6 The Brain
Learning Objectives
- Explain the processes and function of synaptic blooming and synaptic pruning
- Describe the functions that lateralization allows
- Explain the concept of neural plasticity and its implications for the lifespan
- Identify three major brain developments in adolescence
- Explain the asynchrony in two of the brain developments and how it is responsible for certain adolescent behaviors
- Describe abnormal memory loss due to Alzheimer’s disease and dementia
- Describe sleep concerns for infants
- Explain why sleep is important for adolescents
Think back to your earliest memories of school. What types of information did you learn? How did you think about your experience of going to school? What did you think about your life? Compare these memories to how you think now. What types of information are you learning in higher education? How do you think about your life and experience of going to college now? The way we think changes across the lifespan and are fueled by the maturation of our brains. In this chapter, we’ll examine notable biological changes to the brain in infancy and later adulthood. We will discuss the cognitive process of the brain in later chapters. Finally, in this chapter, we will also discuss how sleep changes from infancy to adolescence, and how sleep is important for overall health.
6.1 The Brain in the First Two Years
Some of the most dramatic physical change that occurs during this period is in the brain. At birth, the brain is about 25 percent of its adult weight, and this is not true for any other part of the body. By age 2, it is at 75 percent of its adult weight, at 95 percent by age 6, and 100 percent by age 7 years.

We are born with most of the brain cells that we will ever have; that is, about 85 billion neurons whose function is to store and transmit information (Huttenlocher & Dabholkar, 1997). A neuron a specialized nerve cell, is the body’s messenger and consists of three major parts:
- Cell body (soma): manages the messaging and keeps neuron functioning
- Axon: carries the message away from the cell body, contains terminal buttons at the end to help release the message, and is covered with a fatty white substance called myelin that helps transmit messages faster and more efficiently
- Dendrites: receives the message and transmits it to the cell body (
Review this image of a neuron to identify the major parts:
Most of the brain’s neurons are present at birth, they are not fully mature. During the next several years dendrites, or branching extensions that collect information from other neurons will undergo a period of transient exuberance or temporary dramatic growth (exuberant because it is so rapid and transient because some of it is temporary). Because of this proliferation of dendrites, by age two a single neuron might have thousands of dendrites. Synaptogenesis, or the formation of connections between neurons, continues from the prenatal period forming thousands of new connections during infancy and toddlerhood. This period of rapid neural growth is referred to as synaptic blooming.
The blooming period of neural growth is then followed by a period of synaptic pruning, where neural connections are reduced thereby making those that are used much stronger. It is thought that pruning causes the brain to function more efficiently, allowing for the mastery of more complex skills (Kolb & Whishaw, 2011). Experience will shape which of these connections are maintained and which of these are lost. Ultimately, about 40 percent of these connections will be lost (Webb et al., 2001). Blooming occurs during the first few years of life, and pruning continues through childhood and into adolescence in various areas of the brain.
Another major change occurring in the central nervous system is the development of myelin, a coating of fatty tissues around the axon of the neuron (Carlson, 2014). Myelin helps insulate the nerve cell and speed the rate of transmission of impulses from one cell to another. This enhances the building of neural pathways and improves coordination and control of movement and thought processes. The development of myelin continues into adolescence but is most dramatic during the first several years of life.
The infant’s brain grows very fast. At birth, the brain is about 250 grams (half a pound) and by one year it is already 750 grams (Eliot, 1999). Compared to adult size, the newborn brain is approximately 33% of adult size at birth, and in just 90 days, it is already at 55% of adult size (Holland et al., 2014). Most of the neural activity occurs in the cortex or the thin outer covering of the brain involved in voluntary activity and thinking. The cortex is divided into two hemispheres, and each hemisphere is divided into four lobes, each separated by folds known as fissures.
If we look at the cortex starting at the front of the brain and moving over the top, we see first the frontal lobe (behind the forehead), which is responsible primarily for thinking, planning, memory, and judgment. Following the frontal lobe is the parietal lobe, which extends from the middle to the back of the skull and is responsible primarily for processing information about touch. Next is the occipital lobe, at the very back of the skull, which processes visual information. Finally, in front of the occipital lobe, between the ears, is the temporal lobe, which is responsible for hearing and language (Jarrett, 2015).
Although the brain grows rapidly during infancy, specific brain regions do not mature at the same rate. Primary motor areas develop earlier than primary sensory areas, and the prefrontal cortex, which is located behind the forehead, is the least developed (Giedd, 2015). As the prefrontal cortex matures, the child is increasingly able to regulate or control emotions, plan activities, strategize, and have better judgment. This is not fully accomplished in infancy and toddlerhood but continues throughout childhood, adolescence, and into adulthood.
Lateralization is the process in which different functions become localized primarily on one side of the brain. For example, in most adults, the left hemisphere is more active than the right during language production, while the reverse pattern is observed during tasks involving visuospatial abilities (Springer & Deutsch, 1993). This process develops over time, however, structural asymmetries between the hemispheres have been reported even in fetuses (Chi et al., 1997; Kasprian et al., 2011) and infants (Dubois et al., 2009).
