20
Aubrey Plourde
Introduction
Keywords
- prosthetic
- passive prosthetic
- body-powered prosthetic
- myoelectric prosthetic
- neural prosthetic
- motor cortex
- posterior parietal cortex
- magnetic resonance imaging (MRI)
- diffusion MRI
- functional MRI
Learning Objectives
- Identify the purpose of prosthetics
- Differentiate between the different types of prosthetics
- Give examples of successful neural prosthetics
- Explain the history of MRIs and how they work
- List some ways that MRIs have evolved/are evolving
Over the past 20 years, there have been countless technological advancements in the medical field, specifically in prosthetics and magnetic resonance imaging (MRI), that have changed the face of medicine for the better. Doctors and scientists have been working on ways to improve prosthetics and restore amputees’ and paralytics’ feeling of movement and touch. Additionally, MRI technology has evolved and become more advanced than ever before. Both prosthetics and MRI development will shape the future of medicine and bring it to new levels.
Nowadays, prosthetic limbs make everyday life easier for amputees. They are able to use the prosthetic as a replacement for the body part they do not have. There is ample research on how to make prosthetics work exactly as a real limb would. The possibility of a prosthetic having the same functionality as a real limb is highly likely and would allow amputees to feel a sense of normalcy. MRI machines are constantly being revolutionized in order to produce higher quality images of organs and tissues that were originally very difficult to scan. The technology is also being changed to allow patients to feel more comfortable while receiving an MRI scan. With this new technology, diseases could be spotted earlier and treated better, saving many lives.
Prosthetics
Key Takeaway
The use of prosthetics has been greatly developed over time, and it is still growing. The new possibilities of prosthetics could dramatically impact the way amputees and paralytics live their everyday lives.
A prosthetic or prosthesis is an artificial device that replaces a missing or dysfunctional body part. Prosthetic limbs have been around for thousands of years, the earliest found in Egypt dating back to between 950-710 B.C.E. It was actually the big toe of a noblewoman, and while it is not what most people think of as a prosthetic, it was important to Egyptians at the time to have the big toe (Bender, 2015). As time has passed, the need for prosthetics has increased, and in turn, prosthetics have evolved into what they are today. Prosthetics are classified into four main categories: above the elbow, below the elbow, above the knee, and below the knee. Leg amputees use prosthetics for mobility and stability and to prevent muscle atrophy, whereas arm amputees use prosthetics mainly for aesthetic purposes (Nevils-Karakeci, 2020).

“Prosthetic toe” by Jon Bodsworth is in the Public Domain
There are many different types of prosthetics with different purposes. Passive prosthetics have very little function other than having a natural appearance. They are lightweight which require less effort to wear and typically provide more comfort. Prosthetic fingers and toes can also be made for aesthetic purposes. Body-powered prosthetics consist of harnesses and cables that are controlled by the chest and shoulders. The cables and harness allow the prosthetic hand to open or close which gives an amputee the opportunity to do different activities. Myoelectric prosthetics are controlled by sensors that are connected to muscles that can detect electrical impulses. The sensors can be connected to the remainder of an arm if the nerves and muscles are still responsive, or the back or chest muscles if the arm nerves and muscles are too damaged (Nevils-Karakeci, 2020).
Lower-body amputees can use prosthetics for mobility beyond crutches or a wheelchair. A prosthetic leg is fitted based on the residual limb, and a socket is fitted to attach the prosthesis. The socket fit is very important because if it is not properly fit to the residual limb, it can cause discomfort, friction, swelling, and skin damage. Above-the-knee amputees have many options to choose from regarding the new knee prosthetic. The prosthetic knee can have a single axis or multiple axes, weight-activated or muscle controlled stability, and the potential to have a prosthetic that allows for a more natural gait. Additionally, these amputees use more energy and take in more oxygen than depending on the type of amputation they have. Prosthetic selection involves gait training, many socket fittings, and physical and occupational therapy. Because of everything that goes into getting a prosthetic, the process is very well thought-out and carefully considered and individualized for every amputee (Nevils-Karakeci, 2020)

“Below-knee amputee runs for berth in 2012 Paralympics” by Jon Bodsworth is licensed under CC BY 2.0
Neural Prosthetics
Key Takeaway
The most recent development of prosthetics is the research of neural prosthetics. They are very useful in bringing back most, if not all functionality to an amputee or paralytic. Doctors and scientists have had lots of success in their neural prosthetic experimentation.
A neural prosthetic (or neural prosthesis) is an assistive device that restores functions lost as a result of neural damage (Prochazka et al., 2001). They are connected to neurons, the specialized cells in the brain, and help restore any sensory loss. Neurons send electrical signals to various parts of the body to coordinate brain activity. Using this information, scientists are able to mimic the electrical signals with a neural prosthetic. The oldest form of neural prosthetic is a cochlear implant that helps people with different levels of hearing loss. It does not completely restore a person’s hearing ability, but it does greatly improve the amount of sound they can pick up (Lehrman, 2015).

