Chapters
“While we teach, we learn” —Seneca
Precepting is an organized, evidence-based, outcome-driven approach to assuring competent practice (Eley, 2015). Clinical heath education often employees a preceptor model for senior practicum courses and frequently as part of orienting new employees. Through clinical experiences and orientation activities, learners acquire knowledge and essential skills for professional practice. The preceptor plays a vital role in developing students as professionals and a critical role in successfully integrating new staff.
For student learners, a representative from the student’ institution is often part of the teaching–learning team along with the student and a preceptor who is an employee of the clinical agency. Each member of the trio usually has specific roles and responsibilities, with the faculty representative often supporting and advising the preceptor. While the preceptor has important roles in student evaluation, the faculty member usually makes critical decisions on final grades and on whether a learner passes or fails a practicum.
Being a preceptor for a student or new employee is an essential role but not one for which most preceptors are formally prepared. The short- and long-term success of the student or employee can be enhanced greatly by an excellent preceptor or affected negatively by a preceptor who is not well prepared for the role. The goal of this chapter is to provide readers with knowledge, skills and attitudes that are key to being an effective preceptor in the clinical setting. As with most careers, when you are well prepared and able to excel in a role, those you work with are positively affected. As you carry out your role well, your level of satisfaction with the role is also enhanced. This leads to a positive cycle with affirmative effects on all involved, including recipients of care.
This chapter discusses the difference between preceptoring and mentoring, examines the theoretical foundations of effective preceptoring, and presents strategies for becoming and being a successful preceptor. We conclude with a discussion of the preceptor–preceptee relationship. The strategies included provide a road map for practitioners who are new to precepting. The chapter is infused with practical creative ideas and founded on theory, making it both a stand-alone chapter for educators embarking on being a great preceptor and part of the greater understanding of becoming skilled as a clinical educator.
The Difference Between a Mentor and a Preceptor
The origin of the concept of mentorship is well documented. In Homer’s Odyssey a Mentor, a wise and trusted friend of Odysseus, takes on the rearing of Odysseus’ son in his absence (Roberts, 1999). The mentor is depicted as an older, wiser male who takes on the responsibility for a younger male’s learning and development, acting rather like a guardian. The term mentor is traditionally associated with professions such as medicine, law and business, but it began appearing in nursing literature in the 1990s (Andrews & Wallis, 1999).
Much of the current mentor literature focuses on defining the concept, yet a precise and complete definition that is universally embraced remains elusive (Dawson, 2014; Gopee, 2011; Mentoring Resources, n.d.). To confuse it further, terms such as preceptor, coach and facilitator are used interchangeably in some instances. In jurisdictions such as Great Britain, practicing nurses who are responsible for students in the clinical area are called mentors, while in most North American jurisdictions, these supervising nurses are called preceptors. Commonly the term mentor is reserved for a longer-term personal development relationship between a less experienced and a more experienced person, with the focus of the relationship being assistance, befriending, guiding and advising (Eby, Rhodes & Allen, 2007). More concisely the mentor is less focused on assessment and supervision and more focused on the mentee’s well-being and career advancement (Eby, Rhodes & Allen, 2007).
In contrast a preceptor–preceptee relationship is usually shorter term and the preceptor has responsibility for teaching and assessing clinical performance. In the base definition of preceptor, the focus of the preceptor’s work is to uphold a precept or law or tradition. Myrick & Yonge (2005, p. 4) define a nursing preceptor as a skilled practitioner who oversees students in a clinical setting to facilitate practical experience with patients.
The roles of mentor and preceptor do overlap. For example, a preceptor who has no concern for the well-being of the preceptee is not likely to provide the learner with a positive clinical experience. Likewise a mentor who does not assess student practice will not have the information needed to be an effective mentor. The assessment in which a mentor engages is more likely to be formative in nature and focused on providing the mentor with knowledge to fulfill the role of guide effectively.
Students in practice-based health care professions rely on others to support, teach and supervise them in practice settings. The underlying rationale for this approach to learning is the belief that working alongside practitioners aids students to become safe caregivers who are successfully socialized to the clinical world (Benner, 1984). In this chapter we focus on the role of the preceptor.
Theoretical Foundations of Effective Preceptoring
Effective preceptoring of students in health care clinical environments can be understood by briefly examining adult learning theory, transformational learning theory, and the novice to expert model. Here we outline each theory or model and discuss each in relation to the preceptoring literature.
