19
Case
Age: 35-year-old white woman
Reason for referral to ophthalmology: Double vision
Past medical history: None
Past ocular history: None
Medications: None
Habits: Non-smoker and non-drinker
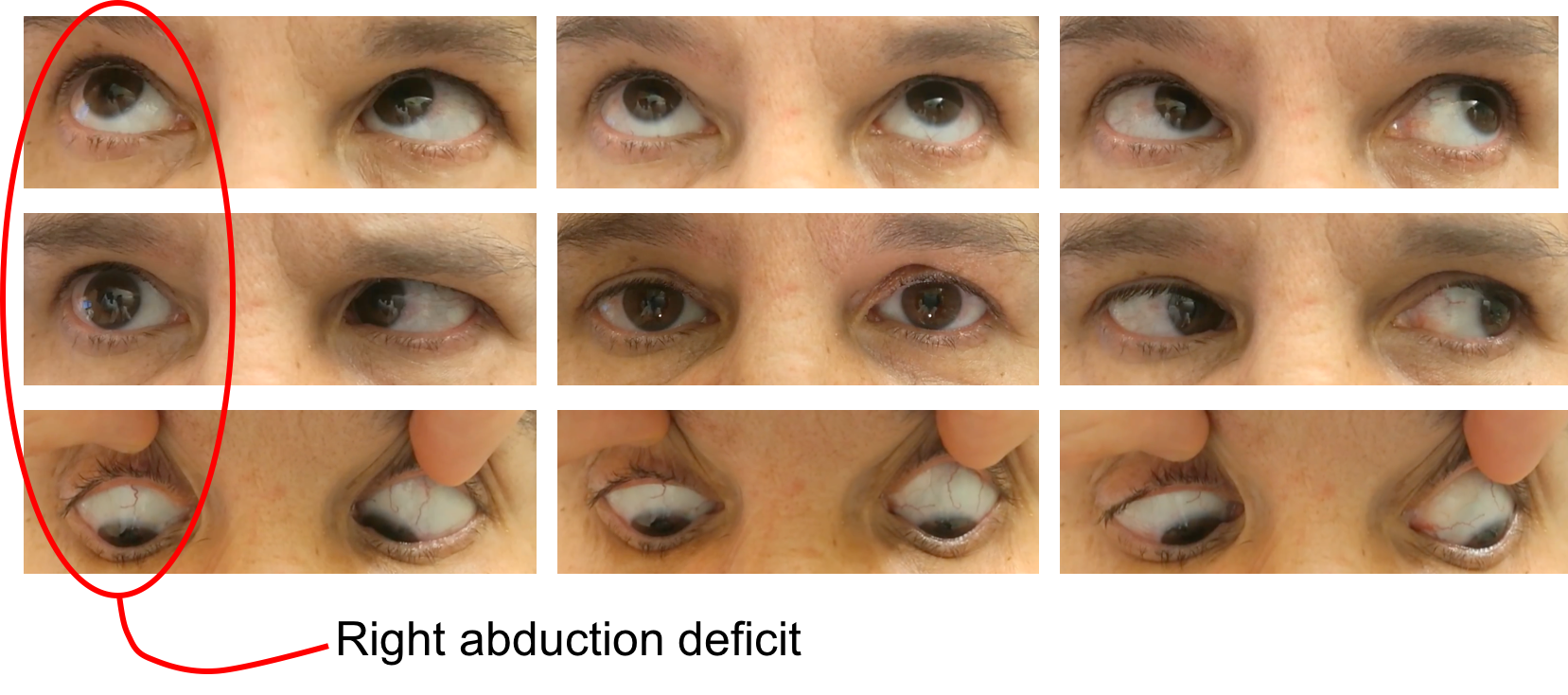
HPI: Six days ago, she started to notice double vision with objects separated horizontally. The double vision is worse when looking to the right and improves when looking to the left or when reading. The double vision persisted, which prompted her to go to the emergency room. An ophthalmology consultation was requested.
