Chapter 13: Vitamins
“It’s difficult to think anything but pleasant thoughts while eating a homegrown tomato.”
-Lewis Grizzard (1946-1994), American writer and humorist
Vitamins are organic compounds (meaning they contain carbon) and vital nutrients that organisms require in small amounts. Just like other essential nutrients, vitamins must be obtained from the diet since the organism cannot make them (or cannot make enough of them) for survival. Interestingly, not all organisms have the same vitamin requirements. For example, ascorbic acid (one form of vitamin C) is an essential vitamin for humans, because the human body cannot make it, but most other animals have the ability to make this vitamin for themselves. Vitamins are micronutrients, and in this chapter you will see that the vitamins are measured in microgram (mcg or µg) or milligram (mg) amounts. Remember that there are 1,000 mg in 1 gram and 1,000 mcg in 1 mg. Those are tiny quantities and yet we can not live without them!
Learning Objectives
- Differentiate between the characteristics of fat-soluble and water-soluble vitamins.
- Define bioavailability and list characteristics that affect the bioavailability of micronutrients.
- Differentiate between fortified and enriched foods.
- Define the Dietary Reference Intakes (DRIs) and explain how they are used to promote healthy diets.
- Describe common food sources for each vitamin, it’s functions in the body, and the consequences of deficiency and/or toxicity of each vitamin including names for deficiency/toxicity conditions.
- Describe how free radicals develop and the role of antioxidants in fighting oxidative stress.
13.1 Basic Concepts of Vitamins
The first vitamins were identified over 100 years ago. Initially scientists could only classify vitamins based on their solubility. If the vitamin was soluble in fat, it was called vitamin A. If the vitamin was soluble in water it was called vitamin B. As science advanced, it was discovered vitamin A and B were actually several unique organic compounds.1 These new compounds were each given their own letter designation (C, D, E). It was also discovered that vitamin B was actually a group of interrelated substances with similar characteristics but slightly different chemical structures, making them each a unique vitamin. Because of their similarities, B vitamins were each given a number such as B1, B2, B6, B12, but the group is often referred to as B-complex vitamins.2 Thirteen essential vitamins are universally recognized. Some researchers believe there are more vitamins that have yet to be discovered. They are still categorized by their solubility (fat- vs water-soluble), but it is important to note that the term “vitamin” can refer to a number of compounds that all show the biological activity associated with a particular vitamin. For example, “vitamin A,” includes the compounds: retinal, retinol, retinoic acid and four known carotenoids. All of these compounds can be converted into active vitamin A in the body.
For the most part, vitamins are obtained from food, but a few are obtained by other means. For example, microorganisms in the intestine—commonly known as “gut flora” or the “gut microbiome”—produce vitamin K and biotin, while one form of vitamin D is synthesized via the skin with the help of the natural ultraviolet wavelength of sunlight. Humans can produce some vitamins from precursors they consume. Examples include vitamin A, produced from beta-carotene, and niacin, produced from the amino acid tryptophan.
There are a few food sources that contain many of the micronutrients that are required for good health. Dark, green leafy vegetables (collards, turnip greens, kale, spinach, chard, and lettuces) are a great source of vitamins including vitamins A, C, K, folate, and numerous antioxidants. Liver is a great animal source of vitamins. One serving of liver contains copious amounts of vitamins A, B6, B12, thiamin, riboflavin, niacin, and pantothenic acid.
Vitamins have diverse biochemical functions. Most of the vitamins have several important functions, not just one. Some vitamins, such as vitamins A and D, have hormone-like functions where they travel through the blood and tell certain cell types what to do. Other vitamins function as antioxidants (vitamins C and E, for example). The largest number of vitamins, the B vitamins, act as coenzymes and are necessary for enzymes to function, especially in metabolic processes.
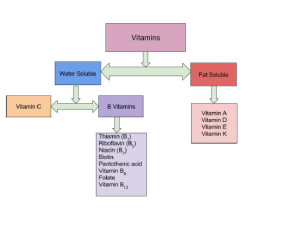
Water-Soluble vs Fat-Soluble Vitamins
Solubility determines where vitamins act in the body. Water-soluble vitamins dissolve in water and therefore act in the cytosol of cells or in extracellular fluids such as blood. Fat-soluble vitamins dissolve in fat and are more easily stored in tissue, so the body has access to them as needed.
Another major difference between fat-soluble vitamins and water-soluble vitamins is the way they are absorbed in the body. Vitamins are absorbed primarily in the small intestine and their bioavailability is dependent on the food composition of the diet. Fat-soluble vitamins are absorbed along with dietary fat. Therefore, if a meal is very low in fat, the absorption of the fat-soluble vitamins will be impaired. Fat-soluble vitamins are packaged and incorporated into chylomicrons along with other fatty acids, absorbed into the lacteal within the villi of the small intestine and transported via the lymphatic system to the liver. Water-soluble vitamins are absorbed into the capillaries within the villi of the small intestine walls and are transported in the blood directly to the liver.
Fat-soluble vitamins can be stored in the body’s visceral and subcutaneous fat. Because of this storage capability, it is more difficult for the body to become deficient in a fat soluble vitamin. However, excessive intake, especially through dietary supplementation or fortification, can cause toxicity. On the other hand, water-soluble vitamins are not readily stored in the body. When someone over-consumes water-soluble vitamins from food (and sometimes dietary supplements), the kidneys filter out the excess and it is excreted in urine. Because of this lack of storage, water-soluble vitamins must be consumed almost every day to avoid deficiency, but toxicity is rare (although can occur with dietary supplementation in some forms such as B6).

Can you consume too many vitamins?
As you read about each of the vitamins and their important roles in human health, keep in mind there can be too much of a good thing. These days, many people have access to high-dose vitamin supplements. Large doses of vitamin supplements can make it easy to get to toxic amounts of vitamins. Think of vitamins as being on a continuum where you can be deficient (too low), just right, or toxic (too high). If you are just a little deficient you may only be able to detect the deficiency with a blood test but if you are deficient long enough and severely enough, systems of the body will eventually begin to lose function and you will see signs and symptoms overtly. At that stage it is called a “deficiency disease.” If a deficiency disease is caught early enough it can usually be reversed by providing the deficient vitamin, but in some cases the damage that has been done is too severe and cannot be reversed.
Table 13.1.1 Summary of Differences between Fat-Soluble and Water-Soluble Vitamins
| Characteristics of Water-Soluble Vitamins | Characteristics of Fat-Soluble Vitamins |
| Act in the cytosol of cells or in extracellular fluids such as blood | Protect cell membranes from free radical damage; act within the cell’s nucleus to influence gene expression |
| Absorbed directly into blood | Absorbed into lymph with fats |
| Little to no storage capacity | Large storage capacity in fatty tissues |
| Need to be consumed regularly to prevent deficiency | Does not need to be consumed daily to prevent deficiency (may take months to develop) |
| Toxicity is rare | Toxicity is more likely |
Nutrient Bioavailability
Bioavailability is the amount of a nutrient that is absorbed and subsequently used by the body. Although a particular food may be an abundant source of a micronutrient, not all of the vitamin or mineral may be bioavailable. Many things can influence the bioavailability of a particular micronutrient. Some preparation, cooking, and storage methods may destroy vitamins. Water-soluble vitamins are especially vulnerable to destruction when boiled, overcooked, or with excessive exposure to light. Be sure to store foods properly to avoid nutrient loss. Other factors that influence the bioavailability of micronutrients in foods are the source of the nutrient. Almost always, nutrients naturally found in food are more bioavailable than those found in supplements or fortified foods. Sometimes the bioavailability of a nutrient has to do more with the person than with the food itself. Some medications may interfere with absorption or metabolism of particular nutrients. Consumption of alcohol or illicit drugs can also modify the bioavailability of nutrients. And underlying health conditions may also play a role. In addition, the genes we inherit from our biological parents can enhance or impede our ability to absorb and use nutrients. Finally, as we age, our ability to absorb and use some nutrients can become impaired.
Effects of Processing on Nutrient Content in Foods
The best way to ensure you are getting all the micronutrients needed for a healthy diet is to eat a wide variety of foods from all food groups. Whole unprocessed foods (e.g., fresh vegetables and fruits, whole grains, lean meats, and low-fat dairy foods) contain more micronutrients than their processed counterparts. For example, a whole baked potato contains significantly more vitamin C, folate, and potassium than a French fry. The nutrient content of foods is typically highest when foods are allowed to ripen on the plant, allowing the plant to full develop the nutrients and phytochemicals it needs to sustain life. Harvesting plants in the peak state of ripeness helps to ensure maximum vitamin and mineral content, and consuming freshly picked or harvested produce usually maximizes nutrient bioavailability. But not all foods can be consumed immediately after harvest. How foods are handled, processed, stored, and prepared can impact how much of that peak nutrient level remains in the food.
Processing of food is an important step in our food supply. Harvesting and transporting foods to communities increases access to a variety of foods. Preservation techniques like canning and freezing extend the shelf life of foods and increase their availability outside of their peak harvest season. In fact, because fresh foods can deteriorate rapidly, food processing techniques may result in better nutrient retention over time when compared to fresh items. However, some vitamins are more stable than others, and the amount retained depends on the specific vitamin and the processing technique. Water-soluble vitamins are the most susceptible to the effects of processing, though other nutrients can be impacted as well.