Adult Learning Theory
As described in chapter 1, Malcolm Knowles (1984) is credited with naming the theory of andragogy, a theory specifically for adult learning. Andragogy emphasizes how adult learners differ from child learners in being self-directed and taking responsibility for their learning decisions. Further, according to Knowles, adults want to know why they are learning something, need to learn experientially (including having the opportunity to make mistakes), use problem-solving to learn, and learn most effectively if they can apply what they learn immediately. Knowles states that adults learn best if their teacher is primarily a facilitator or resource person. Smith (2002) further discusses Knowles’ andragogy theory, highlighting the ideas that a) learners move from being dependent to self-directed, b) learners accumulate a reservoir of experience and knowledge, and c) a learner’s motivation to learn is internal. Given these principles of adult learning, teaching strategies such as simulations, role-play and case studies are considered useful. Likewise, clinical practicum learning opportunities with the student working alongside a preceptor are compatible with the principles of andragogy. Practicum students are directed by a more knowledgeable person (the preceptor) until they can accumulate experience and knowledge to be independent practitioners.
Sandlin, Wright & Clark (2013) further our understanding of Knowles’ theory by additional focus on Knowles’ beliefs that adult learners are autonomous, rational and capable of action, and on the assumption that autonomy and rationality are desirable and attainable in adult learners. Their perspective on Knowles’ fundamental views provides an interesting contrast in considering the role of preceptor in the clinical environment. The tenets of Knowles’ adult learning theory offer no substantive role for the preceptors who hold responsibility for overseeing, guiding and evaluating the work of the preceptee, as learners are thought to be totally autonomous and capable of independence. In contrast, as Sandlin, Wright & Clark (2013) propose, adult learners may actually be at various levels of autonomy and rationality and thus a skilled preceptor does have a role in adult learning.
Transformational Learning Theory
As explained in chapter 1, Jack Mezirow (1995) is credited with making significant contributions to the theory of transformative learning. The essence of this theory is that learners must engage in critical reflection on their experiences in order to transform their beliefs, attitudes and perspectives, which Mezirow terms their meaning schemes. Others have critiqued some of Mezirow’s assumptions and views. Boyd & Myers (1988) note that learners must be open to changing their meaning schemes; to adopt new perspectives, they must realize that their old perspectives are no longer relevant. Dirkx, Mezirow & Cranton (2006) emphasize the self-actualization possibilities of transformative learning with the statement “learning is life – not a preparation for it” (p. 123). They note the importance of a relationship between the learner and others, which is required to make sense of one’s perspective and to become aware of (and transform to) new meanings.
To Mezirow, the essence of learning is change. To be truly transformational, learners must engage in inquiry, critical thinking and interaction with others. Brookfield (2000) adds that transformative learning must include a fundamental questioning of one’s thinking and actions. Reflection alone does not result in transformative learning unless this reflection includes an analysis of taken-for-granted assumptions.
Part of the entry-to-practice competencies for health professionals include elements of critical reflection, adoption of professional values, beliefs and attitudes, and ongoing questioning of taken-for-granted assumptions and values. If Mezirow is correct that acquiring a competency does require the involvement of others, this becomes part of the role of the skilled preceptor. Preceptors may be well placed to encourage honest self-review and critical reflection that ends in learner transformation. In this view, preceptors need to be aware of strategies to engage learners in reflection, causing learners to gaze deeply into long- and deeply-held values and biases that they may not even be aware they hold.
The ‘From Novice to Expert’ Model
Benner’s (1984) well-used and much respected From Novice to Expert model has implications for understanding the role of an effective preceptor for health care learners. While Benner focused on nursing students in the clinical setting, her theory likely applies to learners from other health care disciplines. This model holds that nurses develop skills over time from both education (including clinical experience) and personal experience. The model identifies five levels of nursing experience: novice, advanced beginner, competent, proficient and expert. Novices are beginners with no experience—they learn rule-governed tasks by being told and by following instructions. Advanced beginners have gained experience in actual nursing situations and recognize recurring elements that create principles they can use to guide actions. Competent nurses have more clinical experience and use it to become more efficient in providing care. Proficient nurses have an understanding of the bigger picture that improves decision making and allows for changes in plans as needed. Experts no longer need principles or rules to guide action—they use intuition to guide their flexible, highly proficient clinical approaches. As learners transition from novice to expert, they rely less on principles, they see a situation more holistically, and they engage in situations from the inside rather than being external to a situation.
Preceptors can play a vital role in this transition. Benner’s model requires clinical experience for the transition to occur and guidance in the clinical situation is essential for successful transition. Preceptors need to have awareness of the needs of learners at various stages of the continuum and be attuned to the stage(s) at which their students are functioning. For example, a novice student needs a preceptor who provides more direct guidance in learning the rules to guide their actions. A preceptor for an advanced beginner helps learners recognize recurring patterns and develop them into principles of effective care.