“Infant with cochlear implant” by bjorn knetsch is licensed under CC BY 2.0
Both amputees and paralytics can benefit from neural prosthetics. Amputees have had one or more of their limbs amputated or were born without one or more of their limbs. A paralytic is someone who suffers from paralysis, a loss of control over a muscle or group of muscles in a part of the body. Since paralytics and amputees have brain functionality, they are still able to plan out movements in their brain, they just cannot execute them. With a brain implant, a person’s brain signals can be observed and recorded that develop an algorithm to create the prosthetic. The prosthetic would give the person the opportunity to restore his or her motor functions that were previously lost (Andersen et al., 2010).
There have been many success stories of neural prosthetics. At the University of Michigan, in March 2020, a prosthetic hand was developed that responds to brain signals. At the beginning of the experimentation, it was difficult to get the appropriate response from the prosthetic because nerve signals are so small and quiet. To bypass the issue, the peripheral nerves were connected to a piece of muscle. Allowing the nerve to control the entire muscle made the signal large enough to control the prosthetic hand. The test patients were able to grasp objects and have finger-level control of the prosthetic hand. The amputees that tested the hand even said “it’s like you have a hand again” (University of Michigan Engineering, 2020).
In 2015, at the California Institute of Technology, researchers figured out exactly where to place the neural prosthesis to maximize the correct movement in as fluid of a motion as possible. Originally, the neural prosthesis was placed in the motor cortex, the part of the brain that executes the motions of the body. This resulted in jerky, irregular motions that do not imitate a real limb. After more thinking, the neural prosthesis was moved to the posterior parietal cortex, the part of the brain responsible for planning movement. The test patient had much more fluid motion of the prosthetic arm when he visualized the planned-out movements. He was able to shake another person’s hand and even play rock paper scissors (Caltech, 2015).
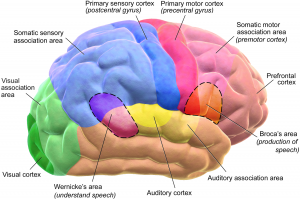
“Blausen 0102 Brain Motor&Sensory” by BruceBlaus is licensed under CC BY 3.0
At the University of Pittsburgh, Dr. Robert Gaunt was able to give Nathan Copeland the feeling of touch again. Nathan Copeland was in a car accident and paralyzed from the neck down. He does have slight movement in his shoulders and wrists, but for the most part, has no functionality. Gaunt connected Copeland to the Brain Computer Interface (BCI) that allowed him to control a robotic arm. The surgeons who attached the BCI to Copeland’s brain had to choose specific locations of his brain to make sure it would properly work. When Dr. Gaunt touched parts of the prosthetic hand, it felt as if Copeland’s own hand was being touched. There was electrical stimulation to his neurons that allowed the feeling of touch to be as real as possible. With all of the new technology development of neural prosthetics, the life of an amputee or paralytic could be greatly improved and potentially give them back full functionality of their body (UPMC, 2016).
Magnetic Resonance Imaging
Key Takeaway
Magnetic Resonance Imaging (MRI) has changed the face of medicine. It has been evolving since its invention and researchers have been refining and will continue refining the technology and techniques of MRI.
Magnetic resonance imaging (MRI) uses a strong magnetic field and radio waves to create detailed images of organs and tissues inside the body (Marcin, 2018). The human body is full of water, which means that it is also full of hydrogen nuclei (protons), which are positively charged. An MRI machine generates a strong electric field that affects the protons’ spin and causes them to become unaligned. When the machine is turned off, the protons gradually align back with their proper spin, a process called precession. The protons returning to their natural spin can be measured by the MRI, and different organs and tissues return at different speeds. There are multiple magnetic fields that can produce images at different angles (Lewis, 2017).

“Patient being positioned for MR study of the head and abdomen” by Ptrump16 is licensed under CC BY-SA 4.0
There are two main types of MRIs: diffusion and functional. Diffusion MRI measures how water molecules diffuse through body tissues. Certain diseases, like a stroke or a tumor, can restrict diffusion, so diffusion MRI can help diagnose them. Functional MRI is used to visualize brain activity by measuring blood flow changes to the brain. It can be used to observe brain structures and determine how the brain is handling critical functions. It is also used to evaluate any possible head trauma or Alzheimer’s disease (Lewis, 2017).
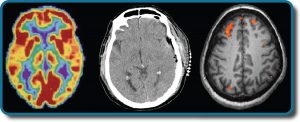
“FMRI” by OpenStax is licensed under CC BY 4.0
There are a few precautions before getting an MRI scan. Since an MRI is essentially a giant magnet, any kind of metal in a person’s body can pose a problem. It could heat up or move a metal implant such as a pacemaker, artificial joints, cochlear implants, or metal rods, plates, or screws (Lewis, 2017). Pregnant women should also avoid getting an MRI scan, especially in the first trimester. While there is no definitive evidence that the magnetic field really affects the fetus, there is also no definitive evidence that it does not, so doctors typically like to know if a patient is pregnant before going into an MRI (Alorainy et al., 2006). Lastly, people who are claustrophobic and/or sensitive to sound would feel uncomfortable in the MRI. The patient has to lie down and stay as still as possible for about an hour while the scan is being done, and the MRI machine is a relatively small enclosed space. Sometimes the patient has to be sedated or put under anesthesia to be able to get the scan. Additionally, the machine makes a lot of noise, so much so that most patients wear ear protection.
