Chapter 9: Energy Balance and Disordered Eating
“Don’t dig your grave with your own knife and fork.”
-English proverb
As you probably already know, the number of people who struggle with being overweight or obese has been rising steadily in the US and in many other countries around the world. According to the World Health Organization (WHO), obesity has nearly tripled since 1975. Worldwide about 39% of adults (almost 2 billion people) are overweight, 650 million of these are obese. Most of the world’s population live in countries where obesity kills more people than underweight.1 In the US, obesity rates are even higher. Obesity is complicated. Many factors increase or decrease the likelihood that a person will develop obesity. In this chapter you will learn how to assess body weight and fatness. You will also learn that it is not only society and environment that play a role in body weight and fatness, but also physiology, genetics, and behavior—and that all of them interact. We will discuss the health risks of being underweight and overweight, learn evidence-based solutions to maintain body weight at the individual level, and assess the current state of affairs of combating the obesity epidemic in the US.
Learning Objectives
- Define hyperplasia vs hypertrophy of adipose tissue and their implications for weight loss or gain.
- Describe the prevalence of obesity in the US and obesogenic environments.
- Be able to calculate and categorize body mass index (BMI) given a particular weight and height and discuss the limitations of using BMI.
- Name the methods of assessment and factors that affect body composition and body fat distribution and how these relate to overall health.
- Discuss energy balance and be able to calculate estimated energy requirements (EER).
- Summarize the factors involved in total daily energy expenditure (TDEE) and the factors affecting basal metabolic rate (BMR).
- Summarize factors affecting energy intake and energy expenditure.
- Describe health risks associated with being overweight and underweight.
- Differentiate among the various forms of eating disorders.
- Explain the characteristics of successful weight management.
- Differentiate among the various forms of weight loss surgery.
9.1 Obesogenic Environments and Obesity Rates
Adipose tissue contains fat cells. In the body, adipose tissue can grow two ways: the number of fat cells can increase (hyperplasia), or the existing fat cells can grow in size (hypertrophy). Genes and diet affect these two growth mechanisms. In general, during periods of growth, both mechanisms occur—fat cells increase in size and in number. This means that from the time we are conceived until we stop physically growing (the end of puberty), we experience both hypertrophy and hyperplasia of fat cells. Once we are adults, our adipose tissue primarily undergoes hypertrophy with only very limited hyperplasia in extreme circumstances. To summarize, when children gain weight they gain both size and number of fat cells. Those cells remain in the body into adulthood. Children who are overweight or obese are much more likely to remain that way throughout their lifetime, partly because of the number of fat cells they created during childhood. As adults, only the size of the fat cell changes. When weight is gained, hypertrophy of adipose tissue occurs. When weight is lost, atrophy (shrinking) of fat cells occurs, but the number of fat cells remain. That may partly explain why lost weight so easily returns.
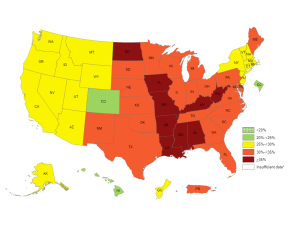
The prevalence of obesity has increased greatly since 1980. There is a term being used to try to understand this rapid rise in obesity: obesogenic environment. The Centers for Disease Control and Prevention (CDC) defines an obesogenic environment as “an environment that promotes increased food intake of non-healthful foods, and physical inactivity.” The CDC reports that in 2017-18 in the US, 42.4% of adults (up from 30% in 1999) have obesity, and 9.2% of adults struggle with severe obesity.2 In children aged 2-19 years, the prevalence of obesity is 18.5%, lowest in ages 2-5, highest in ages 12-19. These numbers have tripled since 1980.3 The health consequences of too much body fat are numerous and include increased risks for cardiovascular disease, type 2 diabetes, and some forms of cancer. The medical costs related to obesity are over $147 billion (up from $78.5 billion in 1998) and on the individual level, people who are obese spend $1,429 more per year for medical care than people of healthy weight.4 No one wants to become obese, so what are the factors causing rates of obesity to rise so rapidly? What can we do about these factors?
Numerous obesogenic agents contribute to the immense public health problem that has become a part of everyday life in American society. People consume more than half of their meals outside the home. Food portions have been getting bigger since the 1960s, and in the 1990s North American society experienced the “super-size” marketing boom, which is still very popular. Another factor is physical inactivity is becoming more common. Between 1960 and 2000 more than 123 million vehicles were added to American society. Escalators, elevators, and horizontal walkways now dominate shopping malls and office buildings, factory work has become increasingly mechanized and automated, the typical American spends more than four hours daily watching a screen for non-work activities, and in many workplaces the only tools required to conduct work are a chair, a desk, and a computer. The list of all the societal obesogenic factors goes on and on. They are the result of modernization, industrialization, and urbanization without individuals, public health officials, or government adequately addressing the concurrent rise in overweight and obesity.2
9.2 Indicators of Health: Body Mass Index, Body Composition, and Fat Distribution
Although the terms “overweight” and “obese” are often used interchangeably and considered as gradations of the same thing, they can denote different things. You weigh what you weigh because of your: water weight, lean muscle weight, bone weight, and weight from body fat (adipose). Overweight refers to having more weight than is typical for a particular height. That weight may be the result of water weight, muscle weight, or fat mass. Obese refers specifically to having excess body fat. In most cases people who are overweight also have excessive body fat and therefore body weight is an indicator of obesity in much of the population.
Often people ask how much they “should” weigh. The idea that there is an “ideal” weight is problematic. The focus should be on how healthy you are, not a number on the scale. Each of us should focus on eating healthfully (not just saying it, but doing it) and exercising regularly. However, medical doctors, public health officials and others needed to find a simple tool to look at patterns of weight gain in the US and elsewhere. The easy tool that was developed is called the Body Mass Index (BMI). BMI is a tool meant to tell an individual if they weigh too much, too little or just right. BMI uses the information that we already have readily available from every doctor’s visit: weight and height. The general idea is, if you are very tall and have a low weight you are probably underweight. If you are very short and you weigh a lot you are probably overweight. It is a crude tool but one that can quickly and inexpensively give estimates of overweight and/or underweight for large populations.
Body Mass Index (BMI)
BMI is calculated using height and weight measurements and is more predictive of health risk than using weight alone. BMI measurements are used to indicate whether an individual may be underweight (with a BMI less than 18.5), overweight (with a BMI over 25), or obese (with a BMI over 30). The BMI is defined as the body mass divided by the square of the body height, and is universally expressed in units of kg/m2, resulting from weight in kilograms and height in square meters. Please note that this equation applies only to adults. For children aged 2-19 years, BMI is age and sex specific.
The BMI attempts to quantify the amount of tissue mass (muscle, fat, and bone) in an individual and then categorize that person as underweight, healthy weight, overweight, or obese based on that value. However, there is some debate about where on the BMI scale the dividing lines between categories should be placed. See Table 9.2.1 for the commonly accepted BMI ranges. If you would like to check your BMI, you can visit the National Heart, Lung, and Blood Institute or the CDC websites and use their automatic BMI calculators.
Table 9.2.1 Categories of BMI5
| Category | BMI (kg/m2) |
| Underweight | < 18.5 |
| Healthy Weight | 18.5 – 24.9 |
| Overweight | 25 – 29.9 |
| Obese | > 30 |
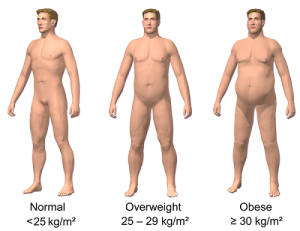
For most adults, BMI is a good indicator of risk. In general, the higher the BMI the higher the risk for chronic conditions like heart disease, type 2 diabetes, gallstones, osteoarthritis, sleep apnea, and certain cancers (colon, breast, endometrial, gallbladder).6 BMI does not diagnose body fatness or the health of an individual and it should not be used in this manner. However, very high AND very low BMI appears to increase a person’s risk of dying prematurely from all causes. If you look at a graph of BMI as it relates to this risk, it has a “J shaped Curve” or a “U shaped Curve” because being too low or too high both raise your risk. Instead, you’d like to be in the middle range of the BMI which is what they use for “healthy weight.” Even though you will be categorized as “overweight” at a BMI of 25 and “obese” at a BMI of 30, the risk of premature mortality goes up gradually. The decision of exactly where to draw the lines for underweight, healthy weight, overweight and obese are somewhat arbitrary.
Limitations of the BMI
BMI is a fairly simple measurement but does not take into account fat mass or fat distribution in the body, both of which are additional predictors of disease risk. Body fat is less dense than muscle mass, so the same volume of body fat will weigh less than that of muscle. Therefore, BMI can sometimes underestimate the amount of body fat in overweight or obese people and overestimate it in more muscular people. For instance, a muscular athlete will have more muscle mass than a couch potato of the same height. Based on their BMIs the muscular athlete may be categorized as more overweight or obese than the couch potato; however this is an infrequent problem with BMI calculation. Most adults do not have muscular bodies like athletes so BMI is a useful tool to provide general information for most people. Additionally, BMI tends to underestimate body fat in older populations. Overall, BMI is a useful, inexpensive tool to categorize people and is highly correlated with disease risk, but other measurements are always needed to individually diagnose obesity and more accurately assess an individual’s risk of developing disease.
Measuring Body Fat Content (Body Composition)
Water, organs, bone tissue, fat, and muscle tissue make up a person’s weight, and body composition is the ratio of a person’s body fat to everything else (water, bone tissue, muscle, organs) which we call “lean” or “fat free mass (FFM).” We all need some body fat in order to survive (calledessential fat) with a little left over to fuel movement and for emergencies (storage fat). Having more fat mass may be indicative of disease risk, but fat mass also varies with sex, age, and physical activity level. Females have more total fat mass, which is needed for reproduction and, in part, is a consequence of different levels of hormones. The optimal fat content of a female is 20-30% of her total weight (12-15% essential plus 8-15% storage); while a male’s optimal fat content is 12-20% (3-5% essential plus 8-15% storage). We use percent body fat to indicate a person’s body composition. If a person has 20% fat mass, the other 80% is considered lean (fat free or FFM). There are various ways to estimate a person’s body composition with varying costs, portability, and levels of accuracy.