Benner also comments that expert clinicians may not be the most effective in preceptoring roles. Expert clinicians may have difficulty explaining their actions in a step-by-step manner because they are functioning by intuition and may not be consciously aware of the rules and principles that they use to make clinical judgments. Analogous to riding a bike, beginners are very aware of the steps needed to balance the bike, propel it forward, stop momentum and avoid obstacles. An expert at cycling is able to just ride without thinking about how to ride and thus may have a challenge teaching a new cyclist.
Strategies for Being and Becoming a Successful Preceptor
This section focuses on strategies for being (and becoming) a successful preceptor for students from various health care professions in clinical learning environments. We also address the challenges and rewards of being a preceptor and characteristics of effective preceptors. The goal is to provide both new and established preceptors with new knowledge that can be used as a road map to beginning and continuing this journey with learners.
Challenges of Precepting
You are invited by your manager to be a preceptor. You are both honoured and terrified. If this is your first time formally in this role, you have a lot to learn. To begin, recognize that becoming a really good preceptor takes experience, just as becoming a competent (even expert) care provider takes experience. Reading this chapter and other resources will help. You may be fortunate that the agency you work for provides preceptor education. The first step is to determine what is available in the form of lectures, workshops, preceptor manuals, etc. and to engage with these before your preceptee arrives. You cannot possibly be fully prepared on day one no matter how much homework you do, so begin with a positive attitude and a sense that you are going to learn every day through reflection, experience and ongoing formal learning. Know that your apprehension is normal—with preparation, this apprehension can be lessened. With a positive approach, being a preceptor can be a fulfilling experience for you and a gift to a learner.
From the Field
Learning Together
I was delighted to be asked to be a preceptor! This would be my first time. I thought “Wow they think I am good enough to teach a new person—that’s super!” My sense of excitement was soon drowned out by horror. What if I made a mistake? What if my student asked a question I couldn’t answer? What if…? I didn’t sleep a wink the night before our first shift together. I just did my best to have a positive attitude and kept reminding myself—my student and I will learn together.
Beth Perry Professor, Faculty of Health Disciplines, Athabasca University, Athabasca, AB.
Once you overcome the initial challenge of self-doubt about your ability to be a preceptor, you can become aware of some of the realities and challenges faced by preceptors. One important challenge is that preceptors must balance the needs of preceptees with the needs of patients they are caring for and the realities of the workplace. Patients may be seriously ill (or become seriously ill during a shift) and work environments may have high staff turnover and other challenges (Hallin & Danielson, 2009). As a preceptor you may feel torn between the needs of your patients and those of the preceptee. The reality is that patient safety always supersedes anything else. If you keep this in mind, you will know what to do. If you do have to make a choice and the preceptee’s needs are not addressed at that point, explain the situation later to the learner and use it as a learning moment to help understand setting priorities.
All students are not going to succeed (at least not at first). You may have a learner who lacks appropriate knowledge, skills and attitudes to perform safe, competent (for their level) and ethical care in the clinical environment. You may be the only line of defense for the patient and your responsibility to, and advocacy for, the patient and society may become your priority. As Luhanga, Yonge & Myrick (2008) write, preceptors must be able to recognize and manage unsafe practice in students—preceptors are the “gatekeepers for the profession” (p. 214). If you have a learner who is disruptive and exhibits other problematic or unsafe behaviours, Luhanga, Yonge & Myrick (2008) provide strategies gathered from preceptors with experience in such situations. Their first recommendation is to catch unsafe practices early or even prevent them if possible. A key first step is giving the learner a complete orientation to the learning environment and establishing clear expectations. Preceptors need to make their own expectations clear, ask learners about their expectations, and understand the program expectations before the learning experience begins. Clear expectations, understood by all involved, can prevent issues and problems. One preceptor in the Luhanga, Yonge & Myrick (2008) study describes how she presents her expectations (p. 216).
Actively involved preceptors often prevent problem behaviours and unsafe practices in learners by providing learners with demonstrations, chances to practice, cues, prompts and frequent feedback throughout the learning experience (Hendrickson & Kleffner, 2002). Such active involvement of the preceptor, including close observation especially in the early days of the relationship, may give learners the best chance for success. As learners gain confidence and competence, preceptors may deliberately step back and encourage more independence within agency guidelines. However, that initial investment of time and energy by the preceptor can be crucial as learners stretch towards practicing at their full scope.
Preventing unsafe and disruptive behaviours is not always possible. If a learner is doing something that is jeopardizing the safety of another (or themselves) the preceptor must stop the behaviour immediately. Further actions (Luhanga, Yonge & Myrick, 2008) include:
- communicating concerns directly to the learner, to determine whether the learner is aware of the problem
- working with the learner to set up a detailed plan for improving performance
- involving the faculty advisor, if the learner is a student.
