6
Learning Objectives
At the end of this chapter, the learner will:
- Conduct a health history pertaining to the respiratory system.
- Identify anatomic landmarks in identifying underlying structures and the location of physical findings.
- Inspect the thorax for pattern of respiration, skin, symmetry, and use of accessory muscles.
- Auscultate the anterior and posterior thorax for normal breath sounds and adventitious sounds.
- Describe the findings using correct terminology.
- Document the findings of the respiratory exam.
I. Overview of the Respiratory System
The assessment of the respiratory system includes assessing the thorax, lungs, ventilatory function and oxygenation of the body. Focused assessment techniques will be applied intensively in this system: inspect level of consciousness, agitation, skin color, clubbing fingers, shortness of breath, use of accessory muscles, position and alignment of the spine; auscultate breathing sounds; palpate position of the trachea, subcutaneous emphysema; percuss to assess the underlying structure of the chest.
II. Anatomy and Physiology
Identifying thoracic landmarks is essential to the systematic examination of the respiratory system. Click the link below to review anatomy and physiology of the respiratory system. You will need to apply your knowledge in the assessment process.
III. Medical Terminology
Important terms to know and understand:
| Adventitious sounds | abnormal breath sounds |
| Apnea | involuntary cessation of breathing |
| Atelectasis | incomplete expansion or collapse of a part of the lungs |
| Bradypnea | slow rate of breathing |
| Cheyne-Stokes Respirations | gradual increase and then gradual decrease in depth of respiration followed a period of apnea |
| Crackles | crackling sounds made as air moves through wet secretions in the lungs |
| Crepitus | a grating sound or sensation under the skin around the lungs, or in the joints |
| Cyanosis | bluish coloring of the skin |
| Dyspnea | difficult or labored breathing |
| Hemoptysis | sputum containing blood |
| Hyperventilation | condition in which there is more than the normal amount of air entering and leaving lungs |
| Hypoventilation | decreased rate or depth of air movement into the lungs |
| Hypoxia | inadequate amount of oxygen available to the cells |
| Nasal Flaring | nostrils widen while breathing indicates difficulty in breathing |
| Orthopnea | shortness of breath when lying flat and relieved by sitting or standing |
| Pneumothorax | air in the pleural space |
| Stridor | harsh, high-pitched sound usually heard on inspiration when upper airway become narrowed |
| Tachypnea | rapid rate of breathing |
| Tripod position or orthopneic position | a person sits or stands leaning forward and supports the upper body with hands on knees or other surface, often adopted by people experiencing respiratory distress |
| Wheezes | high-pitched, musical noise that sounds like a squeak |
IV. Step by Step Assessment
Safety considerations:
- Perform hand hygiene.
- Check room for contact precautions.
- Introduce yourself to patient.
- Confirm patient ID using two patient identifiers (e.g., name and date of birth).
- Explain process to patient.
- Be organized and systematic in your assessment.
- Use appropriate listening and questioning skills.
- Listen and attend to patient cues.
- Ensure patient’s privacy and dignity.
- Apply principles of asepsis and safety.
- Check vital signs.
| Steps | Additional Information |
| 1. Conduct a focused interview related to history of respiratory disease, smoking, and environmental exposures. | Ask relevant questions related to dyspnea, cough/sputum, fever, chills, chest pain with breathing, previous history, treatment, medications, etc. |
2. Inspect:
Note: Click the hyperlink to access more details. Copyrighted materials used with permission of the author, A. Chandrasekhar, Loyola University Medical Education Network. |
Patients in respiratory distress may have an anxious expression, pursed lips, and/or nasal flaring.