- Skinfold Measures. The simplest and lowest-cost way is the skinfold (sometimes called fatfold) test. A trained health professional uses a caliper to measure the thickness of subcutaneous fat at standardized places on the body—usually the chest, arm, waist, thigh, but other parts of the body are also used, and compares these measures to standards to estimate body fatness. The more locations measured the more accurate the test. It is a noninvasive, inexpensive, and fairly accurate method of measuring fat mass when measurements are taken by someone experienced in the technique, but similar to BMI, is compared to standards of mostly young to middle-aged adults. The calipers used to measure can range from $30-$300. They are portable so this form of measurement is easily done almost anywhere.
- Underwater Weighing. This technique is based on Archimedes’ principle of water displacement. Let’s say that you filled your bathtub with five inches of water. You then placed an infant in the water, and measured how much the level of the water rose with the infant in it. Now take out the infant, and you get into the water instead. Note the level change of the water when you are in it. The level has risen higher with you than it did with the infant because your body volume was larger and “displaced” more of the water in the middle of the tub, causing the water level on the edges to rise higher. To use this technique to estimate body composition requires a chamber full of water big enough for the whole body to fit in. First, a person is weighed outside the chamber and then weighed again while immersed in water. Bone and muscle are denser than water, but fat is less dense so it “floats.” Therefore, a person with a higher muscle and bone mass will “sink” and displace more water than a person with less bone and muscle mass. The person who displaces more water would have lower levels of body fat than a similar person who displaces less. Because this test requires access to special equipment and must be done by people with special training, it is expensive and is primarily done in research settings. An underwater weighing testing apparatus can cost $3,000-$5,000.
- Bioelectric Impedance Analysis (BIA). Although the body contains quite a bit of water, it is not equally distributed among body tissues. Muscle tissue is about 75% water while fat tissue is less than 25%. To estimate body fat percentage, this device measures how long it takes for a very low level electrical current to move through the body. The current will move faster through lean tissue (like muscle) due to its higher water content than it will through fat. Therefore the faster it moves the leaner you are. Some BIA machines look like and are used like typical scales that measure body weight and are sold for home use. Others can be handheld or use leads attached to your extremities. Because body water is such an integral part of the measurement it is imperative that subjects test only after they are well-hydrated. Machines can range from $50-$2,000 and vary widely in accuracy.
- Dual-energy X-Ray Absorptiometry (DEXA). This technique can be used to measure bone density. It can also determine fat content via the same method, which directs two low-dose x-ray beams through the body and determines the amount of the energy absorbed from the beams. The amount of energy absorbed is dependent on the body’s content of bone, lean tissue mass, and fat mass. Using standard mathematical formulas, fat content can be accurately estimated. This form of testing is the most accurate, but is also the most expensive with machines costing more than $100,000. This form of testing is primarily done in medical and research settings. Since this machine measures bone density so accurately, it is also the most common method for diagnosing osteoporosis.
- Air Displacement Plethysmography (BodPod). While underwater weighing is based on displacement of water, you can also estimate body mass (and body fat) using a machine that measures displacement of air. A machine called a BodPod that looks like a human sized egg is used. Cost for the machine ranges from $20,000-$30,000, but the test is accurate and easier to do than underwater weighing. Because of the high cost it is also most often done in research settings.
Measuring Fat Distribution
Total body fat mass or percent body fat is one predictor of health; another is how the fat is distributed in the body. You may have heard that it’s healthier to be shaped like a pear than it is to be shaped like an apple. That, in fact, seems to be true. Fat on the hips is better than fat around the belly, if total body fat is the same. Fat can be found in different areas in the body and it does not all act the same, meaning it differs physiologically based on location. Fat deposited around the organs in the abdominal cavity (abdominal obesity) is called visceral fat and is an additional predictor of disease risk. Visceral fat releases hormones and inflammatory factors that contribute to disease risk. Fat found under the skin throughout the body is called subcutaneous fat. This fat is less metabolically active, and so is not as dangerous as visceral. The most accurate way to measure abdominal obesity is via a computed topography (CT) or magnetic resonance imaging (MRI).
However, these types of tests are expensive and require not only special equipment, but also special training for interpretation. Scientists have found an inexpensive alternative that is useful for the general population and the only tool required is a measuring tape. Scientists have found that waist circumference measure correlates with disease risk. The measurement of waist circumference is taken at the natural waist (usually just above the belly button) (site B on Figure 9.2.2). Men with a waist circumference greater than 40 inches and women with a waist circumference greater than 35 inches are predicted to face greater health risks. Measures of less than 37 inches for men and 31.5 inches for women are considered low risk.7
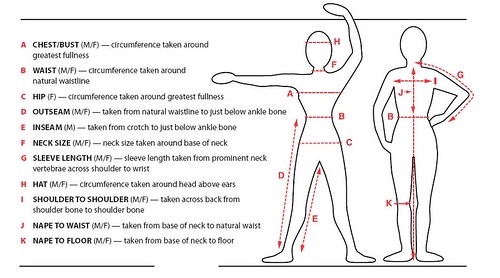
A second circumference measured at the hip, along with the waist circumference, is called the waist-to-hip ratio. This ratio can also be used to predict disease risk. For most conditions and populations it is considered a better measurement than waist circumference alone. To calculate your waist-to-hip ratio:
- Use a measuring tape to measure your waist circumference (site B, Figure 9.2.2)
- Measure your hip circumference at its widest part (site C, Figure 9.2.2)
- Divide the waist circumference by the hip circumference to arrive at your waist-to-hip ratio
Abdominal obesity is defined by the WHO as having a waist-to-hip ratio above 0.90 for males and above 0.85 for females. Observational studies have demonstrated that people with “apple-shaped” bodies (who carry more weight around the waist) have greater risks for chronic disease than those with “pear-shaped” bodies (who carry more weight around the hips). A study published in the November 2005 issue of Lancet with more than 27,000 participants from 52 countries concluded that the waist-to-hip ratio is highly correlated with heart attack risk worldwide and is a better predictor of heart attacks than BMI.8
9.3 Energy Balance
Balancing energy intake means consuming the right amount of calories that your body requires, not more, not less. Recall that the macronutrients you consume are either converted to energy, stored, or used to synthesize macromolecules.
The main function of carbohydrate is to provide a source of energy (4 kcal/g). After it is consumed, digested, absorbed into the blood and taken to the liver, it can then be used immediately for energy, or stored as glycogen in liver or skeletal muscle. Glycogen storage sites are finite in size so if those glycogen stores are full, the remaining glucose can be converted to storage fat. Lipids are our main source of energy, providing 9 kcal/g. Lipids are easily stored in our adipose tissue to be used by the body for energy (like filling your car with gasoline). Protein can also be used for energy (4 kcal/g), although that is not its primary function. Protein in the body has many functions besides energy production, and is generally not used for energy unless intake of carbohydrate is low. Remember that excess protein is not stored as protein in the body. Proteins are used to make hormones, neurotransmitters, antibodies, and other body structures and secretions. If more protein is consumed than the body requires, the nitrogen is stripped from the amino acids, becoming urea and being eliminated by the body in urine. The rest of the amino acid can then be converted into glucose (gluconeogenesis) if glucose is unavailable, or stored as fat (lipogenesis).
Our bodies excel at saving excess calories as storage fat in adipose tissue—no matter their original source (carbohydrate, lipid, or protein). For the vast majority of human existence, excess calories were not an issue. Our ancestors had to hunt and gather, or toil for many hours to find or grow adequate calories to support life, so when excess calories were available, bodies adapted to store what they could in order to have enough stores to live on when adequate food was not available. It’s only been over the past few decades that this ability to so easily store excess calories as storage fat has become problematic.
A nutrient’s metabolic path is dependent upon energy balance. When you are in positive energy balance the excess nutrient energy will be stored as discussed above, or be used to grow (e.g., during childhood, pregnancy, and wound healing). When you are in negative energy balance you are not taking in enough energy to meet your needs, so your body will need to use its stores to provide energy. Energy balance is achieved when intake of energy is equal to energy expended. Weight can be thought of as a whole body estimate of energy balance; body weight is maintained when the body is in energy balance, lost when it is in negative energy balance, and gained when it is in positive energy balance. In general, weight is a good predictor of energy balance, but many other factors play a role in energy intake and energy expenditure. Some of these factors are under your control and others are not. Let us begin with the basics on how to estimate energy intake, energy requirement, and energy output. Then we will consider the other factors that play a role in maintaining energy balance and hence, body weight.
Estimating Energy Requirements
To maintain body weight, you have to balance the kcal obtained from food and beverages with the kcal expended every day. Here, we will review how to calculate your energy needs in kcal per day so that you can determine whether your caloric intake falls short, meets, or exceeds your energy needs. The National Academy of Medicine (NAM) has devised a formula for calculating your Estimated Energy Requirement (EER). It takes into account your age, sex, weight, height, and physical activity level (PA). The EER is a standardized mathematical prediction of a person’s daily energy needs in kcal per day required to maintain weight. It is, as the name suggests, an estimate for an average person of similar characteristics. EER values are different for children, pregnant or lactating women, and for overweight and obese people. Also, remember from Chapter 2 that the EER is calculated based on weight maintenance, not for weight loss or weight gain.
It can be calculated via the following formulas:
Adult male: EER = 662 – [9.53 x age (y)] + PA x [(15.91 x wt (kg)) + (539.6 x ht (m))]
Adult female: EER = 354 – [6.91 x age (y)] + PA x [(9.36 x wt (kg)) + (726 x ht (m))]
Note: To convert lb to kg, divide weight in lb by 2.2; To convert feet to meters, divide height in feet by 3.3; Use Table 9.3.1 to identify the appropriate PA value. Remember that most people greatly overestimate their PA level.