Table 13.1.2 The Effects of Processing on Nutrient Retention.3
| Method of Processing | Effect on Nutrient Retention | How to Minimize Nutrient Loss |
| Air exposure and time | Enzymes present in foods and exposure to air can destroy nutrients, because as soon as the food is harvested, it begins to slowly decompose. |
|
| Temperature | Cooking helps kill bacteria, makes foods more appealing, and in some situations improves bioavailability of nutrients. But high temperatures for prolonged amounts of time can destroy some vitamins. |
|
| Water | Minerals and water-soluble vitamins can leach into the water. |
|
| Canning | High temperatures may be used, which can destroy water-soluble vitamins, but commercial techniques usually use rapid heating, which helps to reduce nutrient loss. |
|
| Freezing | Freezing does not reduce nutrient content, but if foods are blanched prior to freezing it may slightly reduce levels of water-soluble vitamins. |
|
| Refining of grains | Many B vitamins, minerals, and phytochemicals (as well as fiber), are lost when whole grains are refined (see Chapter 5) |
|
Fortified vs. Enriched
Many consumers think that the terms fortified and enriched mean the same thing. Both are used to describe the addition or enhancement of nutrients in processed foods. However, they are different. A fortified food can contain added nutrients that do not naturally occur in the food product. One example is calcium-fortified orange juice. There is very little calcium in an orange, but when food manufacturers fortify the juice with calcium, it becomes a good source of this mineral. Enrichment is the replacement of nutrients lost in processing. Not all nutrients lost are replaced. In general, the more the food is processed the more nutrients are lost. The most commonly enriched foods are flour, rice, farina, pasta, cornmeal, and corn grits. Fortified = added; Enriched = replaced.
Vitamin Deficiencies
Humans must consume vitamins periodically but with differing schedules, to avoid deficiency. The human body’s stores for different vitamins vary widely; vitamins A, D, and B12 are stored in significant amounts in the human body, mainly in the liver, and an adult human’s diet may be deficient in vitamins A and D for many months and B12 in some cases for years, before developing a deficiency condition. However, vitamin B3 (niacin and niacinamide) is not stored in the human body in significant amounts, so stores may last only a couple of weeks. For vitamin C, the first symptoms of scurvy in experimental studies of complete vitamin C deprivation in humans have varied widely, from a month to more than six months, depending on previous dietary history that determined body stores.
Deficiencies of vitamins are classified as either primary or secondary. As discussed in Chapter 1, a primary deficiency occurs when one does not consume enough of the vitamin. A secondary deficiency may be due to an underlying disorder that prevents or limits the absorption or use of the vitamin, due to a “lifestyle factor,” such as smoking, excessive alcohol consumption, or the use of medications that interfere with the bioavailability of the vitamin. People who eat a varied diet are unlikely to develop a severe primary vitamin deficiency. In contrast, restrictive diets, particularly those that eliminate multiple foods or foods groups, have the potential to cause prolonged vitamin deficits, which may result in often painful and potentially deadly diseases.
Well known human vitamin deficiencies involve thiamin (beriberi), niacin (pellagra), vitamin C (scurvy), and vitamin D (rickets). In much of the developed world, such deficiencies are rare; this is due to an adequate supply of food and fortification of vitamins and minerals to common foods. Specific deficiencies are discussed later in this chapter.
13.2 Dietary Reference Intakes (DRIs)
In Chapter 2, Dietary Reference Intakes (DRIs) were introduced, but let’s take a deeper dive into how these DRIs are set. Chapter 2 also provided an in depth discussion of the Dietary Guidelines for Americans. DRIs and the Dietary Guidelines are both very useful tools, but provide different information for different audiences. Dietary Guidelines provide qualitative advice to the public about the role of one’s diet in chronic disease prevention and maintaining health. DRIs provide quantitative advice to professionals about amounts of nutrients or food components to be of benefit. Set by the National Academy of Medicine (NAM), DRIs are a common set of reference values for a healthy population based on the relationships between nutrient intakes and health or the prevention of disease.
DRIs are a collective term to refer to these components:
- Estimated Energy Requirement (EER)
- Estimated Average Requirement (EAR)
- Recommended Dietary Allowance (RDA)
- Adequate Intake (AI)
- Tolerable Upper Intake Level (UL)**
*A number of people refer to the UL as simply the “upper limit,” leaving off “tolerable.”
Remember, we previously calculated EER in Chapters 2 and 11. To review, EER is the estimated number of Calories needed to maintain energy (caloric) balance. Using weight as a reference, this means you are taking in no more Calories, and also no fewer Calories, than are needed to maintain that exact weight. To gain weight, you’d need to consume more than your EER, and to lose weight you’d need to consume less than your EER. Unlike some of the other DRIs, EER is individual-specific and is based on calculations that take into account multiple variables, including an individual’s age, sex, weight, height, and physical activity level.4
Estimated Average Requirement (EAR) is the nutrient intake level that will meet the average requirement for healthy individuals in an age and sex-specific group. Based on a bell curve, the EAR is set at a level for each nutrient that will meet the requirements for 50% of the population.
The Recommended Dietary Allowance (RDA) is the measure that professionals use to assess the quality of people’s diets. It is set for individual nutrients as the requirement estimated to meet the nutrient needs of 97.5% of healthy people in a population.
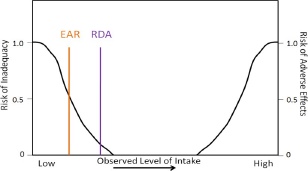
The RDA is calculated using the EAR. Therefore, the EAR needs to be set before an RDA can be set. An EAR is the estimated requirement for 50% of the population (hence the “Average” in its name), as shown in Figure 13.2.1. On the left vertical axis is the risk of inadequacy, and on the bottom of the figure is the observed level of intake that increases from left to right. We will talk about the right axis label in a later figure. Look at where the intake line (black) crosses the EAR and RDA lines in the figure. Where the lines intersect denotes where the level of intake would be inadequate to support the body’s requirements, called the risk of inadequacy. Notice that for the EAR, the risk for inadequacy is 0.5 (50%) whereas the RDA the risk of inadequacy is 0.025 (2.5%).
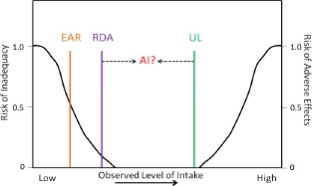
For nutrients lacking the research evidence needed to set an EAR and thus a RDA, an Adequate Intake (AI) is set instead. An AI is a level that appears to be adequate in a defined population or subgroup. As you can see, the EAR is adequate for 50% of the population and is lower than the RDA. The RDA is adequate for 97.5% of the population, and higher than the EAR. The AI level of intake is believed to be between the EAR/RDA and the UL, but since there is not yet a scientific consensus based on current research, it is not exactly known where this level falls as shown in Figure 13.2.2. AI is a current “best guess” and levels are revisited periodically by scientists who examine new research to determine if the levels should be modified. If, during this reexamination, scientists determine that an EAR can be set, they then set a RDA.
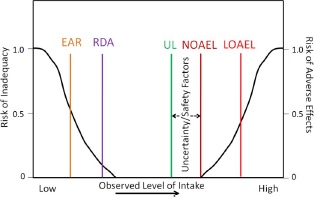
The last of the DRIs is the UL. This is the highest level of daily nutrient intake from all sources (e.g. food, beverages, supplements, fortification) that is unlikely to pose risk of adverse health effects to almost all individuals in the population. To set this, the committee first sets a No Observed Adverse Effect Level (NOAEL) and/or the Lowest Observed Adverse Effect Level (LOAEL). The UL is then set lower (as shown below) based on a number of uncertainty/safety factors, such as natural constituents, substances intentionally and directly added (e.g., food additives), substances indirectly added (e.g., pesticides), and contaminants such as naturally occurring chemicals, industrial products & by-products, and biological agents.5 The right vertical axis is used to represent the risk of an adverse event. Notice the NOAEL at the point where no adverse effects have been reported. The LOAEL is somewhere above the NOAEL. Therefore the UL for a particular nutrient is set at a level where it is believed that people will not experience adverse, toxic effects. In most cases it is difficult to exceed the UL using food alone, but those taking dietary supplements or consuming high amounts of fortified food products should be vigilant.
How are Americans doing in meeting the DRIs? Figure 13.2.4 shows the percentage of Americans that are not meeting the EAR for some of the earlier micronutrients that had DRIs set. Keep in mind that the EAR is set below the RDA.
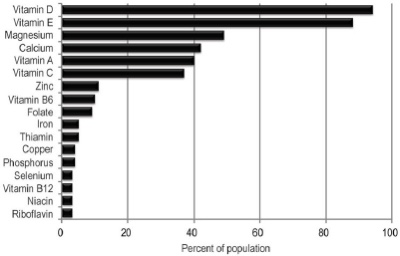
As you can see, a large percentage of Americans don’t meet the EAR for vitamins A, D , C, E, magnesium, and calcium. In the case of vitamin D, for example, more than 95% of Americans don’t even reach the recommended level set for half of the population. This diagram clearly shows that American intakes of these micronutrients are alarmingly low. Also, keep in mind that this diagram does not include micronutrients that have AIs instead of EARs and RDAs.
Personal Application
The USDA has a DRI calculator. Enter your personal data into the calculator, and a list of DRIs for you will be generated.