Ophthalmological examination:
Blood pressure: 121/82, heart rate 74
Visual acuity is 20/20 OD, 20/20 OS
Pupils are equal sizes and reactive to light, there is no RAPD
Color vision is 14/14 OD and 14/14 OS correct Ishihara plates
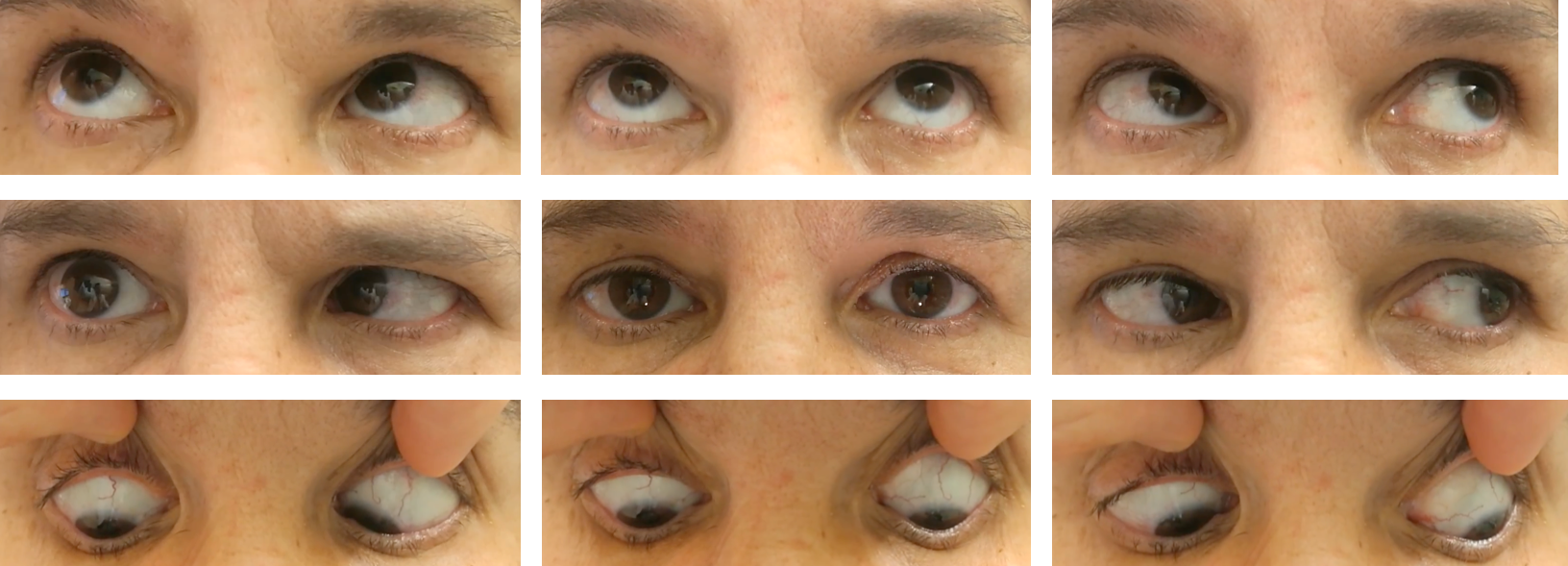
Ocular motility and alignment are shown below
Slit lamp examination are normal
Visual fields are normal in both eyes
Neurological examination is otherwise normal
1. Which of the following is included in the differential diagnosis for this patient:
- Thyroid eye disease
- Ocular myasthenia gravis
- Right orbital mass
- Right sixth nerve palsy
- All of the above
1. Which of the following is included in the differential diagnosis for this patient: 5. All of the above
This young patient has an incomitant esotropia with limitation of abduction in the right eye. Incomitant means that the esotropia varies in magnitude with position of gaze. In this case, the esotropia is greatest in right gaze, consistent with the right abduction deficit. The differential diagnosis includes lesions in the right orbit, neuromuscular junction, 6th peripheral nerve or nerve fascicle. Orbital lesions include restriction from a large medial rectus muscle from thyroid eye disease or a an orbital mass. Neuromuscular junction conditions include ocular myasthenia gravis and the peripheral sixth nerve may be affected by compression by cavernous sinus or skull base tumors. Parenchymal lesions in the pons may affect the sixth nerve fascicle, which is the portion of the nerve between the abducens nucleus and it’s exit from the pons. Clinical assessment should therefore include examination for orbital signs, a detailed cranial nerve examination, and assessment for signs of myasthenia gravis.
2. How could you differentiate restriction from paresis in this patient?
- Forced duction testing
- Alternate cover test
- Dilated fundus examination
- These cannot reliably be differentiated
2. How could you differentiate restriction from paresis in this patient? 1. Forced duction testing
Forced duction testing involves grasping the eye with toothed forceps (after topical or local anesthesia) and mechanically moving the eye in different positions of gaze. If the eye cannot be moved in a particular direction, there is mechanical restriction. If, however, the eye can be moved in a full range of motion in all directions of gaze, the strabismus is due to paresis. If this patient had a 6th nerve palsy, the eye would freely move in all directions of gaze, but if there was restriction from a large medial rectus muscle from thyroid eye disease, for example, the eye would not fully abduct with forced duction testing.
Forced duction is not routinely used in the clinic, but may be important when evaluating patients after trauma who are suspected of having a restrictive strabismus or in patients under general anesthesia.
