3 Female Reproductive System
STUDENT LEARNING OUTCOMES
At the end of this chapter you should be able to
- Recall the difference between oviparity and viviparity
- Explain why the amniotic egg confers the ability to adopt a terrestrial lifestyle
- Discuss why internal fertilization would lead to the evolution of the sex organs
- Identify and describe the human female sex organs and external genitalia
- Discuss why comparatively little is known about female genitalia
Primary sexual dimorphism is the result of the evolution of life on land
As explained in the earlier chapter the Evolution of Sex, sexual reproduction involves “mating” between two different individuals and the joining of their respective haploid gametes, resulting in a genetically distinct diploid zygote. The evolution of dimorphic structures to produce and deliver gametes for successful fertilization was an important part of the trajectory of the advancement of sexual reproduction. The evolution of sex happened multiple times but also always in an aquatic environment permitting individuals to release gametes for external fertilization. As life evolved to transition to terrestrial environments, selection for modifications in the reproductive organs to support internal fertilization and protection of the developing zygote also occurred. The key features of the basic female reproductive system are ovaries that produce eggs, and accessory organs for the transfer and reception of eggs and sperm all of which are under hormonal regulation.
Internal fertilization and the amniotic egg
There is diversity in how mating occurs across vertebrate taxa. In aquatic environments, females and males can synchronize the release of gametes directly into the water, and fertilization happens externally. Species that have adapted to a completely terrestrial lifestyle are unable to engage in external fertilization because of the problem of desiccation and instead rely on internal fertilization. Males introduce sperm into the female reproductive tract whereby a sperm can fuse with an egg in a protected environment.

The evolution of the amniotic egg protected by a calcified shell that houses the amniotic membrane, in addition to the chorion, allantois, and yolk sac was a major step that allowed vertebrates to reproduce in a terrestrial environment. Many vertebrate species are oviparous meaning fertilized eggs are laid outside the body, whereby embryos can complete development through an external incubation period. In viviparous species, the embryo completes development (or nearly so) inside the mother’s reproductive tract (see the image on left forcomparison of the two). Viviparity has evolved independently in multiple lineages “in at least 142 occasions in vertebrate history” (Blackburn 1999). It is exhibited within multiple groups including sharks, caecilians, anurans (frogs and toads), salamanders, snakes, lizards, and mammals.
Female accessory sex organs of the reproductive system evolved along with the amniotic egg. The accessory organs transitioned from a “simple tube-like structure present at embryogenesis that develops into a specialized oviduct in oviparous species…” or as in eutherian mammals “…a highly vascularized structure for supporting complete embryogenesis…” (Major et al. 2022). The eutherian mammals (of which humans are a member) are characterized by having a placenta that supports embryonic development, contrasted from monotremes (oviparious mammals) and marsupials (embryos develop in a specialized pouch). The female reproductive tract of eutherians is also distinct when compared to the other tetrapods, a group whose members include mammals, amphibians, birds, and reptiles. Those non-eutherian tetrapods have a common urogenital opening called a cloaca whereas eutherians have a separate complex perineal structure (Hall, Rodriguez-Sosa, and Plochocki 2017) that provides compartmentalization for increased complexity (Pavlicev, Herdina, and Wagner 2022).
Human female sex organs and genitalia
Key events in the development of the female reproductive tract unfold during embryonic development and puberty. Development is described in the previous chapter and the processes of puberty and sexual maturation are described in the chapter on the Reproductive Cycle. Much is still unknown about the evolution and functionality of female sex organs and genitalia, and as Sloan and Simmons (2019) point out, “traditionally, male genitalia have been the overwhelming focus of evolutionary studies”. For female empowerment, we need a more complete knowledge of female evolution, anatomy, physiology, and so forth.
The primary sex characteristics and anatomical structures within the female reproductive system are discussed below, including ovaries, Fallopian tubes, uterus, cervix, vagina, and external genitalia.
Ovaries
A pair of ovaries is the site of oocyte development and the production and secretion of the steroid hormones estrogen, inhibin, progesterone, and testosterone. Each ovary is suspended in the pelvic cavity by a suspensory ligament (attached to the lateral margin of the ovary and extends to the lateral pelvic sidewall) and an ovarian ligament (connects the ovary to the side of the uterus). They are also attached to the peritoneal covering through the mesovarium which projects from the posterior surface of the broad ligament and attaches to the ovary. The mesovarium is a double-layered fold of the peritoneum (a thin membrane that lines the abdominal cavity and covers organs) that helps anchor and support the ovaries in their position within the pelvic cavity.
The ovaries are covered on the outside by a layer of simple cuboidal epithelium called germinal (ovarian) epithelium. Below the ovarian epithelium is a dense connective tissue capsule, called the tunica albuginea, a Latin term that roughly translates to “white coat”. It is so named because of its dense, white, fibrous appearance and it functions as a protective sheath.