Table 13.2.1 Summary of DRIs5
| DRI | Definition | Individual or population |
| EER | Estimated number of kcal needed to maintain current weight | Calculated using individual characteristics such as sex, height, weight, age, and activity level |
| EAR | Nutrient intake value that is estimated to meet the requirement of half the healthy individuals in a group | Set for a population or group; based on robust scientific research and agreed upon by scientific community |
| RDA* | Average daily dietary intake level that is sufficient to meet the nutrient requirement of nearly all (97.5%) healthy individuals in a group | Individual recommendation based on the population-based EAR |
| AI* | Nutrient intake value based on observed or experimentally determined approximations of nutrient intake by a group (or groups) of healthy people | AI is set when an EAR/RDA cannot be determined |
| UL | Highest level of daily nutrient intake that is likely to pose no risk of adverse health effects to almost all individuals in the general population. As intake increases above the UL, the risk of adverse effects increases. | UL is set only for those nutrients that have possible negative effects when taken in large doses |
*Every micronutrient has either an RDA or an AI.
DRIs are more than numbers in the table, even though that is often how many people view them. RDAs and AIs are used as the basis for %DV on food labeling, and in diet assessment software that evaluates the adequacy of a person’s diet. Appendix 2 contains the tables that many people commonly associate with the DRIs.
13.3 Water-Soluble Vitamins
Water-soluble vitamins dissolve easily in water and, in general, are readily excreted from the body in urine. Because they are not stored in the body as easily, more consistent intake is important. Water-soluble vitamins play an important role in energy metabolism as coenzymes and are required for blood renewal and function.
Thiamin (Vitamin B1)
Thiamin (also known as thiamine) or vitamin B1 was discovered in 1906.6 Thiamin is especially important in glucose metabolism. It acts as a coenzyme necessary for the conversion of glucose to energy (ATP) in the body. Thiamin also plays a key role in nerve cells, and in the synthesis of neurotransmitters, RNA, and DNA.7 Whole grains, meat, and fish are great sources of thiamin. The US, as well as many other countries, enrich their refined grains with thiamin.
Table 13.3.1 Thiamin Content of Various Foods6
| Food | Serving | Thiamin (mg) | %DV |
| White rice, enriched | ½ c | 1.4 | 117 |
| Breakfast cereals, enriched | 1 | 1.2 | 100 |
| Egg noodles, enriched | ½ c | 0.5 | 42 |
| Pork chop, broiled | 3 oz | 0.4 | 33 |
| Black beans, boiled | ½ c | 0.4 | 33 |
| English muffin, enriched | 1 | 0.3 | 25 |
| Tuna, cooked | 3 oz | 0.2 | 17 |
| Acorn squash, baked | ½ c | 0.2 | 17 |
| Sunflower seeds, roasted | 1 oz | 0.1 | 8 |
| 2% milk | 8 oz | 0.1 | 8 |
The RDA for thiamin is 1.2 mg/day for men and 1.1 mg/day for women. There is no UL currently for thiamin, as there is no human data for adverse effects from high doses. Therefore, there is no toxicity disease or condition associated with excess thiamin consumption.7
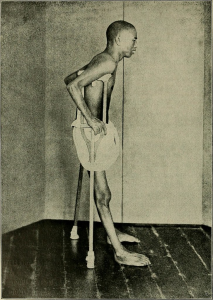
The brain and heart are most affected by a deficiency in thiamin. Thiamin deficiency, also known as beriberi, can cause symptoms of fatigue, confusion, movement impairment, pain in the lower extremities, swelling and heart failure. It is prevalent in societies whose main dietary staple is white rice. During the processing of white rice, the bran is removed along with it’s several nutrient components(such as thiamin) that are vital for metabolism. Another common thiamin deficiency, Wernicke-Korsakoff syndrome, like beriberi, can cause similar symptoms such as confusion, loss of coordination, vision changes, hallucinations, and may progress to coma and death. This condition is most prevalent in those suffering with severe alcoholism as alcohol inhibits thiamin absorption. Other individuals at risk include those with eating disorders, the elderly, and individuals who have undergone gastric bypass surgery.7
Riboflavin (Vitamin B2)
Riboflavin, or vitamin B2, first discovered in 1933, is an essential component of flavoproteins, which are coenzymes involved in many metabolic pathways of carbohydrate, lipid, and protein metabolism.6 Flavoproteins aid in the transfer of electrons in the electron transport chain. Furthemore, the functions of other B vitamin coenzymes (such as vitamin B6 and folate) are dependent on the action of flavoproteins. The “flavin” portion of riboflavin gives a bright yellow color to riboflavin, an attribute that helped lead to its discovery. When riboflavin is taken in excess as a dietary supplement, the excess will be excreted through your kidneys and appear bright yellow in your urine. Although the color may alarm you, it is harmless.
Riboflavin can be found in a variety of different foods but it is important to remember that it can be destroyed by sunlight. Milk is a good source of riboflavin. In the past, milk was packaged in glass bottles. The packaging has now changed to translucent plastic containers or cardboard to block light from destroying riboflavin in the milk.
Table 13.3.2 Riboflavin Content of Various Foods8
| Food | Serving | Riboflavin (mg) | %DV |
| Beef liver | 3 oz | 2.9 | 223 |
| Breakfast cereals, enriched | 1 c | 1.3 | 100 |
| Instant oats, fortified | 1 c | 1.1 | 85 |
| Plain yogurt, fat-free | 1 c | 0.6 | 46 |
| 2% milk | 1 c | 0.5 | 38 |
| Beef, tenderloin steak | 3 oz | 0.4 | 31 |
| Portabella mushroom, sliced | ½ c | 0.3 | 23 |
| Egg, scrambled | 1 large | 0.2 | 15 |
| Quinoa | 1 c | 0.2 | 15 |
| Spinach, raw | 1 c | 0.1 | 8 |
The RDA for riboflavin is 1.3 mg/day for men and 1.1 mg/day for women. There is no UL for riboflavin because no toxicity has been reported when an excess amount has been consumed through foods or supplements. Therefore, there is no toxicity disease or condition associated with excess riboflavin consumption.8

Riboflavin deficiency, also referred to as ariboflavinosis, is often accompanied by other dietary deficiencies (most notably protein) and can be common in people suffering from alcoholism. This deficiency will usually occur in conjunction with deficiencies of other B vitamins because the majority of B vitamins have similar food sources. Signs and symptoms of ariboflavinosis include dry, scaly skin, cracking of the lips (stomatitis) and at the corners of the mouth (cheilosis), sore throat, itchy eyes, and light sensitivity.8
Niacin (Vitamin B3)
Niacin, or vitamin B3, was first discovered in 1926. Niacin was actually the first vitamin to be synthesized, back in 1867, although at that time it’s association with nutrition was unknown.6 Niacin is a component of the coenzymes NADH, NADPH, which are involved in both the catabolism (breakdown) and anabolism (build up) of carbohydrates, lipids, and protein. NADH is the predominant electron carrier and transfers electrons to the electron transport chain to make ATP. NADPH is also required for the anabolic pathways of fatty acid and cholesterol synthesis. In contrast to other vitamins, niacin is unique in that it can be synthesized by humans from the amino acid tryptophan in an anabolic process requiring enzymes dependent on riboflavin, vitamin B6, and iron. Niacin is made from tryptophan only after tryptophan has met all of its other needs in the body.
Niacin can be found in a variety of different foods such as yeast, meat, poultry, fish, and grains. In plants, especially mature grains, niacin can be bound to sugar molecules which can significantly decrease its’ bioavailability.
Table 13.3.3 Niacin Content of Various Foods9
| Food | Serving | Niacin (mg) | %DV |
| Chicken breast, grilled | 3 oz | 10.3 | 64 |
| Turkey breast, roasted | 3 oz | 10.0 | 63 |
| Salmon, sockeye, cooked | 3 oz | 8.6 | 54 |
| Beef (90% lean), pan browned | 3 oz | 5.8 | 36 |
| Brown rice, cooked | 1 c | 5.2 | 33 |
| Peanuts, roasted | 1 oz | 4.2 | 26 |
| Russet potato, baked | 1 medium | 2.3 | 14 |
| Bread, whole wheat | 1 slice | 1.4 | 9 |
| Banana | 1 medium | 0.8 | 5 |
| Broccoli, boiled | ½ c | 0.4 | 3 |
The RDA for niacin is 16 mg/day for men and 14 mg/day for women. The UL for niacin applies only to supplemental niacin and is 35 mg for both men and women. Consumption of 35 mg or higher is more associated with “niacin flush” where a person’s face, arms, and chest becomes a reddish color resulting from vasodilation of small blood vessels. Flushing is often accompanied by sensations of burning, tingling, and itching. These symptoms are often transient and while unpleasant, fairly harmless. However, more serious signs and symptoms include headache, rash, dizziness, and a decrease in blood pressure.9 Many pre-workout supplements contain high amounts of niacin, as much as 35 mg per serving. Some people consuming these report the flushing sensations listed above which they attribute to the supplement getting them “pumped up.” Physiologically speaking, however, these symptoms do not provide an increase in metabolism or muscle contraction.
Mild niacin deficiency has been shown to cause fatigue, decreased appetite, indigestion, and decreased tolerance to cold. Severe deficiency of niacin in the diet causes the disease pellagra, which is characterized by the 4 D’s: diarrhea, dermatitis (as seen in Figure 13.3.3), dementia, and eventually death if not treated.
Native Americans who grew and consumed corn as a staple in their diet learned to avoid pellagra by treating their corn with alkali – soaking it in wood ashes (North America) or calcium hydroxide (pickling lime) in Central and South America prior to grinding it into corn meal. This allows the niacin to become more bioavailable. This process called nixtamilization is applied to make masa harina, the corn meal used to make corn tortillas and tamales.
