14
Case
Age: 63-year-old white man
Reason for referral to ophthalmology: Transient monocular vision loss
Past medical history: Type 2 diabetes, hypertension, dyslipidemia
Past ocular history: None
Medications: Metformin, amlodipine, hydrochlorothiazide, atorvastatin
Habits: Smokes 1 pack of cigarettes per day for 30 years, does not drink alcohol
HPI: For the past 2 days, he has had episodes of transient loss of vision in his right eye that lasted a few minutes. He saw a grey shadow that started in his superior visual field that lifted up after a minute or two and his vision returned to baseline shortly afterwards. He had 4 episodes in the past 2 days. He presented to the emergency room and an ophthalmology consultation was requested.
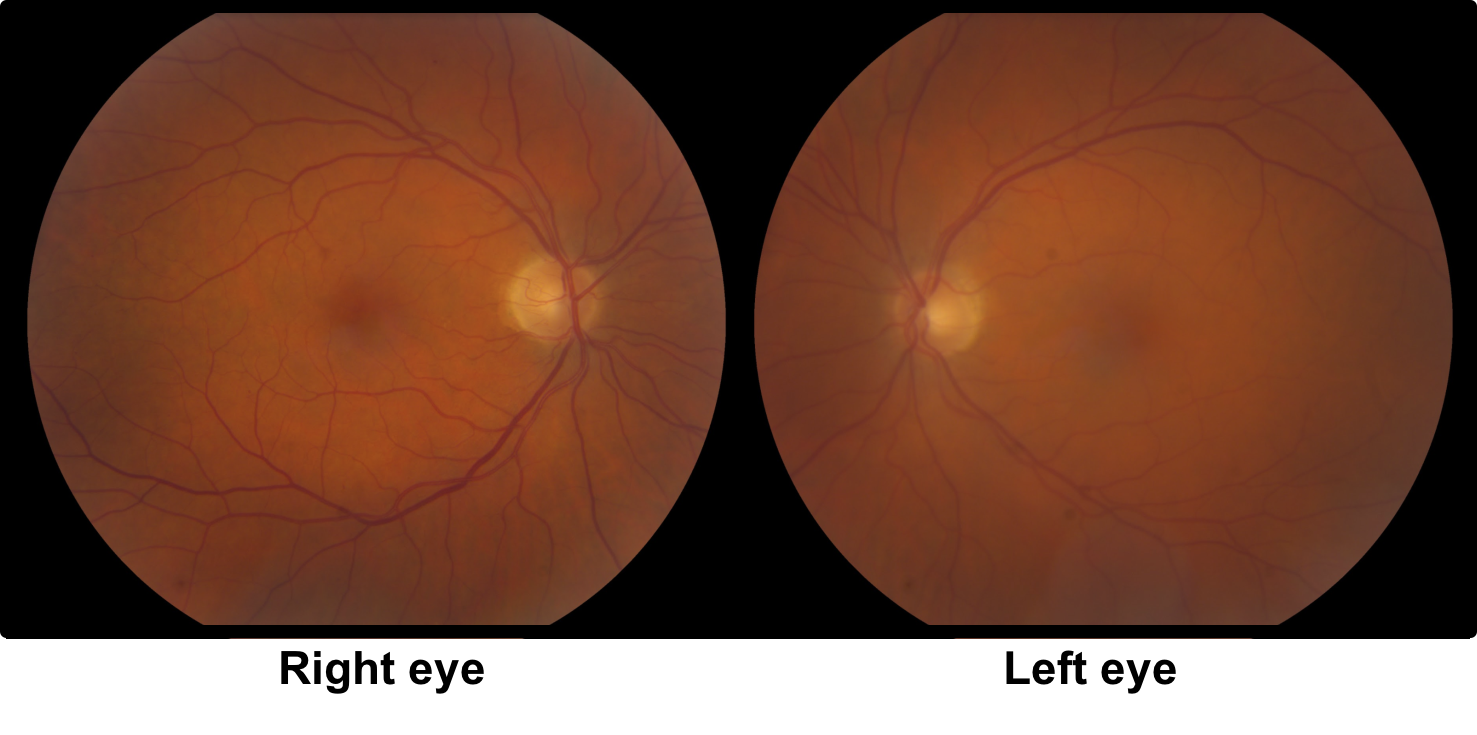
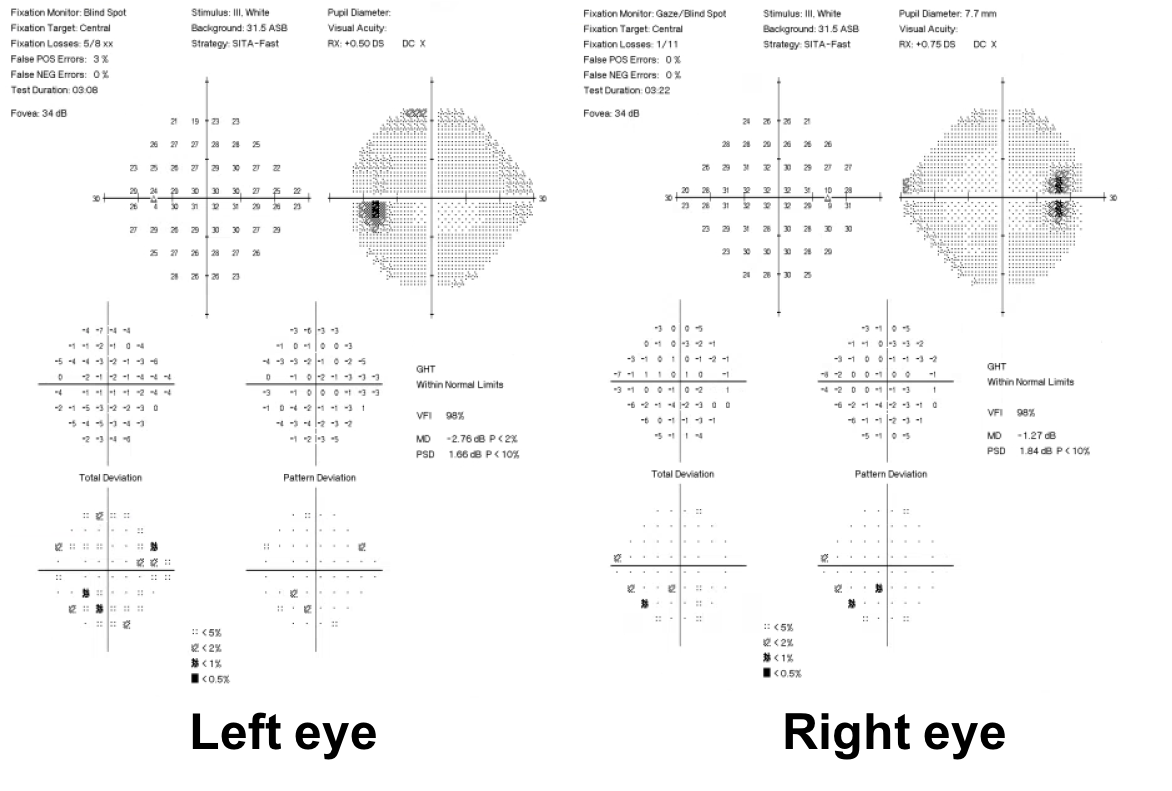
Ophthalmological examination:
Blood pressure: 163/89, heart rate 80
Visual acuity is 20/20 OD and 20/20 OS
Pupils are equal sizes and reactive to light, there is no RAPD
Color vision: 14/14 correct Ishihara plates in both eyes
Ocular motility and alignment are normal
Neurological examination is normal
1. What are the most important blood tests to obtain at this time?
- Hemoglobin A1c
- LDL, HDL and total cholesterol
- Liver function tests
- CBC, ESR, and CRP
1. What are the most important blood tests to obtain at this time? 4. CBC, ESR, and CRP
In this 63-year-old patient with transient monocular vision loss, giant cell arteritis must be considered in the differential diagnosis. In patients with ischemic optic neuropathy from giant cell arteritis, transient vision loss preceded permanent vision loss in 7-18% of patients. Therefore, a CBC, ESR, and CRP are indicated in this patient at this time.
Clinical Pearl
Any patient over 50 years of age with transient monocular vision loss must be evaluated for giant cell arteritis.
2. If giant cell arteritis is suspected, what further testing in the eye clinic might be helpful?
- B-scan ultrasound
- OCT of the macula
- Fluorescein and indocyanine green angiography
- Corneal topography
2. If giant cell arteritis is suspected, what further testing in the eye clinic might be helpful? 3. Fluorescein and indocyanine green angiography
