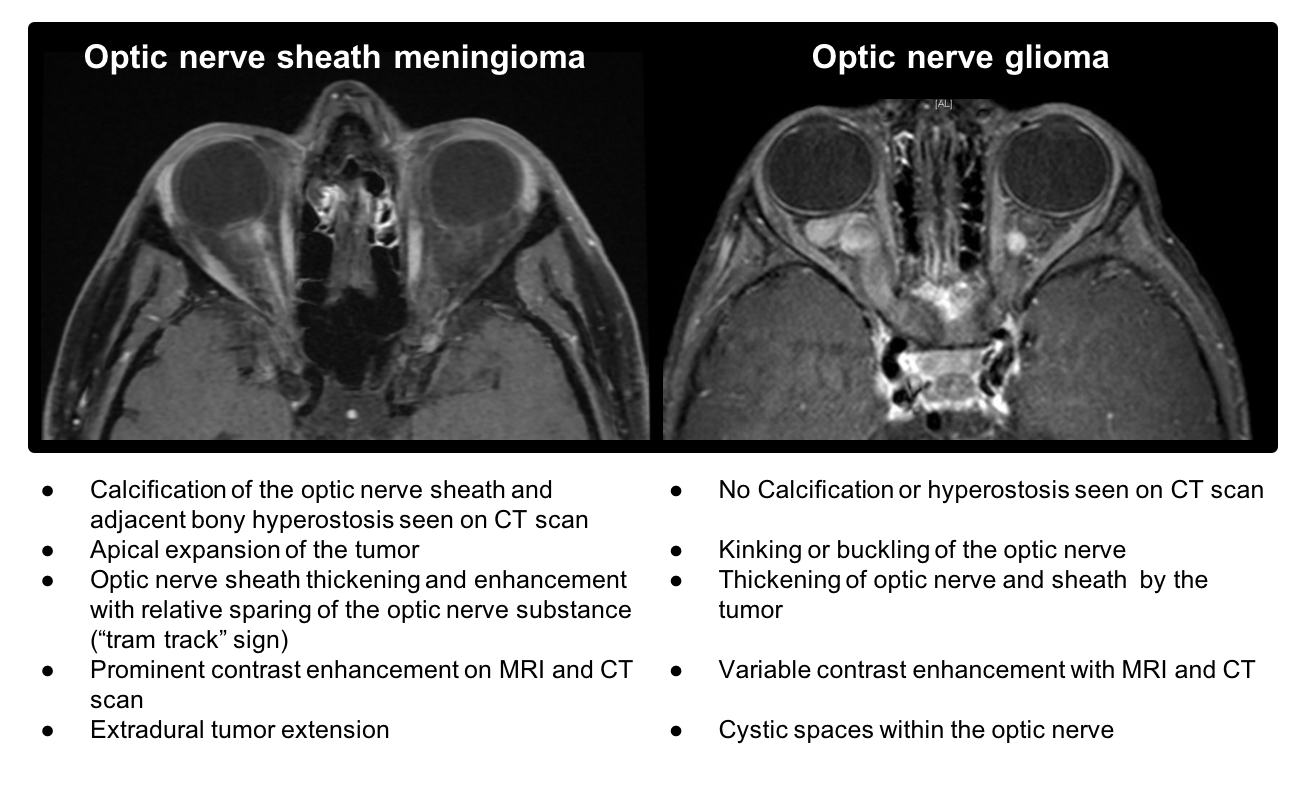
14. Which radiological feature is more characteristic of optic nerve gliomas compared to optic nerve sheath meningiomas? 1. Kinking or buckling of the optic nerve
The radiological characteristics of optic nerve sheath meningiomas and optic nerve gliomas are summarized in the figure below. Kinking or buckling of the optic nerve is characteristic of optic nerve gliomas whereas calcification, thickening and enhancement of the optic nerve sheath with sparing of the optic nerve substance (“tram tracking”), and extradural tumor extension are features of optic nerve sheath meningiomas.
15. A patient is diagnosed with a right optic nerve glioma. What other examination finding in this patient would lead to a diagnosis of neurofibromatosis I (NFI)?