3. What is the next most appropriate course of action for this patient :
- MRI of the brain and orbits with contrast
- MRA of the head and neck
- CT scan of the chest
- HIV, B12, folate, ANA, ANCA, liver function tests and extended electrolytes
3. What is the next most appropriate course of action: 1. MRI of the brain and orbits with contrast
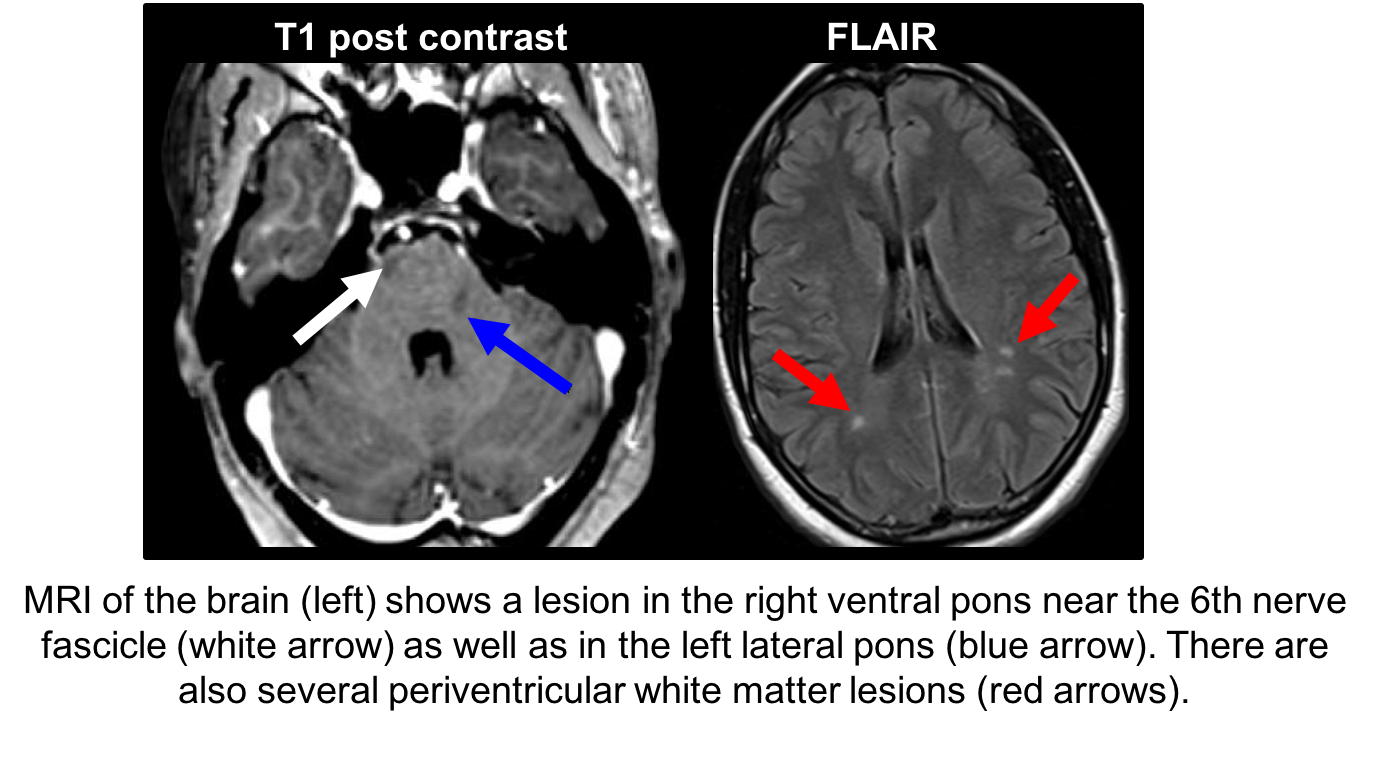
The differential diagnosis includes lesions of the right 6th nerve fascicle, peripheral nerve, or orbital lesions and an MRI of the brain and orbits with contrast will be able to evaluate for these causes. Other tests to consider include acetylcholine receptor antibodies and thyroid function tests. It would be inappropriate to observe this young patient since she may have an orbital/intracranial mass or demyelinating lesion that warrants further investigation and treatment.
4. This patient meets the 2017 revisions to the McDonald criteria for the diagnosis of multiple sclerosis because:
- She has both symptomatic lesions and asymptomatic lesions
- She has evidence of lesions disseminated in time (contrast enhancing and non-contrast enhancing lesions) and space (infratentorial and supratentorial white matter lesions)
- She is symptomatic from a white matter lesion
- She does not meet the McDonald criteria at this time
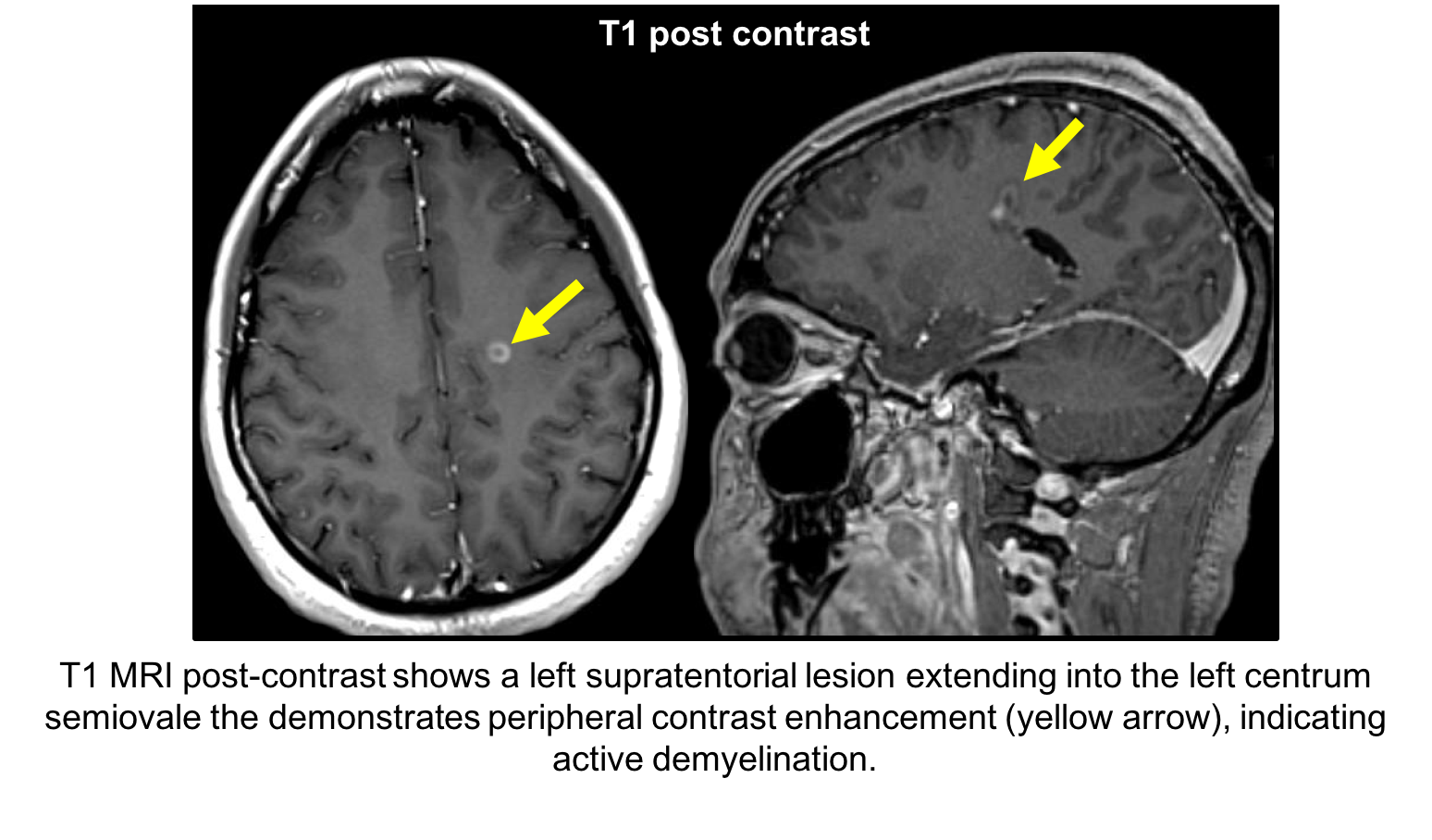
4. This patient meets the 2017 revisions to the McDonald criteria for the diagnosis of multiple sclerosis because: 2. She has evidence of lesions disseminated in time (contrast enhancing and non-contrast enhancing lesions) and space (infratentorial and supratentorial white matter lesions)
According to the 2017 revisions to the McDonald criteria, diagnosis of multiple sclerosis (MS) requires dissemination of lesions in time and space. In a patient with 1 clinical attack and objective clinical evidence of 1 lesion, dissemination in time is established by simultaneous contrast-enhancing and non-contrast enhancing lesions at any time or a new T2 and/or contrast enhancing lesion on follow-up MRI irrespective of timing or a second clinical attack. Cerebrospinal fluid-specific oligocloncal bands may also be used to establish dissemination in time. This patient has evidence of dissemination in space due to the presence of enhancing and non-enhancing lesions.