Delayed or absent filling of the choroid is a useful way of differentiating arteritic from non-arteritic causes of vision loss. Extremely poor filling of the choroid has been reported in patients with arteritic ischemic optic neuropathy (one study found 69 seconds from first appearance to filling in GCA patients compared to 5.5 seconds in patients with non-arteritic ischemic optic neuropathy). Choroidal perfusion defects in this patient may be seen despite a normal examination and would increase the suspicion for giant cell arteritis. This patient had normal fluorescein and indocyanine green angiography.
The results of the bloodwork are shown below:
Hemoglobin 133 g/L (normal 135-175g/L)
WBC 7.2 x 109/L (normal 4.0-11.0 x 109/L)
Platelets 348 x 109/L (normal 150-400 x 109/L) Normal
ESR 15 mm/h (normal is (age/2) Normal
CRP 2.1 mg/L (normal <5 mg/L) Normal
3. What neuroimaging is the best choice for this patient?
- CT scan of the head with contrast
- MRI of the brain and MRA of the head and neck
- MRI of the orbits with fat suppression
- None of the above
3. What neuroimaging is the best choice for this patient? 2. MRI of the brain and MRA of the head and neck
In this patient with sudden, transient monocular vision loss, vascular imaging of the head and neck. should be performed with either a CTA or MRA. The choice of CTA or MRA will depend on availability and the preference of the neuroradiologist.
4. If this patient was seen in a community eye clinic, how should this neuroimaging and stroke workup be obtained?
- Arranged as an outpatient with his primary care provider
- Immediately in the emergency room or rapid stroke clinic
- Ordered as an outpatient by an ophthalmologist
- Ordered an an outpatient with a non-urgent neurology consultation
4. If this patient was seen in a community eye clinic, how should this neuroimaging and stroke workup be obtained? 2. Immediately in the emergency room or rapid stroke clinic
The characteristics of this patient’s transient vision loss are very concerning for a retinal transient ischemic attack (TIA). If this is the case, the patient is at high risk of a stroke and there is a short window of opportunity for prevention. A study that analyzed four cohorts of patients who had a recent ischemic stroke found that TIAs occurred most often in the 48 hours prior to the stroke. In another study, the risk of stroke after a TIA was found to be approximately 5 percent within 24 hours. Therefore, the emergency room or rapid stroke clinic is the best way to evaluate this patient. Waiting for an outpatient workup would result in an unacceptably high risk of stroke in this patient.