Table 9.3.1 Physical Activity (PA) Categories and Values
| Activity Level | Male PA value | Female PA Value | Description |
| Sedentary | 1.00 | 1.00 | No physical activity beyond that required for independent living |
| Low | 1.11 | 1.12 | Equivalent to walk up to 3 miles per day at 3-4 mph in addition to activities of independent living |
| Moderate | 1.25 | 1.27 | Equivalent of walking 3 to 10 miles per day at 3-4 mph in addition to activities of independent living |
| High | 1.48 | 1.45 | Equivalent of walking 10 or more miles per day at 3-4 mph in addition to activities of independent living |
Total Daily Energy Expenditure (TDEE)
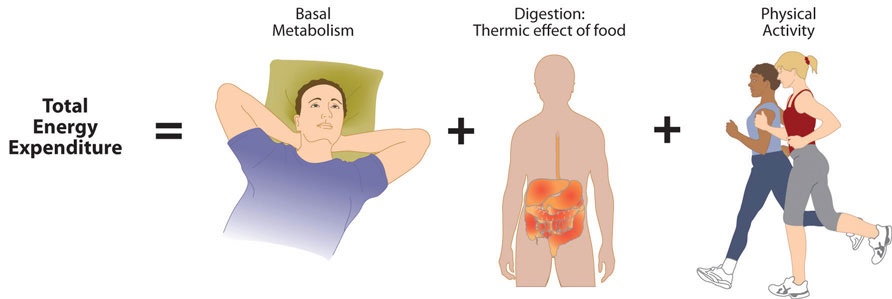
While EER is an estimate of the number of kcal a person needs to maintain their current weight, the total number of kcal (energy) a person actually expends daily is referred to as total daily energy expenditure (TDEE). The amount of energy you expend every day depends on many factors. For most people the largest portion is used for basal metabolism which is made up of those metabolic pathways necessary to support and maintain the body’s basic functions (e.g., breathing, heartbeat, liver and kidney function, brain function) while at rest. The basal metabolic rate (BMR) is the amount of energy required by the body to conduct its basic functions over a certain time period. Unless you are a professional athlete or have a job requiring hours and hours of physical labor, the great majority of daily energy expended (50-70%) is from conducting life’s basic processes. BMR is dependent on body size, body composition, sex, age, nutritional status, and genetics. People with a larger frame size have a higher BMR simply because they have more mass. Muscle tissue burns more calories than fat tissue even while at rest and thus the more muscle mass a person has, the higher their BMR. Since females typically have less muscle mass and a smaller frame size than men, their BMRs are generally lower. As we get older muscle mass declines and thus so does BMR. Nutritional status also affects basal metabolism. Caloric restriction as occurs while dieting, for example, causes a decline in BMR. This is because the body attempts to maintain homeostasis and will adapt by slowing down its basic functions to offset the decrease in energy intake. Body temperature and thyroid hormone levels are additional determinants of BMR.
Table 9.3.2 Factors influencing basal metabolic rate (BMR)
| Factors that Increase BMR | Factors that Decrease BMR |
| Stress | Aging |
| Large frame size | Small frame size |
| High amount of muscle tissue/muscle gain | Small amount of muscle tissue/muscle loss |
| High body temperature | Severe caloric restriction (fasting/starvation) |
| High thyroid levels | Low thyroid levels |
| Pregnancy/lactation | |
| Growth |
The second largest component of TDEE is the energy spent moving throughout the day. Physical activity increases energy expenditure significantly and it is recommended that adults get 150-300 minutes each week of moderate intensity physical activity. More about the recommendations for and additional health benefits of regular exercise can be found in Chapter 11, Nutrition and Fitness. Depending on lifestyle, the energy required for this ranges between 15-30% of total energy expended. However, in some athletes who spend many hours training, energy spent on physical activity can be much higher than 30% of TDEE. Energy used for physical activity is the most variable of all of the factors contributing to TDEE. It is the category of TDEE that one has the greatest ability to change by increasing one’s exercise.
Another component of TDEE is called the thermic effect of food (TEF) or diet-induced thermogenesis which is the energy required to digest, absorb, transport, and store nutrients from a meal. In general, the larger the meal the more time it takes to digest and absorb the nutrients. If you consume large amounts of food at a holiday meal, for example, you may feel warmer for a few hours following as you experience TEF. Why does this occur? Metabolism is the sum total of all chemical reactions taking place in the body. You may recall from previous chapters that many, many enzymatic reactions take place during food digestion and absorption, so a large meal requires more of those reactions. TEF accounts for up to 10% of your total energy expended per day.
In recent years another component has been recognized as part of TDEE: non-exercise activity thermogenesis (NEAT). This is the energy expended for everything we do that is not “sleeping, eating, or sports-like activities.”9 It consists of activities of daily living and ranges from fidgeting or typing to walking, standing, and yard work. It varies greatly from one person to another and from day to day, but can make up quite a large portion of daily expenditure. It also seems to play a major role in weight loss and weight maintenance with kcal expenditures up to 2000 kcal/day.10 To increase your NEAT, choose more activity throughout the day like taking stairs instead of an elevator, parking further from doorways when it is safe to do so, or using a standing desk instead of sitting at your workplace. A recent review of the literature showed that standing for six hours per day instead of sitting for those six hours can provide additional energy expenditure of about 54 kcals per day. If intake remains the same, this could be the equivalent of a loss of 2.5 kg (5.5 lb) per year.11
To summarize, the amount of energy you expend every day (total energy expenditure or TDEE) includes not only the kcal you burn during physical activity, but also the kcal you burn while at rest (BMR), the kcal you burn when you digest food (TEF), and the kcal you burn while doing the activities of daily living (NEAT).
Calculating TDEE can be tedious, but has been made easier as there are now calculators available online. TDEE is dependent on age, sex, height, weight, and physical activity level. The equations are based on standardized formulas produced from actual measurements on groups of people with similar characteristics. To get accurate results from web-based TDEE calculators, it is necessary to record your daily activities and the time spent performing them. A spreadsheet for doing so is available online at Health-calc.com. This website also offers an interactive TEE calculator.
9.4 Factors Affecting Energy Intake
Physiological Influences
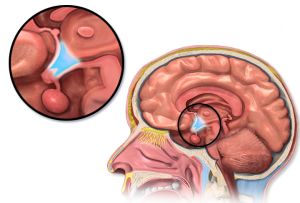
In the last few decades scientific studies have revealed that how much we eat and what we eat is controlled not only by our own desires, but is also regulated physiologically and influenced by genetics. The hypothalamus in the brain is the main control point of hunger. It receives hormonal and neural signals, which determine if you feel hungry or full. Hunger is an unpleasant sensation of feeling empty that is communicated to the brain by both mechanical and chemical signals from the periphery. Conversely, satiety is the sensation of feeling full and it is also determined by mechanical and chemical signals relayed from the periphery. The hypothalamus contains distinct centers of neural circuits that regulate hunger and satiety.
Hunger pangs are real and so is a “growling” stomach. When the stomach is empty it contracts, producing the characteristic pang and “growl.” The stomach’s mechanical movements relay neural signals to the hypothalamus, which relays other neural signals to parts of the brain. This results in the conscious feeling of the need to eat. The hormone ghrelin is released from the upper portion of the stomach when it is empty and is called the “hunger hormone.” Once released it travels through the blood to the hypothalamus, where it initiates signals in the brain to urge you to find food.
Alternatively, after you eat a meal the stomach stretches (gastric distension) which sends a neural signal to the brain stimulating the sensation of satiety and relaying the message to stop eating. The stomach also sends out certain hormones when it is full and others when it is empty.
Nutrients themselves also play a role in influencing food intake. The hypothalamus senses nutrient levels in the blood. When they are low the hunger center is stimulated, and when they are high the satiety center is stimulated. Carbohydrate is the most easily digestible macronutrient, so when glucose enters the blood it sends an early signal to the brain that food intake can slow or stop. Protein and lipids take longer to digest, and when they enter the blood they send a longer term signal that you are “full” between meals. Fiber in the intestines also signals fullness. Neural signaling, the hormone ghrelin, and nutrients in the blood are involved in short term regulation of food intake—changes in feeding behaviors in a single day.
Table 9.4.1 Summary of physiological influences on regulation of short term food intake (daily, meal to meal)
| Type of Signal | Result | |
| Empty Stomach | Neural: Empty stomach reduces stomach mechanical movements | Nerves in stomach walls send message to brain to initiate eating |
| Hormonal: Ghrelin | Released from top of stomach when empty; messages hypothalamus to initiate search for food; “hunger hormone” | |
| Full Stomach | Neural: Gastric distension (expansion of the stomach and increases in stomach mechanical movements) | Nerves in stomach walls send message to brain to stop eating |
| Circulating nutrients | Circulating carbohydrate promotes early satiety; circulating lipid and amino acids signal satiation between meals |
Fat tissue plays a role in regulating food intake over the long term—over weeks, months, or years. When insulin is released, it stimulates fat tissue to produce the hormone leptin, which communicates to the satiety center in the hypothalamus that the body is in positive energy balance. Because of this function it’s often called the “satiety hormone.” The discovery of leptin’s functions in the 1990s sparked a craze in the research world and in the diet pill industry as it was hypothesized that if you give leptin to a person who is overweight, they will decrease their food intake. Alas, this is not the case. In several clinical trials it was found that people who are overweight or obese are actually resistant to the hormone, meaning their brain does not respond as well to it.12 Therefore, when you administer leptin to an overweight or obese person there is typically no sustained effect on food intake. There are several other hormones that affect hunger and appetite such as cholecystokinen and neuropeptide Y.
Genetic Influences
Have you ever been frustrated by nutritional advice? One study may say a food provides great benefits, and another study says it should be avoided. It seems that scientists can’t make up their minds when it comes to nutrition. But could the different reactions to food be in our genes? As mentioned in chapter 1, scientists are studying nutrigenomics and nutrigenetics—links between food, your genes, and health outcomes—to try to determine if what you eat (or don’t eat) affects genes and health. Genes may explain why some people lose weight on a particular diet and some don’t, or why some patients respond well to a drug intervention and some experience negative side effects. What we know is that genetics plays a role in many health factors including body weight and food intake. It’s the nature versus nurture debate. We see that children who have been adopted typically are similar in weight and body fatness to their biological parents. Moreover, identical twins are twice as likely to be of similar weights as compared to fraternal twins.
Could the tendency to be overweight also be in the genes? The scientific search for obesity genes is ongoing and a few have been identified, such as the gene that encodes for leptin. However, overweight and obesity that manifests in millions of people is not likely to be attributed to one or even a few genes, but to rather the interactions of hundreds of genes with the environment. In fact, when an individual has a mutated version of the gene coding for leptin, they are obese, but only a few dozen people around the world have been identified as having a completely defective leptin gene. One day it may be possible to “eat based on your genes,” but more scientific research is needed.