MRI Advancements
In the 21st century, there have been countless advancements to magnetic resonance imaging. An important advancement is the way MRI machines have been developed to make patients more comfortable. New software is allowing MRI scan time to be significantly shortened, which not only helps with any patient discomfort, but also helps doctors find out results quicker. There is also technology for noise reduction in the MRI machine. It is difficult to lie still while the machine is so loud, so having little to no noise while the scan is being done is extremely important. Finally, more and more hospitals have open MRI machines. Open MRI machines not only help patients with claustrophobia, but it also allows any patients whose size or weight would make an MRI scan difficult or impossible (Fornell, 2019).
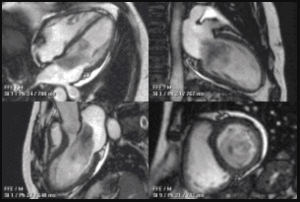
“Myxoma CMR” by Jccmoon is licensed under CC BY 3.0
There have also been advancements in the possibility of lung and cardiac MRIs. Lung MRIs were always difficult to get because there are not many hydrogen atoms in the lungs. Since the misalignment and realignment of the protons in the hydrogen atoms create the imaging, lung scans were usually inaccurate or unclear. In 2015, Toshiba introduced a new technology that allows lung MRIs to be possible and accurate. Cardiac MRIs were always limited due to the complexity, long exam times, and high costs. New technology for cardiac MRIs was announced by GE Healthcare in 2015. It allows a full 3-D chest scan that includes the full motion of the myocardium, blood flow, time, and quantification to create what GE calls a 7-D cardiac MRI exam. The new cardiac MRI also shortened the time from about 70 minutes to about 10 minutes (Fornell, 2019).
Chapter Summary
- There are multiple types of prosthetics, each with different purposes and levels of functionality.
- Neural prosthetics have been increasingly developed in the past 20 years and there are multiple success stories that will change the face of medicine.
- Magnetic resonance imaging (MRI) is used by doctors to create detailed images of organs and tissues.
- There have been many advancements to MRI technology that help with patient comfort and imaging ability.
Review Questions
1. What is the earliest prosthetic found in history?
a. A foot
b. A toe
c. A hand
d. A finger
2. What kind of prosthetic helps restore any lost functionality due to brain damage?
a. Passive
b. Body-powered
c. Myoelectric
d. Neural
3. The magnetic field in an MRI affects which of the following?
a. Protons
b. Electrons
c. Neutrons
d. All of these
4. Why is getting a prosthetic a long, well-thought-out process for amputees?
5. Explain some of the precautions of getting an MRI scan.
Answers
- B, 2. D, 3. A, 4. Can be found in section 26.2 5. Can be found in section 26.4
References
Alorainy, I. A., Albadr, F. B., & Abujamea, A. H. (2006). Attitude towards MRI safety during pregnancy. Annals of Saudi medicine. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6074503/.
Andersen, R. A., Hwang, E. J., & Mulliken, G. H. (2010). Cognitive neural prosthetics. Annual review of psychology. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2849803/.
Bender, E. (2015, September 21). The History of Prosthetics. http://unyq.com/the-history-of-prosthetics/.
Berger, A. (2002, January 5). Magnetic resonance imaging. BMJ (Clinical research ed.). https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1121941/.
Caltech. (2015, May 25). Next Generation of Neuroprosthetics: Science Explained. Youtube. https://www.youtube.com/watch?v=F4wAvlA_Of0
Fornell, D. (2019, August 27). Recent Advances in MRI Technology. Imaging Technology News. https://www.itnonline.com/article/recent-advances-mri-technology.
Lehrman, E. (2015, March 16). Bionic Senses: How Neuroprosthetics Restore Hearing and Sight. Science in the News. http://sitn.hms.harvard.edu/flash/2013/issue138a/.
Lewis, T. (2017, August 12). What is an MRI (Magnetic Resonance Imaging)? LiveScience. https://www.livescience.com/39074-what-is-an-mri.html.
Marcin, J. (2018, July 24). MRI Scans: Definition, uses, and procedure. Medical News Today. https://www.medicalnewstoday.com/articles/146309.
Nevils-Karakeci, R. (2020, May 2). The Basics of Prosthetic Limbs and How They Work. https://interestingengineering.com/the-basics-of-prosthetic-limbs-and-how-they-work.
Prochazka, A., Mushahwar, V. K., & McCreery, D. B. (2001, May 15). Neural prostheses. The Journal of physiology. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2278603/.
University of Michigan Engineering. (2020, March 4). Ultra-precise, mind-controlled prosthetic hand for amputees via RPNI neural interface [Video]. YouTube. https://www.youtube.com/watch?v=PoKcRtDmKJw
UPMC. (2016, October 13). Touched by Science: Paralyzed Man Feels Again Through Mind-Controlled Robotic Arm [Video]. YouTube. https://www.youtube.com/watch?v=L1bO-29FhMU&feature=emb_logo