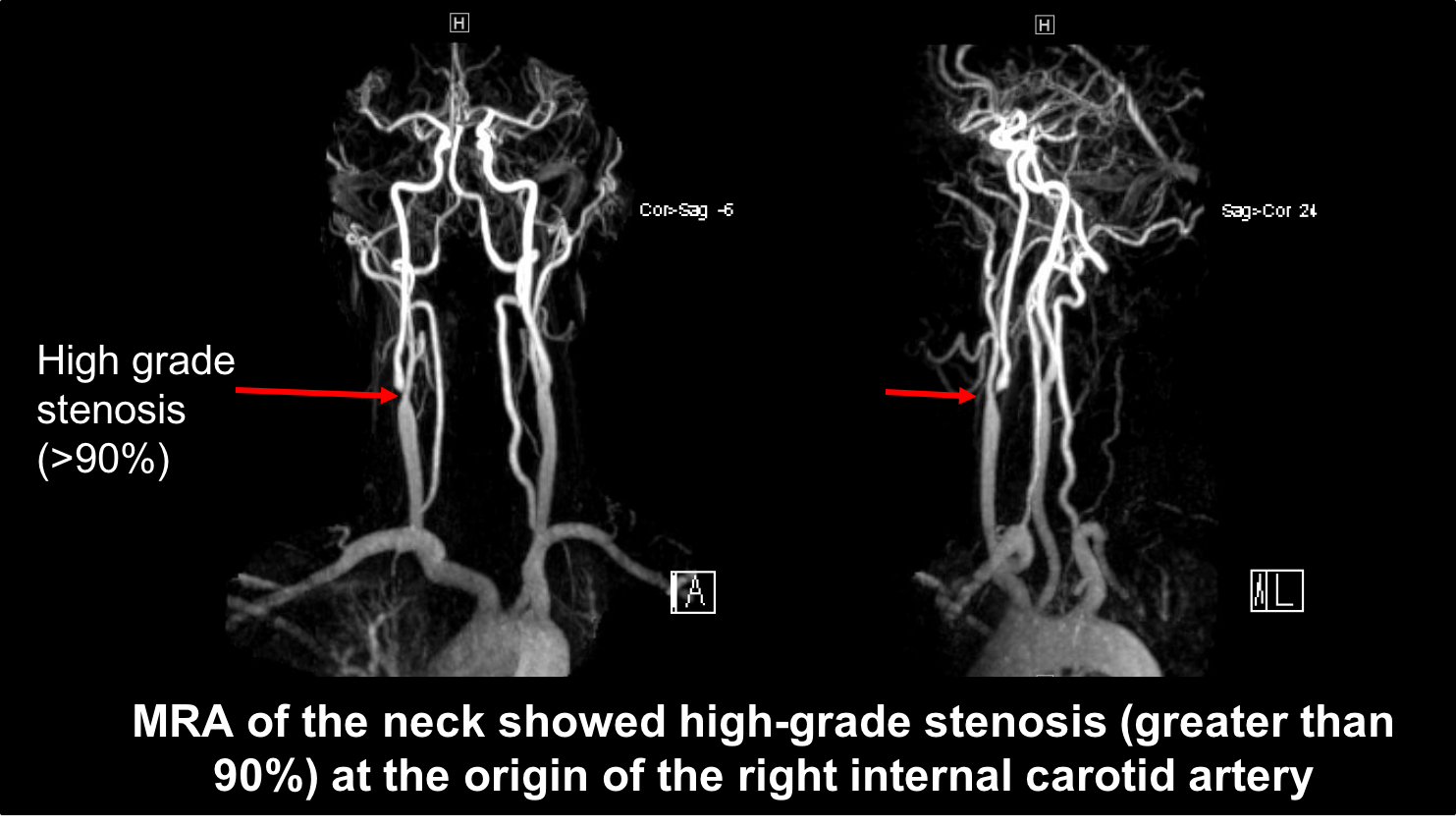
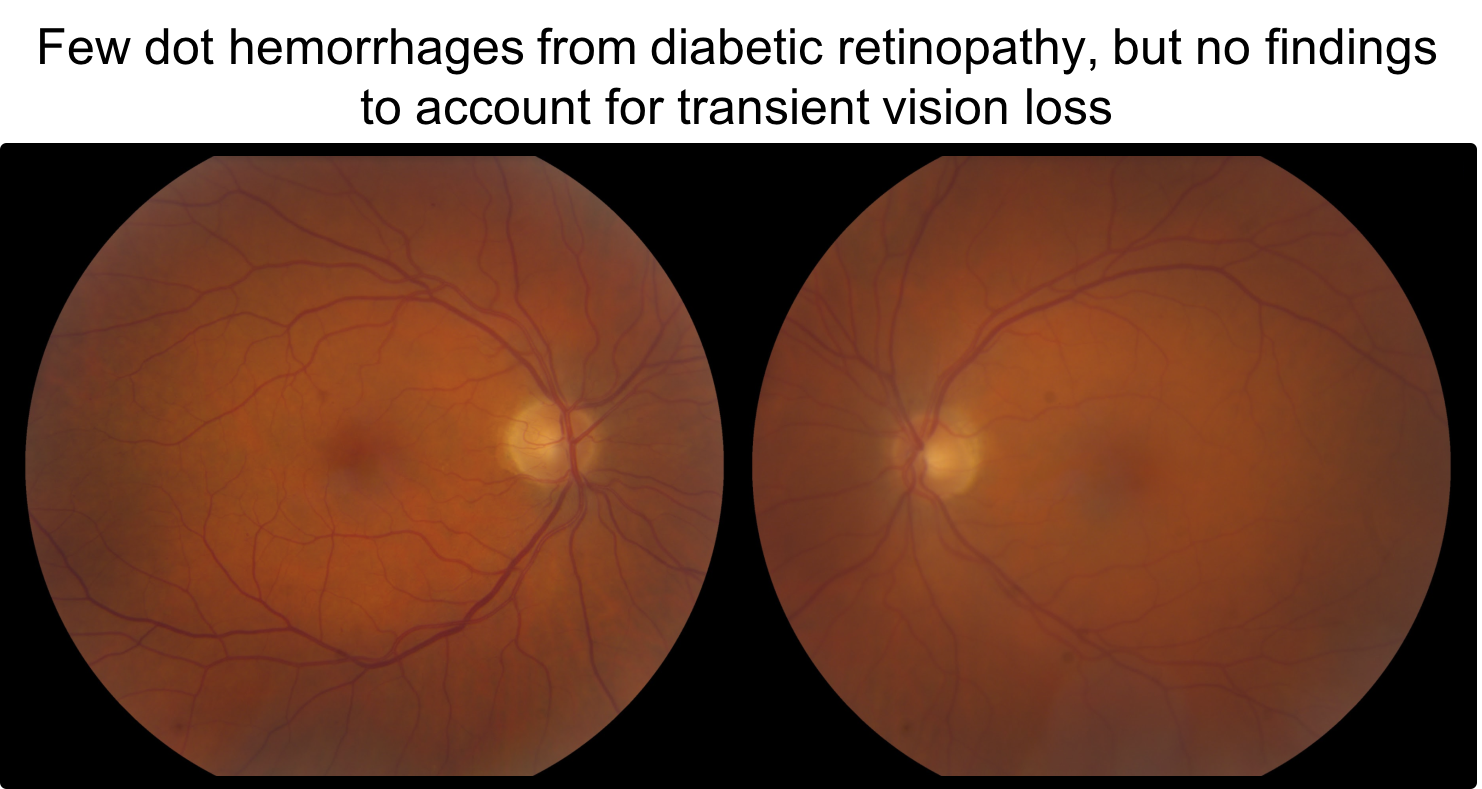
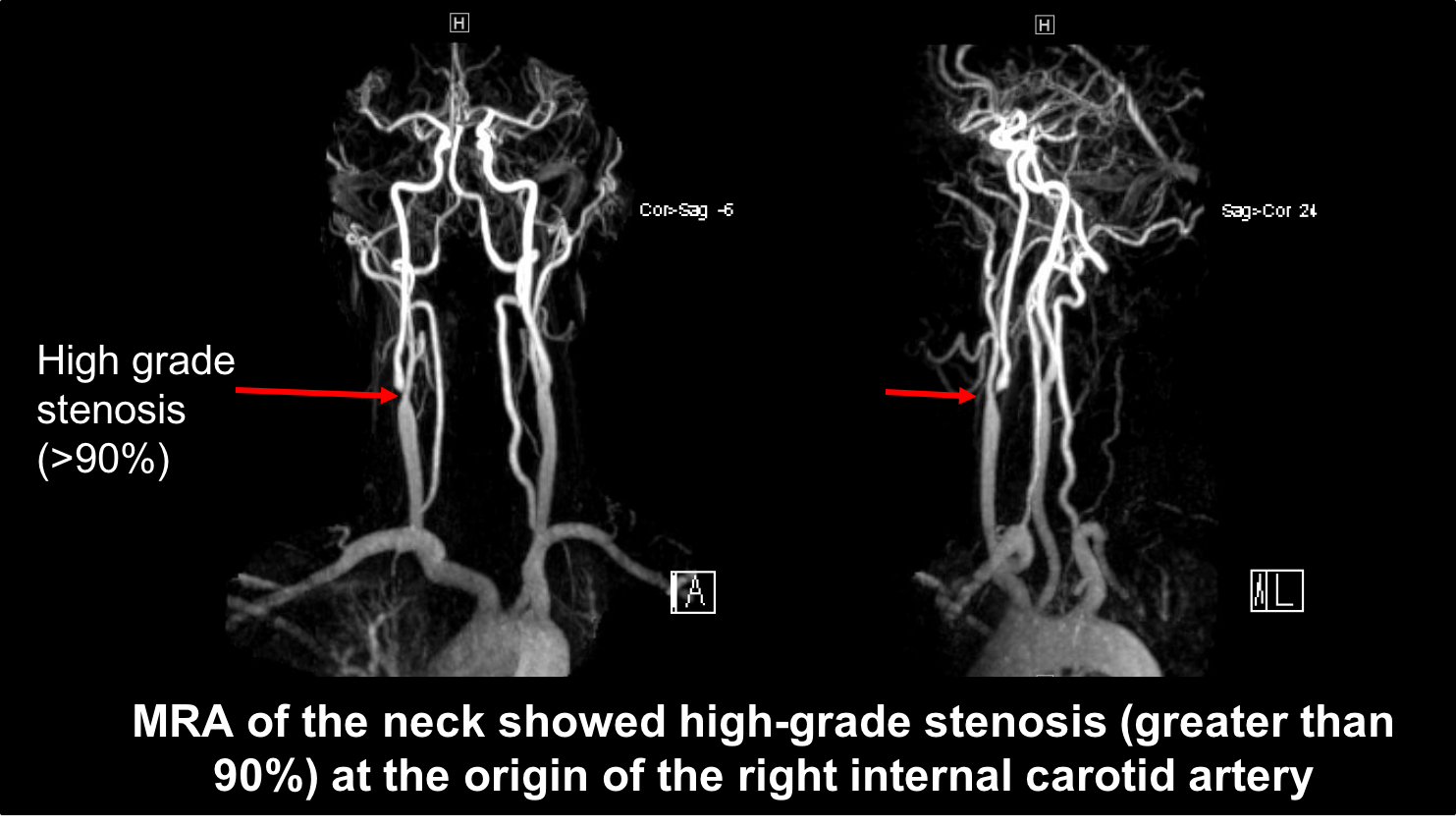
This patient had normal inflammatory blood markers and a high-grade stenosis in the right internal carotid artery (shown below).