Preparing preceptors for their role is important to the success of the preceptor–preceptee relationship. Ensuring preceptors are enthusiastic about being preceptors is essential. Careful preparation can fuel this enthusiasm and prepare the preceptor for positive outcomes from their preceptoring experience, encouraging them to continue in this role. Hallin & Danielson (2009) do note that in some clinical environments in which students are preceptored, turnover is high. Preceptors may be placed in the role before they have appropriate orientation, being appointed not because they are ready to be preceptors but because “now it is your turn.” If you are asked to be a preceptor and do not, after careful reflection and self-assessment, feel safe in this role, then do discuss your concerns with your manager before agreeing. Again, the principle of patient safety over-rides all else.
Characteristics of Effective Preceptors
Research has been carried out on the qualities of effective preceptors in various health care disciplines. Effective preceptors in pharmacy have professional expertise, actively engage learners, create a positive learning environment, are collegial, and discuss career-related topics and concerns (Huggett, Warrier & Malo, 2008). Pharmacy students value preceptors who they perceive as role models, who are interested in teaching, relate to learners as individuals, are available to provide direction and feedback, and spend time with learners (Young, Vos, Cantrell & Shaw, 2014). Medical students note that effective preceptor behaviours include openness to questions, constructive feedback, enthusiasm, review of differential diagnoses, and delegation of patient responsibilities (Elnicki, Kolarik & Bardella, 2003). Nursing learners value experienced, knowledgeable professionals who guide them to think critically and create a supportive and nurturing environment (Phillips, 2006).
While these studies note slightly different emphasis on the characteristics of effective preceptors, some commonalities are clear. First, excellent preceptors want to be preceptors, or at least are able to be perceived as wanting this role. Students are attentive to the level of enthusiasm and support that preceptors bring to the relationship. Second, effective preceptors have expertise to share and share it willingly with learners. Learners appreciate preceptors who share their knowledge by involving learners in the learning process—preceptors who make learning interactive and two-way, challenging learners to think critically. Finally, we can note a theme of openness, collegiality, support, respect and nurturing. Students report learning best in a positive learning environment infused with these attitudes.
Creative Strategies
How to be Positive When You Don’t Feel Very Positive
This could also be called the ‘fake it until you make it’ approach. You are human. You have days when you don’t feel like being at work, let alone having a student with you. You have more than enough to do to get through the day and you just don’t have one ounce of energy left over to answer another question!
When this happens, forgive yourself. Remember you do have limits. You can try for an attitude adjustment—give yourself a little lecture and start fresh. If that fails, just take one hour or even one moment at a time and try to be a positive preceptor for just a short period. Fake your enthusiasm until, perhaps after one or two positive exchanges, your real enthusiasm may start to return.
Perry (2008) concludes that nurses who do their job very well come to know they are making a difference for patients (and in your case learners). This realization starts a positive cycle of feeling good about their work, trying even harder to do well, and feeling even better about their success in their role.
So on those days that you just don’t want to be a preceptor, fake it until you can get this positive cycle started. The result may be a great day after all!
What Helps People be Better Preceptors?
You can use multiple strategies to become an outstanding preceptor. First, be sure you have the support you need to succeed. Being a preceptor can be stressful but you can be more effective if you receive support from faculty advisors, managers, colleagues and clinical educators on the unit (Yonge et al., 2002). Support can come in many forms, including formal education programs and workshops through your agency, opportunity to meet with faculty advisors to learn about their expectations of a preceptor, discussion with colleagues about how they enhance their success as a preceptor, or informal chats with clinical educators for teaching tips. You can identity the forms and sources of support most useful to your knowledge gaps. Do reflect on your needs and ask for the support you need to perform your role well.
A second important strategy is preparation. Less experienced preceptors may feel unprepared and unsure of their roles and responsibilities, which adds to the stress of the role. Hallin & Danielson (2009) recommend that, in addition to the preparation outlined earlier in this chapter, preceptors confirm that they have clear guidelines on expectations for their role and what students are allowed to do in clinical settings. In part to gain this knowledge and to learn the more subtle skills of being an effective preceptor, Hallin & Danielson (2009) suggest that inexperienced preceptors be preceptored by experienced preceptors. This requires team-preceptoring rather than initially being a single preceptor on your own and may be effective for some individuals. In particular, new preceptors must be specifically prepared for student evaluation, which can be idiosyncratic to each student’s agency, complex and demanding.
Creative Strategies
Consider Forming a Preceptor Support Group
You can organize a group of preceptors in your agency for regular gatherings to share experiences, debrief problems and engage in professional development on being an exemplary preceptor. You may meet in person or online through Skype or another real-time meeting software.