Dissemination in space is demonstrated by at least one T2 lesion in at least two MS typical CNS regions (periventricular, juxtacortical, infratentorial, spinal cord) or awaiting a clinical attack implicating a second CNS site. This patient has dissemination in space since there are periventricular and infratentorial (pontine) lesions. A thorough evaluation did not reveal any evidence of other demyelinating or connective tissue disorders.
5. What treatment should be considered for this patient:
- Low-dose oral prednisone
- Intravenous high-dose methylprednisolone and disease modifying therapy for multiple sclerosis
- Optimization of vascular risk factors
- Low-dose aspirin
5. What treatment should be considered for this patient: 2. Intravenous high-dose methylprednisolone and disease modifying therapy for multiple sclerosis
This patient was diagnosed with multiple sclerosis and disease-modifying treatment was recommended. For patients with multiple sclerosis, exacerbations that result in neurological symptoms and increased disability are often treated with glucocorticoids. A common regimen is intravenous methylprednisolone 1 g daily for 3 to 5 days with or without an oral taper. Vitamin D is also recommended by a majority of MS specialists (approximately 4000 IU per day).
6. Why is the peripheral 6th cranial nerve not expected to be affected in multiple sclerosis?
- It is myelinated by oligodendrocytes
- It is myelinated by Schwann cells
- It is not myelinated
- It is affected by multiple sclerosis
6. Why is the peripheral 6th cranial nerve not expected to be affected in multiple sclerosis? 2. It is myelinated by Schwann cells
Multiple sclerosis is a demyelinating disease of the central nervous system. All cranial nerves, with the exception of the olfactory and optic nerve, are myelinated by Schwann cells as opposed to oligodendrocytes. Oligodendrocytes are the target of immune attacks in MS, but not Schwann cells. The optic nerve is myelinated by oligodendrocytes, which is why optic neuritis is a common feature in patients with MS. This patient has a 6th nerve palsy due to demyelination in the pons (central nervous system) whereas the 6th peripheral nerve is myelinated by Schwann cells.