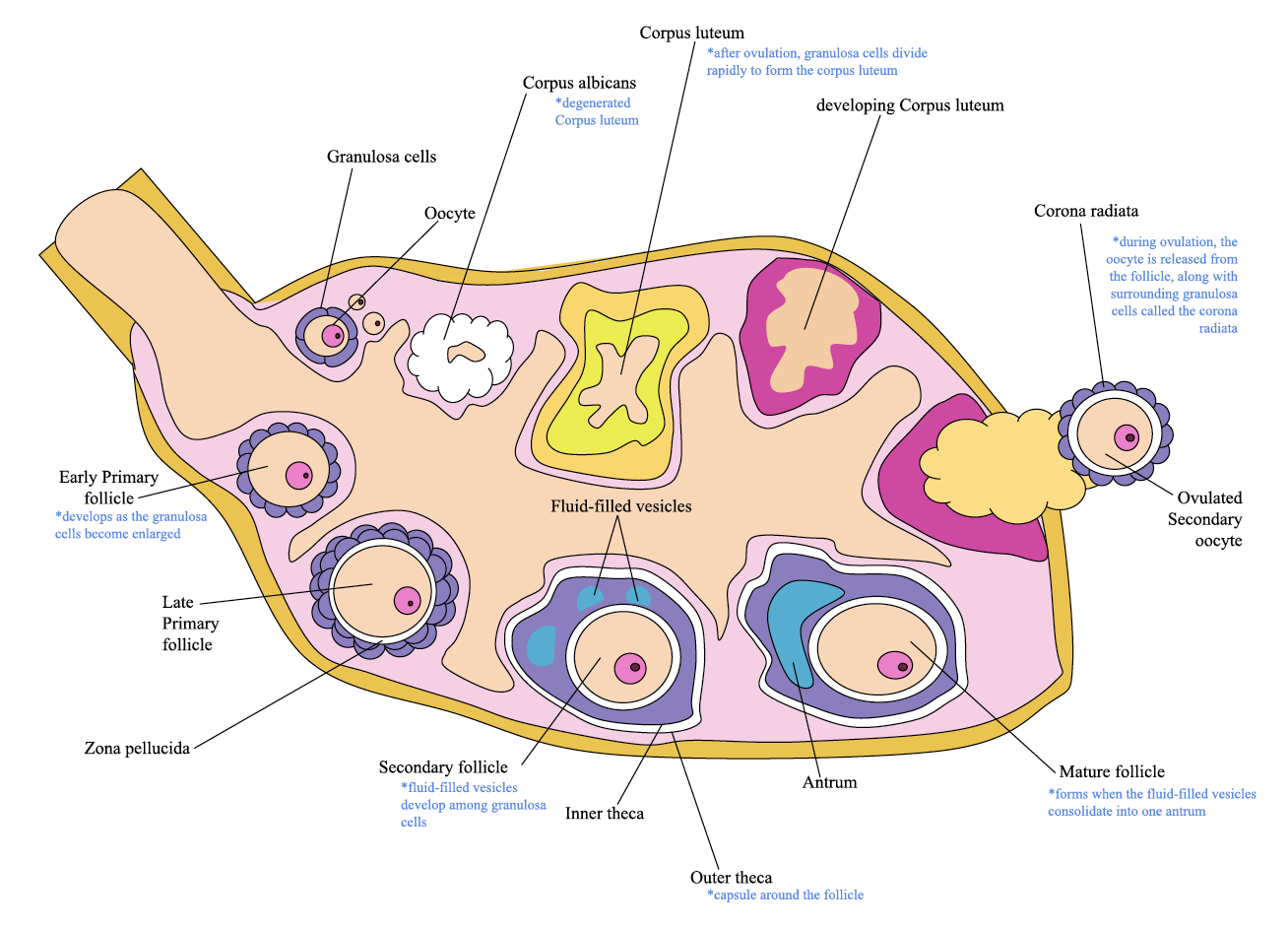
Within can be found the inner medulla: a heterogeneous mix of immune cells, blood vessels, nerves, stem cells, and lymphatic vessels, all of which make up the ovarian interstitial stroma (Kinnear et al. 2020). A membrane, the basal lamina, separates the interstitial stroma from the functional units of the ovary known as the ovarian follicles. These lie within the outer cortex (Oktem and Urman 2010). The follicles are composed of oocytes surrounded by granulosa cells at various stages of development (details on follicles can be found in the Reproductive Cycle chapter). The diagram below illustrates an ovary with the follicles at varied stages of development.