-
- Bilateral vestibular schwannomas
- Epiretinal membrane
- Iris hamartomas
- Peripheral neuropathy
15. A patient is diagnosed with a right optic nerve glioma. What other examination finding in this patient would lead to a diagnosis of NFI? 3. Iris hamartomas
Iris hamartomas, otherwise known as Lisch nodules, are important in the diagnosis of NFI. They are less common in young children (detected in fewer than 10% of children less than 6 years of age) but are seen in greater than 90% of adults. The diagnostic criteria for NFI is summarized in the box below.
The diagnostic criteria for NF1 requires at least two of the following features:
- Six or more café-au-lait macules
- Two or more neurofibromas or one plexiform neurofibroma
- Axillary or inguinal freckling
- Optic glioma
- Two or more Lisch nodules
- A distinctive bony lesion (eg. sphenoid dysplasia)
- First-degree relative with NFI
16. Which of the following is true regarding the genetics of NFI?
- Almost all cases are sporadic
- It is inherited in an autosomal dominant manner
- It is inherited in an autosomal recessive manner
- It is X-linked recessive
16. Which of the following is true regarding the genetics of NFI? 2. It is inherited in an autosomal dominant manner
About one-half of NFI cases are inherited and the remainder are sporadic. It is inherited in an autosomal dominant manner and due to mutations in the NF1 gene located on chromosome 17 (this can be remembered by counting the number of letters in neurofibromatosis, 17). The penetrance (likelihood an individual with the mutation will manifest the disorder) is complete, but the expression is variable.
17. A patient has a right optic nerve sheath meningioma, posterior subcapsular cataracts and a unilateral vestibular schwannoma. What is the most likely diagnosis?
- NF1
- NF2
- Tuberous Sclerosis
- von Hippel Lindau
17. A patient has a right optic nerve sheath meningioma, posterior subcapsular cataracts and a unilateral vestibular schwannoma. What is the most likely diagnosis? 2. NF2
NF2 is a dominantly inherited condition that predisposes patients to central nervous system tumors. The most common tumors are bilateral vestibular schwannomas and intracranial and spinal meningiomas. The diagnostic criteria for NF2 is summarized below.
Diagnostic criteria for NF2
A clinical diagnosis of NF2 can be made by the presence of one of the following:
- Bilateral vestibular schwannomas before age 70
- Unilateral vestibular schwannoma before age 70 and first-degree relative with NF2
- Any two of: meningioma, non-vestibular schwannoma, neurofibroma, glioma, cerebral calcification, cataract AND:
-
- First degree relative with NF2 OR
- Unilateral vestibular schwannoma and negative LZTR1 testing (if two or more non-intradermal schwannomas)
- Multiple meningiomas AND:
-
- Unilateral vestibular schwannoma OR
- Any two of : non-vestibular schwannoma, neurofibroma, glioma, cerebral calcification, cataract
- Constitutional or mosaic pathogenic NF2 from the blood or identification of identical mutation in two tumors from the same individuals