Psychological and Behavioral Influences
When your mouth waters in response to the smell of a roasting Thanksgiving turkey and fresh out of the oven pie, you are experiencing a psychological influence on food intake called appetite. A person’s perception of good-smelling and good-tasting food influences what they eat and how much they eat. Mood and emotions are associated with food intake. Depression, low self-esteem, compulsive disorders, and emotional trauma are sometimes linked with increased food intake and obesity.
Certain behaviors can be predictive of how much a person eats. Some of these are how much food a person heaps onto their plate, how often they snack on energy dense, salty foods, how often they watch television or sit at a computer, and how often they eat out. Sometimes we eat because of the time of day, not because we are actually experiencing physical symptoms of hunger. Or we eat because of where we are or what we are doing. For example, if you are at a family reunion potluck dinner you may eat much more than if you were eating alone at home. Of course many behaviors are reflective of what we have easy access to—a concept we will discuss next.
Societal Influences
There are many societal influences on our food choices. We tend to eat differently when we are alone versus eating with friends or family. If you eat with someone who is eating a large amount, we tend to eat more. The opposite is also true. We are greatly influenced by our peers. They model what we perceive as acceptable behavior, and then we follow their lead. When you begin to date someone, often your eating behaviors change to match theirs, or their behaviors change to match yours. There is an intrinsic reward when our eating patterns converge with those with which we have close social connections.13
In addition to the influences on our eating behaviors from the individuals with whom we have relationships, it is without a doubt that the American society affects what and how much we eat. Portion sizes have increased dramatically over the past few decades. For example, a bagel is now more than twice the size it was in the 1960s. People unintentionally consume more kcal when portion sizes increase.14 Today, American teenagers have access to a massive amount of energy dense foods and beverages, which is a large contributor to the recent rapid increase in overweight and obesity in adolescents in this country. Even different cultures within the US have different eating habits. For instance, southern Americans, in general, consume more foods high in sodium, which is a contributing factor to their higher incidences of hypertension than Americans who live in the northern states.15
Eating away from home also plays a significant role in our eating behaviors and our health. It is almost impossible to drive down an urban thoroughfare and not see a restaurant or convenience store. Since 2010, more than half of our food budgets are spent on foods away from home, and these sources provide about 34% of total daily kcal. Quick-service restaurants (often called fast food or fast casual) provided the greatest source of these foods, but other sources such as prepared meals from grocery stores and convenience stores are also growing. These types of food tend to be higher in saturated fats and sodium, and lower in beneficial nutrients like iron, calcium, and fiber.16 Eating at these types of restaurants two or more times per week is associated with being overweight or obese, and having poor health status. However, just living near these types of restaurants was not associated with poor health.17
Eating Healthier while Eating Out
Support the consumer movement of pushing the fast food industry and your favorite local restaurants into serving more nutrient dense foods or smaller portions. You can begin this task by starting simple, such as requesting extra tomatoes and lettuce on your burger and more nutrient dense choices in the salad bar. You can also choose their low calorie menu options and help support the emerging market of healthier choices in the fast food industry. In today’s fast-paced society, it is difficult for most people to avoid fast food all the time. When you do need a quick bite on the run, choose the fast food restaurants that serve healthier foods. When you’re in a sit down restaurant where portion sizes tend to be large, ask if they have half-portions instead. The more people that ask, the more likely restaurants are to modify their menus to reflect more realistic portions.
9.5 Factors Affecting Energy Expenditure
Physiological and Genetic Factors
Why is it so difficult for some people to lose weight and for others to gain weight? One theory is that every person has a “set point” of energy balance. This set point can also be called a fat set point, meaning the brain senses body fatness and triggers changes in energy intake or expenditure to maintain body fatness within a target range. Some believe that this theory provides an explanation as to why after dieting, most people return to their original weight not long after stopping the diet. It is theorized that leptin may play a role in this. When people lose fat, leptin levels may also be reduced. This may mediate the satiety effect, causing an increase in food intake. Another theory is referred to as the “settling point” theory, which takes into account (more so than the “set point” theory) the contribution of the obesogenic environment to weight gain. In this model, the reservoir of body fatness responds to energy intake or energy expenditure, such that if a person is exposed to a greater amount of food, body fatness increases, or if a person watches more television body fatness increases. A third “dual intervention model” combines the two. Body weight homeostasis is complicated, and many factors play a role including genetics.18
It may be that there is some biological control, but environmental factors can override biology. Not all individuals who take a prescription weight loss drug lose weight and not all people who smoke are thin. An explanation for these discrepancies is that each individuals’ genes respond differently to a specific environment. Alternatively, environmental factors can influence a person’s gene profile, which is exemplified by the effects of the prenatal environment on body weight and fatness and disease incidence later in life. One of the first scientific investigations of prenatal control over energy balance was conducted in Germany. In this observational study, scientists found that offspring born to mothers who experienced famine were more likely to be obese in adulthood than offspring born to mothers who were pregnant just after World War II who lived in the same geographical locations.19 Other studies have shown that the offspring of women who were overweight during pregnancy have a greater propensity for being overweight and for developing type 2 diabetes.20 Thus, undernutrition and overnutrition during pregnancy may influence body weight and disease risk for offspring later in life. They do so by adapting energy metabolism to the early nutrient and hormonal environment in the womb.
Psychological and Behavioral Influences
One of the most important influences on energy expenditure is physical activity. Sedentary behavior is defined as the participation in the pursuits in which energy expenditure is no more than 1.5 times the amount of energy expended while at rest and includes sitting, reclining, or lying down while awake. Of course, the sedentary lifestyle of many Americans contributes to their average energy expenditure in daily life. Simply put, the more you sit, the less energy you expend. To maintain current weight, aim for 150-300 minutes of moderate intensity physical activity every week. Unfortunately, fewer than 25% of adults achieve this level of physical activity. To lose weight, more activity is required along with changes to dietary intake.21 Remember that activity does not have to be vigorous to provide positive results.22
Societal Influences
In the US, many societal factors play a role in determining energy expenditure. Escalators, moving walkways, and elevators (not to mention cars!) are common modes of transportation that reduce average daily energy expenditure. Office work, high stress jobs, and occupations requiring extended working hours are all societal pressures that reduce the time allotted for exercise of large populations of Americans. Many neighborhoods lack sidewalks or parks, and some are unsafe for outdoor activities. Even the remote controls for various electronic devices in homes contribute to the US society being less active.
Socioeconomic position has been found to be inversely proportional to weight gain meaning as income goes down, weight rises. One reason for this relationship is that inhabitants of lower income neighborhoods have reduced access to safe streets and parks for walking. Another is that fitness clubs are expensive and few are found in lower income neighborhoods. Often people must work multiple jobs to make ends meet, leaving little time for engaging in physical activity. The number of homeless in this country is rising with many children and adults living in hotels and cars. As you can imagine neither of these “home spaces” has a kitchen, making it impossible to cook nutritious meals and resulting in increased economically forced access to cheap, unhealthy foods, such as that at a nearby convenience store.
9.6 Health Risks of Being Overweight or Obese
As stated previously, worldwide obesity has nearly tripled since 1975, and 39% of adults and 18% of children in the world are overweight. Most of the world’s population live in countries where obesity kills more people than underweight. Obesity previously was a condition primarily in higher income countries, but is on the rise in developing countries as well.1 Obesity remains highest in the US, and worldwide obesity rates are highest in women, in ethnic minorities, and in those with lower incomes.23
According to the CDC, in the US in 2017-20182:
- 42.4% of adults age 20 years and older were obese
- 9.2% of adults had severe obesity (BMI>40)
- 30% of adults age 20 years and older were overweight (but not obese)
- 20.6% of adolescents age 12-19 years were obese
- 18.4% of children age 6-11 years were obese
- 13.9% of children age 2-5 years were obese
The health consequences of obesity are great. As BMIs increase over 25 kg/m2 risk increases for the development of chronic diseases including heart disease, cancer, type 2 diabetes, gallbladder disease, osteoarthritis, hormonal disorders, high cholesterol, sleep apnea, and liver disease.24 It is related to six of the top ten leading causes of death: heart disease, cancer, stroke, diabetes, kidney disease, and Alzheimer’s disease. Although obesity is not often listed on death certificates as causal, it is estimated that overweight and obesity are responsible for hundreds of thousands of deaths per year in the US.25
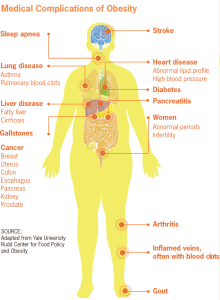
The individual consequences of obesity are great, but there are also societal costs. Obesity-related medical care costs top $147 billion. Annual nationwide productivity costs of obesity-related absenteeism range between $3.38 and $6.38 billion ($79-$132 per obese individual).24 There are also implications for armed forces recruitment and retention in the service. Overweight is the leading medical reason for failing to qualify for military service, with 27% of American young adults aged 17-24 unable to serve because of their weight. Many lose weight in order to meet the standards and enter the military, but are unable to maintain the weight loss so are at increased risk for administrative action including discharge. In 2008, among the active duty population, 60% of males and 40% of females were overweight, and over the last 15 years the rate of actively serving obese individuals has more than tripled. In 2010, more than 5.3% had at least one obesity-related medical diagnosis. In addition, approximately 70% of adult beneficiaries and 72% of military veterans are overweight or obese. There is a huge financial cost for the military, not just for the medical treatment of overweight or obese military personnel, their families, and veterans, but also for the lost monetary and training time investment in those who are discharged due to their weight.26
Binge Eating Disorder
While many recognized eating disorders are related to a lack of intake and a person being underweight, one, binge eating disorder (BED) is often associated with obesity. BED is the most common eating disorder in the US. People who have BED feel they have lost control over their eating and will periodically binge several thousand calories, but their loss of control over eating is not followed by fasting, purging, or compulsive exercise. As a result, people with this disorder are often overweight or obese, and their chronic disease risks are those linked to having an abnormally high body weight such as hypertension, cardiovascular disease, and type 2 diabetes. Additionally, they often experience guilt, shame, and depression. BED is commonly associated with depression and anxiety disorders. According to the National Institute of Mental Health (NIMH), BED is more prevalent than anorexia and bulimia combined, and affects 3.5% of females and 2.0% of males at some point during their lifetime. Treatment often involves antidepressant medication as well as nutritional and psychiatric counseling, and about 43% of people with this disorder seek treatment.27
9.7 Health Risks of Being Underweight and/or Disordered Eating
The 2015-2016 National Health and Nutrition Examination Survey (NHANES) estimated that 1.5% of adults have BMIs less than 18.5 kg/m2 in the US and are underweight.28 In children, 3% are considered underweight based on BMI for age.29 Being underweight is linked to nutritional deficiencies, especially iron deficiency anemia, and to other problems such as delayed wound healing, hormonal abnormalities, increased susceptibility to infection, and increased risk of some chronic diseases such as osteoporosis. In children, being underweight can stunt growth. The most common underlying cause of underweight in America is inadequate nutrition. Other causes are wasting diseases such as cancer, multiple sclerosis, tuberculosis, and eating disorders. People with wasting diseases are encouraged to seek nutritional counseling with a registered dietitian, as a healthy diet greatly affects survival and improves responses to disease treatments.