Do set some guidelines for your group on requirements for participation, frequency of meeting, nature of discussions, etc. Just as in the learning environment you are creating with students, the group should be a positive, supportive, nurturing and engaging gathering. Confidentially will be an important consideration. Give your group a catchy name, like the Preceptor Partners or the Pre Ceptors, to instil a sense of togetherness and build group morale. Adding an element of food sharing or exercise (meet while you walk) can augment the group purpose.
The Preceptor–Preceptee Relationship
Being a preceptor is being a teacher. To succeed as a preceptor you need to be skilled both as a clinician and as an educator. Previous chapters offer numerous clinical teaching strategies that you can apply as a preceptor. Here is a brief overview of some educational strategies you might be able to incorporate into your role.
As a preceptor, developing an effective relationship with the learner is an essential starting point and critical to learning. The preceptor–preceptee relationship has potential to be more effective with mutual respect and a demonstration that the preceptor cares for the learner as a unique individual. A warm welcome is the first step. The tone of the first interaction with the preceptee is important to the success of the relationship. A smile and pleasant tone set the stage for a mutually satisfying respectful relationship and for optimum learning. If the initial contact is by telephone or email, a pleasant welcoming tone is equally important. Something as simple as remembering (and using) the names of learners demonstrates respect.
Beyond a personal welcome, the preceptor must take steps to help the preceptee feel part of the team by introducing the learner to other team members (Hilli, Salmu & Jonsén, 2014). An effective preceptor makes time for the learner to ask questions and become familiar with routines and the culture of the environment. Preceptees also need orientation to practical things like washroom location, what to do if they need to call in sick, break times, daily schedules, and the idiosyncrasies of each workplace.
Trust is built over time. As a preceptor, your goal is to help the learner feel like a partner who evolves to function to the full extent of their skill and knowledge level over time. Preceptors can build trust by seeing preceptees as a valuable addition to the team, by being honest and saying “I don’t know” if they are not sure of the answer to a question, and by being open to new ideas introduced by the preceptee (Vancouver Coastal Health, 2006).
Kramer (1974) describes four stages of reality shock for new employee preceptees: honeymoon, shock, recovery and resolution. These stages are a normal part of learning. In the honeymoon phase preceptees are enthusiastic and full of energy that a good preceptor can harness and encourage. During the shock phase preceptees may become unmotivated and discouraged and struggle with self-doubt. The recovery and eventual resolution phases see a cautious optimism resolving into a positive outlook. Excellent preceptors are mindful that learners may be at any of these stages of reality shock during their time together. Being attentive to how learners are feeling and finding time to chat with them about what makes them anxious, excited or worried can help build a trusting relationship that poises the learner (and preceptor) for success.
Creative Strategies
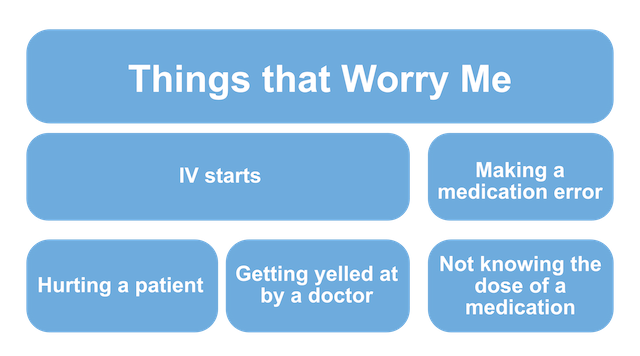
Create a Worry Quilt
Sometimes people are reluctant or unable to share their worries with others, especially with a person in a position of perceived power such as a preceptor. Sensitive preceptors may notice a learner expressing anxiety in clinical situations. You can chat privately with the learner to encourage sharing of anxieties. One strategy that you could use prior to this chat is to have the learner create a worry quilt. You can ask the learner to create visual representations of things that worry them in the clinical situation. The learner places each worry on a quilt square and pieces them together into a quilt pattern. The quilt squares can be pieces of coloured paper or they can be virtual boxes. What the learner puts into the squares can be words or images. When the quilt is pieced together as a whole, you and the learner have a visual depiction of the learner’s major worries. Themes may become evident and lead to specific strategies for mitigating stressors. The constructed quilt may show that the learner is worrying about the same issue in different ways. Being able to address the worries expressed, or condense them into one issue that can be addressed, may help the learner move forward.
A Strengths-Based Approach
Clinical instructors may encounter difficulties in their relationships with students through personality or value differences, or seemingly limited skills or interest on the part of learners (Cederbaum & Klusaritz, 2009). A strength-based approach focuses on learners’ self-determination and strengths. This can be a useful strategy for preceptors encountering difficult relationships with learners (McCashen, 2005). In a strengths-based approach, the preceptor places emphasis on discovering, enhancing and promoting the interests, knowledge and goals of the learner. The preceptor facilitates self-discovery and clinical reflection, creating a learning environment with mutuality and respect and a focus on strengths over deficits. If a strengths-based approach is used effectively, learners feel empowered and affirmed. Some learners who are more familiar with a deficit model may feel uneasy at first if they expect a teacher-centred top-down teaching approach. The strengths perspective can provide an innovative framework for working with students, one that emphasizes student empowerment, collaborative learning and mutual growth (Cederbaum & Klusaritz, 2009).