18. Which of the following are ocular manifestations of NF2?
- Posterior subcapsular or wedge-shaped cortical cataracts
- Epiretinal membranes
- Retinal hamartomas
- Combined hamartomas of the retina and retinal pigment epithelium
- All of the above
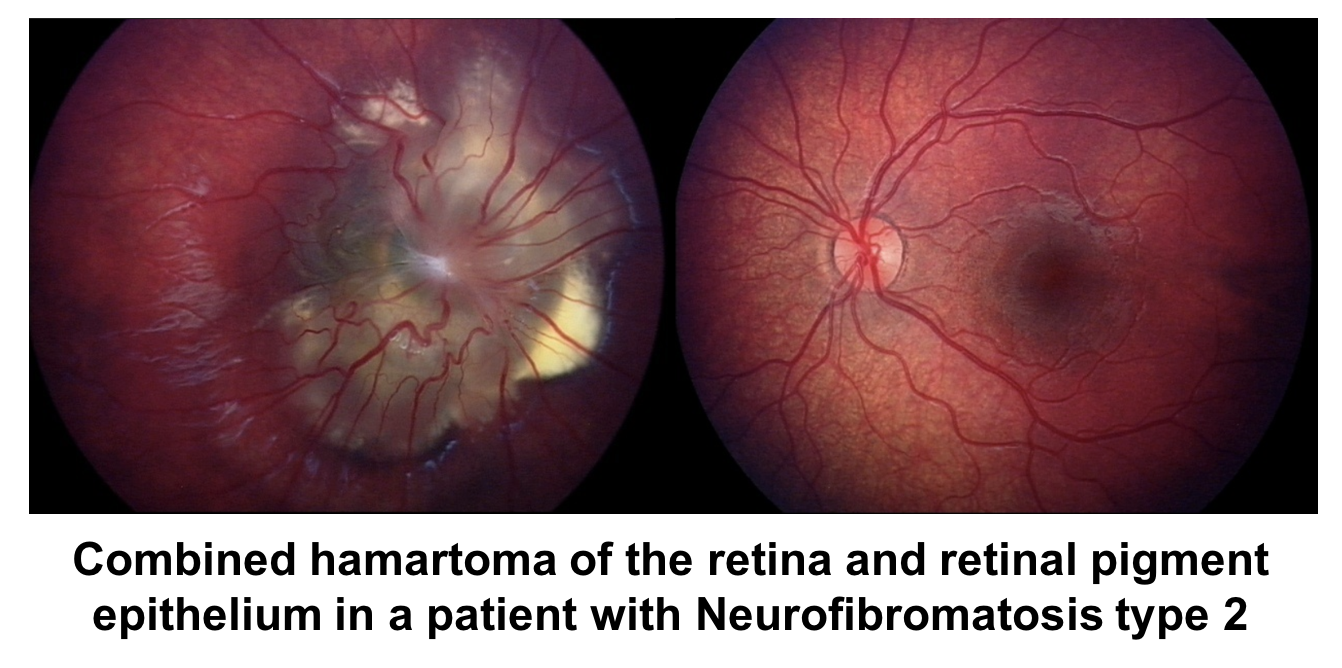
18. Which of the following are ocular manifestations of NF2? 5. All of the above
The most characteristic ocular finding in NF2 are lens opacities (posterior subcapsular or wedge-shaped cortical cataracts), but also include epiretinal membranes (seen in up to 80% of patients). Less common findings include retinal hamartomas and combined hamartomas of the retina and retinal pigment epithelium (shown below).
20. A patient has the following retinal lesion and ipsilateral arteriovenous malformation in the CNS. What is the inheritance pattern of this condition?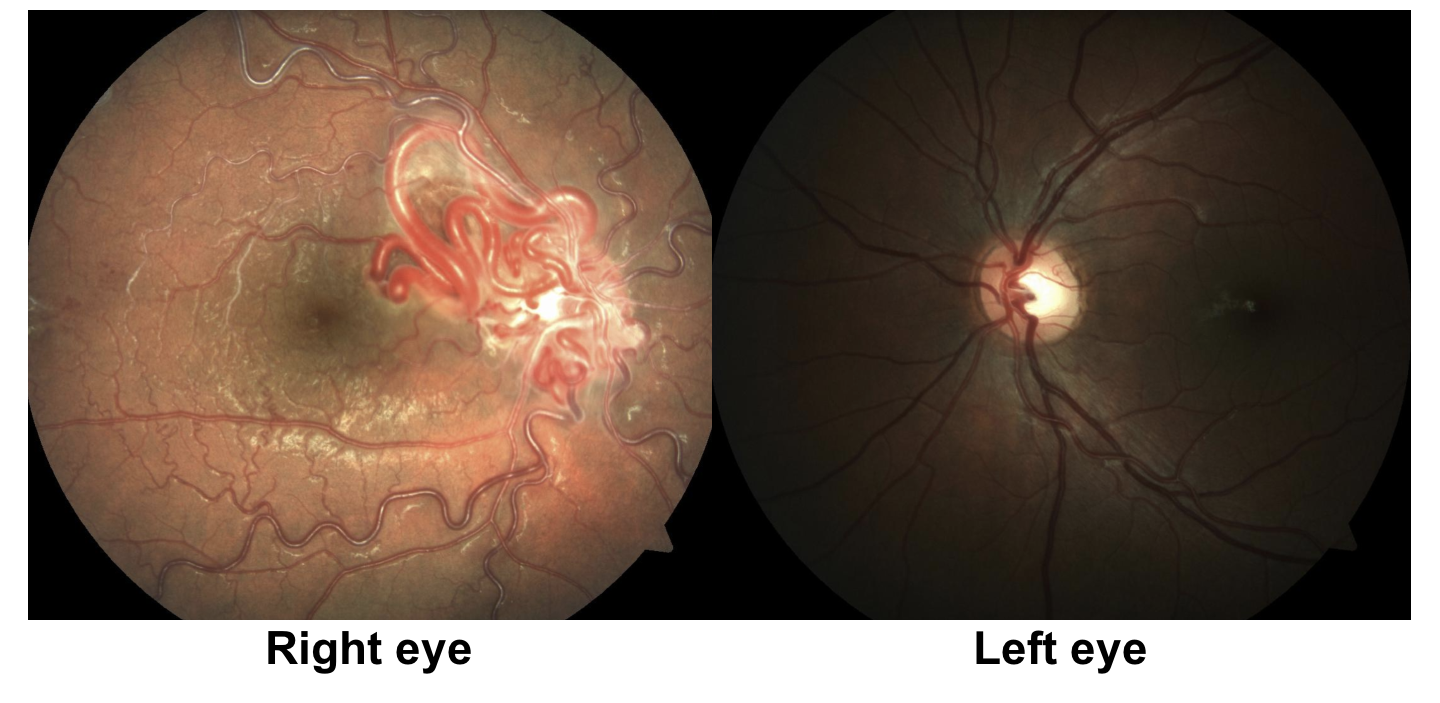
-
- Autosomal dominant
- Autosomal recessive
- X-linked recessive
- Sporadic
20. A patient has the following retinal lesion and ipsilateral arteriovenous malformation in the CNS. What is the inheritance pattern of this condition? 4. Sporadic
This patient has a retinal arteriovenous malformation (AVM) also known as a racemose angioma. The combination of this AVM and an ipsilateral CNS AVM indicates a diagnosis of Wyburn Mason syndrome, which is a sporadic condition.
The phacomatoses are a group of disorders characterized by hamartomas of various parts of the body including the skin, eyes, CNS, and visceral organs. They include NF1 (autosomal dominant), NF2 (autosomal dominant), von Hippel Lindau disease (autosomal dominant), Sturge Weber Syndrome (sporadic), tuberous sclerosis (autosomal dominant), Wyburn Mason Syndrome (sporadic), and ataxia telangiectasia (autosomal recessive). Wyburn Mason syndrome is characterized by arteriovenous malformations of the retina and ipsilateral arteriovenous malformations of the CNS.