Oviducts (Fallopian tubes)
There are two oviducts (uterine tubes) approximately 7 to 12 cm long. One is associated with each ovary, also called the Fallopian tube after Gabrielle Fallopius (Mortazavi et al. 2013). These serve as conduits that receive mature ovum from the ovaries, the site for fertilization and transport of the zygote to the uterus.
Within the oviduct
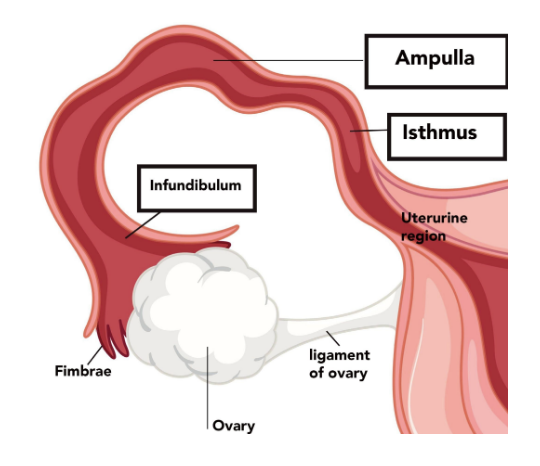
The oviduct is divided into four regions (from ovary to uterus) pictured below. 1) the infundibulum, which is surrounded by fingerlike extensions called fimbriae that are not directly connected to the ovary but “brush” the ovary; 2) the ampulla, 3) the isthmus and 4) the uterine region.
The inner mucosal layer of the oviduct is composed of epithelial cells responsive to estrogen and progesterone. The epithelial tissue on the inner surface of the oviduct is comprised of two main cell types: ciliated epithelial cells and nonciliated secretory epithelial cells. A muscular layer lies between the inner mucosa and the contractions of this muscular layer work in conjunction with cilia movements and tubal secretory fluids to achieve ovum transport along the length of the oviduct (Sokal 2011).
Uterus
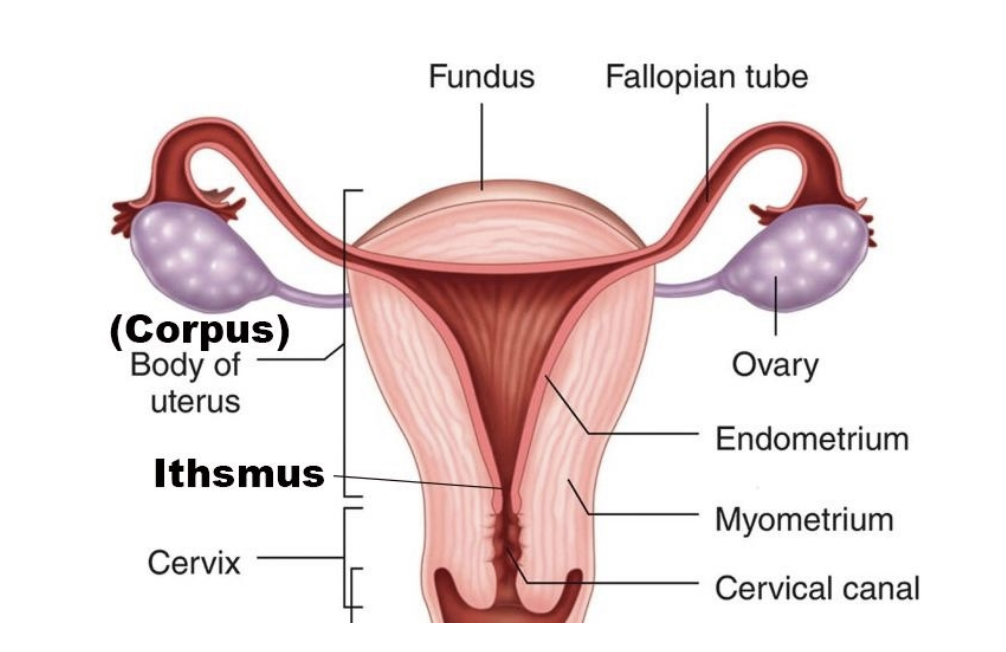
Anatomy of the uterus.
The uterus is a fibromuscular organ with an endometrial lining that functions by preparing for and ultimately supporting the embryo. As the embryo grows and matures, the uterus expands to accommodate the developing fetus.
There are three main parts to the uterus, cervix, fundus, and main body. Ovaries and fallopian tubes have been omitted for emphasis.The endometrium varies greatly depending on the phase of the menstrual cycle. The proliferation of the endometrium occurs under the influence of estrogen; maturation occurs under the influence of progesterone. Details are provided in the Reproductive Cycle chapter.