Disordered Eating
The term disordered eating describes a wide range of eating patterns and affect anyone at any age. Most of us have undertaken a disordered eating pattern at times such as avoiding a food group, eating what we perceive to be “clean,” or altering food intake and exercise patterns to achieve a specific goal. But when these behaviors become obsessive, more frequent, or being to interfere with personal or professional activities, the disordered eating has become problematic and may indicate an eating disorder. People who exhibit disordered eating may or may not meet the criteria for a diagnosed eating disorder. People who exhibit disordered eating may or may not meet the criteria for a diagnosed eating disorder. For example, a person may purge at times, but not often enough to meet the diagnostic criteria for bulimia. However, disordered eating without progression to a can be problematic and put people at risk for serious health consequences. Disordered eating behaviors can also progress to a diagnosable eating disorder.30 Signs and symptoms of disordered eating include30:
- Frequent dieting, anxiety associated with specific foods, and/or meal skipping
- Chronic weight fluctuations
- Rigid rituals and routines surrounding food and exercise
- Feelings of guilt and shame associated with eating
- Preoccupation with food, weight and body image that negatively impacts quality of life
- A feeling of loss of control around food, including compulsive eating habits
- Using exercise, food restriction, fasting or purging to “make up for bad foods” consumed
Eating disorders are serious but treatable conditions that can affect anyone. They are complex medical and psychiatric illnesses considered bio-psycho-social diseases which means that genetic, environmental, biological, and social elements all play a role. Surveys estimate that 20 million women and 10 million men in America will have an eating disorder at some point in their lives. There are many risk factors associated with eating disorders. These include a history of having an anxiety disorder or having a close relative with an eating disorder or a mental health condition like anxiety, depression, or addiction. Those experiencing body image dissatisfaction with a history of dieting or who are perfectionists with behavioral inflexibility are more likely to be diagnosed with an eating disorder. Society also plays a role. In the US there is a harmful weight stigma, leading to discrimination or stereotyping of a person based on their weight. Over 60% of those with a diagnosed eating disorder report that they experienced bullying, teasing, and/or weight shaming which contributed to the development of their disorder.31
For a diagnosis of an eating disorder one must meet the diagnostic criteria listed by the American Psychological Association Diagnostic Manual (DSM-5). The most common are anorexia nervosa, bulimia nervosa, and binge eating disorder.
Anorexia Nervosa
Anorexia nervosa, more often referred to as “anorexia,” is a treatable, life-threatening illness in which a person has an intense fear of weight gain. Their body image is distorted and they believe they are heavier than they actually are. There are two main types of anorexia: restrictive type (severe limitation of food intake), and binge/purge type (cycling between severe limitation of intake, leading to bingeing and purging). Anorexia results in extreme nutrient inadequacy and eventually to organ malfunction. Anorexia is relatively rare—the National Institute of Mental Health (NIMH) reports that 0.9% of females and 0.3% of males will have anorexia at some point in their lifetime, but it is an extreme example of how an unbalanced diet can affect health. The median age of onset is 18 years old.27 Anorexia frequently manifests during adolescence and those between 15 and 24 with anorexia have 10 times the risk of dying compared to their peers.32
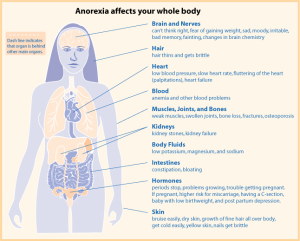
The primary signs and symptoms of anorexia are extremely restricted eating and/or intensive and excessive exercise, extreme thinness (emaciation), relentless pursuit of thinness and unwillingness to maintain a healthy weight, and intense fear of weight gain. The secondary signs and symptoms of anorexia are all related to the caloric and nutrient deficiencies of the unbalanced diet and include excessive weight loss, a multitude of skin abnormalities, diarrhea or extreme constipation, cavities/tooth loss, osteoporosis, low blood pressure, anemia, and infertility. Body temperature also falls due to the loss of fat for insulation. This can lead to lanugo which is the growth of fine hair all over the body. In extreme cases brain damage and multiple organ failure is possible and anorexia can be fatal. In fact, it has the highest mortality of all mental illnesses. Only about one-third of people with anorexia seek treatment specifically for this disorder.27
Bulimia Nervosa
Bulimia nervosa (bulimia), like anorexia, is a medical and psychiatric illness that can have severe health consequences. The NIMH reports that 0.5% of females and 0.1% of males will have bulimia at some point in their lifetime. Bulimia is characterized by episodes of eating large amounts of food (bingeing), while feeling a lack of control over eating behavior. This is followed by compensatory behaviors for the overeating including vomiting, the use of laxatives and/or diuretics, fasting, excessive exercise, or a combination of these (purging).
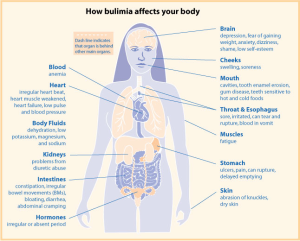
Unlike people with anorexia, those with bulimia often have a healthy or overweight BMI, making the disorder more difficult to detect and diagnose. The disorder is characterized by signs similar to anorexia such as fear of being overweight, extreme dieting, and bouts of excessive exercise. Secondary signs and symptoms include gastric reflux, severe erosion of tooth enamel, dehydration, electrolyte imbalances, lacerations in the mouth from vomiting, esophageal and peptic ulcers. Repeated damage to the esophagus puts people with bulimia at an increased risk for esophageal cancer. The disorder is also highly genetic, linked to depression and anxiety disorders, and most commonly occurs in adolescent girls and young women. About 43% of people with bulimia seek treatment which often involves antidepressant or antianxiety medications and nutritional and psychiatric counseling.27
Other Disordered Eating Patterns
There are several additional patterns of dietary intake that fall under the disordered eating category. Pica involves craving and consuming non-food substances such as ice, dirt, chalk, hair, and others. It is most often observed in children, pregnant women, and individuals with mental disabilities.33 Avoidant Restrictive Food Intake Disorder (AFRID) is also most often seen in children and is more than just “picky” eating. It is defined by a persistent failure to consume adequate calories to meet nutritional and/or energy requirements.31 Orthorexia is the unhealthy obsession with healthy eating until the number and amount of “acceptable” foods consumed does not meet body requirements. It is not an official eating disorder, but may be a form of obsessive-compulsive disorder.31 A category of eating patterns that may not meet specific diagnostic criteria but can be serious and life-threatening fall into a category called Other Specified Feeding or Eating Disorders (OSFED; formerly Eating Disorders Not Otherwise Specified or EDNOS). These can be atypical anorexia or bulimia, binge eating at low frequency or limited duration, purging disorder, or night eating syndrome.
Table 9.7.1 Eating Disorders: Characteristics and Associated Behaviors31
| Eating Disorder | Characteristics | Behaviors |
| Anorexia Nervosa | Weight loss or lack of appropriate weight gain in children and adolescents; difficulties maintaining appropriate body weight for height, age, stature; distorted body image; intense fear of weight gain | Calorie restriction (self-starvation); some may also experience binge/purge cycles and/or compulsive exercise; preoccupation with weight, food, kcal, dieting; food rituals; avoid meal times or situations involving food; restrained emotions; inflexible thinking; denial of hunger |
| Bulimia Nervosa | Bingeing on excessive kcal, then purging with compensatory behaviors (vomiting, exercise, laxatives, diet pills, diuretics, fasting); weight is typically healthy or overweight and may fluctuate greatly; dry hair, skin, and nails; may also struggle with co-conditions such as self-injury (ex. cutting), substance abuse, impulsivity | Large amounts of food missing in short time frame; evidence of purging such as frequent trips to bathroom after meals or smelling like vomit; stealing/hoarding food in strange places; excessive use of mouthwash, gum, mints; calluses on back of hand or swelling of cheeks or jaw; frequent dieting; withdrawal from family and friends; weight loss/dieting are primary concern |
| Binge Eating Disorder (BED) | Recurrent episodes of eating large quantities of food (often very quickly and to the point of discomfort); a feeling of a loss of control during the binge; experiencing shame, distress or guilt afterwards; not regularly using unhealthy compensatory measures (e.g., purging) | Eating alone because of embarrassment about the amount of food consumed; extreme concern with body weight or shape; frequent dieting; withdrawal from family, friends, and activities |
| Orthorexia (Not yet in DSM-5) | Obsession with proper or “healthful” eating (usually treated as a combination of anorexia and obsessive-compulsive disorder) | Compulsive checking of food labels and ingredient lists; only eating foods they consider “healthy” or “pure”; cutting out an increasing number of food groups; unusual interest in the health of what others eat; obsessive following of social media about health and healthy eating |
| Avoidant Restrictive Food Intake Disorder (ARFID) | Limitations in type and amount of food consumed, but does not involve stress about body shape/size or fear of fatness; common in those with other disorders like autism spectrum disorder, ADHD, anxiety disorders, intellectual disabilities | Dramatic food restriction; fear of choking; lack of appetite or interest in food; limited range of preferred foods that becomes narrower over time |
| Compulsive Exercise/Muscle dysmorphia (Not yet in DMS-5) |
Exercise that significantly interferes with important activities, occurs at inappropriate times or in inappropriate settings, or when the individual continues to exercise despite injury or other medical complications; Intense anxiety, depression, irritability, feelings of guilt, and/or distress if unable to exercise | Maintaining an excessive, rigid exercise regimen despite weather, fatigue, illness or injury; uncomfortable with rest/inactivity; uses exercise to manage emotions, permission to eat, and/or means of purging kcal; withdrawal from family and friends; feelings of not being fast enough, good enough, or pushing hard enough; |
Treating Eating Disorders
Like other illnesses, it is important to seek early treatment for eating disorders. People with eating disorders have a high risk of experiencing additional mental disorders such as anxiety or depression, and are at high risk for substance abuse. The risks of suicide and medical complications are also high. Treatment programs usually involve several health professionals including psychiatrists, psychologists, counselors, registered dietitians, and social workers.31 Treatment can be inpatient or outpatient, and must be tailored to the individual. Usually some sort of individual or group psychotherapy is involved and often includes family members. Some people benefit from medications such as antipsychotics, antidepressants, or mood stabilizers.27
Full recovery is possible, but can take months or years and high levels of commitment from all involved.31 Relapses are the norm rather than the exception. It is difficult to relearn normal eating habits and coping skills and often there are stressors that can initiate a return to disordered behaviors. These stressors include moving (going to college or moving away from home), infertility, pregnancy/birth of a baby, marriage or divorce, financial challenges, menopause, diagnosis of a disease, and/or death of a loved one. There are three areas that must be addressed during treatment: physical recovery, behavioral recovery, and psychological recovery. Goals of treatment include:31
- addressing any immediate medical concerns caused by the disorder,
- reducing or eliminating disordered behaviors,
- addressing issues like depression, anxiety or trauma, and
- developing a plan to prevent relapse.