7. What clinical finding would a lesion of the 6th cranial nerve nucleus be expected to show?
- Contralateral gaze palsy
- Ipsilateral gaze palsy
- Abduction deficit in one eye
- Abduction deficit in both eyes
7. What clinical finding would a lesion of the 6th cranial nerve nucleus be expected to show? 2. Ipsilateral gaze palsy
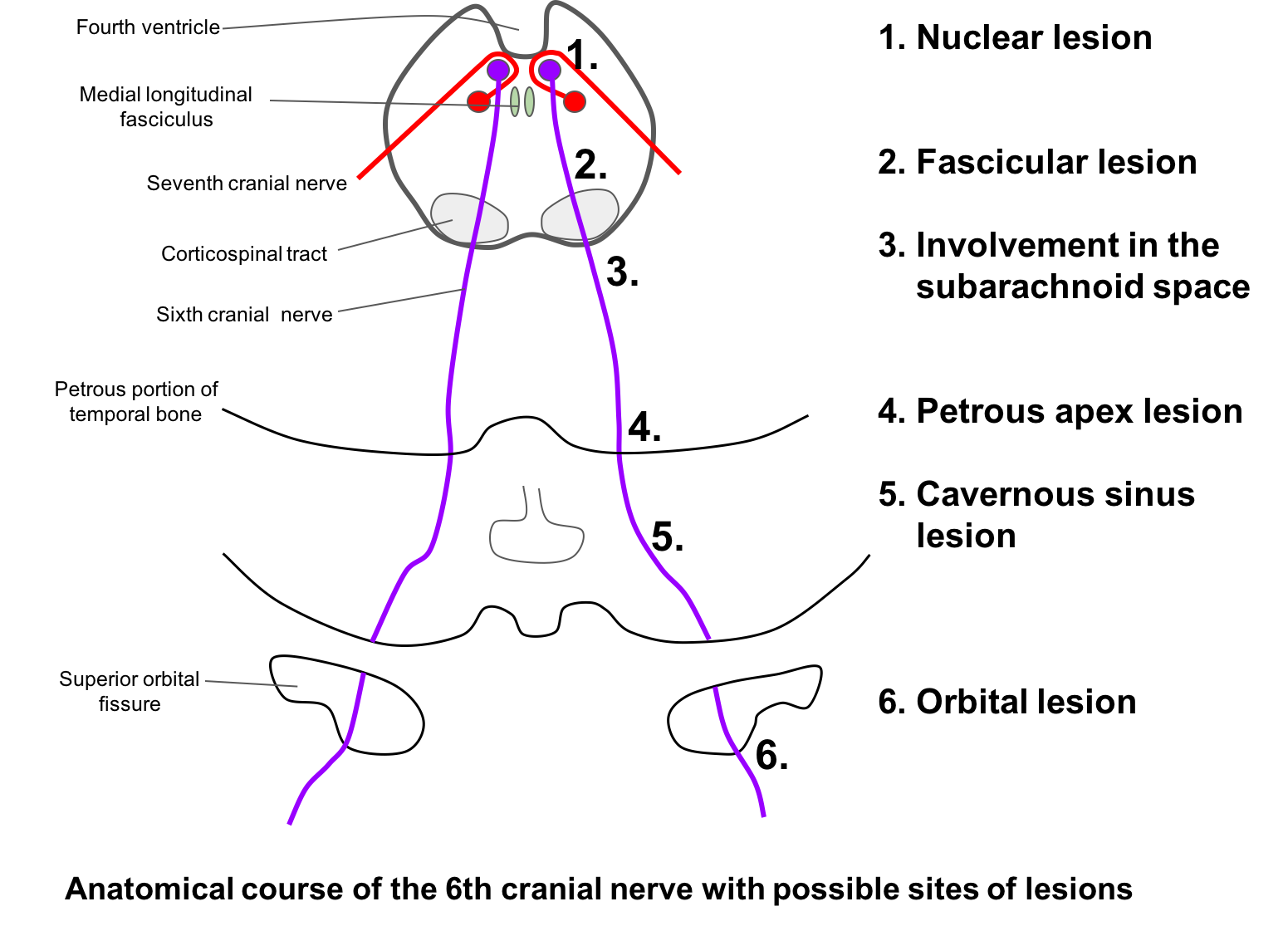
The 6th nerve nucleus is located in the dorsal pons and contains motor neurons that innervate the ipsilateral lateral rectus and cell bodies of internuclear neurons that cross the midline and ascend in the contralateral medial longitudinal fasciculus (MLF). Therefore, lesions of the 6th cranial nerve nucleus cause a conjugate gaze palsy to the ipsilateral side. For instance, a patient with a lesion of the left 6th nerve nucleus would not be able to look to the left with either eye. In most cases, there is also a peripheral ipsilateral facial palsy present since the facial nerve fascicle loops around the 6th nerve nucleus before exiting the brainstem (shown below).
8. A patient has a 6th and 7th nerve palsy with contralateral hemiplegia. This localizes the lesion to the:
- Cerebral cortex
- Midbrain
- Pons
- Medulla
8. A patient has a 6th and 7th nerve palsy with contralateral hemiplegia. This localizes the lesion to the: 3. Pons
A patient with 6th and 7th nerve palsies with contralateral hemiplegia has a lesion in the ventral pons, ipsilateral to the side with the 6th and 7th nerve palsies (known as Millard-Gubler syndrome).
Other eponymous syndromes of the 6th nerve fascicle are:
- Raymond syndrome: lesion of 6th nerve fascicle and corticospinal tract leading to ipsilateral 6th nerve palsy and contralateral hemiparesis
- Foville syndrome: lesion of the 6th and 7th nerve fascicle or nucleus with contralateral ataxia and sensory disturbance. There may also be loss of taste from the anterior two-thirds of the tongue, ipsilateral Horner’s syndrome, ipsilateral analgesia of the face, ipsilateral peripheral deafness, and contralateral loss of pain and temperature sensation on the body. Usually it is caused by occlusion of the anterior inferior cerebellar artery.
9. In a patient with unilateral or bilateral 6th nerve palsies, what other pertinent finding from the ophthalmological examination is important to document?