The anteroposterior (AP) diameter of the thorax should be approximately 1/2 of the lateral diameter. 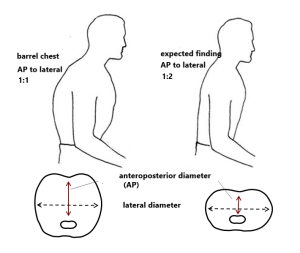 Asymmetrical chest expansion may indicate conditions such as pneumothorax, rib fracture, severe pneumonia, or atelectasis. With hypoxemia, cyanosis of the extremities or around the mouth may be noted. |
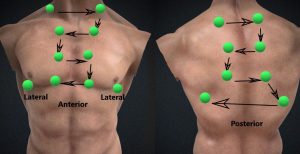
3. Auscultate lungs for breath sounds and adventitious sounds.
|
Fine crackles (rales) may indicate asthma and chronic obstructive pulmonary disease (COPD).
Coarse crackles may indicate pulmonary edema. Wheezing may indicate asthma, bronchitis, or emphysema. Low-pitched wheezing (rhonchi) may indicate pneumonia. Pleural friction rub (creaking) may indicate pleurisy. Interventions should be provided if decrease or absence of breath sounds is noted. It may indicate severe respiratory problems such as airway obstruction, pneumonia, pneumothorax, pleural effusion, or atelectasis (Reyes et al., 2020). |
| 4. Report and document assessment findings and related health problems according to agency policy. | Accurate and timely documentation and reporting promote patient safety. |
A more detailed overview of respiratory examination is available at: Lung Exam (text) and Respiratory Sounds (text and video)
Knowledge Check
[h5p id=”43″]
V. Documentation of Assessment Findings
A sample narrative documentation:
A & O x 4, denies shortness of breath or chest pain, RR18, without use of accessory muscles, symmetrical chest wall movement, clear breath sounds in all lung fields, O2 98% in room air.
VI. Related Laboratory and Diagnostic Procedures/ Findings
A spirometry test (pulmonary function test), have the patient inhale and exhale through a device to check the lung capacity. It can be used to diagnose asthma and chronic obstructive pulmonary disease. A chest X-ray is used to view the structure inside of the chest and is a useful test to diagnose pneumonia. A computerized tomography (CT) scan may also be used to identify respiratory problems that an X-ray cannot detect. Bronchoscopy is an invasive procedure that a fiberscope is inserted into the patient’s airway to examine bronchi. It can be used to retrieve tissues in the airway (biopsy) to diagnose lung cancer or to treat airway blockage or obstruction due to foreign objects.
VII. Learning Exercises
 [h5p id=”49″]
[h5p id=”49″]VIII. Attributions and References
- Anderson, R., Doyle, G. R., & McCutcheon, J. A. Clinical procedures for safer patient care. https://pressbooks.bccampus.ca/clinicalproceduresforsaferpatientcaretrubscn/chapter/2-7-head-to-toe-assessment-chest-respiratory-assessment/ Accessed July 4th, 2021.
- Deviant Art: Male torso render image by Illtrytobeapro. Oct. 7, 2013. ODI: https://www.deviantart.com/illtrytobeapro/art/Male-Torso-render-405887318 Accessed July 4th, 2021.
- Doyle, G. R. & McCutcheon, J. A. Step by Step Checklist adapted from https://opentextbc.ca/clinicalskills/chapter/2-5-focussed-respiratory-assessment/
- Khan Academy: Meet the lungs by Rishi Desai. https://www.khanacademy.org/science/high-school-biology/hs-human-body-systems/hs-the-circulatory-and-respiratory-systems/v/meet-the-lungs
- Reyes, F.M. Modi, P., & Le, J.K. (Updated July 10, 2020). Lung Exam. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan. DOI: https://www.ncbi.nlm.nih.gov/books/NBK459253/ Accessed July 5th, 2021.
- Wikipedia contributors. (2019, July 30). Respiratory sounds. In Wikipedia, The Free Encyclopedia. Retrieved 23:46, August 29, 2019, from https://en.wikipedia.org/w/index.php?title=Respiratory_sounds&oldid=908541418
- Wikimedia Commons. Barrel chest adapted from DOI: https://commons.wikimedia.org/wiki/File:%CE%92%CF%85%CF%84%CE%B9%CE%BF%CE%B5%CE%B9%CE%B4%CE%AE%CF%82_%CE%B8%CF%8E%CF%81%CE%B1%CE%BA%CE%B1%CF%82_(barrel_chest).png