Lastly, neuroplasticity refers to the brain’s ability to change, both physically and chemically, to enhance its adaptability to environmental change and compensate for injury. The control of some specific bodily functions, such as movement, vision, and hearing, is performed in specified areas of the cortex, and if these areas are damaged, the individual will likely lose the ability to perform the corresponding function. The brain’s neurons have a remarkable capacity to reorganize and extend themselves to carry out these particular functions in response to the needs of the organism, and to repair any damage. As a result, the brain constantly creates new neural communication routes and rewires existing ones. Both environmental experiences, such as stimulation and events within a person’s body, such as hormones and genes, affect the brain’s plasticity. So too does age. Adult brains demonstrate neuroplasticity, but they are influenced less extensively than those of infants (Kolb & Fantie, 1989; Kolb & Whishaw, 2011).
6.2 The Adolescent Brain
The brain undergoes dramatic changes during adolescence. Although it does not get larger, it matures by becoming more interconnected and specialized (Giedd, 2015). The myelination and development of connections between neurons continue. This results in an increase in the white matter of the brain that allows the adolescent to make significant improvements in their thinking and processing skills. Different brain areas become myelinated at different times. For example, the brain’s language areas undergo myelination during the first 13 years. Completed insulation of the axons consolidates these language skills but makes it more difficult to learn a second language. With greater myelination, however, comes diminished plasticity as a myelin coating inhibits the growth of new connections (Dobbs, 2012).
Even as the connections between neurons are strengthened, synaptic pruning occurs more than during childhood as the brain adapts to changes in the environment. This synaptic pruning causes the gray matter of the brain, or the cortex, to become thinner but more efficient (Dobbs, 2012). The corpus callosum, which connects the two hemispheres of the brain, continues to thicken allowing for stronger connections between brain areas. Additionally, the hippocampus becomes more strongly connected to the frontal lobes, allowing for greater integration of memory and experiences into our decision-making.
The limbic system, which regulates emotion and reward, is linked to the hormonal changes that occur at puberty. The limbic system is also related to novelty seeking and a shift toward interacting with peers. In contrast, the prefrontal cortex, which is involved in the control of impulses, organization, planning, and making good decisions, does not fully develop until the mid-20s. According to Giedd (2015), an important outcome of the early development of the limbic system combined with the later development of the prefrontal cortex is the “mismatch” in timing between the two. The approximately ten years that separate the development of these two brain areas can result in increases in risky behavior, poor decision-making, and weak emotional control for the adolescent. When puberty begins earlier, this mismatch lasts even longer.
Teens typically take more risks than adults and according to research, it is because they weigh risks and rewards differently than adults do (Dobbs, 2012). The brain’s sensitivity to the neurotransmitter dopamine peaks during adolescence, and dopamine is involved in reward circuits, so adolescents may judge that the possible rewards outweigh the risks. Adolescents respond especially strongly to social rewards during activities, and they prefer the company of others their same age. Chein et al. (2011) found that peers sensitize brain regions associated with potential rewards. For example, adolescent drivers make more risky driving decisions when with friends to impress them, and teens are much more likely to commit crimes together in comparison to adults (30 and older) who commit them alone (Steinberg et al., 2018). In addition to dopamine, the adolescent brain is affected by oxytocin which facilitates bonding and makes social connections more rewarding. With both dopamine and oxytocin engaged, it is no wonder that adolescents seek peers and excitement in their lives that could end up endangering them.
Because of all the changes that occur in the brain during adolescence, the chances for abnormal development, including the emergence of mental illness, also rise. 50% of all mental illnesses occur by the age of 14 and 75% occur by age 24 (Giedd, 2015). Additionally, during this period of development, the adolescent brain is especially vulnerable to damage from drug exposure. For example, repeated exposure to marijuana can affect cellular activity in the endocannabinoid system. Consequently, adolescents are more sensitive to the effects of repeated marijuana exposure (Weir, 2015).
However, researchers have also focused on the highly adaptive qualities of the adolescent brain which allow the adolescent to move away from the family towards the outside world (Dobbs, 2012; Giedd, 2015). Novelty-seeking and risk-taking can generate positive outcomes including meeting new people, trying new activities, and seeking out new situations. Separating from the family and moving into new relationships and different experiences are quite adaptive – for adolescents and society.
In sum, the adolescent years are a time of intense brain changes. Interestingly, two of the primary brain functions develop at different rates. Brain research indicates that the part of the brain that perceives rewards from risk, the limbic system, kicks into high gear in early adolescence. The part of the brain that controls impulses and engages in longer-term perspective, the frontal lobes, matures later. This may explain why teens in mid-adolescence take more risks than older teens. As the frontal lobes become more developed, two things happen. First, self-control develops as teens are better able to assess cause and effect. Second, more areas of the brain become involved in processing emotions, and teens become better at accurately interpreting others’ emotions.[1]
Link to Learning – 6 Unique Facts
As you learn about brain development during adolescence, consider these six facts from The National Institute of Mental Health:
1. Your brain does not keep getting bigger as you get older
For girls, the brain reaches its largest physical size at around 11 years old, and for boys, the brain reaches its largest physical size around age 14. Of course, this difference in age does not mean either boys or girls are smarter than one another!
2. But that doesn’t mean your brain is done maturing
For both boys and girls, although your brain may be as large as it will ever be, your brain doesn’t finish developing and maturing until your mid-to late-20s. The front part of the brain called the prefrontal cortex, is one of the last brain regions to mature. It is the area responsible for planning, prioritizing, and controlling impulses.