- Presence of retinal hemorrhages
- Presence of optic disc edema
- Presence of iris transillumination defects
- Presence of cataract
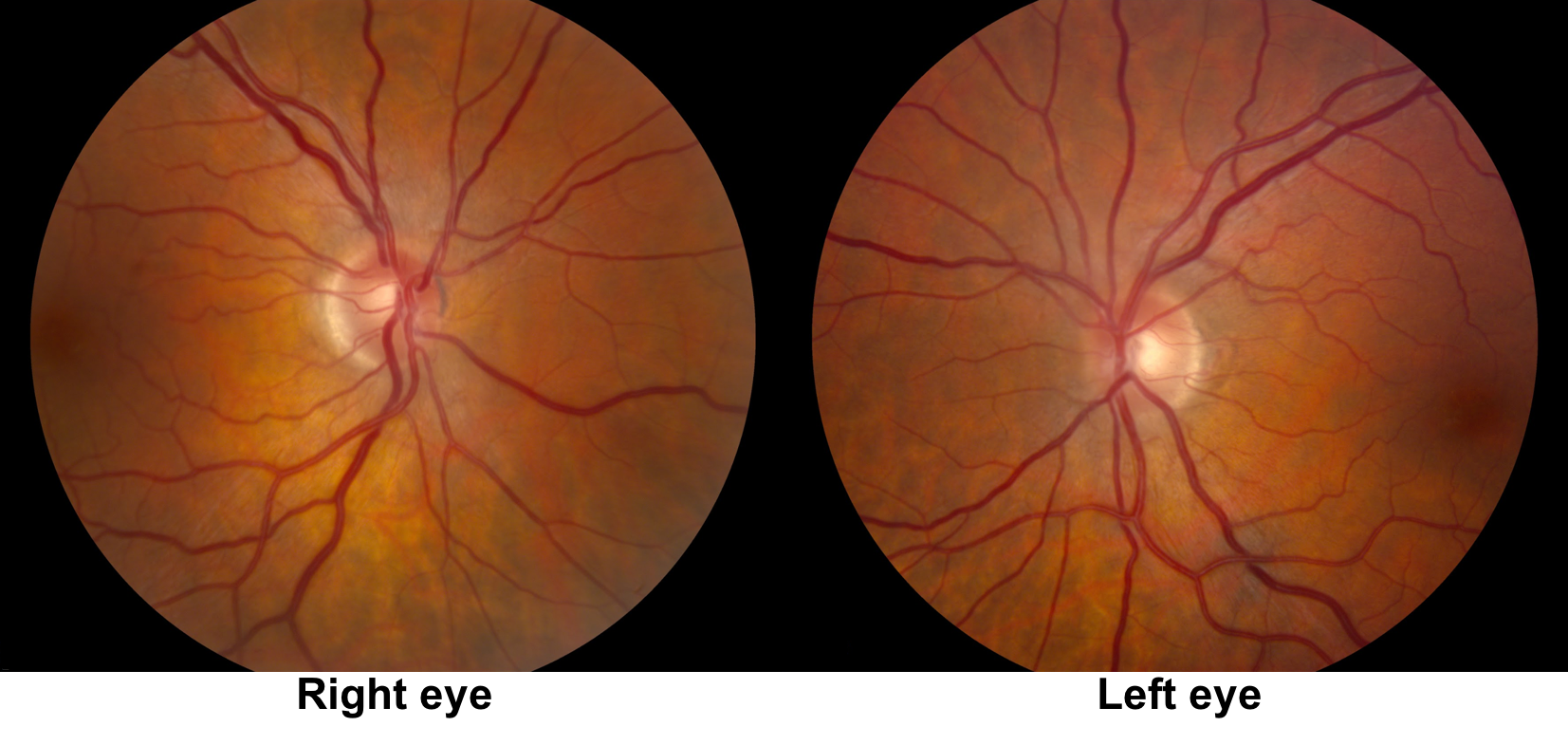
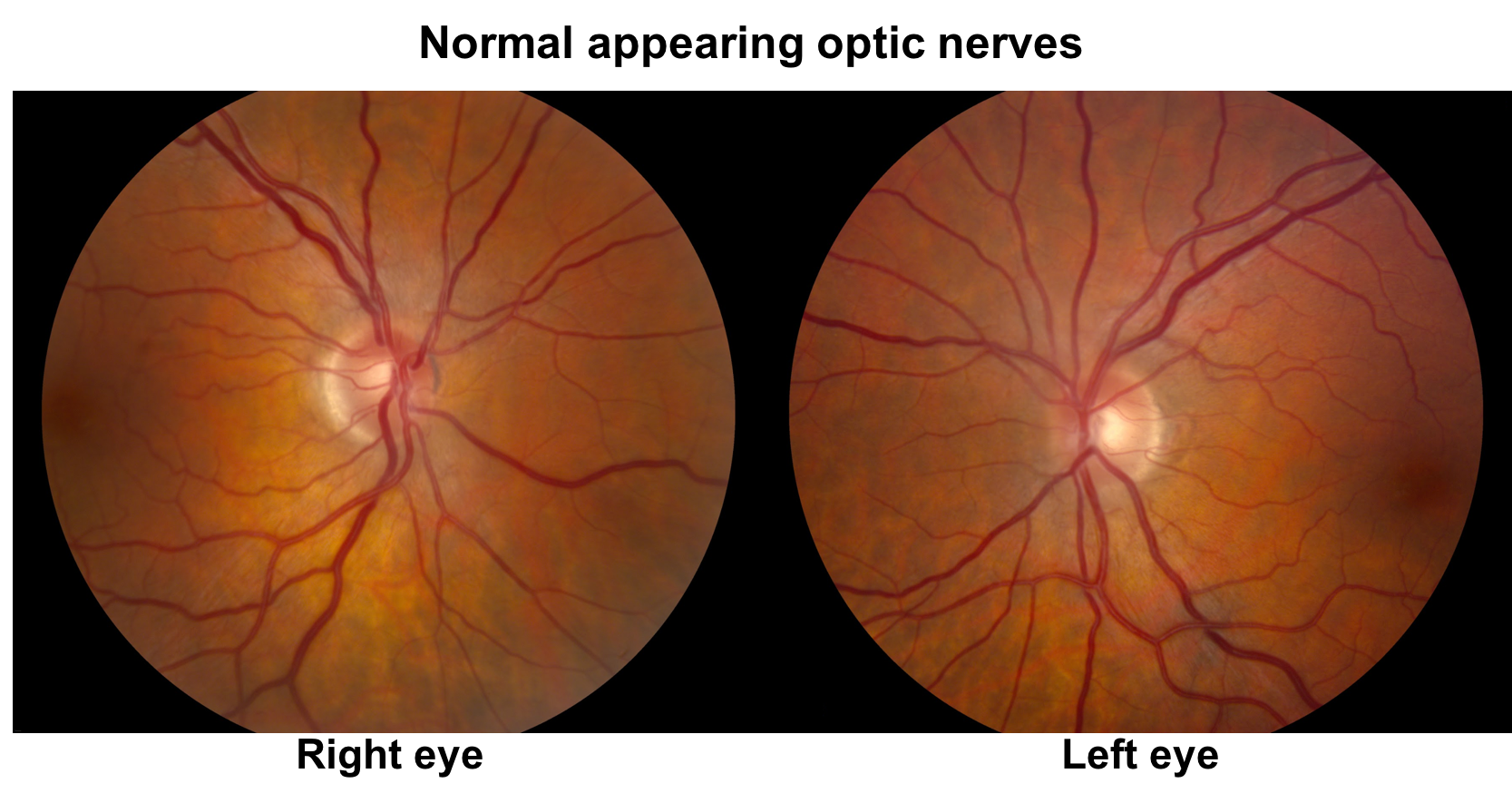
9. In a patient with unilateral or bilateral 6th nerve palsies, what other pertinent finding from the ophthalmological examination is important to document? 2. Presence of optic disc edema
Changes in intracranial pressure (ICP), either increased or decreased, may cause a 6th nerve palsy, which is a false localizing sign. Elevated ICP may lead to downward displacement of the brainstem and stretching of the 6th nerve across the sharp edge of the petrous temporal bone. A similar mechanism plays a role in patients with low intracranial pressure that can develop after lumbar puncture, shunting, or spontaneously.
Clinical Pearl
Sixth nerve palsies may be seen in the context of intracranial hypertension or hypotension.
10. What is Gradenigo’s syndrome?
- Localized inflammation of the meninges at the petrous apex
- A syndrome involving the 3rd, 4th and 6th cranial nerves
- Frequently caused by superior sagittal sinus thrombosis
- All of the above
10. What is Gradenigo’s syndrome? 1. Localized inflammation of the meninges at the petrous apex
Gradenigo’s syndrome is characterized by a 6th nerve, palsy, 7th nerve palsy and ipsilateral facial pain, photophobia, decreased corneal sensation and lacrimation (5th nerve involvement). It is classically seen in patients with severe mastoiditis as the inflammation extends to the tip of the petrous bone, producing localized inflammation of the meninges, leading to inflammation of the adjacent 5th, 6th and 7th nerves. It can also be seen with tumors, aneurysms and lateral sinus thrombosis. With the increased use of antibiotics for otitis media, the incidence of Gradenigo syndrome has greatly declined.
11. What additional sign, if present, would help localize the lesion to the right cavernous sinus?