How can preceptors enact a strengths-based approach? One strategy is to use a learning contract, as explained in chapter 6. This contract can be verbal or written, outlining by mutual agreement the roles and responsibilities of the preceptor and preceptee and emphasizing the mutuality of the learning experience. Another strategy is to express concerns positively and frame overcoming of problems as adding to existing strengths rather than overcoming deficiencies. Preceptors who embrace strengths-based approaches view the clinical situation from the perspective of the learner and try to create a positive learning space (Cederbaum & Klusaritz, 2009).
Creative Strategies
Catch Them Doing Something Right—And Tell Them
Being a preceptor is a challenge. Getting caught up in a spiral of finding weaknesses and trying to think of creative ways to address these is unfortunately too easy. If you focus on the positive, be sure to spend time and energy finding and praising the things that are done well. If you see something positive, tell the person right away and pause for a moment to relish the feelings of success.
Debriefing
Halfer (2007) calls debriefing a magnetic strategy for preceptoring learners. Preceptors can use debriefing as an intentional teaching strategy and an example of guided discovery learning. Usually debriefing is a short exchange that occurs between the preceptor and preceptee after a care experience. Ideally, debriefing occurs in a private and safe location away from others who are not involved in the experience (Wickers, 2010). Debriefing has four elements: reflection, rules, reinforcement and correction (Roberts, Williams, Kim & Dunnington, 2009). Initially a preceptee is invited to reflect on his or her performance, giving the preceptor an opportunity to gain insight into the learner’s perspective. This reflection requires learners to gather their thoughts and share them, which is often a learning experience in itself. Next, the preceptor teaches general rules about the procedure, reinforces them, and corrects errant thinking expressed or demonstrated by the learner. Wickers (2010) emphasizes that “structuring a seemingly unstructured learning event is paramount to the effectiveness of the debriefing session” (p. 83) and reminds us that positive support is part of the successful debriefing model.
Reflective Practice
Preceptors can use the instructional strategy of reflective time to enhance consolidation of theory and practice (Duffy, 2009), encouraging students to reflect on their practice through guided reflection. Schon (1983) suggests that the capacity to reflect on action as part of engaging in a process of continuous learning is one of the defining characteristics of professional practice. Schon differentiates the capacity to reflect in action (while doing something) and on action (after you have done it). To elicit real reflection, the preceptor must ask appropriate questions that move the reflection beyond self-justification or self-indulgence. The desired result is learning, and perhaps behaviour change or enhanced skills proficiency.
Creative Strategies
Instant Replay Without a Camera
Consider using a sports approach to encourage reflection on action. The instant replay allows athletes to review the effectiveness of their actions by watching a video of the action. In a health care interaction the preceptor will not have a video camera in hand to provide this tool, but after the interaction the preceptor can invite the learner to replay (role play) the scenario—creating their own instant replay. Through acting out the interaction, learners will have a chance to reflect on action. After the replay the preceptor and learner can discuss what happened, lessons learned, and changes the learner would make the next time.
Educational Process: Assessment, Planning, Implementation, Evaluation
The educational process parallels the health care process with four stages or steps: assessment, planning, implementation and evaluation. Preceptors need to spend time assessing the learning needs, goals, strengths and limitations of each learner to be able to coach and guide the student to maximum learning. No two learners are the same and thus skilful assessment helps personalize the learning experiences that are facilitated by the preceptor. While assessment is quite important at the outset of the relationship, assessment is also an ongoing activity for preceptors.
Excellent assessment sets the stage for planning instructional opportunities to meet the knowledge and skill gaps identified for each learner. After learning strategies are implemented, evaluation by the learner in consultation with the preceptor determines if the knowledge and skill gaps have been addressed. If not, further specific learning activities need to be sought to continue addressing learning needs and goals. Each evaluation feeds back into assessment and the cycle continues.
The key to success in skilfully implementing this cycle is effective communication through building of excellent rapport between the preceptor and learner. Positive interpersonal relationships are the starting point for rich learning experiences in the clinical environment. A successful preceptorship requires honest and respectful interaction. particularly when the preceptor provides feedback or evaluation to the learner.
Creative Strategies
Talk Out Loud
One strategy for communicating clearly with preceptees is to talk to yourself! Talk out loud as you ask yourself how you are assessing patients, planning care, or implementing and evaluating the success of your intervention. Students benefit from hearing the preceptor’s thought processes aloud (Smedley, Morey & Race, 2010). No extra time is needed to complete a task if you include the verbal commentary, yet hearing your thought processes provides learners with great learning—especially the auditory learners.