9.8 Successful Weight Management
It is very apparent that carrying excess weight is problematic for the almost 70% of Americans who are overweight or obese. Successful weight loss is defined as individuals intentionally losing at least 10% of their body weight and keeping it off for at least one year.34 Most interventions include a reduction in kcal which results in early, rapid weight loss followed by a weight plateau, then a progressive regain of the weight. Within two years more than 50% have regained their lost weight. Within five years more than 80% of people have regained their lost weight, suggesting that fewer than 20% of participants are successful at weight loss as defined above. Many lose weight, but maintaining that loss is almost impossible.35
Why is it so difficult to maintain weight loss? It’s complicated, and scientists don’t yet know all of the answers. One reason is that we live in an obesogenic environment as discussed earlier in the chapter—one where we have easy access to inexpensive, energy dense foods, sedentary jobs, and sedentary lifestyles. Many also harbor unrealistic expectations about the amount of weight one can lose with moderate changes in diet or exercise levels. We’d like to think that we could just introduce a calorie deficit of 3500 kcals per week and we would lose one pound (lb) of body fat per week. However, that doesn’t take into consideration all of the hormonal adaptations that occur when weight is lost, which promotes weight regain.36 The weight plateau and subsequent regain occurs because of physiology, not psychology. Our bodies are designed to fight against weight loss because in the past it was detrimental to health. It’s estimated that for each kg of body weight lost (2.2 lb) there is a reduction in energy expenditure of 20-30 kcals per day. Hormonal influences increase appetite by about 100 kcal per day in an attempt to regain lost weight. There is a constant battle against this biology. Many blame themselves for this ‘failure’, but those who regain are not lazy or lacking willpower.37
Short term interventions such as popular fad diets are highly unlikely to provide lasting results. Most health professionals recommend a slow and steady weight loss averaging 0.5 to 2.0 lb per week, using a combination of dietary changes and increases in physical activity. This also requires ongoing long term support.36
Food for Thought
The National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) has a Body Weight Planner which allows you to make personalized calorie and physical activity plans to reach goal weight within a specific time period and to maintain it afterwards. Enter your proposed physical activity changes, the amount of weight you wish to lose, and the time frame, and it will provide a calorie recommendation for weight loss and weight maintenance.
The National Weight Control Registry (NWCR) tracks over 10,000 people who have been successful in losing at least 30 lb and maintaining this weight loss for at least one year. Their research findings are that 98% of participants in the registry modified their food intake and 94% increased their physical activity (mainly walking).38 Although there are a great variety of approaches taken by NWCR members to achieve successful weight loss, most report that their approach involved adhering to a low-calorie, low-fat diet and participating in high levels of activity (approximately one hour of exercise per day). Moreover, most “successful losers” eat breakfast every day, watch fewer than ten hours of television per week, and weigh themselves at least once per week. About half of them lost weight on their own and the other half used some type of weight loss program. In most scientific studies, successful weight loss is accomplished by changing the diet and increasing physical activity. Doing one without the other limits the amount of weight lost and the length of time that weight loss is sustained. On an individual level it is quite possible to achieve successful weight loss, as over 10,000 Americans can attest. Moreover, losing as little as 10% of your body weight can significantly improve health and reduce disease risk.39 You do not have to be overweight or obese to reap benefits from eating a healthier diet and increasing physical activity as both provide numerous benefits beyond weight loss and maintenance.
Evidence-Based Dietary Recommendations
Losing weight gradually and steadily is recommended. And small amounts of weight loss of just 5-10% can provide many health benefits. That means that if you currently weigh 200 lb, a loss of just 10-20 lb can provide improvements in blood pressure, cholesterol levels, and blood glucose control.40 The CDC provides steps for getting started on your weight loss journey.41
- Step 1: Make a commitment. The most important first step is to make a commitment to yourself. Some people find it useful to write down the reasons they want to lose weight and the changes they are willing to make. Then sign it, like a contract.
- Step 2: Take stock of where you are. You have to know where you are to figure out where you are going. Use the ABCDEF tools of nutrition assessment discussed in Chapter 1 to find your baseline and identify changes that may be beneficial. Keeping a food diary for a few days may provide some insights into what, where, and when you are eating. Your healthcare provider can help evaluate your current health and weight status based on your BMI, lab values, and other measures. Examine your current lifestyle to identify things that may pose challenges to your lifestyle changes such as a busy schedule reducing your ability to exercise, or co-workers who bring high-calorie items to share. On the other hand, there may be aspects of your current lifestyle that can help you lose weight so identify those too.
- Step 3: Set realistic goals. Goal setting is not easy, and most people set goals that are too vague, so they never achieve them. Goals should be specific and realistic. “Exercise more” is not specific enough. Instead, a goal like “I will walk 15 minutes during my lunch hour Monday through Friday at the park across the street from my office” is very specific and realistic. If your big goal is to lose 30 lb, start with 5. When you’ve achieved the 5 lb loss, reward yourself before going on to the next 5 lb. Expect and plan for occasional setbacks. When they happen, get back on your plan as soon as possible, and take some time to think about what you’ll do differently if the same thing happens again. Choose healthy foods and activities that you enjoy. Everyone is different, so what works for your neighbor may not work for you. It may take trying multiple activities before you determine what’s best for you.
- Step 4: Identify a support system. Enlist friends, family, coworkers, or a support group to help you on your weight loss journey.
- Step 5: Check in with yourself to monitor your progress. Keep a journal of what’s working and not working for you, and modify accordingly. Use the ABCDEF tools to reassess. If you are consistently achieving your goals, add a new goal. Reward yourself for your achievements using non-food items such as fresh flowers, spa day, or new clothing.
The 2020-2025 Dietary Guidelines for Americans offers specific, evidence-based recommendations for dietary changes aimed at keeping calorie intake in balance with physical activity, which is key for weight management.42 The focus is on consuming a healthy eating pattern over the course of days, weeks, months and years versus focusing on a single meal or snack. Focus on variety, consuming nutrient dense foods such as fruits and vegetables, and limiting kcal from added sugars and saturated fats. Shift to healthier food and beverage choices. Chapter 2 discussed dietary guidelines in detail.
Dietary changes should be gradual. The CDC recommends that you reflect on your current dietary intake, identifying both your positive and negative eating habits, and common triggers for unhealthy eating. Maybe you eat really fast, or while standing instead of sitting at a table. Maybe you eat when you’re not really hungry, or always feel that you have to clean your plate. Maybe you skip meals, making you really hungry later in the day. Once you’ve identified some of these unhealthy habits, strategize about how to replace them with healthier practices. Maybe planning meals ahead or slowing down your eating so that you can concentrate on the signals your body is giving you would be ways to minimize your unhealthy eating patterns. After making some of these changes, reinforce your good habits by rewarding yourself. Be patient with yourself. Even if you make a food choice you regret, you can get back on track with your next food choice. All is not lost.43
Tips for Restaurant Ordering including Takeout or Delivery
With Americans consuming more than half of their meals from restaurants, it is helpful to be able to decipher menu terms when ordering. Terms like “crunchy,” “crispy,” “battered,” “breaded,” “creamy,” “cheesy,” and “Alfredo” generally mean the food is higher in fat (especially saturated fat) or kcal. Instead choose “baked,” “grilled,” “roasted,” “steamed,” “marinara,” or “al fresco.” Terms like “Teriyaki,” “barbecue” or “sweet” often indicate a higher sugar content. When ordering sides, skip the fries and choose steamed vegetables or fruits. Sauces and dressings should be ordered “on the side” so that you can control how much you actually serve yourself, and choose low- or no-calorie beverages like water or unsweetened tea.
If you’re eating in a restaurant that serves free pre-meal items like chips and salsa or breadsticks, ask that they be removed or put some on a plate to eat instead of eating directly from the serving bowl. Once your food comes to your table, ask immediately for a “to-go” container. Restaurant portion sizes tend to be large, so before starting on your meal, put half of it into the container and set aside (as long as you are going directly home after the meal). Most people are satisfied with half of the portion. Then you’ll have a second meal for lunch the next day. If you’re getting food delivered, ditch the containers and serve yourself on a plate so that you can see the portions.
Weight Loss Surgery
For those with severe obesity who struggle to lose weight through dietary change and exercise alone, or those with severe health conditions related to obesity, weight loss or bariatric surgery may be an option. There are several different types. While all types will reduce the amount of food you can comfortably consume at one time, some also modify how food is digested and/or absorbed. All types have risks and complications, so the decision to have bariatric surgery should not be taken lightly. Most people who have weight loss surgery lose weight rapidly, but regain some weight later. However, those who follow diet and exercise recommendations and maintain their medical follow up appointments can keep weight off.
Bariatric surgery can improve many health conditions related to obesity such as type 2 diabetes, high blood pressure, unhealthy cholesterol levels, and sleep apnea. Many patients see their quality of life improve as well, with improved physical functionality and mood. However, there can be risks or complications including infections, diarrhea, nutritional inadequacies, gallstones, hernias, or others.44 Most surgeries now are done laparoscopically which means they make several small cuts in the abdomen and insert surgical tools into the cuts as opposed to one very large incision. A scope with a camera is also inserted, and the camera projects the images onto a video monitor. This type of surgery causes less pain and scarring and may lead to faster recovery. In the US, three types of bariatric surgery are most commonly used.