Humans have a pear-shaped uterus suspended by several ligaments, including the utero-ovarian ligament, round ligament, broad ligament, cardinal ligament, and uterosacral ligament. The uterus is further supported (inferiorly) by the pelvic diaphragm, urogenital diaphragm, and perineal body. The size varies tremendously depending on hormonal status, pregnancy, and prior pregnancies.
The uterus subdivides into four main anatomic segments (from superior to inferior): the fundus; a broad curved area in which oviducts connect to the uterus, the corpus (body); the main part of a uterus, and it starts directly below the level of fallopian tubes and continues downward, the isthmus is a lower neck region of the uterus, and cervix; which extends downwards from the isthmus and opens in the vagina.
In addition to the endometrial layer, the uterus has a muscular layer that lies beneath (myometrium). The outer surface is covered by a thin epithelial layer (perimetrium) known as the serosa.
Cervix
The cervix is a fibromuscular organ that protrudes into the uterine cavity and down to the vagina, (linking the two together). It contains columnar epithelium that produces cervical fluid secretion which varies dramatically in response to estrogen (Levin 2003). At the upper end of the endocervical canal at the junction with the uterine cavity is the internal os, and the external os is the opening of the cervix within the vagina. Above the external os lies the fusiform endocervical canal, approximately 2 cm long and lined with columnar epithelium and endocervical glands. The intersection where the squamous epithelium of the exocervix and columnar epithelium of the endocervical canal meet, the squamocolumnar junction, is dependent on hormonal stimulation and is also known as the transformation zone (Sokal, 2011).
Vagina
The vagina is an elastic, muscular tube connected to the cervix proximally and extends to the external surface through the vulva vestibule. The vaginal opening is located posterior to the urethra opening. The vagina has many functions: to act as a reservoir and passageway for semen during sexual intercourse, an exit for menstrual blood, a sensitive area for sexual stimulation; and a birth canal for the passage of the baby from the uterus. The vaginal wall consists of three layers: a) an inner mucous-type stratified squamous cell epithelium supported by a thick lamina propia, that undergoes hormone-related cyclical changes, b) the muscularis composed of outer longitudinal smooth muscle fibers and inner circular fibers, and c) an outer fibrous layer, rich in collagen and elastin, which provides structural support to the vagina.
Vaginal lubrication during sexual stimulation
Lubrication is needed to promote sexual pleasure however the vagina’s lubrication does not come from glands but from a transducive fluid expressed through vaginal epithelial cells with the aid of nitric oxide (NOs) (Levin, 2003). The exact mechanism is not completely understood but research indicates that estrogen promotes both blood flow and NOs and the transducate is produced when the blood vessels of the lamina propria become engorged during sexual arousal creating pressure (Musicki et al. 2009).
The Vulva
The vulva, illustrated below, describes the external female genitalia: mons pubis, labia majora, labia minora, clitoris, and vulvar vestibule.
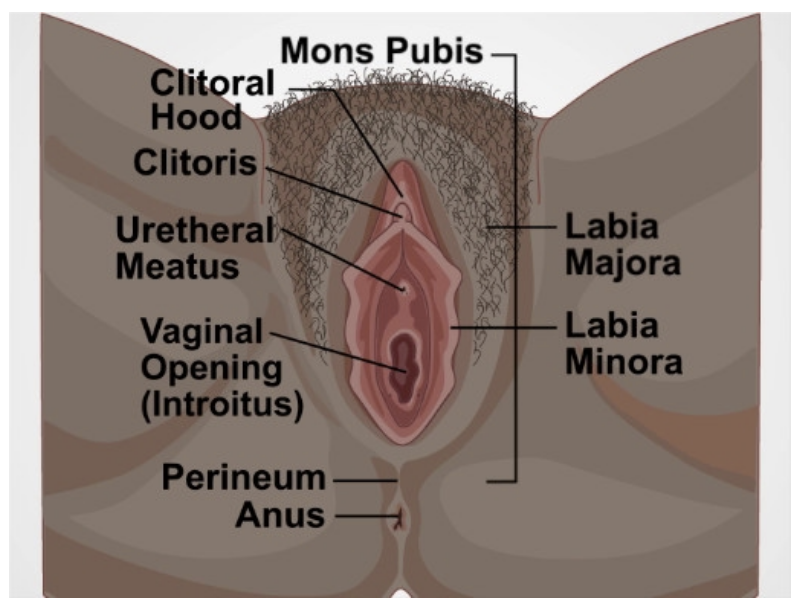
Mons pubis
The mons pubis is a mound of adipose tissue located directly anterior to the pubic bones. Upon puberty, it becomes covered in pubic hair. According to Nguyen and Duong (2022) the mons pubis functions as a source of cushioning during sexual intercourse. The mons pubis also contains sebaceous glands that secrete pheromones to induce sexual attraction.