Case Summary
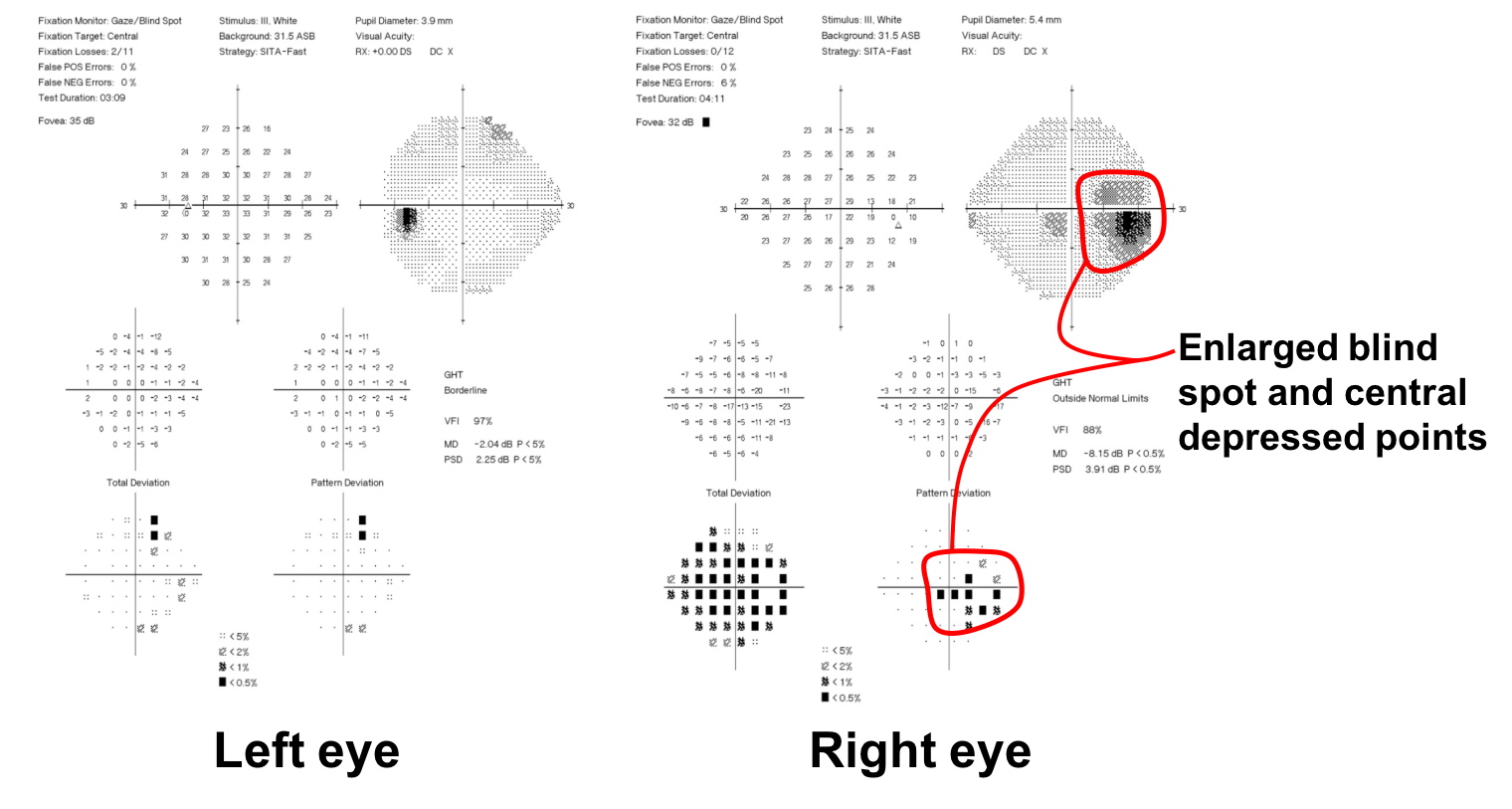
She was noted to have right optic disc edema without any visual symptoms. MRI of the brain and orbits with contrast revealed a right optic nerve sheath meningioma. She was treated with stereotactic fractionated radiotherapy and had improvement in her visual field. She was followed for 5 years and did not have any recurrence or changes in her vision.
Further reading:
-
Miller NR. New concepts in the diagnosis and management of optic nerve sheath meningioma. J Neuroophthalmol 2006;26(3):200-208. https://www.ncbi.nlm.nih.gov/pubmed/16966942
- Berman D, Miller NR. New concepts in the management of optic nerve sheath meningiomas. Ann Acad Med Singapore 2006;35:168-74. http://www.annals.edu.sg/pdf/35volno3200604/v35n3p168.pdf
-
Dutton JJ. Optic nerve sheath meningiomas. Surv Ophthalmol 1992;37:167-83. https://www.ncbi.nlm.nih.gov/pubmed/1475751
-
Bidot S, Bruce BB, Saindane AM, Newman NJ, Biousse V. Asymmetric papilledema in idiopathic intracranial hypertension. J Neuroophthalmol 2015;35(1):31-36. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4326590/
-
Korf BR. Neurofibromatosis. Handb Clin Neurol 2013;111:333-40. https://www.ncbi.nlm.nih.gov/pubmed/23622184