4. What treatment is indicated in this patient?
- Intravenous corticosteroids
- Carotid endarterectomy
- Acetazolamide
- Topical brimonidine
4. What treatment is indicated in this patient? 2. Carotid endarterectomy
In this patient with symptomatic high-grade (>70%) stenosis of the internal carotid artery, carotid endarterectomy is indicated to reduce the future risk of stroke. This was shown by the NASCET trial that compared conventional medical therapy to carotid endarterectomy in patients with transient monocular vision loss, hemispheric transient ischemic attack, or hemispheric mild stroke. This study found that carotid endarterectomy considerably reduced the risk of ipsilateral stroke if carotid stenosis was greater than 70%. In patients who are poor surgical candidates, endovascular stenting may also be considered.
Clinical Pearl
Carotid endarterectomy is indicated in symptomatic patients with greater than 70% stenosis of the internal carotid artery.
Carotid endarterectomy is contraindicated in patients with complete occlusion (100%) of the internal carotid artery.
5. A new patient had a transient right homonymous hemianopia from an embolus in the posterior circulation. Why did she report that she had transient vision loss only in the right eye?
- The temporal visual field is larger
- The left eye is her dominant eye
- The temporal visual field has greater contrast sensitivity
- Her right eye likely has a larger pupil size
5. A new patient had a transient right homonymous hemianopia from an embolus in the posterior circulation. Why did she report that she had transient vision loss only in the right eye? 1. The temporal visual field is larger
It may be difficult for patients to recall if their transient vision loss was in one eye or both eyes and they often do not cover each eye to check during the episode. Few patients will realize that a transient homonymous visual field defect occurred in both eyes and usually localize the vision loss to the eye with the temporal visual field, which is larger than the nasal visual field. Clues to differentiate monocular from binocular vision loss include reading impairment, which usually does not occur with monocular vision loss, and vision loss confined to a vertical hemifield, which usually does not occur with monocular vision loss.
6. A patient has transient vision loss in both eyes for only a few seconds with changes in position such as getting up from a seated position or bending over. What examination finding is most likely to be found?
- Narrow angles
- Corneal edema
- Bilateral optic disc edema
- Subretinal fluid
6. A patient has transient vision loss in both eyes for only a few seconds with changes in position such as getting up from a seated position or bending over. What examination finding is most likely to be found? 3. Bilateral optic disc edema
Bilateral transient vision loss for a brief period (seconds) may be reported in patients with papilledema, optic disc drusen or anomalous optic discs and is usually referred to as transient visual obscurations. This is likely a result of a transient reduction in perfusion pressure to the optic nerves. A dilated examination should be performed in patients with this complaint with careful attention to the appearance of the optic nerves.
7. A patient reports several episodes of painless transient vision loss in his right eye that lasted 30 minutes to 2 hours. What examination finding is most likely to be found?
- Narrow angles
- Posterior subcapsular cataract
- Diabetic retinopathy
- Tortuous retinal venules
7. A patient reports several episodes of painless transient vision loss in his right eye that lasted 30 minutes to 2 hours. What examination finding is most likely to be found? 4. Tortuous retinal venules
Transient vision loss may be seen in the context of an impending central retinal vein occlusion. Typically the vision loss is longer (15 minutes to few hours) than that seen with transient monocular vision loss from an arterial source (1 to 30 minutes). Dilated retinal venules may be the only clue to this diagnosis. Patients may come back later with an established central retinal vein occlusion.
8. A patient with transient monocular vision loss has a refractive, yellow cholesterol embolus seen at the bifurcation of a major retinal arteriole. What is the most likely source of this embolus?
- Carotid artery
- Heart valves
- Aorta
- Superior vena cava
8. A patient with transient monocular vision loss has a refractive, yellow cholesterol embolus seen at the bifurcation of a major retinal arteriole. What is the most likely source of this embolus? 1. Carotid artery
Retinal emboli may originate from various sources (summarized below). Since this is a cholesterol embolus, the most likely source is the common or internal carotid artery.
-
- Cholesterol emboli (Hollenhorst plaque) classically originate from the common or internal carotid artery. They usually have a yellow or orange color, refractile or rectangular appearance and are most frequently located at major vessel bifucations.
- Platelet-fibrin emboli classically originate from the walls of atherosclerotic vessels and heart valves. They have a dull grey-white color, a long smooth shape, and a concave meniscus at each end.
- Calcium emboli classically originate from the heart or large vessels. They are large, have a chalky white appearance, a round shape and lodge at the first or second vessel bifurcation.
9. How could a transient right homonymous hemianopia from transient right occipital lobe ischemia be accounted for by an embolus that originated in the right internal carotid artery?
- Anteriorly displaced basilar artery
- Persistent fetal origin of the posterior cerebral artery
- Hypoplastic anterior communicating artery
- Dominant right carotid artery
9. How could a transient right homonymous hemianopia from transient right occipital lobe ischemia be accounted for by an embolus that originated in the right internal carotid artery? 2. Persistent fetal origin of the posterior cerebral artery
A common anatomical variant is a persistent fetal origin of the posterior cerebral artery from the internal carotid artery. This anatomic variation may be unilateral or bilateral and has a prevalence of up to 30%. In these cases, the fetal circulation persists into adulthood with hypoplastic development of the vertebrobasilar circulation with a predominant supply of the posterior cerebral artery from the anterior circulation via the internal carotid artery and dominant posterior communicating artery. Evaluation of the carotid arteries is important in patients with retrochiasmal vision loss if there is a fetal posterior cerebral artery.