The War on Pellagra

Pellagra was first identified among Spanish peasants in 1735. Because of the skin lesions that developed, it was often mistaken for leprosy. In the US cases were reported in the 1820s, but pellagra was not officially identified here until 1907. In the early 20th century, pellagra was rampant, killing many poor Southerners and it was a public health problem. From 1907-1940, there were as many as 3 million cases and 100,000 deaths. Dr. Joseph Goldberger, who had been battling other epidemic diseases, was asked to head the investigation into pellagra. At that time, most doctors were convinced that pellagra was an infectious disease caused by germs. However, anecdotal evidence from mental institutions and prisons showed that inmates often contracted pellagra but staff almost never did. This led Goldberger to question the infectious disease hypothesis and instead he theorized that the disease was related to diet. To test this he had shipments of food sent to two orphanages and the Georgia State Asylum. The results were clear, those children and inmates who had pellagra who were fed fresh meat, milk and vegetables instead of a corn-based diet recovered. Those without pellagra who ate the new diet never developed it.
Many doctors refused to believe pellagra was caused by a dietary deficiency. Goldberger hoped to convince them by injecting blood and swabbing secretions from a person with pellagra into himself and several volunteers. They also swallowed capsules containing scabs of rashes from the skin of pellagra victims. None of them got pellagra. Although the actual dietary deficiency, niacin, was not identified until after Goldberger’s death, he was honored posthumously for his selfless devotion to relieving the suffering of those with pellagra.10
Pantothenic acid (Vitamin B5)
Pantothenic acid, or vitamin B5, was first discovered in 1931.6 It is required to synthesize coenzyme A (CoA) which is the carbon carrier of glucose, fatty acids, and amino acids in the Kreb’s cycle. CoA is also involved in the synthesis of lipids, cholesterol, and acetylcholine (a neurotransmitter). Pantothenic acid is widely distributed in all types of food, which is why a deficiency in this nutrient is rare. Its name derives from the Greek pantothen, meaning “from everywhere.”
Table 13.3.4 Pantothenic Acid Content of Various Foods11
| Food | Serving | Pantothenic Acid (mg) | %DV |
| Shiitake mushrooms, cooked | ½ c | 2.6 | 52 |
| Sunflower seeds | ¼ c | 2.4 | 48 |
| Chicken breast, roasted | 3 oz | 1.3 | 26 |
| Fresh tuna, cooked | 3 oz | 1.2 | 24 |
| Avocado | ½ fruit | 1.0 | 20 |
| 2% milk | 1 c | 0.9 | 18 |
| Egg, hard boiled | 1 large | 0.7 | 14 |
| Ground beef (85%), broiled | 3 oz | 0.6 | 12 |
| Whole wheat pita | 1 large | 0.5 | 10 |
| Broccoli, boiled | ½ c | 0.5 | 10 |
The RDA for pantothenic acid is 5 mg/day for men and women. There is no UL currently for pantothenic acid, as there is insufficient human data to identify adverse effects from high doses. Therefore, there is no toxicity disease or condition associated with excess pantothenic acid consumption.11
A severe pantothenic acid deficiency is exceptionally rare. Signs and symptoms include fatigue, irritability, numbness, headache, and a burning sensation of the hands and feet.11
Vitamin B6 (Pyridoxine)
Vitamin B6 was first discovered in 1934.6 Vitamin B6 refers to a group of chemically similar compounds which can be interconverted in biological systems (pyridoxine, pyridoxamine, pyridoxic acid, etc). It acts as a coenzyme in a wide variety of functions in the body. One major function is the nitrogen transfer between amino acids which plays a role in amino acid synthesis and catabolism. It also functions to release glucose from glycogen and is required for the synthesis of multiple neurotransmitters and hemoglobin.
Vitamin B6 can be found in a wide variety of foods. However, cooking, storage and processing loses some vitamin B6 depending on the form of the vitamin present in food. The richest sources include fish, beef liver, potatoes, and other starchy vegetables.
Table 13.3.5 Vitamin B6 Content of Various Foods12
| Food | Serving | Vitamin B6 (mg) | %DV |
| Chickpeas, canned | 1 c | 1.1 | 65 |
| Fresh tuna, cooked | 3 oz | 0.9 | 53 |
| Salmon, sockeye, cooked | 3 oz | 0.6 | 35 |
| Potatoes, boiled | 1 c | 0.4 | 25 |
| Banana | 1 medium | 0.4 | 25 |
| Ground beef (85%), broiled | 3 oz | 0.3 | 18 |
| Cottage cheese (1%) | 1 c | 0.2 | 12 |
| Squash, winter, baked | ½ c | 0.2 | 12 |
| White rice, enriched, cooked | 1 c | 0.1 | 6 |
| Watermelon | 1 c | 0.1 | 6 |
The RDA for vitamin B6 is 1.3 mg/day for men and women. The UL for vitamin B6 is 100 mg/day and this applies to both food and supplement intakes. Chronic vitamin B6 supplementation has been shown to cause severe and progressive neuropathy and loss of control of bodily movements.12
A deficiency in vitamin B6 can cause anemia, but it is a different type than that caused by insufficient folate, vitamin B12, or iron, although the symptoms are similar. The size of red blood cells is normal or somewhat smaller, but the hemoglobin content is lower. This means that each red blood cell has less capacity for carrying oxygen, resulting in muscle weakness, fatigue, and shortness of breath. Other deficiency symptoms can include dermatitis, mouth sores, and confusion.
Biotin (Vitamin B7)
Biotin, or vitamin B7, was first discovered in 1926.6 It is required as a coenzyme in the Kreb’s cycle and in lipid metabolism. It is also required as an enzyme in the synthesis of glucose and some nonessential amino acids. It is also widely available in dietary supplements for hair and nails. A specific enzyme, biotinidase, is required to release biotin from protein so that it can be absorbed in the gut. There is some bacterial synthesis of biotin that occurs in the colon, however this is not a significant source of biotin. Biotin can be found in foods such as eggs, fish, meat, seeds, nuts, and some vegetables.
Table 13.3.6 Biotin Content of Various Foods13
| Food | Serving | Biotin (mcg) | %DV |
| Egg, cooked | 1 large | 10 | 33 |
| Salmon, canned | 3 oz | 5.0 | 17 |
| Pork chop, cooked | 3 oz | 3.8 | 13 |
| Sunflower seeds | ¼ c | 2.6 | 9 |
| Sweet potato, cooked | ½ c | 2.4 | 8 |
| Almonds, roasted | ¼ c | 1.5 | 5 |
| Tuna, canned in water | 3 oz | 0.6 | 2 |
| Spinach, boiled | ½ c | 0.5 | 2 |
| Broccoli, fresh | ½ c | 0.4 | 1 |
| Banana | ½ c | 0.2 | 1 |
Because there is little information on the requirements for biotin, instead of an RDA, an AI of 30 mcg has been identified for men and women. There is no UL currently for biotin, as there is insufficient human data to identify adverse effects from high doses.13
Biotin deficiency is rare, but can be caused by eating large amounts of egg white over an extended period of time. This is because a protein in egg whites tightly binds to biotin making it unavailable for absorption. A rare genetic disease causing malfunction of the biotinidase enzyme also results in biotin deficiency.
Folic Acid (Vitamin B9)
Folic acid, or vitamin B9, was first discovered in 1931, isolated in 1939, and made in a lab in 1946.6 Folate, a reduced form of folic acid, is a required coenzyme for the synthesis of the amino acid methionine, and for making RNA and DNA. Therefore, rapidly dividing cells are most affected by folate deficiency. Red blood cells, white blood cells, and platelets are continuously being synthesized in the bone marrow from dividing stem cells. When folate is deficient, these cells cannot divide normally. A consequence of folate deficiency is macrocytic, megaloblastic anemia. Macrocytic refers to large sized and megaloblastic refers to immature cells that contain less hemoglobin. These cells are unable to produce DNA and RNA fast enough; cells grow but do not divide making them larger in size.
Folate is found naturally in a wide variety of foods including vegetables (particularly dark green leafy vegetables), fruits, nuts, peas, dairy products and more. In fact, the term “folic” is from the Latin word folium, which means leaf. Spinach, asparagus, and Brussels sprouts are among the foods with the highest folate levels. The FDA began requiring manufacturers to enrich breads, cereals, flours, and cornmeal in 1998 to increase the consumption of folate in the American diet.
Table. 13.3.7 Folate Content of Various Foods14
| Food | Serving | Folate (mcg DFE) | %DV |
| Beef liver, braised | 3 oz | 215 | 54 |
| Spinach, boiled | ½ c | 131 | 33 |
| Black eyed peas, boiled | ½ c | 105 | 26 |
| Asparagus, boiled | 4 spears | 89 | 22 |
| Brussels sprouts, boiled | ½ c | 78 | 20 |
| Spaghetti, enriched, cooked | ½ c | 74 | 19 |
| Avocado, raw | ½ c | 59 | 15 |
| Broccoli, chopped, cooked | ½ c | 52 | 13 |
| Orange juice | ¾ c | 35 | 9 |
| Egg, hard boiled | 1 large | 22 | 6 |
Folate is found naturally in foods, while folic acid is the chemical form that is used in dietary supplements as well as enriched foods, such as grains. The Food and Nutrition board of the NAM developed dietary folate equivalents (DFE) to reflect the fact that folic acid is more bioavailable and easily absorbed than folate found in food. This is unique to folate—that the supplemental form is more bioavailable than what is found naturally in foods. One DFE is defined as 1 mcg of dietary folate, or 0.6 mcg of folic acid supplement.14
The RDA for folate is 400 mcg DFE/day for men and women. The UL for folate is 1,000 mcg/day and applies to supplemental intakes. Large amounts of folate can mask vitamin B12 deficiency, but not the neurological damage associated with it.14
As stated previously, folate deficiency can lead to macrocytic, megaloblastic anemia which can include the following signs and symptoms: weakness, fatigue, heart palpitations, shortness of breath, headache, and open sores on the tongue.