3. The teen brain is ready to learn and adapt
In a digital world that is constantly changing, the adolescent brain is well prepared to adapt to new technology—and is shaped in return by experience.
4. Many mental disorders appear during adolescence
All the big changes the brain is experiencing may explain why adolescence is the time when many mental disorders—such as schizophrenia, anxiety, depression, bipolar disorder, and eating disorders—emerge.
5. The teen brain is resilient
Although adolescence is a vulnerable time for the brain and for teenagers in general, most teens go on to become healthy adults. Some changes in the brain during this important phase of development may help protect against long-term mental disorders.
6. Teens need more sleep than children and adults
Although it may seem like teens are lazy, science shows that melatonin levels (or the “sleep hormone” levels) in the blood naturally rise later at night and fall later in the morning than in most children and adults. Many teens are unable to fall asleep until 11:00 p.m. This may explain why many teens stay up late and struggle with getting up in the morning. Teens should get about 9-10 hours of sleep a night, but most teens don’t get enough sleep. A lack of sleep makes paying attention hard, increases impulsivity, and may also increase irritability and depression.
6.3 Adulthood and the Aging Brain
Research has demonstrated that the brain loses 5% to 10% of its weight between 20 and 90 years of age (Fjell & Walhovd, 2010). This decrease in brain volume appears to be due to the shrinkage of neurons, decreases in the number of synapses, and increasingly shorter axon lengths. According to Garrett (2015), normal declines in cognitive ability throughout the lifespan are associated with brain changes, including reduced activity of genes involved in memory storage, synaptic pruning, plasticity, and glutamate and GABA (neurotransmitters) receptors.
There is also a loss in white matter connections between brain areas. Without myelin, neurons demonstrate slower conduction and impede each other’s actions. A loss of synapses occurs in specific brain areas, including the hippocampus (involved in memory) and the basal forebrain region. Older individuals also activate larger regions of their attentional and executive networks, located in the parietal and prefrontal cortex, when they perform complex tasks. This increased activation coincides with reduced performance on both executive tasks and tests of working memory when compared to that of younger people (Kolb & Whishaw, 2011).
Continued Neurogenesis
Researchers at the University of Chicago found that new neurons continue to form in old age. Tobin et al. (2019) examined the post-mortem brain tissue of individuals between the ages of 79 and 99 (average age 90.6) and found evidence of neurogenesis in the hippocampus. Approximately 2000 neural progenitor cells and 150, 000 developing neurons were found per brain, although the number of developing neurons was lower in people with cognitive impairments or Alzheimer’s disease. Tobin et al. (2019) hypothesized that the lower levels of neurogenesis in the hippocampus were associated with symptoms of cognitive decline and reduced synaptic plasticity.
The brain in late adulthood also exhibits considerable plasticity, and through practice and training, the brain can be modified to compensate for any age-related changes (Erber & Szuchman, 2015). Park and Reuter-Lorenz (2009) proposed the Scaffolding Theory of Aging and Cognition which states that the brain adapts to neural atrophy (dying of brain cells) by building alternative connections, referred to as scaffolding. This scaffolding allows older brains to retain high levels of performance. Brain compensation is especially noted in the additional neural effort demonstrated by those individuals who are aging well. For example, older adults who performed just as well as younger adults on a memory task used both prefrontal areas, while only the right prefrontal cortex was used in younger participants (Cabeza et al., 2002). Consequently, this decrease in brain lateralization appears to assist older adults with their cognitive skills.
6.4 Neurocognitive Disorders
As the brain ages, several common disorders can result from changes in brain functioning that impact cognition and personality.
Dementia
Dementia is the umbrella category used to describe the general long-term and often gradual decrease in the ability to think and remember that affects a person’s daily functioning. The manual used to help classify and diagnose mental disorders, the Diagnostic and Statistical Manual of Mental Disorders, or DSM-5, classifies dementia as a “major neurocognitive disorder,” with milder symptoms classified as “mild cognitive impairment.” However, the term dementia is still in common use. Dementia generally refers to severely impaired judgment, memory, or problem-solving ability. It can occur before old age and is not an inevitable development even among the very old. Common symptoms of dementia include emotional problems, difficulties with language, and a decrease in motivation. A person’s consciousness is usually not affected. Globally, dementia affected about 46 million people in 2015. About 10% of people develop the disorder at some point in their lives, and it becomes more common with age. About 3% of people between the ages of 65–74 have dementia, 19% between 75 and 84, and nearly half of those over 85 years of age. In 2015, dementia resulted in about 1.9 million deaths, up from 0.8 million in 1990. As more people are living longer, dementia is becoming more common in the population as a whole.
Dementia can be caused by numerous diseases and circumstances, all of which result in similar general symptoms of impaired judgment, etc. Alzheimer’s disease is the most common form of dementia and is incurable, but there are also nonorganic causes of dementia that can be prevented. Malnutrition, alcoholism, depression, and mixing medications can also result in symptoms of dementia. If these causes are properly identified, they can be treated. Cerebral vascular disease can also reduce cognitive functioning.
Alzheimer’s Disease
Alzheimer’s disease (AD), also referred to simply as Alzheimer’s, is the most common cause of dementia, accounting for 60-70% of its cases. Alzheimer’s disease has a gradual onset with subtle personality changes and memory loss that differs from normal age-related memory problems occurring first. Confusion, difficulty with change, and deterioration in language, problem-solving skills, and personality become evident next. In the later stages, the individual loses physical coordination and is unable to complete everyday tasks, including self-care and personal hygiene (Erber & Szuchman, 2015).