Gastric Banding (LAGB)
The Food and Drug Administration (FDA) has approved laparoscopic adjustable gastric banding (LAGB) for those with a BMI greater than 30 kg/m2 with one or more diagnosed health problems associated with obesity. In this type of surgery, a band containing an inner inflatable tube is placed around the top of the stomach, creating a small pouch. The pouch limits the amount of food that can be consumed before feeling full. A small port is placed in the abdomen under the skin which holds a saline solution. Using a syringe, the surgeon can inject or remove the solution, which changes the inflation level of the tube, increasing or decreasing the size of the stomach pouch. After surgery it may take several adjustments to find the right size for the patient and weight loss success depends on strict adherence to the recommended diet. This is currently the only reversible bariatric surgery as the band can be removed if the patient has problems.45
Gastric Sleeve (Sleeve Gastrectomy)
In this type of bariatric surgery, the stomach is cut vertically and about 80% of the stomach is removed. What remains of the stomach is about the size and shape of a banana and is closed with staples. This type of surgery helps reduce weight by decreasing the amount of food that can be comfortably consumed, and by surgically removing the part of the stomach that releases gut hormones like ghrelin (the hunger hormone) and gut bacteria that may affect appetite and metabolism. This type of surgery is permanent.45
Gastric Bypass (Roux-en-Y)
In this type of bariatric surgery, the stomach is stapled creating a very small pouch (about the size of a golf ball and able to hold about one oz of food) in the upper section. The surgeon also cuts the small intestine in the jejunum, and attaches the lower part of it directly to the stomach pouch. Food bypasses most of the stomach and the duodenum and first section of the jejunum. However, the duodenum is still attached to the main part of the stomach so digestive juices still move through the pyloric sphincter. The end of the top part of the intestine is attached further down the ileum, so that these digestive juices can mix with the food from the stomach pouch. This bypass also modifies gut hormones and other factors that promote satiety and suppress hunger. It produces significant long term weight loss (60-80% excess weight loss). However, it can lead to long term vitamin or mineral deficiencies, especially vitamin B12, folate, iron, and calcium. It is difficult to reverse this type of surgery although it is possible if medically necessary to do so.45
9.9 What We Can Do
The main causes of the obesity epidemic worldwide are the increased intake of energy dense food and decreased level of physical activity that is mainly associated with modernization, industrialization, and urbanization. The environmental changes that contribute to the dietary and physical activity patterns of the world today are associated with the lack of policies that address the obesity epidemic in the health, urban planning, agriculture, food industry, and education sectors.23 Changes are needed now to remedy this growing problem. Policies are being created, implemented, and reinforced at all levels of society including: education, agriculture, industry, urban planning, health care, and government. Reversing and stopping obesity are two different things. The former will require much more societal and individual level change than the latter. The following are some ideas or practices for constructing an environment in America that promotes health and confronts the obesity epidemic:
- Individual Level: What you can do NOW
- Purchase fewer prepared foods and eat more whole foods.
- Decrease portion sizes when eating or serving food.
- Eat out less, and when you do eat out choose low-calorie options.
- Walk or bike to work. If this is not feasible, walk while you are at work.
- Take the stairs when you come upon them or better yet, seek them out.
- Walk your neighborhood and know your surroundings. This benefits both health and safety.
- Reduce non-work screen time.
- Community Level: What you and your friends, family and co-workers can do together
- Request that your college/workplace provides more access to healthy low-cost foods.
- Support changes in school lunch programs—this is happening now but needs vocal parents to continue!
- Participate in cleaning up local green spaces and then enjoy them during your leisure time, get outside!
- Patronize local farms, farmer’s markets, and fruit and vegetable stands.
- Talk to your grocer and ask for better whole food choices and seafood at a decent price.
- Ask your favorite restaurant to serve more nutritious food and provide portion size options such as “lunch” portions at dinner or half-portions any time.
- National Level: What we can do as a country
- Support policies that increase the ability to walk and cycle safely in cities.
- Support national campaigns addressing obesity, such as America on the Move.
- Support policies that support local farmers and the increased access and affordability of healthy food.
Key Takeaways
- Obesity is a multi-faceted condition, with rising numbers of overweight and obese in the US and the world.
- Hyperplasia is an increase in number of cells including fat cells and occurs during periods of growth from conception through puberty; hyperplasia is an increase in cell size and occurs in childhood and adulthood. Atrophy is a decrease in size that can occur during weight loss.
- Body mass index (BMI), body fat distribution, and total body fat are all correlated with disease risk. There are various ways to estimate body composition, each with it’s own advantages and limitations.
- Energy balance is achieved when energy intake is equal to energy expended. Estimated Energy Requirements (EER) and Total Daily Energy Expenditure (TDEE) can be calculated.
- The amount of energy you expend every day (TDEE) includes not only the kcal you burn during physical activity, but also the kcal you burn at rest (basal metabolism), and the kcal you burn when you digest food (TEF), and the kcal you use doing activities of daily living (NEAT). Basal metabolic rate (BMR) is dependent on body size, body composition, sex, age, nutritional status, genetics, body temperature, and thyroid hormone levels. The great majority of energy expended (50-70%) daily comes from conducting life’s basic processes. The main control a person has over TDEE is to increase physical activity.
- Energy intake is regulated by complex physiological responses and is influenced by genetics, behavior, and society.
- The number of people considered overweight and obese in the world has now surpassed the number that is starving.
- There are many health consequences of being overweight or obese. As BMIs increase over 25 kg/m2 the risks increase for heart disease, type 2 diabetes, hypertension, endometrial cancer, breast cancer, colon cancer, stroke, osteoarthritis, liver disease, gallbladder disorders, and more.
- Disordered eating patterns can lead to clinical eating disorders that have serious health consequences. While only three eating disorders have been identified by the DSM-5 (anorexia, bulimia, and binge eating disorder), early treatment involving several health professionals is important for any type of disordered eating pattern.
- Weight loss recommendations include a slow and steady approach comprised of a sustainable change in eating habits as well as increased physical activity. A loss of 0.5-2 lbs per week is recommended, and health benefits can be seen with a loss of 5-10% of body weight.
- There are three weight loss surgeries commonly performed in the US: gastric banding, sleeve gastrectomy, and gastric bypass.
Portions of this chapter were taken from OER Sources listed below:
Tharalson, J. (2019). Nutri300:Nutrition. https://med.libretexts.org/Courses/Sacremento_City_College/SSC%3A_Nutri_300_(Tharalson)
Zimmerman, M., & Snow, B. (2012). An Introduction to Nutrition, v. 1.0. https://2012books.lardbucket.org/books/an-introduction-to-nutrition/
Additional References:
- World Health Organization. (2020, April 1). Obesity and overweight. https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight
- Hales, C. M., Carroll, M. D., Fryar, C. D., & Ogden, C. L. (2020). Prevalence of obesity and severe obesity among adults: United States, 2017-2018. National Center for Health Statistics. Data brief, no 360. https://www.cdc.gov/nchs/data/databriefs/db360-h.pdf
- Hales, C. M., Carroll, M. D., Fryar, C. D., & Ogden, C. L. (2017). Prevalence of obesity among adults and youth: 2015-2016. National Center for Health Statistics. Data brief, no 288. https://www.cdc.gov/nchs/products/databriefs/db288.htm
- Finkelstein, E. A., Trogden, J. G., Cohen, J. W., & Dietz, W. (2009). Annual medical spending attributable to obesity: Payer- and service-specific estimates. Health Affairs Journal, 28(5), w822-831. https://doi.org/10.1377/hlthaff.28.5.w822
- Centers for Disease Control and Prevention. (2020 June 30). About adult BMI. https://www.cdc.gov/healthyweight/assessing/bmi/adult_bmi/index.html
- National Heart, Lung, Blood Institute. (n.d.). BMI tools. National Institutes of Health. https://www.nhlbi.nih.gov/health/educational/lose_wt/bmitools.htm
- Harvard Health Publishing. (2017, January 20). Abdominal obesity and your health. Harvard Medical School. https://www.health.harvard.edu/staying-healthy/abdominal-obesity-and-your-health
- Yusuf, S., Hawken, S., Ounpuu, S., Bautista, L., Franzosi, M. G., Commerford, P., Lang, C. C., Rumboldt, Z., Onen, C. L., Lisheng, L., Tanomsup, S., Wangai, P., Jr., Razak, F., Sharma, A. M., & Anand, S. S. (2005). Obesity and the risk of myocardial infarction in 27,000 participants from 52 countries: A case-control study. Lancet 366(9497), 1640-1649. https://doi:10.1016/S0140-6736(05)67663-5
- Levine, J. A. (2002). Non-exercise activity thermogenesis (NEAT). Best practice & Research: Clinical endocrinology & metabolism, 16(4), 679-702. https://doi.org/10.1053/beem.2002.0227
- Villablanca, P. A., Alegria, J. R., Mookadam, F., Holmes, D. R., Jr, Wright, R. S., & Levine, J. A. (2015). Nonexercise activity thermogenesis in obesity management. Mayo Clinic proceedings, 90(4), 509-519. https://doi.org/10.1016/j.mayocp.2015.02.001
- Saeidifard, F., Medina-Inojosa, J. R., Supervia, M., Olson, T. P., Somers, V. K., Erwin, P. J., & Lopez-Jimenez, F. (2018). Differences of energy expenditure while sitting versus standing: A systematic review and meta-analysis. European journal of Preventive Cardiology, 25(5), 522-538. https://doi.org/10.1177/2047487317752186