The Labia Minora and Majora
There are two pronounced folds of fibroadipose tissue that protect the opening of the vagina which looks like lips called labium, the outer is known as the labia majora and the smaller, inner is known as the labia minora. The inner surface of the labia majora and labia minora lack hair follicles or sweat glands but contain many sebaceous glands that release sebum onto the skin surface. The labia minora are derived from the same tissue as in males and share homology with the penile urethra and part of the skin of the penis in males. The labia minora is composed of dense connective tissue, erectile tissue, and elastic fibers and “laterally, they extend obliquely from the clitoris toward the rear for about 4 cm on either side of the vaginal orifice” (Deliveliotou and Crestas 2006). The fourchette is where the labia minora meet, and below this is the perineum that ends at the anus.
The Clitoris
The clitoris whose etymology may be traced back to the Greek noun “kleis” which means key, is located at the top of the vestibule and has been identified as “the most critical anatomical structure for female sexual arousal and orgasm” (Pauls 2015). As Masters and Johnson (1966) famously wrote in their book Human Sexual Response, “the clitoris is truly unique in the human organ system in that its only known function is that of serving as an erotic focus for both afferent and efferent forms of sexual stimulation”. There is a great deal of size variation in the clitoris and this variation is greater than penile size variation (Wallen and Lloyd 2011). The first comprehensive study of the clitoris was not completed until 1998 by O’Connell et al. (1998).
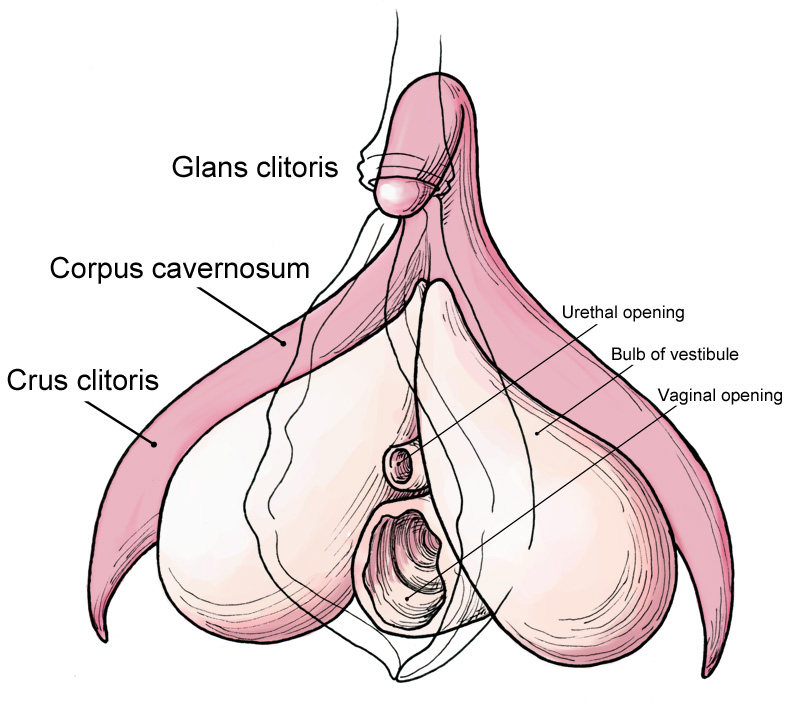
The clitoris, illustrated on the right, is tri-planar with three main parts: the glans clitoris (external); two crura extending down from the glans and deep into the vulva, where the corpora are located; two bulbs that extend on either side of the vagina. Variation in the size and shape of the clitoris exists (Longhurst et al., 2023). The visible portion of the clitoris is a small rounded tubercle (glans clitoris) with many nerve endings and is highly sensitive to touch. The majority of the clitoral anatomy is internal. “The body (corpora) of the clitoris consists of two cylindrical corpora cavernosa composed of thin-walled, vascular channels that function as erectile tissue” (Deliveliotou and Crestas 2006). Both the corpora and glans are homologous to the corpus cavernosa and glans of the male penis (Shih, Cold, and Yang 2013). There are also a pair of bulbs, “the bulbs of the clitoris”, that are contiguous with the glans and corpora of the clitoris that engorge with blood during sexual arousal (O’Connell et al., 1998). Along with the glans, the internal areas are also erotically responsive. The urethra lies surrounded by this complex and extends from the bladder to the outside of the body for the excretion of urine.
Longhurst et al., (2023) note that “historically the stigma and lack of understanding of the function of the clitoris led to the justification and, unfortunately, the performance of clitoridectomies (removal of the clitoris) as a treatment for insanity, epilepsy, catalepsy, and hysteria.” Unfortunately, clitoridectomies and other types of injuries to female genital organs, known as female genital mutilation, are still performed worldwide (Molina-Gallego et al., 2021).