Lastly, individuals lose the ability to respond to their environment, to carry on a conversation, and eventually to control movement (Alzheimer’s Association, 2016). On average people with Alzheimer’s survive eight years, but some may live up to 20 years. The disease course often depends on the individual’s age and whether they have other health conditions.
The greatest risk factor for Alzheimer’s disease is age, but there are genetic and environmental factors that can also contribute. Some forms of Alzheimer’s are hereditary, and with the early onset type, several rare genes have been identified that directly cause Alzheimer’s. People who inherit these genes tend to develop symptoms in their 30s, 40s and 50s. Five percent of those identified with Alzheimer’s disease are younger than age 65. When Alzheimer’s disease is caused by deterministic genes, it is called familial Alzheimer’s disease (Alzheimer’s Association, 2016). Traumatic brain injury is also a risk factor, as well as obesity, hypertension, high cholesterol, and diabetes (Carlson, 2011).
In 2016 an estimated 5.4 million Americans were diagnosed with Alzheimer’s disease (Alzheimer’s Association, 2016), which was approximately one in nine aged 65 and over. By 2050 the number of people aged 65 and older with Alzheimer’s disease is projected to be 13.8 million if there are no medical breakthroughs to prevent or cure the disease. Alzheimer’s is the sixth leading cause of death in the United States.
Alzheimer’s is not a normal part of aging. The greatest known risk factor is increasing age, and the majority of people with Alzheimer’s are 65 and older. But Alzheimer’s is not just a disease of old age. Approximately 200,000 Americans under the age of 65 have younger-onset Alzheimer’s disease (also known as early-onset Alzheimer’s).[3]
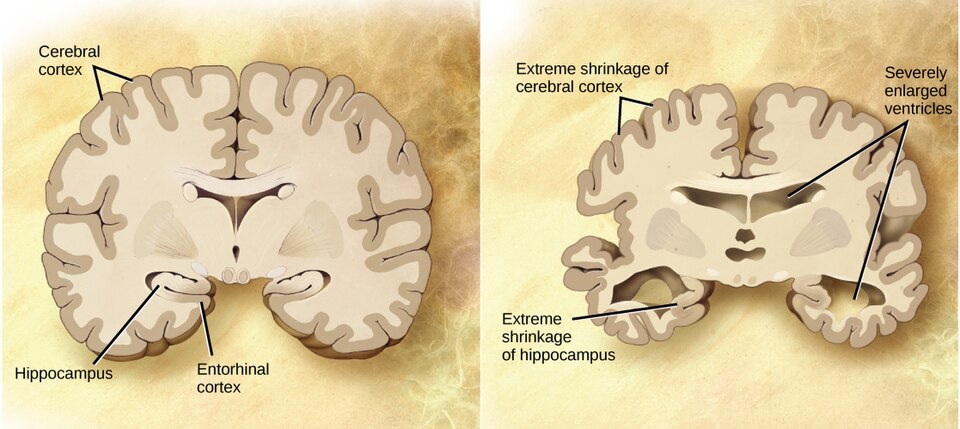
The cause of Alzheimer’s disease is poorly understood. About 70% of the risk is believed to be inherited from a person’s parents with many genes usually involved. Other risk factors include a history of head injuries, depression, and hypertension. The disease process is associated with plaques and neurofibrillary tangles in the brain. A probable diagnosis is based on the history of the illness and cognitive testing with medical imaging and blood tests to rule out other possible causes. Initial symptoms are often mistaken for normal aging, but examination of brain tissue, specifically of structures called plaques and tangles, is needed for a definite diagnosis. Though qualified physicians can be up to 90% certain of a correct diagnosis of Alzheimer’s, currently, the only way to make a 100% definitive diagnosis is by performing an autopsy of the person and examining the brain tissue. In 2015, there were approximately 29.8 million people worldwide with AD. In developed countries, AD is one of the most financially costly diseases.
Healthy Brain Functioning
In longitudinal studies, Cheng (2016) found that both physical activity and stimulating cognitive activity resulted in significant reductions in the risk of neurocognitive disorders. Physical activity, especially aerobic exercise, is associated with less age-related gray and white matter loss, as well and diminished neurotoxins in the brain.
Overall, physical activity preserves the integrity of neurons and brain volume. Cognitive training improves the efficiency of the prefrontal cortex and executive functions, such as working memory, and strengthens the plasticity of neural circuits. Both activities support cognitive reserve, or “the structural and dynamic capacities of the brain that buffer against atrophies and lesions” (Cheng, 2016, p. 85). Although it is optimal to begin physical and cognitive activities earlier in life, it is never too late to start these programs to improve one’s cognitive health, even in late adulthood.
Can we improve brain functioning?
Many training programs have been created to improve brain functioning. ACTIVE (Advanced Cognitive Training for Independent and Vital Elderly), a study conducted between 1999 and 2001 in which 2,802 individuals aged 65 to 94, suggests that the answer is “yes”. These racially diverse participants received 10 group training sessions and 4 follow-up sessions to work on tasks of memory, reasoning, and speed of processing. These mental workouts improved cognitive functioning even 5 years later. Many of the participants believed that this improvement could be seen in everyday tasks as well (Tennstedt et al., 2006).
