10
Learning Objectives
At the end of this chapter, the learner will:
- Obtain the health history of the neurological system.
- Assess the neurological system of the patient including the cranial nerves, sensory function, pain, temperature, and position sense of a patient.
- Document findings of the neurological exam.
I. Overview of the Neurological System
The assessment of the neurological system include examinations of mental status, level of consciousness and examinations of the neurological function. While details of the mental status assessment will be described in the next chapter, this chapter will begin with a review of the 12 pairs of cranial nerves and their functions. It will follow by a collection of some important terminologies of this system, and then continue with key assessment components for the system.
II. Anatomy and Physiology
Click the link below to review anatomy and physiology of the neurological system. In the assessment process, you will need to apply your knowledge of the 12 pairs of cranial nerves and their functions to the neurological system.
A more detailed review of neurological system is available at the link:
III. Medical Terminology
The following are commonly used medical terminologies in the assessment of neurological system.
| Affect | observable behaviors that indicate a person’s feelings or emotions |
| Anxiety | a feeling of uneasiness or discomfort experienced in varying degree |
| Apathy | lack of emotional expression; indifference to stimuli or surroundings |
| Aphasia | a neurological condition in which language function is absent or impaired |
| Cognitive functioning | an intellectual process by which one becomes aware of, perceives, or comprehends ideas |
| Coherency | conversation and behavior that conveys thoughts and feelings in a logical and relevant manner |
| Cerebrovascular Accident (CVA) | a stroke; a blockage or the rupture of a blood vessel in the brain |
| Delirium | a temporary state of confusion |
| Depression | a mood disorder characterized by low mood, a feeling of sadness, and a general loss of interest in things |
| Dementia | impairment of intellectual functioning, memory, and judgment |
| Dysarthria | speech disorder involving difficulty with articulating and pronunciation of specific sounds |
| Dysphagia |
difficulty in swallowing |
| Dysphasia | difficulty with speech |
| Encephalitis | inflammation of the brain |
| Hyperesthesia | abnormally increased sensitivity to sensory stimuli such as touch or pain |
| Labile emotions | unpredictable, rapid shifting of expression of feelings |
| Paralysis | loss of muscle function and or sensation secondary to nervous impairment |
| Paraplegia | a form of paralysis that affects in the lower half of the body |
| Paresis | impaired muscle strength or weakness |
| Paresthesia | abnormal sensation such as numbness, tingling, or burning |
| Quadriplegia | a form of paralysis that affects all four extremities |
| Transient Ischemic Attack (TIA) | A neurological event with the signs and symptoms of a stroke, but which go away within a short period of time |
| Temporomandibular joint (TMJ) | the hinge joint between the temporal bone and the lower jaw |
Terms to Classify Altered Level of Consciousness
| Consciousness | normal |
| Confusion | disoriented; impaired thinking and difficulty following commands |
| Delirium | a temporary state of confusion; restlessness, hallucination, sometimes delusions |
| Lethargy/Somnolence | a state of severe drowsiness can be aroused by moderate stimuli |
| Obtundation | decreased alertness, slowed psychomotor responses; similar to lethargy |
| Stupor | responds only to intense and repeated stimuli; almost unconscious |
| Coma | a profound or deep state of unconsciousness; may lack a gag reflex or a pupillary response |
*Use Glasgow Coma Scale (GCS) to objectively assess the extent of impaired consciousness. GCS is described later in this chapter.
IV. Step by Step Assessment
- Perform hand hygiene.
- Check room for contact precautions.
- Introduce yourself to patient.
- Confirm patient ID using two patient identifiers (e.g., name and date of birth).
- Explain process to patient.
- Assemble equipment prior to starting exam.
- Be organized and systematic in your assessment.
- Use appropriate listening and questioning skills.
- Listen and attend to patient cues.
- Ensure patient’s privacy and dignity.
- Apply principles of asepsis and safety.
- Check vital signs.
| Steps | Additional Information |
|
Ask relevant questions related to past or recent history of head injury, neurological illness, or symptoms, confusion, headache, vertigo, seizures, recent injury or fall, weakness, numbness, tingling, difficulty swallowing (dysphagia) or speaking (dysphasia), and lack of coordination of body movements. |
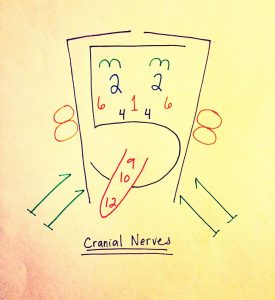
| 3. Assess 12 cranial nerve functions.