Q&A with Prof. Helen E O’Connell AO ,MD MMed FRACS FAICD,

Officer (AO) in the General Division of the Order of Australia, Urological Surgeon
What drew you to study Urology and specifically female genitalia? Urology was definitely a source of great mystery. We had relatively minimal teaching throughout our medical degree. As a young doctor, I was encouraged to look at specialty surgery rather than general surgery, which was regarded as ‘dead’ prior to the rise in laparoscopic surgery. As a young resident, I recall female patients being delighted to have a woman to talk to about their urinary problems. For the first time, it wasn’t an advantage to be female! Our textbook- Lasts Anatomy was full of factual errors and omissions when it came to the description of the female perineum. The use of pejorative language, paucity of diagrams, and outright omission of the clitoris made me angry at first, I was even suspicious about the nature of Anatomy as a science. It appeared that social factors were dominating the discourse.
What have you enjoyed most about your research? The journey itself is a great unknown with the unthinkable evolution of the science and art of female anatomy over my career. The 3-D models based on MRI studies as well as cadaveric studies bring the Anatomy to life. Literally, you can hold the anatomy in your hands. Designers, artists, and prominent speakers are forging, a community-based movement, fed by accurate science that is empowering, both women and men. Understanding the relationship of the clitoris to the vulva, vagina, and urethra is now tangible through good images. This helps women and girls understand their bodies in a way that is wholesome and promotes better health. None of this was foreseeable.
What did you find most challenging about your career? Managing time is probably the most challenging aspect. There is a significant call on a reasonably finite resource and ensuring all of my priorities are looked after takes some doing.
What advice do you have for future women scientists? Get the best training that you can. Do work that will distinguish you from others in a good way. Don’t be too worried about burnout. It will happen and you’ll recover with a good two-week break. Choose good mentors. As you rise up, look after your staff and your mentees and treat everyone with respect. Make time for family, friends, and fun.
Skene’s Glands
Homologous to the prostate in the male, these are branched, tubular glands, adjacent to the distal urethra. Dwyer (2012) reports that the location of Skene’s glands is in an area designated as the Grafenberg spot (G spot) which has been anecdotally associated with stimulation and ejaculation during orgasm.
Vulvar vestibule
Just posterior to the glans clitoris lies the vestibule. This extends to the fourchette of the labia minora. The vestibule contains the vaginal opening and is bordered by the edges of the labia minora.
The Bartholin’s glands also known as the greater vestibular glands
There are two “pea-sized glands located symmetrically at the posterior region of the vaginal opening… which are involved in “mucus secretion and vaginal lubrication. Cyst formation in the glands is common and results from mucus build-up in gland ducts” (Yee and Goldstein 2023).
Variation of mammalian reproductive tracts exists
All female animal reproductive tracts are derived from the Müllerian ducts in the embryo, however, the mammalian female reproductive tract is much more complex when compared to other animals and exhibits diversity across mammalian species (Major et al. 2022). It is through “species-specific differences in Müllerian duct fusion at the midline, growth, and differentiation” that these distinct morphologies arise (Machado, Ontiveros, and Behringer 2022). As illustrated in Kobayashi and Behringer (2003), there are three distinct general morphologies: duplex without a vagina, duplex with vagina or simplex. The duplex uterus is divided into two separate horns that each have separate cervices whereas the simplex uterus has a single chamber. Examples of variation are seen from monotremes through higher primates. Marsupials have duplex uteri with two vaginae; rabbits, rodents, pigs, and marine mammals-duplex uteri with a single vagina (seen below), and higher primates have a simplex uterus.
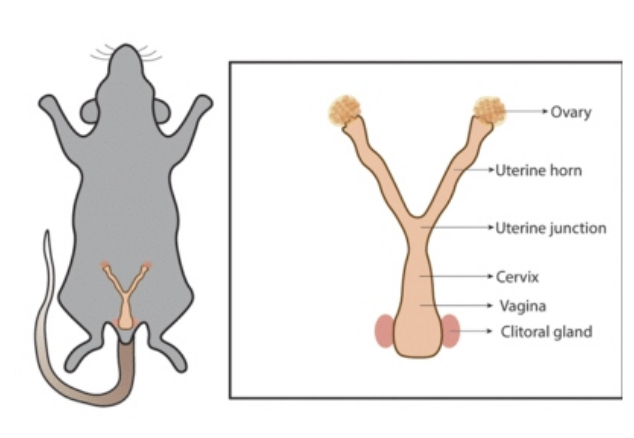
The mammalian female reproductive tract can be considered an evolutionary marvel having undergone significant adaptations and complexities over millions of years. Viviparity, placental development ovulation control, and behavioral complexities are just some of the key adaptations involved in the reproductive tract that have contributed to mammalian success and the great diversification from the early Cretaceous era onward.