However, programs for the elderly on memory, reading, and processing speed training demonstrate that there is improvement in the specific tasks trained, but there is no generalization to other abilities (Jarrett, 2015). Further, these programs have not been shown to delay or slow the progression of Alzheimer’s disease. Although these programs are not harmful, “physical exercise, learning new skills, and socializing remain the most effective ways to train your brain” (p. 207). These activities appear to build a reserve to minimize the effects of primary aging of the brain.
6.5 The Importance of Sleep for the Brain & Body
Infants 0 to 2 years of age sleep an average of 12.8 hours a day, although this changes and develops gradually throughout an infant’s life. For the first three months, newborns sleep between 14 and 17 hours a day, then they become increasingly alert for longer periods of time. About one-half of an infant’s sleep is rapid eye movement (REM) sleep, and infants often begin their sleep cycle with REM rather than non-REM sleep. They also move through the sleep cycle more quickly than adults.
Parents spend a significant amount of time worrying about and losing even more sleep over their infant’s sleep schedule, but there remains a great deal of variation in sleep patterns and habits for individual children. A 2018 study showed that at 6 months of age, 62% of infants slept at least six hours during the night, 43% of infants slept at least 8 hours through the night, and 38% of infants were not sleeping at least six continual hours through the night. At 12 months, 28% of children were still not sleeping at least 6 uninterrupted hours through the night, while 78% were sleeping at least 6 hours, and 56% were sleeping at least 8 hours.[1]
The most common infant sleep-related problem reported by parents is nighttime waking. Studies of new parents and sleep patterns show that parents lose the most sleep during the first three months with a new baby, with mothers losing about an hour of sleep each night, and fathers losing a disproportionate 13 minutes. This decline in sleep quality and quantity for adults persists until the child is about six years old. [2]
While this shows there is no precise science as to when and how an infant will sleep, there are general trends in sleep patterns. Around six months, babies typically sleep between 14-15 hours a day, with 3-4 of those hours happening during daytime naps. As they get older, these naps decrease from several to typically two naps a day between ages 9-18 months. Often, periods of rapid weight gain or changes in developmental abilities such as crawling or walking will cause changes to sleep habits as well. Infants generally move towards one 2-4 hour nap a day by around 18 months, and many children will continue to nap until around four or five years old.[3]
Sudden Unexpected Infant Deaths (SUID)
Each year in the United States, there are about 3,500 Sudden Unexpected Infant Deaths (SUID). These deaths occur among infants less than one-year-old and have no immediately obvious cause (Moon et al. 2016). The three commonly reported types of SUID are:
1) Sudden Infant Death Syndrome (SIDS): SIDS is identified when the death of a healthy infant occurs suddenly and unexpectedly, and medical and forensic investigation findings (including an autopsy) are inconclusive. SIDS is the leading cause of death in infants up to 12 months old, and approximately 1,500 infants died of SIDS in 2013 (Moon et al. 2016). The risk of SIDS is highest at 4 to 6 weeks of age. Because SIDS is diagnosed when no other cause of death can be determined, possible causes of SIDS are regularly researched. One leading hypothesis suggests that infants who die from SIDS have abnormalities in the area of the brainstem responsible for regulating breathing (Weekes-Shackelford & Shackelford, 2005). Although the exact cause is unknown, doctors have identified the following risk factors for SIDS:
- low birth weight
- siblings who have had SIDS
- sleep apnea
- of African-American or Inuit descent
- low socioeconomic status (SES)
- smoking in the home
2.) Unknown cause: The sudden death of an infant less than one year of age that cannot be explained because a thorough investigation was not conducted, and the cause of death could not be determined.
3.) Accidental suffocation and strangulation in bed: Reasons for accidental suffocation include the following: suffocation by soft bedding, another person rolling on top of or against the infant while sleeping, an infant being wedged between two objects such as a mattress and wall, and strangulation such as when an infant’s head and neck become caught between crib railings.
The combined SUID rate declined considerably following the release of the American Academy of Pediatrics safe sleep recommendations in 1992, which advocated that infants be placed on their backs for sleep (non-prone position). These recommendations were followed by a major Back to Sleep Campaign in 1994. According to the CDC, the SIDS death rate is now less than one-fourth of what is was (130 per 100,000 live birth in 1990 versus 40 in 2015). However, accidental suffocation and strangulation in bed mortality rates remained unchanged until the late 1990s. Some parents were still putting newborns to sleep on their stomachs partly because of past tradition. Most SIDS victims experience several risks, an interaction of biological and social circumstances. But thanks to research, the major risk, stomach sleeping, has been highly publicized. Other causes of death during infancy include congenital birth defects and homicide.
Co-Sleeping
 The location of sleep depends primarily on the baby’s age and culture. Bed-sharing (in the parents’ bed) or co-sleeping (in the parents’ room) is the norm is some cultures, but not in others (Esposito et al. 2015) [4]. Colvin et al. (2014)[5] analyzed a total of 8,207 deaths from 24 states during 2004–2012. The deaths were documented in the National Center for the Review and Prevention of Child Deaths Case Reporting System, a database of death reports from state child death review teams. The results indicated that younger victims (0-3 months) were more likely to die by bed-sharing and sleeping in an adult’s bed or on a person. A higher percentage of older victims (4 months to 364 days) rolled into objects in the sleep environment and changed position from side/back to prone. Carpenter et al. (2013)[6] compared infants who died of SIDS with a matched control and found that infants younger than three months old who slept in bed with a parent were five times more likely to die of SIDS compared to babies who slept separately from the parents, but were still in the same room. They concluded that bed-sharing, even when the parents do not smoke or take alcohol or drugs, increases the risk of SIDS. However, when combined with parental smoking and maternal alcohol consumption and/or drug use, the risks associated with bed-sharing greatly increased.