- Gaze-evoked nystagmus on right gaze
- Right Horner’s syndrome
- Right tonic pupil
- Right optic neuropathy
11. What additional sign, if present, would help localize the lesion to the right cavernous sinus? 2. Right Horner’s syndrome
An important sign that localizes the lesion to the right cavernous sinus is the combination of an isolated 6th nerve palsy and ipsilateral Horner’s syndrome. Sympathetic fibers leave the internal carotid artery within the cavernous sinus and join with the 6th nerve for a brief time before separating off and joining the ophthalmic division of the trigeminal nerve. Involvement of this segment of the 6th nerve while it is carrying the sympathetic fibers results in this combination of findings. Documentation of the size of the pupils and presence of ptosis is important in every patient suspected of a 6th nerve palsy.
Clinical Pearl
A 6th nerve palsy and ipsilateral Horner’s syndrome localizes the lesion to the cavernous sinus.
12. What is the most common cause of a 6th nerve palsy in individuals over 50 years of age?
- Intracranial aneurysm
- Giant cell arteritis
- Pituitary adenoma
- Microvascular ischemia
12. What is the most common cause of a 6th nerve palsy in individuals over 50 years of age? 4. Microvascular ischemia
Similar to 3rd nerve palsies, the most common cause of 6th nerve palsy in older individuals is microvascular ischemia. This is usually seen in patients with vascular risk factors such as diabetes, hypertension and dyslipidemia. The natural history of microvascular 6th nerve palsies is good with full recovery typically seen within 3 months of onset. Some neuro-ophthalmologists may observe patients with an isolated abduction deficit and vascular risk factors due to a strong suspicion of a micovascular ischemic 6th nerve palsy. If the deficit does not resolve within 3 months, then an MRI of the brain and orbits should be performed.