Think, Pair, Share
Come up with a list of reasons that there has been a limited amount of research done on the female sex organs and genitalia as compared to the male genitalia.
Discuss reasons why women are not well informed about their sex organs and external genitalia.
Why might there be variation in the structure of the uterus across mammalian taxa? E.g. simplex and duplex?
Across animal taxa, females and males have different sex organs but what other ways are they different?
Deeper Questions
Echidnas and platypus are monotremes and diverged from the eutherians around 187 million years ago. Explain why monotremes provide the key to understanding how viviparity evolved in mammals.
A survey conducted in 2020 of 2,000 women found that nearly 25% misidentified the vagina and 46% could not properly identify the cervix. How can this be rectified?
In an article by Wahllquist published in the Guardian (2020) “The sole function of the clitoris is female orgasm. Is that why it’s ignored by medical science?” Urologist Helen O’Connell (who completed the first comprehensive anatomical study of the clitoris) was interviewed and said “female anatomy should be considered equally alongside male anatomy”. Why is this so important and what challenges still exist that hinder this?
Key terms
Ampulla
Bartholin’s glands
Cervix
Clitoris
Corpus cavernosa
Crura
Endometrium
External os
Fallopian tubes
Fimbriae
Glans clitoris
Infundibulum
Inner medulla
Internal os
Isthmus
Labia majora
Labia minora
Mesovarium
Mons pubis
Myometrium
Outer cortex
Ovaries
Oviduct
Oviparity
Perimetrium
Skene’s glands
Transformation zone
Tunica albuginea
Uterus
Vagina
Vestibule
Viviparity
Vulva
References
Blackburn, D. 1999. “Viviparity and Oviparity: Evolution and Reproductive Strategies.” In Encyclopedia of Reproduction, 4:994–1003. Academic Press.
Chumduri, C., and M. Y. Turco. 2021. “Organoids of the female reproductive tract.” Journal of Molecular Medicine 99: 531–553. https://doi.org/10.1007/s00109-020-02028-0
Deliveliotou, A., and G. Crestas. 2006. “Anatomy of the Vulva.” In The Vulva Anatomy, Physiology and Pathology, 1–7. Informa Health Care.
Dwyer, Peter L. 2012. “Skene’s Gland Revisited: Function, Dysfunction and the G Spot.” International Urogynecology Journal 23 (2): 135–37. https://doi.org/10.1007/s00192-011-1558-1.
Hall, M. I., J. R. Rodriguez-Sosa, and J.H. Plochocki. 2017. “Reorganization of Mammalian Body Wall Patterning with Cloacal Septation.” Scientific Reports 7 (1): 9182. https://doi.org/10.1038/s41598-017-09359-y.
Kinnear, H. M., C. E. Tomaszewski, F. L. Chang, M. B. Moravek, M. Xu, V. Padmanabhan, and A. Shikanov. 2020. “The Ovarian Stroma as a New Frontier.” Reproduction (Cambridge, England) 160 (3): R25–39. https://doi.org/10.1530/REP-19-0501.
Kobayashi, A., and R. R. Behringer. 2003. “Developmental Genetics of the Female Reproductive Tract in Mammals.” Nature Reviews Genetics 4 (12): 969–80. https://doi.org/10.1038/nrg1225.
Levin, R. J. 2003. “The Ins and Outs of Vaginal Lubrication.” Sexual and Relationship Therapy 18 (4): 509–13. https://doi.org/10.1080/14681990310001609859.
Longhurst, G. J., R. Beni, S. Ryeon Jeong, M. Pianta, A. L. Soper, P. Leitch, G. De Witte, and L. Fisher. “Beyond the tip of the iceberg: A meta‐analysis of the anatomy of the clitoris.” Clinical Anatomy 2023.
Machado, D. A., A. E. Ontiveros, and R. R. Behringer. 2022. “Chapter Three – Mammalian Uterine Morphogenesis and Variations.” In Current Topics in Developmental Biology, edited by Thomas Gridley and Leif Oxburgh, 148:51–77. Academic Press. https://doi.org/10.1016/bs.ctdb.2021.12.004.
Major, A. T., M. A. Estermann, Z. Y Roly, and C. A Smith. 2022. “An Evo-Devo Perspective of the Female Reproductive Tract.” Biology of Reproduction 106 (1): 9–23. https://doi.org/10.1093/biolre/ioab166.
Masters, W. H., and V. E. Johnson. 1966. Human Sexual Response. Little, Brown.
Molina-Gallego, B., L. Mordillo-Mateos, G. Melgar de Corral, S. Gómez-Cantarino, B. Polonio-López, and M. Idoia Ugarte-Gurrutxaga. “Female genital mutilation: knowledge and skills of health professionals.” In Healthcare 9(8): 974. MDPI.