The location of sleep depends primarily on the baby’s age and culture. Bed-sharing (in the parents’ bed) or co-sleeping (in the parents’ room) is the norm is some cultures, but not in others (Esposito et al. 2015) [4]. Colvin et al. (2014)[5] analyzed a total of 8,207 deaths from 24 states during 2004–2012. The deaths were documented in the National Center for the Review and Prevention of Child Deaths Case Reporting System, a database of death reports from state child death review teams. The results indicated that younger victims (0-3 months) were more likely to die by bed-sharing and sleeping in an adult’s bed or on a person. A higher percentage of older victims (4 months to 364 days) rolled into objects in the sleep environment and changed position from side/back to prone. Carpenter et al. (2013)[6] compared infants who died of SIDS with a matched control and found that infants younger than three months old who slept in bed with a parent were five times more likely to die of SIDS compared to babies who slept separately from the parents, but were still in the same room. They concluded that bed-sharing, even when the parents do not smoke or take alcohol or drugs, increases the risk of SIDS. However, when combined with parental smoking and maternal alcohol consumption and/or drug use, the risks associated with bed-sharing greatly increased.
Despite the risks noted above, the controversy about where babies should sleep has been ongoing. Co-sleeping has been recommended for those who advocate attachment parenting (Sears & Sears, 2001) [7] and other research suggests that bed-sharing and co-sleeping is becoming more popular in the United States (Colson et al., 2013) [8]. So, what are the latest recommendations?
The American Academy of Pediatrics (AAP) updated its recommendations for a Safe Infant Sleeping Environment in 2016. The most recent AAP recommendations on creating a safe sleep environment include:
- Back to sleep for every sleep. Always place the baby on their back on a firm sleep surface such as a crib or bassinet with a tight-fitting sheet.
- Avoid the use of soft bedding, including crib bumpers, blankets, pillows, and soft toys. The crib should be bare.
- Breastfeeding is recommended.
- Share a bedroom with parents, but not the same sleeping surface, preferably until the baby turns 1 but at least for the first six months. Room-sharing decreases the risk of SIDS by as much as 50 percent.
- Avoid baby’s exposure to smoke, alcohol, and illicit drugs.
As you can see, there is a recommendation to now “share a bedroom with parents,” but not the same sleeping surface. Breastfeeding is also recommended as adding protection against SIDS, but after feeding, the AAP encourages parents to move the baby to their separate sleeping space, preferably a crib or bassinet in the parents’ bedroom. Finally, the report included new evidence that supports skin-to-skin care for newborn infants.[9]
Adolescent Sleep
According to the National Sleep Foundation (NSF; 2016), to function their best, adolescents need about 8 to 10 hours of sleep each night. The most recent Sleep in America poll in 2006 indicated that adolescents between sixth and twelfth grade were not getting the recommended amount of sleep. On average, adolescents slept only 7 ½ hours per night on school nights with younger adolescents getting more than older ones (8.4 hours for sixth graders and only 6.9 hours for those in twelfth grade). For older adolescents, only about one in ten (9%) get an optimal amount of sleep, and those who don’t are more likely to experience negative consequences the following day. These include depressed mood, feeling tired or sleepy, being cranky or irritable, falling asleep in school, and drinking caffeinated beverages (NSF, 2016). Additionally, sleep-deprived adolescents are at greater risk for substance abuse, car crashes, poor academic performance, obesity, and a weakened immune system (Weintraub, 2016).
Why don’t adolescents get adequate sleep?
In addition to known environmental and social factors, including work, homework, media, technology, and socializing the adolescent brain is also a factor. As adolescents go through puberty, their circadian rhythms change and push back their sleep time until later in the evening (Weintraub, 2016). This biological change not only keeps adolescents awake at night, it makes it difficult for them to wake up. When they are awakened too early, their brains do not function optimally. Impairments are noted in attention, academic achievement, and behavior while increases in tardiness and absenteeism are also seen.
 To support adolescents’ later circadian rhythms, the Centers for Disease Control and Prevention recommends that school begin no earlier than 8:30 a.m. Unfortunately, over 80% of American schools begin their day earlier than 8:30 a.m. with an average start time of 8:03 a.m. (Weintraub, 2016). Psychologists and other professionals have been advocating for later start times, based on research demonstrating better student outcomes for later start times. More middle and high schools have changed their start times to better reflect the sleep research. However, the logistics of changing start times and bus schedules are proving too difficult for some schools, leaving many adolescent vulnerable to the negative consequences of sleep deprivation. Troxel et al. (2019) cautions that adolescents should find a middle ground between sleeping too little during the school week and too much during the weekends. Keeping consistent sleep schedules of too little sleep will result in sleep deprivation but oversleeping on weekends can affect the natural biological sleep cycle making it harder to sleep on weekdays.