13. A young patient is referred for a unilateral abduction deficit of unknown duration. There is narrowing of the palpebral fissure and globe retraction on attempted adduction. What is the most likely diagnosis in this patient?
- Orbital mass
- Brainstem glioma
- Duane’s syndrome
- Miller-Fisher syndrome
13. A young patient is referred for a unilateral abduction deficit of unknown duration. There is narrowing of the palpebral fissure and globe retraction on attempted adduction. What is the most likely diagnosis in this patient? 3. Duane’s syndrome
Duane’s syndrome is a congenital cranial dysinnervation disorder characterized by anomalous co-contraction of the medial and lateral rectus muscles on attempted adduction, which causes the globe to retract. Imaging studies have shown that the nucleus of the 6th cranial nerve is absent or hypoplastic and an aberrant branch of the 3rd cranial nerve innervates the lateral rectus muscle. Duane’s type I (limited abduction) should be kept in the differential diagnosis for patients with abduction deficits. For an equal amount of abduction limitation in Duane’s type I and congenital 6th nerve palsy, there is a greater amount of esotropia in primary position in patients with 6th nerve palsies. In addition, patient’s with Duane’s are typically asymptomatic. Duane’s type II is characterized by limited adduction and Duane’s type III is characterized by limited abduction and adduction.
14. A patient is referred for an esotropia and bilateral abduction deficits. When versions (movement of both eyes together) are tested, there are mild abduction deficits in both eyes. When ductions (movement of each eye individually) and oculocephalic testing is performed, there is full abduction in both eyes. There is also significant miosis with attempted abduction of either eye. What diagnosis should be considered in this patient?
- Moebius syndrome
- Spasm of the near reflex
- Tolosa-Hunt syndrome
- Congenital fibrosis syndrome
14. A patient is referred for an esotropia and bilateral abduction deficits. When versions (movement of both eyes together) are tested, there are mild abduction deficits in both eyes. When ductions (movement of each eye individually) and oculocephalic testing is performed, there is full abduction in both eyes. There is also significant miosis with attempted abduction of either eye. What diagnosis should be considered in this patient? 2. Spasm of the near reflex
Spasm of the near reflex is a nonorganic disturbance of ocular motility and alignment characterized by episodes of increased convergence, accommodation and miosis. It may be mistaken for bilateral 6th nerve palsies. The constant occurrence of miosis with adductive eye movements and full abduction with testing of ductions and oculocephalic maneuvers are highly suggestive of spasm of the near reflex. It is almost always nonorganic in nature.
15. A 70-year-old patient has a stroke involving the thalamus and is found to have an esotropia in primary position. This is because:
- There is involvement of the 6th nerve nuclei
- There is also a lesion in the medial longitudinal fasciculus (MLF)
- There is a disturbance of descending inhibitory convergence inputs
- There is a homonymous hemianopia causing decompensation of a previous phoria
15. A 70-year-old patient has a stroke involving the thalamus and is found to have an esotropia in primary position. This is because: 3. There is a disturbance of descending inhibitory convergence inputs
A number of eye movement abnormalities may be seen with lesions of the thalamus. This includes “wrong-way eyes” (conjugate gaze deviation away from the side of the lesion), sustained downward deviation of the eyes, and thalamic esotropia. Thalamic esotropia may simulate a bilateral 6th nerve palsy (“pseduo-abducens palsy”), due to interruption of inhibitory convergence pathways as they traverse the paramedian thalamus to innervate the contralateral 3rd nerve nucleus. Therefore, the esotropia would be expected in the eye contralateral to the lesion.
Case Summary
She had the new onset of binocular horizontal diplopia and examination revealed a right abduction deficit. Pupils were equal sizes and there was no ptosis, signs of intracranial hypertension, fatigability, or orbital signs. The most likely diagnosis was an isolated right 6th nerve palsy and MRI of the brain confirmed a lesion in the pons corresponding to the area of the right 6th nerve fascicle. There were other enhancing and nonenhancing white matter lesions that led to the diagnosis of multiple sclerosis. She was treated with intravenous steroids and started on disease-modifying therapy. Her double vision resolved after 3 weeks and she was tolerating her disease-modifying treatment well.
Further reading:
-
Thompson AJ, Banwell BL, Barkhof F, et al. Diagnosis of multiple sclerosis: 2017 revisions of the McDonald criteria. Lancet Neurol 2018 http://www.thelancet.com/journals/laneur/article/PIIS1474-4422(17)30470-2/fulltext
-
Bruce BB, Newman NJ, Biousse V. Ophthalmoparesis in idiopathic intracranial hypertension. Am J Ophthalmol 2006;42(5):878-80. https://www.ncbi.nlm.nih.gov/pubmed/17056379
-
Kung NH, Van Stavern GP. Isolated ocular motor nerve palsies. Semin Neurol 2015;35(5):539-48. https://www.ncbi.nlm.nih.gov/pubmed/26444399
-
Ghasemi M, Riaz N, Bjornsdottir A, Paydarfar D. Isolated pseudoabducens palsy in acute thalamic stroke. Clin Imaging 2017;43:28-31. https://www.ncbi.nlm.nih.gov/pubmed/28167284
-
Elder C, Hainline C, Galetta SL, Balcer LJ, Rucker JC. Isolated abducens nerve palsy: update on evaluation and diagnosis. Curr Neurol Neurosci Rep 2016;16(8):69. https://www.ncbi.nlm.nih.gov/pubmed/27306521