10. A patient has transient blurry vision when she goes for a run and her body temperature rises. She likely has a history of:
- Epilepsy
- Multiple sclerosis and previous optic neuritis
- Previous stroke
- Optic nerve hypoplasia
10. A patient has transient blurry vision when she goes for a run and her body temperature rises. She likely has a history of: 2. Multiple sclerosis and previous optic neuritis
This patient has Uhtoff’s phenomenon, which is a transient visual blurring during exercise, during an elevation of body temperature, or during emotional distress in patients with multiple sclerosis or other demyelinating conditions. Uhthoff’s phenomenon was reported by about 10% of patients after 6 months in the Optic Neuritis Treatment Trial and is more common in patients that have had optic neuritis and have multiple sclerosis, although it can also be seen in otherwise healthy patients that have had demyelinating optic neuritis. This may be due to conduction block that occurs as the body temperature increases and is reached at a lower point in demyelinated nerves.
11. A 25-year old woman has vision loss in her right eye that developed over 2 days. She went to an ophthalmologist and was found to have a right RAPD and a right inferior altitudinal visual field defect. She was referred to a neuro-ophthalmologist, who repeated the visual field 3 months later, and it was found to be normal. The visual field from her initial and follow-up visits are shown below. What is the most likely reason for this transient altitudinal visual field defect?
- Non-organic vision loss
- Resolved non-arteritic anterior ischemic optic neuropathy (NAION)
- Optic neuritis
- Different visual fields were performed so they cannot be compared
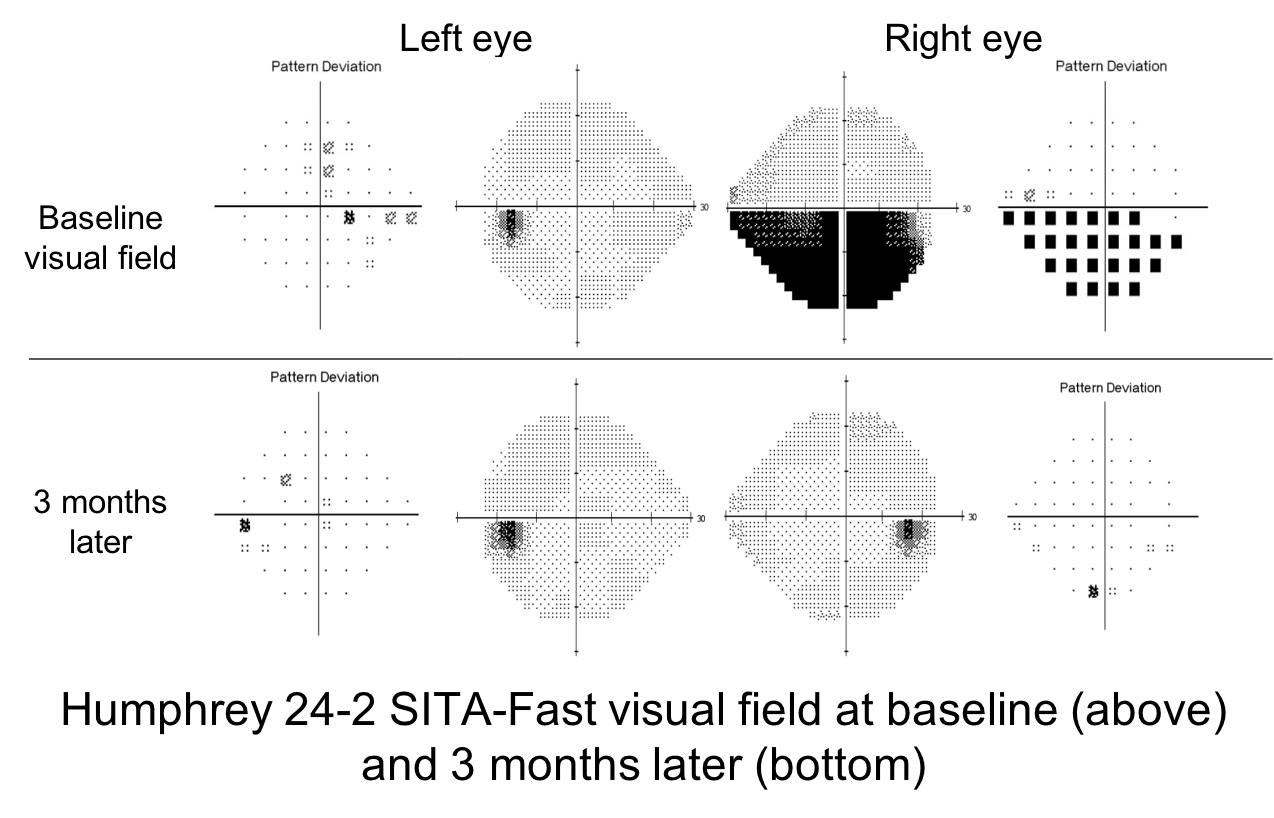
11. A 25-year old woman has vision loss in her right eye that developed over 2 days. She went to an ophthalmologist and was found to have a right RAPD and a right inferior altitudinal visual field defect. She was referred to a neuro-ophthalmologist, who repeated the visual field 3 months later, and it was found to be normal. The visual field from her initial and follow-up visits are shown below. What is the most likely reason for this transient altitudinal visual field defect? 3. Optic neuritis
This young woman had a right RAPD and inferior altitudinal visual field defect at her initial presentation, indicating a right optic neuropathy. Non-organic vision loss and corneal ulcers do not cause an RAPD. Non-arteritic anterior ischemic optic neuropathy and optic neuritis may cause an altitudinal defect but visual defects from NAION do not completely resolve, whereas visual field defects from optic neuritis resolve in the large majority of cases. Therefore, the most likely diagnosis is a right typical optic neuritis. The patient should have a full neurological examination and an MRI of the brain to to assess for multiple sclerosis.