To support adolescents’ later circadian rhythms, the Centers for Disease Control and Prevention recommends that school begin no earlier than 8:30 a.m. Unfortunately, over 80% of American schools begin their day earlier than 8:30 a.m. with an average start time of 8:03 a.m. (Weintraub, 2016). Psychologists and other professionals have been advocating for later start times, based on research demonstrating better student outcomes for later start times. More middle and high schools have changed their start times to better reflect the sleep research. However, the logistics of changing start times and bus schedules are proving too difficult for some schools, leaving many adolescent vulnerable to the negative consequences of sleep deprivation. Troxel et al. (2019) cautions that adolescents should find a middle ground between sleeping too little during the school week and too much during the weekends. Keeping consistent sleep schedules of too little sleep will result in sleep deprivation but oversleeping on weekends can affect the natural biological sleep cycle making it harder to sleep on weekdays.
Sleep in Adulthood
According to the American Academy of Sleep Medicine (Kasper, 2015) adults require at least 7 hours of sleep per night to avoid the health risks associated with chronic sleep deprivation. Less than 6 hours and more than 10 hours is also not recommended for those in middle adulthood (National Sleep Foundation, 2015). Not surprisingly, many Americans do not receive the 7-9 hours of sleep recommended. In 2013, only 59% of U.S. adults met that standard, while in 1942, 84% did (Jones, 2013). This means 41% of Americans receive less than the recommended amount of nightly sleep. Additional results included that in 1993, 67% of Americans felt they were getting enough sleep, but in 2013 only 56% felt they received as much sleep as needed. Additionally, 43% of Americans in 2013 believed they would feel better with more sleep.
Negative Consequences of Insufficient Sleep
There are many consequences of too little sleep, and they include physical, cognitive, and emotional changes. Sleep deprivation suppresses immune responses that fight off infection, and can lead to obesity, memory impairment, and hypertension (Ferrie et al., 2007; Kushida, 2005). Insufficient sleep is linked to an increased risk for colon cancer, breast cancer, heart disease and type 2 diabetes (Pattison, 2015). A lack of sleep can increase stress as cortisol (a stress hormone) remains elevated which keeps the body in a state of alertness and hyperarousal which increases blood pressure. Sleep is also associated with longevity. Dew et al. (2003) found that older adults who had better sleep patterns also lived longer. During deep sleep a growth hormone is released which stimulates protein synthesis, breaks down fat that supplies energy, and stimulates cell division. Consequently, a decrease in deep sleep contributes to less growth hormone being released and subsequent physical decline seen in aging (Pattison, 2015).
Sleep disturbances can also impair glucose functioning in middle adulthood. Caucasian, African American, and Chinese non-shift-working women aged 48–58 years who were not taking insulin-related medications, participated in the Study of Women’s Health across the Nation (SWAN) Sleep Study and were subsequently examined approximately 5 years later (Taylor et al., 2016). Body mass index (BMI) and insulin resistance were measured at two time points. Results indicated that irregular sleep schedules, including highly variable bedtimes and staying up much later than usual, are associated in midlife women with insulin resistance, which is an important indicator of metabolic health, including diabetes risk. Diabetes risk increases in midlife women, and irregular sleep schedules may be an important reason because irregular bedtime schedules expose the body to varying levels of light, which is the most important timing cue for the body’s circadian clock. By disrupting circadian timing, bedtime variability may impair glucose metabolism and energy homeostasis.
Sleep in Late Adulthood
Similar to other adults, older adults (65 and older) need between 7 to 9 hours of sleep per night, but they tend to go to sleep earlier and get up earlier than those younger. This pattern is called advanced sleep phase syndrome and is based on changes in circadian rhythms (National Sleep Foundation, 2009). There are sleep problems in older adults, and insomnia is the most common problem in those 60 and older (NIA, 2016). People with insomnia have trouble falling asleep and staying asleep. There are many reasons why older people may have insomnia, including certain medications, being in pain, having a medical or psychiatric condition, and even worrying before bedtime about not being able to sleep. Using over the counter sleep aids or medication may only work when used for a short time. Consequently, sleep problems should be discussed with a health care professional.
Also, common in older adults are sleep disorders, including sleep apnea, restless legs syndrome, periodic limb movement disorder, and rapid eye movement sleep behavior disorder (NIA, 2016). Sleep apnea refers to repeated short pauses in breathing, while an individual sleeps that can lead to reduced oxygen in the blood. Snoring is a common symptom of sleep apnea, and it often worsens with age. Untreated sleep apnea can lead to impaired daytime functioning, high blood pressure, headaches, stroke, and memory loss. Restless legs syndrome feels like there is tingling, crawling, or pins and needles in one or both legs, and this feeling is worse at night. Periodic limb movement disorder causes people to jerk and kick their legs every 20 to 40 seconds during sleep. Rapid eye movement sleep behavior disorder occurs when one’s muscles can move during REM sleep and sleep is disrupted.
According to the National Sleep Foundation (2009), there are many medical conditions that affect sleep and include gastroesophageal reflux disease, diabetes mellitus, renal failure, respiratory diseases such as asthma, and immune disorders. Diseases such as Parkinson’s disease and multiple sclerosis also commonly cause problems sleeping. Lastly, Alzheimer’s disease can interfere with sleeping patterns. Individuals may wake up many times during the night, wander when up, and yell which can alter the amount of time they sleep. Both minor and major sleep problems in older adults can lead to increased risk of accidents, falls, chronic fatigue, decreased quality of life, cognitive decline, reduced immune function, and depression (Buman, 2013).