- Dardeno, T. A., Chou, S. H., Moon, H-S, Chamberland, J. P., Fiorenza, C. G., & Mantzoros, C. S. (2010). Leptin in human physiology and therapeutics. Frontiers in Neuroendocrinology, 31(3), 377-93. https://dx.doi.org/10.1016%2Fj.yfrne.2010.06.002
- Higgs, S., & Thomas, J. (2016). Social influences on eating behavior. Current Opinions in Behavioral Sciences, 9, 1-6. https://doi.org/10.1016/j.cobeha.2015.10.005
- Centers for Disease Control and Prevention. (2015, August 18). How to avoid portion size pitfalls. https://www.cdc.gov/healthyweight/healthy_eating/portion_size.html
- Smith, S. L., Quandt, S. A., Arcury, T. A., Wetmore, L. K., Bell, R. A., & Vitolins, M. Z. (2006). Aging and eating in the rural, southern United States: Beliefs about salt and its effect on health. Social Science & Medicine, 62(1), 189-198. https://doi.org/10.1016/j.socscimed.2005.05.009
- Saksena, M. J., Okrent, A. M., Anekwe, T. D., Cho, C., Dicken, C., Effland, A., Elitzak, H., Guthrie, J., Hamrick, K. S., Hyman, J., Jo, Y., Lin, B-H., Mancino, L., McLaughlin, P. W., Rahkovsky, I., Ralston, K., Smith, T. A., Stewart, H., …Tuttle, C. (2018). America’s eating habits: Food away from home. USDA Economic Research Service. EIB-196. https://www.ers.usda.gov/webdocs/publications/90228/eib-196.pdf
- Jiao, J., Moudon, A. V., Kim, S. Y., Hurvitz, P. M., & Drewnowski, A. (2015). Health implications of adults’ eating at and living near fast food or quick service restaurants. Nutrition and Diabetes, 5(7), e171. https://dx.doi.org/10.1038%2Fnutd.2015.18
- Müller, M. J., Geisler, C., Heymsfield, S. B., & Bosy-Westphal, A. (2018). Recent advances in understanding body weight homeostasis in humans. F1000Research, 7(F1000 Faculty Rev), 1025. https://doi.org/10.12688/f1000research.14151.1
- Matthews, C. E. (2008). Amount of time spent in sedentary behaviors in the United States, 2003-2004. American Journal of Epidemiology, 167(7), 875-81. https://doi:10.1093/aje/kwm390
- Williams, C. B., Mackenzie, K. C., & Gahagan, S. (2014). The effect of maternal obesity on the offspring. Clinical Obstetrics and Gynecology, 57(3), 508-515. https://doi.org/10.1097/GRF.0000000000000043
- Centers for Disease Control and Prevention. (2015, May 15). Physical activity for a healthy weight. https://www.cdc.gov/healthyweight/physical_activity/index.html
- Duvivier, B. M., Schaper, N. C., Bremers, M. A., van Crombrugge, G., Menheere, P. P., Kars, M., & Savelberg, H. H. (2013). Minimal intensity physical activity (standing and walking) of longer duration improves insulin action and plasma lipids more than shorter periods of moderate to vigorous exercise (cycling) in sedentary subjects when energy expenditure is comparable. PloS One, 8(2), e55542. https://doi.org/10.1371/journal.pone.0055542
- Arroyo-Johnson, C., & Mincey, K. D. (2016). Obesity epidemiology worldwide. Gastroenterology Clinics of North America, 45(4), 571-579. https://doi.org/10.1016/j.gtc.2016.07.012
- Centers for Disease and Prevention. (2020, June 11). Adult obesity causes & consequences. https://www.cdc.gov/obesity/adult/causes.html
- Heron, M. (2019, June 24). Deaths: Leading causes for 2017. National Vital Statistics Reports, 68(6). National Center for Health Statistics. https://www.cdc.gov/nchs/data/nvsr/nvsr68/nvsr68_06-508.pdf
- Tanofsky-Kraft, M., Sbarocco, T., Theim, K. R., Cohen, L. A., Mackey, E. R., Stice, E., Henderson, J. L., McCreight, S. J., Bryant, E. J., & Stephens, M. B. (2013). Obesity and the U.S. military family. Obesity, 21(11), 2205-2220. https://dx.doi.org/10.1002%2Foby.20566
- The National Institute of Mental Health. (2016). Eating disorders. https://www.nimh.nih.gov/health/topics/eating-disorders/index.shtml
- Fryer, C. D., Carroll, M. D, & Ogden, C. L. (2018, September 25). Prevalence of underweight among adults aged 20 and over: United States, 1960-62 through 2015-16. National Center for Health Statistics. https://www.cdc.gov/nchs/data/hestat/underweight_adult_15_16/underweight_adult_15_16.htm
- Fryer, C. D., Carroll, M. D., & Ogden, C. L. (2018, September). Prevalence of underweight among children and adolescents aged 2-19 and over: United States, 1963-65 through 2015-16. National Center for Health Statistics. https://www.cdc.gov/nchs/data/hestat/underweight_child_15_16/underweight_child_15_16.htm
- Anderson, M. (2018). What is disordered eating? Academy of Nutrition and Dietetics. https://www.eatright.org/health/diseases-and-conditions/eating-disorders/what-is-disordered-eating)
- National Eating Disorders Association. (n.d.). What are eating disorders? https://www.nationaleatingdisorders.org/what-are-eating-disorders
- Smink, F. E., van Hoeken, D., & Hoek, H. W. (2012). Epidemiology of eating disorders: Incidence, prevalence and mortality rates. Current Psychiatry Reports, 14(4), 406-414. https://doi: 10.1007/s11920-012-0282-y
- Advani, S., Kochhar, G., Chachra, S., & Dhawan, P. (2014). Eating everything except food (PICA): A rare case report and review. Journal of International Society of Preventive & Community Dentistry, 4(1), 1–4. https://doi.org/10.4103/2231-0762.127851
- Wing, R. R., & Hill, J. O. (2001). Successful weight loss maintenance. Annual Review of Nutrition, 21, 323–341. https://doi.org/10.1146/annurev.nutr.21.1.323
- Anderson, J. W., Konz, E. C., Frederich, R, C., Wood, C. L. (2001). Long-term weight-loss maintenance: A meta-analysis of US studies. American Journal of Clinical Nutrition, 74(5), 579–584. doi:10.1093/ajcn/74.5.579
- Hall, K.D., & Kahan, S. (2018). Maintenance of lost weight and long-term management of obesity. Medical Clinics of North America, 102(1), 183-197. https://doi.org/10.1016/j.mcna.2017.08.012
- Polidori, D., Sanghvi, A., Seeley, R. J., & Hall, K. D. (2016). How strongly does appetite counter weight loss? Quantification of the feedback control of human energy intake. Obesity (Silver Spring), 24(11), 2289-2295. doi:10.1002/oby.21653
- The National Weight Control Registry. (n.d.). NWCR Facts. http://www.nwcr.ws/Research/default.htm
- National Heart, Lung, and Blood Institute Obesity Education Initiative Expert Panel on the Identification, Evaluation, and Treatment of Obesity in Adults (US). (1998). Clinical guidelines on the identification, evaluation, and treatment of overweight and obesity in adults: The evidence report. National Heart, Lung, and Blood Institute. http://www.ncbi.nlm.nih.gov/books/NBK200
- Centers for Disease Control and Prevention. (2020, February 4). Losing weight: Healthy weight. https://www.cdc.gov/healthyweight/losing_weight/index.html
- Centers for Disease Control and Prevention. (2015, December 10). Losing weight: Getting started. https://www.cdc.gov/healthyweight/losing_weight/getting_started.html)
- United States Department of Agriculture and United States Department of Health and Human Services. (2020). Dietary Guidelines for Americans, 2020-2025. (9th ed.). https://www.dietaryguidelines.gov
- Centers for Disease Control and Prevention. (2019, December 3). Improving your eating habits. https://www.cdc.gov/healthyweight/losing_weight/eating_habits.html
- National Institute of Diabetes and Digestive and Kidney Diseases. (n.d.). Bariatric surgery. National Institutes of Health. https://www.niddk.nih.gov/health-information/weight-management/bariatric-surgery
- American Society for Metabolic and Bariatric Surgery. (n.d.). Bariatric surgery procedures. https://asmbs.org/patients/bariatric-surgery-procedures
Media Attributions
- E61EA123-A8CB-4FC4-8E79-F0479D5C7FEC
- 0BD01950-A59A-4FDD-903C-729D93D447ED
- FF0F1139-FE56-4562-A155-C7EA5DE28C13
- E55347E6-FC35-4498-A027-438A834A0626
- 45ABDE68-CBE4-4102-8F57-1B0599AFBDD9
- 10592007-5A74-43CF-8E25-EAEF21651D87
body fat
increase in cell number
increase in the size of a cell or tissue such as fat cells or muscle
A reduction or shrinking of the size of a cell or tissue.
Defined by CDC as an environment that promotes increased food intake of non-healthful foods, and physical inactivity.
Having more weight than is typical for a particular height.
Condition of having excess body fat.
An index of an individual's weight to their height. A crude tool used to indicate an estimate of over/under weight and obesity, especially in large populations.
the amount of fat tissue versus the amount of lean tissue in a body, idetified as % fat
The amount of body fat a person requires to function. In males it is generally considered to be 2-5%, in females 10-12%
The amount of body fat beyond that which is required for essential body functioning. This fat provides energy for movement and other body processes.
body fat found under the skin
body fat centrally located around abdominal organs
Formation of glucose from non-carbohydrate sources such as lipids and fats
The process that forms triglycerides from glycerol and fatty acids.
energy intake is greater than energy required
energy intake is less than energy required
energy intake equals energy required
Total number of kcals a person expends daily. It is made up of BMR, energy spent on physical activity, TEF, and NEAT.
The amount of energy required by the body to conduct basic functions. For most people it is 50-70% of the total calories they require each day.
any bodily movement produced by the contraction of skeletal muscle that increases energy expenditure above a basal level
The energy it takes to digest, absorb, transport, and store nutrients from a meal.
Total of all of the chemical reactions that take place in the body, both anabolic (building) and catabolic (breaking).
Energy expended for everything a person does throughout the day that is not sleeping, eating, or sports-like activities. It consists of activities of daily living and varies greatly from person to person and day to day.
physical feeling of emptiness accompanied by other symptoms caused by lack calorie intake
the sensation of being full
hunger hormone secreted from the stomach when it is empty
stomach stretching
hormone released by fat cells; signals to the hypothalamus that eating is not required, often called the satiety hormone; helps regulate long term food intake
study of the relationships among genes, diet, and health outcomes
the psychological desire for food
Lack of physical activity or activities where energy expenditure is no more than 1.5 times the amount of energy expended while at rest. This includes sitting, reclining, or lying down while awake.
A disturbed and unhealthy eating pattern that may or may not meet the diagnostic criteria for an eating disorder.