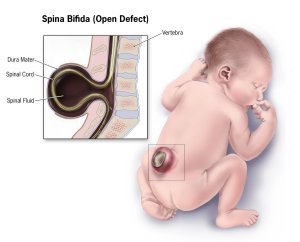
Children whose mothers were folate deficient during pregnancy have a higher risk of birth defects, such as spina bifida. This is a neural tube defect that occurs when the spine does not completely enclose the spinal cord and can lead to many physical and mental disabilities. Results of clinical trials have demonstrated that neural tube defects are significantly decreased in the offspring of mothers who began taking folate supplements at least one month prior to becoming pregnant and through the pregnancy.

In extreme cases, a neural tube fatal defect called anencephaly can occur in which the cerebral hemispheres of the brain do not develop. Prenatal screening for neural tube defects has significantly decreased the number of births of infants with anencephaly, and correction of folate deficiency has reduced the incidence even further. When there is no upper brain development, the eyes and eyelids are the topmost part of the body, giving the head a “frog-eyed” appearance. Anencephaly typically results in spontaneous abortion or stillborn birth. Infants born alive typically die within hours or days.
Vitamin B12 (Cobalamin)
Vitamin B12 was first discovered in 1926, isolated in 1948, and made in a lab in 1970.6 It contains cobalt, making it the only vitamin that contains a metal ion. Vitamin B12 is an essential part of several coenzymes, necessary for fat and protein catabolism, for folate coenzyme function, and for hemoglobin synthesis. An enzyme requiring vitamin B12 is needed by a folate dependent enzyme to synthesize DNA. Thus a deficiency in vitamin B12, similar to a folate deficiency, causes macrocytic, megaloblastic anemia in children and adults, and an increased risk of neural tube defects in children born to B12 deficiency mothers.
Vitamin B12 is found naturally in animal products such as fish, meat, poultry, eggs, and milk products. Although vitamin B12 is generally not found in plant foods, fortified breakfast cereals and some nutritional yeast products may also be sources.
Table 13.3.8 Vitamin B12 Content of Various Foods15
| Food | Serving | Vitamin B12 (mcg) | %DV |
| Clams, cooked | 3 oz | 84.1 | 3,504 |
| Salmon, sockeye, cooked | 3 oz | 4.8 | 200 |
| Tuna, canned in water | 3 oz | 2.5 | 104 |
| Haddock, cooked | 3 oz | 1.8 | 75 |
| Beef, top sirloin, broiled | 3 oz | 1.4 | 58 |
| Milk (2%) | 1 c | 1.2 | 50 |
| Yogurt (2%) | 1 c | 1.1 | 46 |
| Cheese, Swiss | 1 oz | 0.9 | 38 |
| Egg, hard boiled | 1 large | 0.6 | 25 |
| Chicken breast, roasted | 3 oz | 0.3 | 13 |
The RDA for vitamin B12 is 2.4 mcg/day for men and women. There is no UL currently for vitamin B12, because of its low potential for toxicity.15
In order for the human body to absorb B12, the stomach, pancreas, and small intestine must be functioning properly. Cells in the stomach secrete a protein called intrinsic factor that is necessary for vitamin B12 absorption, which occurs in the small intestine. Impairment of intrinsic factor secretion caused by either an autoimmune disease or by chronic inflammation of the stomach (such as that occurring in some people with H. pylori infection) can lead to pernicious anemia, a type of macrocytic anemia. This is a secondary deficiency associated with lack of intrinsic factor and treatment consists of B12 injections to bypass the gastrointestinal tract. B12 deficiency is most common in the elderly who may have impaired functioning of digestive organs, a normal consequence of aging.
Vitamin B12, along with folate, play key roles in converting homocysteine to the amino acid methionine. High levels of homocysteine in the blood increase the risk for heart disease. Therefore, low levels of folate, vitamin B12, and vitamin B6 (which acts as a coenzyme in this conversion) will increase homocysteine levels therefore increasing the risk of heart disease. When there is a deficiency in vitamin B12, inactive folate (from food) is unable to be converted to active folate and used in the body for the synthesis of DNA. Folic acid (that comes from supplements or enriched foods), however, is available to be used as activated folate in the body without B12.
Vitamin C
Vitamin C, also commonly called ascorbic acid, is an essential micronutrient for humans, though most other mammals can readily synthesize it. It was discovered in 1912, isolated in 1926, and first made in a lab in 1933.6 Vitamin C acts as a highly effective antioxidant in scavenging reactive oxygen species, reactive nitrogen species, and many other free radicals. It protects lipids both by disabling free radicals and by aiding in the regeneration of vitamin E. Antioxidants will be discussed in more detail later in this chapter.
Vitamin C is a required part of several enzymes such as signaling molecules in the brain, some hormones, and amino acids. It is essential for the synthesis and maintenance of collagen, which is the most abundant protein in the body and used for different functions such as the structure for ligaments, tendons, blood vessels, and also scars, that bind wounds together. Vitamin C acts as the glue that holds the collagen fibers together.
Vitamin C does have several roles in the immune system, and many people will increase vitamin C intake either from diet or supplements when they have a cold. Many others routinely consume vitamin C in an effort to prevent colds. Contrary to this popular practice, there is no good evidence that this works. A review of more than 50 years of studies concluded that taking vitamin C routinely does not prevent colds in most people, but it may slightly reduce cold severity and duration. Moreover, taking megadoses (up to 4000 mg/day) at the onset of a cold provided no benefits.15 As a water-soluble vitamin, the excess is not stored in significant amounts, so is excreted in urine. In fact, people taking megadoses of vitamin C will often see their urine color become more saturated.
Citrus fruits are great sources of vitamin C as are many other fruits and vegetables. It is not found in significant amounts in animal-based foods. Because vitamin C is water-soluble, it leeches away from foods considerably during cooking, freezing, thawing, and canning. Therefore to maximize vitamin C intake from foods, you should eat fruits and vegetables raw or lightly steamed.
Table 13.3.9 Vitamin C Content of Various Foods17
| Food | Serving | Vitamin C (mg) | %DV |
| Sweet red peppers, raw | ½ c | 95 | 106 |
| Orange juice | ¾ c | 93 | 103 |
| Orange | 1 medium | 70 | 78 |
| Broccoli, cooked | ½ c | 51 | 57 |
| Strawberries | 1 c | 49 | 54 |
| Brussels sprouts, cooked | ½ c | 48 | 53 |
| Grapefruit | ½ medium | 39 | 43 |
| Cantaloupe | ½ c | 29 | 32 |
| Tomato | 1 medium | 17 | 19 |
| Potato, baked | 1 medium | 17 | 19 |
The RDA for vitamin C is 90 mg/day for men and 75 mg/day for women. Individuals who smoke require 35 mg/day more vitamin C than nonsmokers. The UL (for both food and supplement use) is set at 2000 mg/day although vitamin C has low toxicity and is not believed to cause serious adverse effects at high intakes. The most common complaints relate to gastrointestinal disturbances such as diarrhea, nausea, and abdominal cramps.17
Vitamin C is not stored in any significant amount in the body, but once it has reduced a free radical, it is very effectively regenerated and therefore can exist in the body as a functioning antioxidant for many weeks.
The classic condition associated with vitamin C deficiency is scurvy. Signs and symptoms include skin disorders, bleeding gums, painful joints, weakness, depression, and increased susceptibility to infections.
Scurvy
Between the 15th and 18th centuries, scurvy killed more than two million sailors including many on the ships captained by Christopher Columbus. This was the age of great sailing voyages across the Atlantic, Pacific, and Indian Oceans and sailors could be at sea for more than three months at a time. They would suffer greatly from many vitamin deficiencies because the dried and preserved foods they consumed did not contain adequate micronutrients, but the worst was scurvy. The symptoms of scurvy were severe. It would begin with small blisters that would develop into painful, large, bleeding sores. Gums would become black, teeth would fall out. Without vitamin C the body can no longer make collagen, so previously broken bones would rebreak, and old wounds would open up. Arteries would decay so a person would bleed internally. The structure of the brain would deteriorate causing personality changes, vivid dreams, hallucinations, and seizures.18 Sailors who ate the ship’s rats were spared because rats make their own vitamin C. In 1622, sir Richard Hawkins wrote that “sower (sour) lemons and oranges” helped, but it wasn’t until over 100 years later in 1747 that Englishman James Link conducted the first controlled medical experiment on a ship showing that citrus fruits cured scurvy.19 This was more than 150 years before vitamin C was “discovered.”
Choline
Choline is an organic, water-soluble substance that is not classified as a vitamin but is similar to the B vitamins. However, the synthesis of choline is limited and therefore it is recognized as an essential nutrient. Choline is needed to perform functions such as the synthesis of the neurotransmitter acetylcholine, phospholipids used to make cell membranes, lipid transport, and also homocysteine metabolism.