References
Alzheimer’s Association. (2016). Know the 10 signs: Early detection matters. http://www.alz.org/national/documents/tenwarnsigns.pdf
Baum, Cabeza, R., Anderson, N. D., Locantore, J. K., & McIntosh, A. R. (2002). Aging gracefully: Compensatory brain activity in high performing older adults. NeuroImage, 17, 1394-1402.
Carlson, N. (2014). Foundations of behavioral neuroscience (9th ed.). Pearson.
Chein, J., Albert, D., O’Brien, L., Uckert, K., & Steinberg, L. (2011). Peers increase adolescent risk taking by enhancing activity in the brain’s reward circuitry. Developmental Science, 14(2), F1-F10. doi: 10.1111/j.1467-7687.2010.01035.x
Cheng, S. (2016). Cognitive reserve and the prevention of dementia: The role of physical and cognitive activities. Current Psychiatry Reports, 18(9), 85.
Chi, J. G., Dooling, E. C., & Gilles, F. H. (1977). Left-right asymmetries of the temporal speech areas of the human fetus. Archives of Neurology, 34, 346–8.
Dubois, J., Hertz-Pannier, L., Cachia, A., Mangin, J. F., Le Bihan, D., & Dehaene-Lambertz, G. (2009). Structural asymmetries in the infant language and sensori-motor networks. Cerebral Cortex, 19, 414–423.
Dobbs, D. (2012). Beautiful brains. National Geographic, 220(4), 36.
Eliot, L. (1999). What’s going on in there? Bantam.
Erber, J. T., & Szuchman, L. T. (2015). Great myths of aging. John Wiley & Sons.
Fjell, A. M., & Walhovd, K. B. (2010). Structural brain changes in aging: Courses, causes, and cognitive consequences. Reviews in the Neurosciences, 21, 187-222.
Garrett, B. (2015). Brain and behavior (4th ed.) Sage.
Giedd, J. N. (2015). The amazing teen brain. Scientific American, 312(6), 32-37.
Holland, D., Chang, L., Ernst, T. M., Curran, M., Buchthal, S. D., Alicata, D., Skranes, J., Johansen, H., Hernandez, A., Yamakawa, R., Kuperman, J. M., & Dale, A. M. (2014). Structural growth trajectories and rates of change in the first 3 months of infant brain development. JAMA neurology, 71(10), 1266–1274. https://doi.org/10.1001/jamaneurol.2014.1638
Huttenlocher, P. R., & Dabholkar, A. S. (1997). Regional differences in synaptogenesis in human cerebral cortex. Journal of comparative Neurology, 387(2), 167-178.
Jarrett, C. (2015). Great myths of the brain. Wiley
Kasprian, G., Langs, G., Brugger, P. C., Bittner, M., Weber, M., Arantes, M., & Prayer, D. (2011). The prenatal origin of hemispheric asymmetry: an in utero neuroimaging study. Cerebral Cortex, 21, 1076–1083.
Kolb, B., & Fantie, B. (1989). Development of the child’s brain and behavior. In C. R. Reynolds & E.
Kolb, B. & Whishaw, I. Q. (2011). An introduction to brain and behavior (3rd ed.). Worth Publishers.
National Sleep Foundation. (2009). Aging and sleep. https://sleepfoundation.org/sleep-topics/aging-and-sleep
Park, D. C., & Reuter-Lorenz, P. (2009). The adaptive brain: Aging and neurocognitive scaffolding. Annual Review of Psychology, 60, 173-196.
Springer, S. P. & Deutsch, G. (1993). Left brain, right brain (4th ed.). W. H. Freeman.
Steinberg, L., Icenogle, G., Shulman, E.P., et al. (2018). Around the world, adolescence is a time of heightened sensation seeking and immature self-regulation. Developmental Science, 21. https://doi.org/10.1111/desc.12532
Tennstedt, S., Morris, J., Unverzagt, F., Rebok, G., Willis, S., Ball, K., & Marsiske, M. (2006). ACTIVE: Advanced Cognitive Training for Independent and Vital Elderly Clinical Trial. Clinical Trials Database and Worldwide Listings. http://www.clinicaltrialssearch.org/active-advancedcognitive-training-for-independent-and-vital-elderlynct00298558.html
Tobin, M., K., Musaraca, K., Disouky, A., Shetti, A., Bheri, A. Honer, W. G., Lazarov, O. (2019). Human hippocampal neurogenesis persists in aged adults and Alzheimer’s disease patients. Cell Stem Cell, 24(6), 974-982.
Webb, S. J., Monk, C. S., & Nelson, C. A. (2001). Mechanisms of postnatal neurobiological development: Implications for human development. Developmental Neuropsychology, 19, 147-171.
Weir, K. (2015). Marijuana and the developing brain. Monitor on Psychology, 46(10), 49-52.
Media Attributions
- BRAIN BRAIN © CNX OpenStax Biology is licensed under a CC BY-SA (Attribution ShareAlike) license
- night-7984333_1920 © bongbabyhousevn
- father-22194_1280 © PublicDomainPictures is licensed under a CC BY-SA (Attribution ShareAlike) license
- pexels-karolina-grabowska-5877583 © Photo by Photo By: Kaboompics.com is licensed under a CC BY-SA (Attribution ShareAlike) license