12. A 60-year old woman had a gradual decrease in the central vision of her right eye over 1 week that remained stable and then returned to normal 4 weeks later. She was examined by an ophthalmologist within a few days of her vision loss and had a normal examination including no RAPD and normal Humphrey 24-2 visual fields. An MRI of the brain and orbits was performed and was normal. Where does her monocular transient vision loss localize?
- Right cornea
- Right lens
- Right macula
- Right optic nerve
12. A 60-year old woman had a gradual decrease in the central vision of her right eye over 1 week that remained stable and then returned to normal 4 weeks later. She was examined by an ophthalmologist within a few days of her vision loss and had a normal examination including no RAPD and normal Humphrey 24-2 visual fields. An MRI of the brain and orbits was performed and was normal. Where does her monocular transient vision loss localize? 3. Right macula
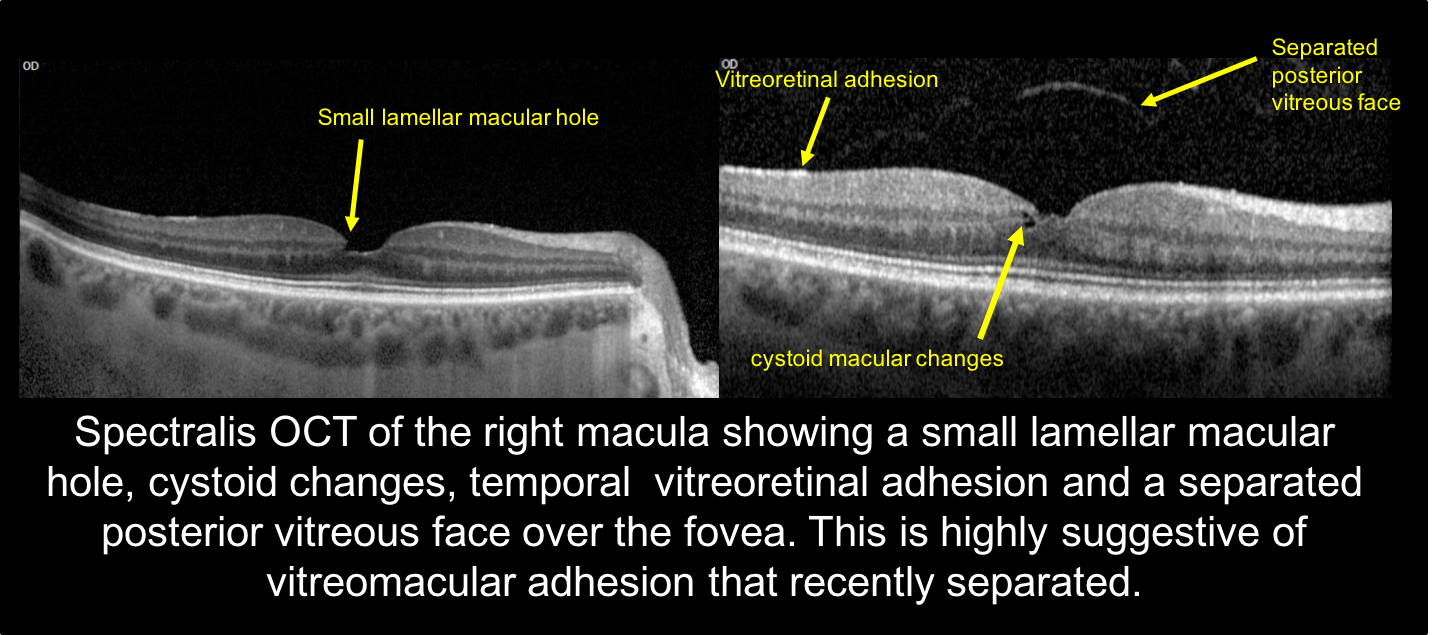
This patient had transient central vision loss in one eye for about 5 weeks. Since the vision loss was only in the right eye, the process localizes to the right optic nerve or right macula. She had no RAPD and normal visual fields during the vision loss episode, localizing the process to the right macula. An OCT of the macula after her vision recovered showed a small lamellar macular hole, an area of vitreoretinal adhesion temporal to the fovea and an separated posterior vitreous face over the fovea. These changes are highly suggestive of vitreomacular traction that resolved (OCT shown below).
13. A 30-year-old man with a past medical history of a recent asthma exacerbation and steroid use developed right eye central vision loss. His vision returned to normal after 3 months. If an OCT of the macula was performed when he had vision loss, what was most likely to have been seen?