Rewards of Being a Preceptor
Although being a preceptor is challenging, and partly because it is challenging, many professionals experience the role as stimulating. The most desired and frequent rewards are often non-tangible. Rewards that preceptors rank highest are the ongoing learning a preceptor achieves, opportunities to share students’ enthusiasm for learning, and fostering professional skills, attitudes and confidence in learners (Campbell & Hawkins, 2009).
In some cases more tangible rewards are provided, depending on the agency involved. Campbell & Hawkins (2009) give examples of preceptors who receive continuing education vouchers; verification of hours towards recertification; reduced price or free admission to museums, lectures, or cultural and sports events; certificates of appreciation; and opportunities to be part of research publications and presentations. Other institutions provide preceptors with paid time off or salary adjustments. As the competition for clinical placements and preceptors becomes more intense, considering some of these more tangible reward systems may be advantageous to clinical practice programs. If administrators and educators plan to offer tangible rewards for participation as preceptors, preceptors must be consulted on what they consider appropriate and valued rewards. Most preceptors are motivated intrinsically and by their values of altruism. They engage in this role because they have a strong desire to pass on their knowledge and skills to the next generation of caregivers.
Creative Strategies
Ideas for Preceptor Rewards
If you are an administrator or educator seeking ideas for rewards that preceptors may find appealing, here are some creative ideas you can consider.
- A plaque with a new inscription for each year a person is a preceptor
- Apprecigrams: Hand-written notes of thanks
- Introduction of preceptors at convocation
- Parking privileges
- Adjunct professor status
- Ask preceptors what they would find rewarding!
Conclusion
Simply put, preceptors are vital. They are charged with the pivotal responsibility of helping learners gain competency to deliver safe, autonomous, professional care. Preceptors have tremendous power to guide the development of professional practice and ultimately the success of learners in the health care professions.
This chapter offered an overview of the roles, challenges and rewards of being a preceptor. Several strategies were discussed to help preceptors excel. The foundational element of all instruction as a preceptor is building a strong relationship with the learner. A caring relationship founded on mutual respect and reciprocity is a prerequisite for a health learning environment. In such an environment learners can thrive and preceptors will be rewarded for devoting time and sharing knowledge, skills and professional insights.
Health care professionals have a responsibility as licensed professional health care team members to help others rise up to meet their potential (Eley, 2015). Preceptors have a responsibility to guide learners, to act as role models, and to lead others into the profession by preparing them to succeed (Hilli, Salmu & Jonsén, 2014). Being an exemplary preceptor can be as rewarding for the teacher as it is for the learner. It is not a role that can be taken lightly. Preparation, reflection on and in action, and continuous learning are fundamental to becoming and excelling as a preceptor.
References
Andrews, M. & Wallis, M. (1999). Mentorship in nursing: A literature review. Journal of Advanced Nursing, 29(1), 201–207.
Benner, P. (1984). From novice to expert: Excellence and power in clinical nursing practice. San Francisco: Jossey-Bass.
Boyd, R. D., & Myers, J. G. (1988). Transformative Education. International Journal of Lifelong Education, 7(4), 261–284.
Brookfield, S.D. (2000). Transformative learning as ideology critique. In J. Mezirow & Associates (Eds.), Learning as transformation. Critical perspectives on a theory in progress (pp. 125–150). San Francisco, CA: Jossey-Bass.
Campbell, S. & Hawkins, J. (2007). Preceptor rewards: How to say thank you for mentoring the next generation of nurse practitioners. Journal of the American Academy Of Nurse Practitioners, 19(1), 24–29.
Cederbaum, J. & Klusaritz, H.A. (2009). Clinical instruction: Using the strengths-based approach with nursing students. Journal of Nursing Education, 48(8), 422–428. 10.3928/01484834-20090518-01
Dawson, P. (2014). Beyond a definition: Toward a framework for designing and specifying mentoring models. Educational Researcher, 43(3), 137–145. doi: 10.3102/0013189X14528751
Dirkx, J.M., Mezirow, J. & Cranton, P. (2006). Musings and reflections on the meaning, context, and process of transformative learning: A dialogue between John M. Dirkx and Jack Mezirow. Journal of Transformative Education, 4(2), 123–139.
Duffy, A. (2009). Guiding students through reflective practice – The preceptors’ experiences. A qualitative descriptive study. Nurse Education in Practice, 9(3), 166–175.
Eby, L. T., Rhodes, J. & Allen, T. D. (2007). Definition and evolution of mentoring. In T. D. Allen and L. T. Eby (Eds.). Blackwell handbook of mentoring. (pp. 1–20). Oxford: Blackwell.