Table. 13.3.10 Choline Content of Various Foods20
| Food | Serving | Choline (mg) | %DV |
| Egg, hard boiled | 1 large | 147 | 27 |
| Beef, top round, braised | 3 oz | 117 | 21 |
| Soybeans, roasted | ½ c | 107 | 19 |
| Chicken breast, roasted | 3 oz | 71 | 13 |
| Shiitake mushrooms, cooked | ½ c | 58 | 11 |
| Red potatoes, baked | 1 large | 57 | 10 |
| Kidney beans, canned | ½ c | 45 | 8 |
| Milk (1%) | 1 c | 43 | 8 |
| Brussels sprouts, boiled | ½ c | 32 | 6 |
| Cottage cheese, non-fat | 1 c | 26 | 5 |
There is insufficient data on choline so the NAM recommends an AI of 550 mg/day for men and 425 mg/day for women, with a UL of 3,500 mg/day. High intakes of choline are associated with a fishy body odor, vomiting, excessive sweating and salivation, hypotension (low blood pressure), and liver toxicity.20
13.4 Fat-Soluble Vitamins
There are four fat-soluble vitamins: A, D, E, and K. Unlike water-soluble vitamins, they dissolve in fats and oils, and are more readily stored in our body’s adipose tissue. The fat-soluble vitamins are present in many foods but they are especially high in foods like nuts and seeds that contain a high concentration of fats and oils. Because they can be stored it is more difficult to become deficient in a fat-soluble vitamin. However, toxicity, especially from supplements, is more likely to occur.
Vitamin A
Vitamin A is a generic term for a group of similar compounds called retinoids. It was discovered in 1915, isolated in 1937, and first made in a lab in 1947.6 There are two types of vitamin A in the diet. Preformed vitamin A includes retinol, found in animal-based foods which can be converted to the biologically active forms in the body, retinal and retinoic acid. Provitamin A includes carotenoids found in plant based foods. Carotenoids are pigments synthesized by plants to give them their yellow, orange, and red color. Over 600 carotenoids have been identified, with beta-carotene being one of the most well known. Approximately 10% of carotenoids can be converted in the body to retinoids.
Since vitamin A is fat-soluble, during digestion it is packaged into chylomicrons in the small intestine and absorbed into the lymphatic system before being transported to the liver. The liver stores and exports vitamin A as needed; it is released into the blood bound to a retinol-binding protein, which transports it to cells. Carotenoids are not absorbed as well as vitamin A, but similar to vitamin A, they do require fat in the meal for absorption. Carotenoids are also packaged into the lipid-containing chylomicrons within the small intestine and then eventually transported to the liver. In the liver, carotenoids are repackaged into lipoproteins, which transport them to cells.
Vitamin A has several important functions in the body including assisting in maintaining vision, the immune system, skin, and the linings of tissues, and regulating growth and development (particularly in the fetal stages of life). Vitamin A also acts similarly to some hormones, in that it is able to change the amount of proteins in cells by interacting with DNA. As an antioxidant, vitamin A protects cellular membranes, helps in maintaining glutathione levels, and influences the amount and activity of enzymes that detoxify free radicals.
Of all vitamin A’s functions, it’s role in vision may be its most well known. The retinoids are aptly named as their most notable function is in the retina of the eye where they aid in vision, particularly in seeing under low-light conditions. This is why night blindness is the most definitive sign of vitamin A deficiency.
Preformed vitamin A is found only in animal foods, with the liver being the richest source because that’s where it is stored. Brightly colored (especially red, yellow, and orange) plant foods are good sources of carotenoids.
Table 13.4.1 Vitamin A Content of Various Foods21
| Food | Serving | Vitamin A (mcg RAE) | %DV |
| Beef liver, pan fried | 3 oz | 6,582 | 731 |
| Sweet potato, baked | 1 whole | 1,403 | 156 |
| Spinach, boiled | ½ c | 573 | 64 |
| Carrots, raw | ½ c | 459 | 51 |
| Ricotta cheese, part-skim | 1 c | 263 | 29 |
| Atlantic herring, pickled | 3 oz | 219 | 24 |
| Milk, skim | 1 c | 149 | 17 |
| Cantaloupe, raw | ½ c | 135 | 15 |
| Sweet red peppers, raw | ½ c | 117 | 13 |
| Egg, hard boiled | 1 large | 75 | 8 |
The RDA for vitamin A is 900 mcg RAE/day for men and 700 mcg RAE/day for women. RAE refers to retinol activity requirements as it takes into account its many different available forms. Therefore, 1 mcg of retinol is equivalent to 12 mcg of beta-carotene. The UL for vitamin A is 3,000 mcg/day and this applies to preformed vitamin A and supplemental intake. Consumption beyond the UL is associated with increased risk of vision and liver problems and birth defects.21
Vitamin A supplements have been found to increase the risk of lung cancer in people who are at high risk for the disease (i.e., smokers, ex-smokers, workers exposed to asbestos). The Beta-Carotene and Retinol Efficacy Trial (CARET) involving over 18,000 participants who were at high risk for lung cancer found that people who took supplements containing very high doses of vitamin A and beta-carotene had a 28% higher incidence of lung cancer midway through the study, which was consequently stopped.22
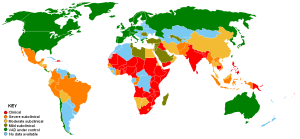
Severe vitamin A deficiency over time can also cause complete vision loss. In fact, vitamin A deficiency is the number one cause of preventable blindness worldwide. Vitamin A not only supports the vision function of eyes but also maintains the coverings and linings of the eyes. Vitamin A deficiency can lead to the dysfunction of the linings and coverings of the eye (e.g., bitot spots), causing dryness of the eyes, a condition called xerophthalmia. The progression of this condition can cause ulceration of the cornea and eventually blindness.
The common occurrence of advanced xerophthalmia in children who died from infectious diseases led scientists to hypothesize that supplementing vitamin A in the diet for children with xerophthalmia might reduce disease-related mortality. In Asia in the late 1980s, targeted populations of children were administered vitamin A supplements, and the death rates from measles and diarrhea declined by up to 50%. Vitamin A supplementation in these deficient populations did not reduce the number of children who contracted these diseases, but it did decrease the severity of the diseases so that they were no longer fatal. Soon after the results of these studies were communicated to the rest of the world, the WHO and the United Nations Children’s Fund (UNICEF) commenced worldwide campaigns against vitamin A deficiency. UNICEF estimates that the distribution of over half a billion vitamin A capsules prevents 350,000 childhood deaths annually.23
Vitamin D
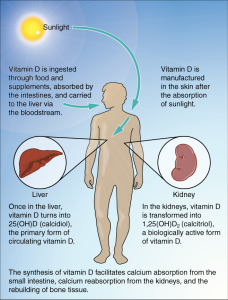
Vitamin D refers to a group of fat-soluble vitamins derived from cholesterol. Vitamins D2 (ergocalciferol) and D3 (calcitriol) are the only ones known to have biological actions in the human body. It was discovered in 1919.6 Vitamin D is unique in that the skin can synthesize it when exposed to sunlight. In fact, for most people, more than 90% of their vitamin D3 comes from the casual exposure to the ultraviolet rays in sunlight. Anything that reduces your exposure to the sun’s UVB rays decreases the amount of vitamin D3 your skin synthesizes. That would include long winters, your home’s altitude, whether you are wearing sunscreen, and the color of your skin (including tanned or darker skin). Less than thirty minutes of sun exposure to the arms and legs will increase blood levels of vitamin D3 more than orally taking 250 mcg of vitamin D3 in most people. Figure 13.4.2 shows how vitamin D is synthesized in the body. The liver and kidneys must “activate” the vitamin to make it bioavailable, so if either organ is impaired, the bioavailability of vitamin D will be reduced.
Table 13.4.2 Vitamin D Content of Various Foods24
| Food | Serving | Vitamin D (mcg) | %DV |
| Cod liver oil | 1 tbsp | 34 | 170 |
| Rainbow trout, farmed, cooked | 3 oz | 16.2 | 81 |
| Salmon, sockeye, cooked | 3 oz | 14.2 | 71 |
| White mushrooms, raw | ½ c | 9.2 | 46 |
| Milk (2%), vitamin D-fortified | 1 c | 2.9 | 15 |
| Atlanta sardines, canned in oil | 2 each | 1.2 | 6 |
| Egg, scrambled | 1 large | 1.1 | 6 |
| Tuna fish, canned in water | 3 oz | 1.0 | 5 |
| Cheddar cheese | 1 oz | 0.3 | 2 |
| Chicken breast, roasted | 3 oz | 0.1 | 1 |
The RDA for vitamin D is 15 mcg/day for men and women. The UL for vitamin D is 1,000 mcg/day for supplemental intake. Vitamin D toxicity is rare but can also raise blood levels of calcium leading to increased risk of kidney stones and more seriously, vascular and tissue calcification.24
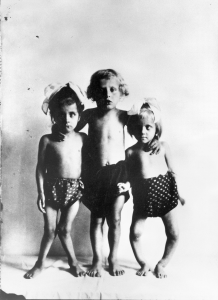
A deficiency of vitamin D in children can lead to rickets. This is characterized by soft, weak, deformed bones that are exceptionally susceptible to fracture. In adults, vitamin D deficiency causes a similar disease called osteomalacia, which is characterized by low bone density. Osteomalacia has the same symptoms and consequences as osteoporosis and often coexists with osteoporosis. Vitamin D deficiency is common, especially in the elderly population, darker skinned populations, and in the many people who live in the northern latitudes where sunlight exposure is much decreased during the long winter season. This is why most milk is now fortified with vitamin D.