Mortazavi, M. M., N. Adeeb, B. Latif, K. Watanabe, A. Deep, C. J. Griessenauer, R. S. Tubbs, and T. Fukushima. 2013. “Gabriele Fallopio (1523-1562) and His Contributions to the Development of Medicine and Anatomy.” Child’s Nervous System : ChNS : Official Journal of the International Society for Pediatric Neurosurgery 29 (6): 877–80. https://doi.org/10.1007/s00381-012-1921-7.
Musicki, B., T.Liu, G. A. Lagoda, T. J. Bivalacqua, T. D. Strong, and A. L. Burnett. 2009. “Endothelial Nitric Oxide Synthase Regulation in Female Genital Tract Structures.” The Journal of Sexual Medicine 6 (Supplement_3): 247–53. https://doi.org/10.1111/j.1743-6109.2008.01122.x.
Nguyen, J., and H. Duong. 2022. “Anatomy, Abdomen and Pelvis, Female External Genitalia.” In StatPearls. Treasure Island FL: StatPearls Publishing.
O’CONNELL, H. E., J. M. HUTSON, C. R. ANDERSON, and R. J. PLENTER. 1998. “ANATOMICAL RELATIONSHIP BETWEEN URETHRA AND CLITORIS.” The Journal of Urology 159 (6): 1892–97. https://doi.org/10.1016/S0022-5347(01)63188-4.
Oktem, O., and B. Urman. 2010. “Understanding Follicle Growth in Vivo.” Human Reproduction 25 (12): 2944–54. https://doi.org/10.1093/humrep/deq275.
Pauls, R. N. 2015. “Anatomy of the Clitoris and the Female Sexual Response.” Clinical Anatomy 28 (3): 376–84. https://doi.org/10.1002/ca.22524.
Pavlicev, M., A. N. Herdina, and G. Wagner. 2022. “Female Genital Variation Far Exceeds That of Male Genitalia: A Review of Comparative Anatomy of Clitoris and the Female Lower Reproductive Tract in Theria.” Integrative and Comparative Biology 62 (3): 581–601. https://doi.org/10.1093/icb/icac026.
Shih, C., C. J. Cold, and C. C. Yang. 2013. “Cutaneous Corpuscular Receptors of the Human Glans Clitoris: Descriptive Characteristics and Comparison with the Glans Penis.” The Journal of Sexual Medicine 10 (7): 1783–89. https://doi.org/10.1111/jsm.12191.
Sloan, N. S., and L. W. Simmons. 2019. “The Evolution of Female Genitalia.” Journal of Evolutionary Biology 32 (9): 882–89. https://doi.org/10.1111/jeb.13503.
Sokal, E. 2011. “Clinical Anatomy of the Uterus, Fallopian Tubes, and Ovaries.” In Global Library Women’s Medicine. DOI 10.3843/GLOWM.10001.
Wallen, K., and E. A. Lloyd. 2011. “Female Sexual Arousal: Genital Anatomy and Orgasm in Intercourse.” Hormones and Behavior 59 (5): 780–92. https://doi.org/10.1016/j.yhbeh.2010.12.004.
Yee, A., and I. Goldstein. 2023. “Marsupialization of the Bartholin Duct Cyst and Recanalization for Symptomatic Recurrent Bartholin Cysts.” The Journal of Sexual Medicine 20 (Supplement_2): qdad061.125. https://doi.org/10.1093/jsxmed/qdad061.125.
Suggested Readings
“The Female Reproductive System: An Anatomical and Histological Atlas” by Konrad Stender, Rainer Winkelmann, and Jürgen Görtz – This atlas provides detailed anatomical and histological illustrations and descriptions of the female reproductive system, making it a valuable resource for understanding its structure and function.
“The Vagina Bible: The Vulva and the Vagina: Separating the Myth from the Medicine” by Dr. Jen Gunter – Dr. Jen Gunter’s book is a comprehensive guide that covers everything you need to know about the female reproductive tract, debunking myths and providing evidence-based information on vaginal and vulvar health.
“She-ology: The Definitive Guide to Women’s Intimate Health. Period” by Sherry A. Ross – The author is a leading ob-gyn, educator and women’s health advocate, Ross addresses every urgent, confounding, culturally taboo or embarrassing question women have about vaginas
“Our Bodies, Ourselves” by the Boston Women’s Health Book Collective – While not exclusively focused on the female reproductive tract, this classic book covers women’s health comprehensively, including detailed information about reproductive anatomy and health.
Interesting Podcast
Ologies with Alie Ward Gynecology (NETHER HEALTH) with Philippa Ribbink