Elnicki, D.M., Kolarik, R. & Bardella, L. (2003). Third-year medical students’ perceptions of effective teaching behaviors in a multidisciplinary ambulatory clerkship. Academy Medicine, 78(8), 815–819.
Eley, S. (2015). The power of preceptorship. Journal of Nursing. Retrieved from http://rnjournal.com/journal-of-nursing/the-power-of-preceptorship
Gopee, N. (2011). Mentoring and supervision in healthcare 2nd Ed. London: Sage.
Halfer, D. (2007). A magnetic strategy for new graduate nurses. Nursing Economics, 21(1), 6–11.
Hallin, K. & Danielson, E. (2009). Being a personal preceptor for nursing students: Registered Nurses’ experiences before and after introduction of a preceptor model. Journal of Advanced Nursing, 65(1), 161–174. doi:10.1111/j.1365-2648.2008.04855.x
Hendricson, W. D. & Kleffner, J. H. (2002). Assessing and helping challenging students: Part One, Why do some students have difficulty learning? Journal of Dental Education, 66(1), 43–61.
Hilli, Y., Salmu, M. & Jonsén, E. (2014). Perspectives on good preceptorship: A matter of ethics. Nursing Ethics, 21(5), 565–575. doi:10.1177/0969733013511361
Huggett, K.M., Warrier, R. & Malo, A. (2008). Early learner perceptions of the attributes of effective preceptors. Adv Health Sci Educ Theory Pract., 13(5), 649–658.
Knowles, M. (1984). The adult learner: A neglected species (3rd ed.). Houston: Gulf.
Kramer, M. (1974). Reality Shock: Why Nurses Leave Nursing. St. Louis: Mosby.
Luhanga, F., Yonge, O. & Myrick, F. (2008). Strategies for preceptoring the unsafe student. Journal for Nurses in Staff Development, 24(5), 214–219.
McCashen, W. (2005). The strengths approach. Victoria, Australia: St Luke’s Innovative Resources.
Mentoring Resources (n.d.). Mentoring Resources [Web site]. Sponsored by the Institute for Clinical Research Education, University of Pittsburgh. Retrieved from http://www.icre.pitt.edu/mentoring/index.aspx
Mezirow, J. (1995). Transformation theory of adult learning. In M.R. Welton (Ed.), Defense of the Lifeworld, (pp. 39–70). NY: State University of New York.
Myrick, F. & Yonge, O. (2005). Nursing Preceptorship: Connecting Practice and Education. NY: Lippincott Williams & Wilkins.
Perry, B. (2008). Shine on: Achieving career satisfaction as a Registered Nurse. Journal of Continuing Education in Nursing, 39(1), 17–25.
Phillips, J.M. (2006). Preparing preceptors through online education. J Nurses Staff Dev., 22(3), 150–156.
Roberts, A. (1999). The origins of the term mentor. History of Education Society Bulletin, 64, 313–329.
Roberts, N.K., Williams, R.G., Kim, M.J. & Dunnington, G.L. (2009). The Briefing, Intraoperative Teaching, Debriefing Model for Teaching in the Operating Room. Journal of the American College of Surgeons, 208(2), 299–303. doi: 10.1016/j.jamcollsurg.2008.10.024
Sandlin, J. A., Wright, R. R. & Clark, C. (2013). Reexamining theories of adult learning and adult development through the lenses of public pedagogy. Adult Education Quarterly, 63(1), 3–23. doi:10.1177/0741713611415836
Schon, D. (1983). The Reflective Practitioner: How professionals think in action. London: Temple Smith.
Smedley, A., Morey, P. & Race, P. (2010). Enhancing the knowledge, attitudes, and skills of preceptors: An Australian perspective. Journal of Continuing Education in Nursing, 41(10), 451–461.
Smith, M. K. (2002). Malcolm Knowles, informal adult education, self-direction and andragogy. In The encyclopedia of informal education. Retrieved from www.infed.org/thinkers/et-knowl.htm
Vancouver Coastal Health. (2006). Preceptor resource guide. Vancouver, BC.
Wickers, M.P. (2010). Establishing the climate for a successful debriefing. Clinical Simulation in Nursing, 6(3), e83–e86. doi:10.1016/j.ecns.2009.06.003
Yonge, O., Krahn, H., Trojan, L., Reid, D. & Haase, M. (2002). Being a preceptor is stressful! Journal for Nurses in Staff Development, 18(1), 22–27.
Young, S., Vos, S. S., Cantrell, M. & Shaw, R. (2014). Factors associated with students’ perception of preceptor excellence. American Journal of Pharmaceutical Education, 78(3), 1–6.