Vitamin E
Vitamin E occurs in eight chemical forms, of which alpha-tocopherol appears to be the only form that is recognized to meet human requirements. It was discovered in 1922, isolated in 1936, and first made in a lab in 1938.6 Vitamin E is an antioxidant that is primarily responsible for protecting cell membranes against lipid destruction caused by free radicals. When alpha-tocopherol interacts with a free radical it is no longer capable of acting as an antioxidant unless it is enzymatically regenerated. Vitamin C helps to regenerate some of the alpha-tocopherol, but the remainder is eliminated from the body. Therefore, to maintain vitamin E levels, you need to regularly consume it as part of your diet. Other important functions of vitamin E include enhancing dilation of blood vessels and inhibiting the formation of blood clots.
Vitamin E is found in many foods, especially those higher in fat, such as nuts and oils. Some spices, such as paprika and red chili pepper, and herbs, such as oregano, basil, cumin, and thyme, also contain vitamin E. But keep in mind spices and herbs are commonly used in small amounts in cooking and therefore are a lesser source of dietary vitamin E.
Table 13.4.3 Vitamin E Content of Various Foods25
| Food | Serving | Vitamin E (mg) | %DV |
| Sunflower seeds, dry roasted | 1 oz | 7.4 | 49 |
| Almonds, dry roasted | 1 oz | 6.8 | 45 |
| Sunflower oil | 1 tbsp | 5.6 | 37 |
| Hazelnuts, dry roasted | 1 oz | 4.3 | 29 |
| Peanut butter | 2 tbsp | 2.9 | 19 |
| Spinach, boiled | ½ c | 1.9 | 13 |
| Broccoli, boiled | ½ c | 1.2 | 8 |
| Kiwifruit | 1 medium | 1.1 | 7 |
| Tomato | 1 medium | 0.7 | 5 |
| Mango, sliced | ½ c | 0.7 | 5 |
The AI for vitamin E is 15 mg mg/day for men and women. The UL for vitamin E is 1,000 mg/day and applies only to supplemental intake. Supplementation of alpha-tocopherol in animals has been shown to cause hemorrhage and disrupt blood coagulation. Extremely high levels of vitamin E can interact with vitamin K dependent clotting factors causing an inhibition of blood clotting.25
Vitamin E deficiency is rare and overt deficiency symptoms have not been seen in healthy people. People with malabsorption disorders, such as Crohn’s disease or cystic fibrosis, and babies born prematurely, are at higher risk for vitamin E deficiency.25
Vitamin K
Vitamin K refers to a group of fat-soluble vitamins that are similar in chemical structure. It was discovered in 1929, isolated in 1939, and first made in a lab in 1940.6 Vitamin K is critical for blood function acting as a coenzyme in blood coagulation (or blood clotting). Blood clotting proteins are continuously circulating in the blood. Upon injury to a blood vessel, platelets stick to the wound forming a plug. Without vitamin K, blood would not clot. Vitamin K is also required for maintaining bone health. It modifies the protein osteocalcin, which is involved in the bone remodeling process. All the functions of osteocalcin and the other vitamin K dependent proteins in bone tissue are not well understood and are being studied further.

Vitamin K is present in many foods, but is found in the highest concentrations in green vegetables such as broccoli, cabbage, kale, parsley, spinach, and lettuce. Additionally, vitamin K can be synthesized via bacteria in the large intestine. The exact amount is unknown, but it is likely less than 10% of the recommended intake. Newborns have low vitamin K stores and it takes time for the sterile newborn gut to acquire the good bacteria it needs to produce vitamin K. So, it has become a routine practice to inject newborns with a single intramuscular dose of vitamin K. This practice has basically eliminated vitamin K dependent bleeding disorders in babies.
Table 13.4.4 Vitamin K Content of Various Foods26
| Food | Serving | Vitamin K (mcg) | %DV |
| Collard greens, boiled | ½ c | 530 | 442 |
| Turnip greens, boiled | ½ c | 426 | 355 |
| Spinach, raw | 1 c | 145 | 121 |
| Kale, raw | 1 c | 113 | 94 |
| Broccoli, boiled | ½ c | 110 | 92 |
| Soybeans, roasted | ½ c | 43 | 36 |
| Pumpkin, canned | ½ c | 20 | 17 |
| Pine nuts, dried | 1 oz | 15 | 13 |
| Blueberries | ½ c | 14 | 12 |
| Canola oil | 1 tbsp | 10 | 8 |
The AI for vitamin K is 120 mcg/day for men and 90 mcg/day for women. There is no UL currently for vitamin K because of its low potential for toxicity.26
A deficiency in vitamin K causes bleeding disorders. It is relatively rare, but people who have liver or pancreatic disease, celiac disease, or malabsorption conditions are at higher risk for vitamin K deficiency. Signs and symptoms include nosebleeds, easy bruising, broken blood vessels, bleeding gums, and heavy menstrual bleeding in women. The function of the anticoagulant drug warfarin is impaired by excess vitamin K intake from supplements. Calcium additionally plays a role in activation of blood clotting proteins.
13.5 Free Radicals and Antioxidants
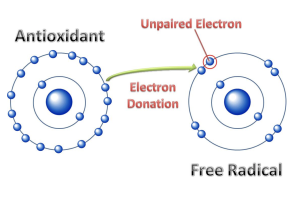
Before you can understand what an antioxidant is, it is important to have an understanding of oxidants. In chemistry, oxidation occurs when a molecule loses an electron. If another molecule picks up the lost electron, we say that this molecule with an added electron is reduced. Although this sounds like the opposite of addition, because electrons are negatively charged, the addition of a negative “reduces” the charge of the molecule. This oxidation-reduction system occurs in many instances in the body and in the environment.
Electrons prefer to be partnered together in molecules, so when an electron is lost and oxidation occurs, one electron is unpaired. A molecule with an unpaired electron is called a free radical. This molecule becomes highly reactive because it actively seeks an electron to partner with to stabilize it. These free radicals are called reactive oxidative species (ROS). Sometimes there are so many ROS formed that there are not enough extra electrons to pair with. When the formation of free radicals exceeds the body’s ability to provide electron relief, the body comes under oxidative stress, and the body cells and tissues become damaged.
Free radicals can be generated by a variety of sources that can be endogenous (coming from within the body) or exogenous (coming from outside the body). Endogenous sources include the body’s mitochondria where most of the body’s energy production occurs. High-intensity, long duration exercise like distance running, for example, increases the production of free radicals. Exogenous sources include ultraviolet light, ozone, radiation, heavy metals, smoking, air pollution, and asbestos.27 Accumulation of free radicals can cause inflammation. Free radical-induced damage, when left unrepaired, destroys lipids, proteins, RNA, and DNA, and can contribute to disease. Oxidative stress has been implicated as a contributing factor to cancer, atherosclerosis, arthritis, diabetes, kidney disease, Alzheimer’s disease, Parkinson’s disease, schizophrenia, bipolar disorder, emphysema, and cataracts.28
Not all free radicals are bad. While our bodies have acquired multiple defenses against them, we also use free radicals to support its functions. For example, the immune system uses the cell-damaging properties of free radicals to kill pathogens. First, immune cells engulf an invader (such as a bacterium), then they expose it to free radicals such as hydrogen peroxide, which destroys its membrane. The invader is thus neutralized. Scientific studies also suggest free radicals may aid with tissue repair when you get cut, help produce thyroid hormone, help dilate blood vessels, and act as chemical signaling molecules. However, we must attempt to maintain balance between the number of free radicals and our ability to neutralize them to avoid oxidative stress.
Antioxidants
Antioxidants are molecules that can combat free radicals and oxidative stress. They donate one of their electrons to a free radical to generate a stable compound (Figure 13.5.1). Many vitamins (and other compounds) serve as antioxidants (Table 13.5.1), and consuming a varied diet, rich in colorful plants is highly recommended to provide these critical nutrients that are free radical fighters.
Table 13.5.1 Some Antioxidants Obtained from the Diet and Their Related Functions
| Antioxidant | Functions Attributed to Antioxidant Capacity |
| Vitamin A | Protects cellular membranes, prevents glutathione depletion, maintains free radical detoxifying enzyme systems, reduces inflammation |
| Vitamin C | Protects DNA, RNA, proteins, and lipids, aids in regenerating vitamin E |
| Vitamin E | Protects cellular membranes, prevents glutathione depletion |
| Carotenoids | Free radical scavengers |
| Lipoic acid | Free radical scavengers, aids in regeneration of vitamins C and E |
| Phenolic acids | Free radical scavengers, protect cellular membranes |
Antioxidant Supplementation?
The market is flooded with advertisements for “super antioxidant” supplements teeming with molecules that block free radical production, stimulate the immune system, prevent cancer, and reduce the signs of aging. Based on the antioxidant supplement industry’s success, the general public appears to believe these health claims. However, these claims are not backed by scientific evidence; rather there is some evidence suggesting antioxidant supplements can actually cause harm. While scientists have found evidence supporting the consumption of antioxidant-rich foods, primarily vegetables and fruits, as a method of reducing risk of chronic disease, there is no “miracle cure.” No pill or supplement alone can provide the same benefits of a diet.
Key Takeaways
- There are 13 vitamins that are organic micronutrients classified by their solubility in fat or water and needed in very small amounts.
- Most vitamins come from whole foods like fruits, vegetables, meats, legumes, nuts, and seeds, but some vitamins can be made by microorganisms in our intestines.
- Vitamins have diverse biochemical functions.
- There are differences between fat-soluble and water-soluble vitamins in how they are absorbed, where they work in the body, where and if they are stored, and how easy it is to become deficient in the vitamin.