- Cystoid macular edema
- Subretinal fluid
- Epiretinal membrane
- Macular hole
13. A 30-year-old man with a past medical history of a recent asthma exacerbation and steroid use developed right eye central vision loss. His vision returned to normal after 3 months. If an OCT of the macula was performed when he had vision loss, what was most likely to have been seen? 2. Subretinal fluid
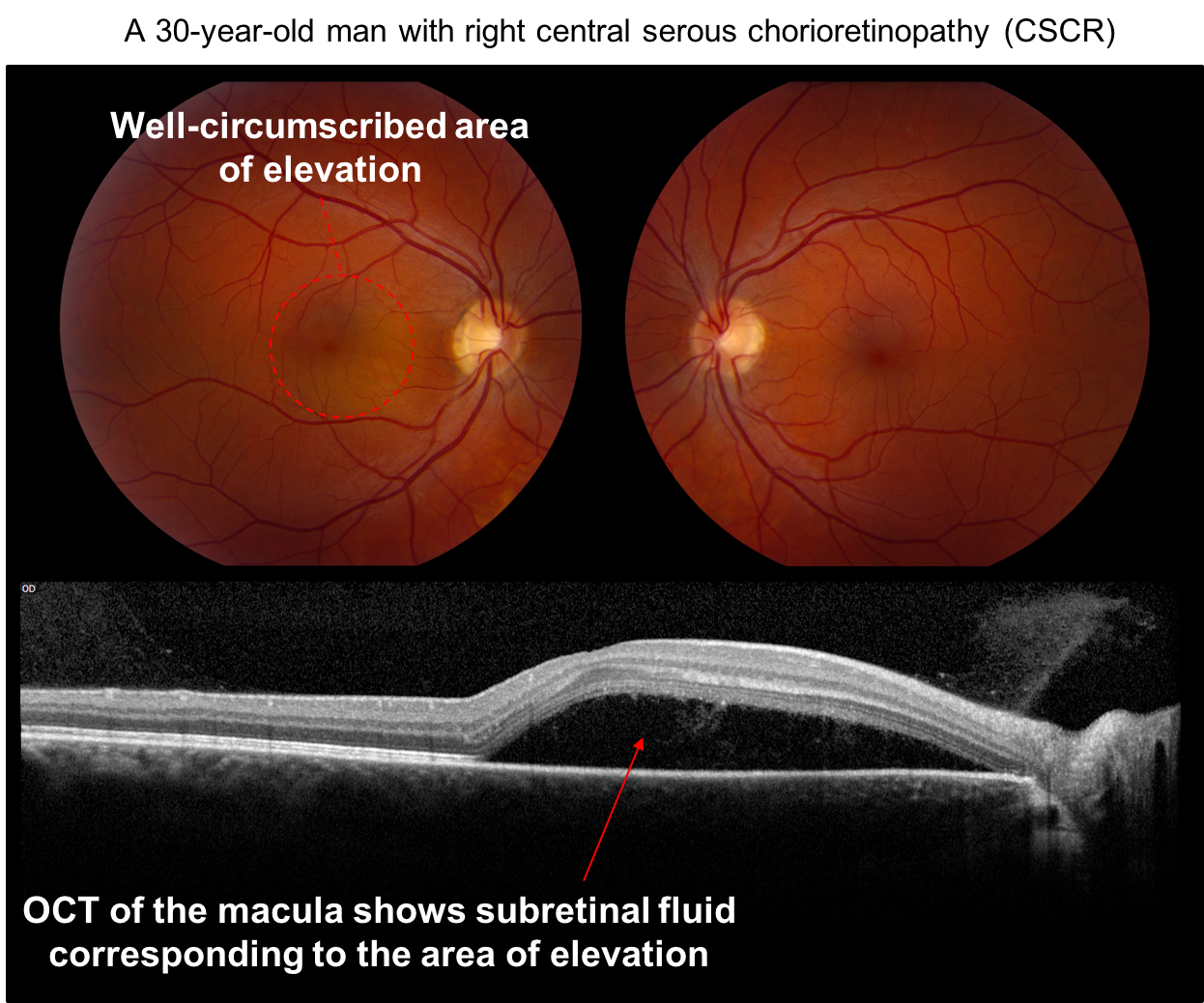
This patient most likely had central serous chorioretinopathy (CSCR), which is an idiopathic condition characterized by well-circumscribed, serous detachments of the reitna. It is most often seen in young men (age 25 to 55) and use of exogenous steroids, endogenous hypercortisolism, and pregnancy are risk factors. Optical coherence tomography is an excellent noninvasive tool used for diagnosis and monitoring and demonstrates subretinal fluid, retinal pigment epithelial detachments and choroidal thickening. Most patients spontaneously recover vision after 3-4 months. Fundus photos and OCT of the macula from a patient with CSCR are shown below.
Case Summary
He presented with transient vision loss in the right eye that lasted a few minutes. Dilated fundus examination was normal but MRA showed high-grade stenosis of the right internal carotid artery. He underwent carotid endarterectomy and had no further recurrence of his symptoms.
Further reading:
-
Biousse V, Nahab F, Newman NJ. Management of acute retinal ischemia: Follow the guidelines! Ophthalmology 2018 https://www.ncbi.nlm.nih.gov/pubmed/29716787
-
Ahmed R, Foroozan R. Transient monocular vision loss. Neurol Clin 2010;28:619-629. http://www.neurologic.theclinics.com/article/S0733-8619(10)00042-3/abstract
-
Miller N. Embolic causes of transient monocular visual loss. Ophthalmol Clin North Am 1996;9:359–80.
-
Rothwell PM, Warlow CP. Timing of TIAs preceding stroke: time window for prevention is very short. Neurology 2005;54(5):817. https://www.ncbi.nlm.nih.gov/pubmed/15753415
-
Chandratheva A, Mehta Z, Geraghty OC, et al. Population-based study of risk and predictors of stroke in the first few hours after a TIA. Neurology 2009;72(22):1941. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2690971/