- The bioavailability of nutrients is affected by cooking, preparation, storage, medication, the age or health condition of the person, and consumption of medications, illicit drugs, or alcohol.
- Fortified foods have nutrients added, enriched foods have nutrients that were lost in processing replaced.
- There are two types of deficiencies of micronutrients: primary and secondary. Primary occurs because of lack of intake while secondary occurs because of an underlying disorder or lifestyle factor that affects bioavailability.
- Dietary Reference Intakes (DRIs) are a common set of reference values (EAR, RDA, AI, UL) for a healthy population based on the relationships between nutrient intakes and health or the prevention of disease.
- Water-soluble vitamins include all of the B vitamins (B-complex) and Vitamin C. Fat-soluble vitamins are A, D, E, and K. They have various food sources, functions, and some have deficiency diseases.
- Antioxidants help to fight free radicals by donating electrons to the unstable molecules to make them stable. Many vitamins serve as antioxidants.
Portions of this chapter were taken from OER Sources listed below:
Jellum, L., Hitzeman, J., Krauss, M., Henderson, S., Harnden, T., Elsberry, C., & Ford, G. (2018). Principles of Nutrition Textbook, Second Edition. Nursing and Health Sciences Open Textbooks. 5. https://oer.galileo.usg.edu/health-textbooks/5
Tharalson, J. (2019). Nutri300:Nutrition. https://med.libretexts.org/Courses/Sacremento_City_College/SSC%3A_Nutri_300_(Tharalson)
Titchenal, A., Calabrese, A., Gibby, C., Revilla, M.K.F., & Meinke, W. (2018). Human Nutrition. University of Hawai’i at Manoa Food Science and Human Nutrition Program Open Textbook. https://pressbooks.oer.hawaii.edu
Additional References:
- Carpenter, K. J. (2003). A short history of nutritional science: Part 2 (1885-1912). Journal of Nutrition, 133, 975-84.
- Carpenter, K. J. (2003). A short history of nutritional science: Part 3 (1912-1944). Journal of Nutrition, 133, 3023-32.
- Devi, R. (2015). Food processing and impact on nutrition. Scholars Journal of Agricultural and Veterinary Sciences, 2 (4A), 304-311. http://saspjournals.com/wp-content/uploads/2015/08/SJAVS-24A304-311.pd
- Gerrior, S., Juan, W., & Peter, B. (2006). An easy approach to calculating estimated energy requirements. Preventing Chronic Disease, 3(4), A129.
- Institute of Medicine Food and Nutrition Board. (1998). Dietary reference intakes: A risk assessment model for establishing upper intake levels for nutrients. National Academies Press (US). https://pubmed.ncbi.nlm.nih.gov/20845565/
- Price, C. (2015). Vitamania: How vitamins revolutionized the way we think about food. Penguin Books.
- Office of Dietary Supplements. (2020, June 3). Thiamin. National Institute of Health. https://ods.od.nih.gov/factsheets/Thiamin-HealthProfessional/
- Office of Dietary Supplements. (2020, June 3). Riboflavin. National Institute of Health. https://ods.od.nih.gov/factsheets/Riboflavin-HealthProfessional/
- Office of Dietary Supplements. (2020, June 3). Niacin. National Institute of Health. https://ods.od.nih.gov/factsheets/Niacin-HealthProfessional/
- National Institutes of Health. (n.d.) Dr. Joseph Goldberger & the War on Pellagra. National Institutes of Health, Office of NIH History & Stetten Museum. https://history.nih.gov/pages/viewpage.action?pageld=8883184
- Office of Dietary Supplements. (2020, June 3). Pantothenic Acid. National Institute of Health. https://ods.od.nih.gov/factsheets/PantothenicAcid-HealthProfessional/
- Office of Dietary Supplements. (2020, February 24). Vitamin B6. National Institute of Health. https://ods.od.nih.gov/factsheets/VitaminB6-HealthProfessional/
- Office of Dietary Supplements. (2020, June 3). Biotin. National Institute of Health. https://ods.od.nih.gov/factsheets/Biotin-HealthProfessional/
- Office of Dietary Supplements. (2020, June 3). Folate. National Institute of Health. https://ods.od.nih.gov/factsheets/Folate-HealthProfessional/
- Office of Dietary Supplements. (2020, March 30). Vitamin B12. National Institute of Health. https://ods.od.nih.gov/factsheets/VitaminB12-HealthProfessional/
- Douglas, R.M., Hemilä, H., Chalker, E., D’Souza R. R.D., Treacy, B., & Douglas, B. (2004). Vitamin C for preventing and treating the common cold. Cochrane Database of Systematic Reviews 4. https://doi.org/10.1002/14651858.CD000980.pub2
- Office of Dietary Supplements. (2020, February 27). Vitamin C. National Institute of Health. https://ods.od.nih.gov/factsheets/VitaminC-HealthProfessional/
- Worrall, S. (2017, January 15). A nightmare disease haunted ships during the age of discovery. National Geographic. https://www.nationalgeographic.com/news/2017/01/scurvy-disease-discovery-jonathan-lamb/#close
- White, M. (2016, October 4). James Lind: The man who helped to cure scurvy with lemons. BBC.com. https://www.bbc.com/news/uk-england-37320399
- Office of Dietary Supplements. (2020, June 3). Choline. National Institute of Health. https://ods.od.nih.gov/factsheets/Choline-HealthProfessional/
- Office of Dietary Supplements. (2020, February 14). Vitamin A. National Institute of Health. https://ods.od.nih.gov/factsheets/VitaminA-HealthProfessional/
- Goodman, G. E., Thornquist, M. D., Balmes, J., Cullen, M. R., Meyskens, F. L., Omenn, G. S., Valanis, B., & Williams, J. H. (2004). The beta-carotene and retinol efficacy trial: Incidence of lung cancer and cardiovascular disease mortality during 6-year follow up after stopping beta-carotene and retinol supplements. Journal of the National Cancer Institute, 96(23), 1743-50.https://doi.org/10.1093/jnci/djh320
- Sommer, A. (2008). Vitamin A deficiency and clinical disease: An historical overview. The Journal of Nutrition, 138(10), 1835-39. https://doi.org/10.1093/jn/138.10.1835
- Office of Dietary Supplements. (2020, March 24). Vitamin D. National Institute of Health. https://ods.od.nih.gov/factsheets/VitaminD-HealthProfessional/
- Office of Dietary Supplements. (2020, February 28). Vitamin E. National Institute of Health. https://ods.od.nih.gov/factsheets/VitaminE-HealthProfessional/
- Office of Dietary Supplements. (2020, June 3). Vitamin K. National Institute of Health. https://ods.od.nih.gov/factsheets/vitaminK-HealthProfessional/
- Lobo, V., Patil, A., Phatak, A., & Chandra, N. (2010). Free radicals, antioxidants and functional foods: Impact on human health. Pharmacognosy Reviews, 4(8), 118-126. https://doi.org/10.4103/0973-7847.70902
- Phaniendra, A., Jestadi, D. B., & Periyasamy, L. (2015). Free radicals: Properties, sources, targets, and their implication in various diseases. Indian Journal of Clinical Biochemistry, 30(1), 11-26. https://doi.org/10.1007/s12291-014-0446-0
Media Attributions
- 5F842728-B086-4FC5-916C-4F32369C6592
- 56F4CEB9-7237-4ED8-B4D2-25512AD051B9
- F9C11827-5687-467F-908F-F45894DDAAF6
- 1E02A87E-ACF9-42E5-B9B4-FEF98F803761
- 87A52EAB-CA66-4846-B4EF-4C15633C5B27
- 880FE2C7-6BB5-4CAF-B7D3-8AAA23E49EF4
- 819A1120-A033-42E7-980F-5E057543B226
- 99CCC6DD-24DA-4FEA-B4AC-147A6792FAA2
- 937BB474-A8CE-4279-9863-26A54D5B8B6D
- 38EC25E0-DBF1-48A3-B519-382D125F6DAE
- 1C17C730-541A-4B14-8ABF-FBEF972500CF
- ABA03AF4-A7C7-4897-A4D5-2565E77B9D7A
The amount of a substance that is absorbed, transported, and subsequently used in the body
fat located in and around body organs
fat found directly beneath the skin
being "toxic" or poisonous - able to cause damage to the body
Nutrients added to a food product that would not naturally occur in that product.
Replacement of nutrients that are lost with food processing.
nutrient deficiency caused by inadequate intake
Adequate intake of a nutrient occurs, but for some reason the body cannot use it so deficiency signs and symptoms occur.
Condition caused by deficiency of thiamin (vitamin B1)
Condition of deficiency of riboflavin (vitamin B2)
breakdown
building
Side effect in some people of excessive consumption of niacin (vitamin B3). Causes redness of the face, arms, chest due to vasodilation of small blood vessels. You may also experience tingling, burning and itching.
condition caused by severe niacin (vitamin B3) deficiency
The soaking of corn in wood ash or pickling lime to make the niacin more bioavailable. Native American cultures so it when making masa harina, the corn meal used to make corn tortillas and tamales.
substance made in the stomach that is required for vitamin B12 absorption; secretion of this substance slowly naturally declines after age 50
Condition caused by deficiency of vitamin C
Severe drying of the eyes caused by a deficiency of vitamin A
Condition of soft, weak, deformed bones in children caused by a deficiency of vitamin D
low bone density in adults
a molecule with an unpaired electron
an imbalance between reactive oxidative species (ROS) formed and the number of electrons available to neutralize them causing cell damage