(See chart below for more details). |
CNI – Assess smell
CNII- Assess visual acuity by using Snellen chart. Normal vision is 20/20. The top number indicates the distance of the patient can see, and the bottom number indicates what a person with normal vision can see. 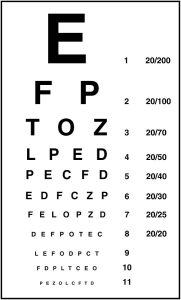
CNIII/IV/VI – assess extraocular eye movements with 6 cardinal directions of gaze. Ask the patient to keep the head still and only move eyes. Follow the examiner’s finger or an object to move in 6 directions. 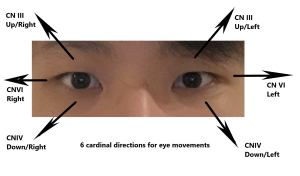
 CN V – assess jaw clench and sharp/dull sensation over three branches (forehead, cheek, and chin) bilaterally. CN VII – ask the patient to raise eyebrows, smile, puff out cheeks, show teeth, squeeze eyes shut. CN VIII – assess hearing by whispering or by lightly rubbing the examiner’s fingers next to ear. CN IX /CN X – assess swallow, and check movement of soft palate and gag reflex. CN XI – assess motor function of the spinal accessory nerve by asking the patient to shrug shoulders while the examiner applies pressure. Trapezius muscles should be strong and symmetric. CN XII – assessing tongue movement |
4. Assess motor strength and sensation.
|
Unequal motor strength and unusual sensation may indicate underlying neurological disease or injury, such as stroke or head injury.
   Expected findings should be equal strength bilaterally, no pain/numbness/tingling sensation. |
| 5. Report and document assessment findings and related health problems according to agency policy. | Accurate and timely documentation and reporting promote patient safety. |
Knowledge Check
[h5p id=”29″]
Assess 12 Cranial Nerve Functions
Click all hyperlinks to access more details.
| Mnemonic | # | Name | Function (Sensory/Motor/Both) | Assessment |
| On | I | Olfactory | Smell (S) | |
| Old | II | Optic | Vision (S) | Visual acuity Visual field |
| Olympus’ | III | Oculomotor | Eye movements (M) |
Eye movements (CN III, IV, VI) |
| Towering | IV | Trochlear | Eye movements (M) | |
| Tops | V | Trigeminal | Sensory/motor – face (B) | Facial movement and sensation |
| A | VI | Abducens | Eye movements (M) | |
| Finn | VII | Facial | Motor – face, taste (B) | Facial motor function |
| And | VIII | Auditory (Vestibulocochlear) | Hearing/balance (S) | Hearing |
| German | IX | Glossopharyngeal | Motor – throat, taste (B) | Movement of the soft palate and gag reflex
(CNIX and X) |
| Viewed | X | Vagus | Motor/sensory – viscera (autonomic) (B) | |
| Some | XI | Spinal Accessory | Motor – head and neck (M) | Shrug shoulder |
| Hops | XII | Hypoglossal | Motor – lower throat (M) | Tongue |
Copyrighted materials used with permission of the author, A. Chandrasekhar, Loyola University Medical Education Network.
Table adapted from Biga et al. Anatomy & Physiology. https://open.oregonstate.education/aandp/chapter/13-3-spinal-and-cranial-nerves/
Watch the cranial nerve assessment video below. In this video, the examiner uses ophthalmoscope to check the fundus of the eye (optic disc) which bedside nurses normally do not perform during head to toe or shift assessment.
Knowledge Check
[h5p id=”30″]
Glasgow Coma Scale (GCS) Assessment
Glasgow Coma Scale is a scale to assess the level of consciousness of patients who have an acute brain injury or trauma in emergency situations. It contains assessment of three components: eye, verbal and motor responses. A fully awake person has the highest score of 15 and a person in deep coma receives the lowest score of 3.
| Response | Scale/Score |
|
Best eye-opening response Record “C” if eyes closed due to swelling. |
Spontaneously (4)
To speech (3) To pain (2) No response (1) |
| Best motor response (to painful stimuli)
Press at fingernail bed and record best upper-limb response. |
Obeys verbal command (6)
Localizes pain (5) Flexion – withdrawal (4) Flexion – abnormal (3) Extension – abnormal (2) No response (1) |
| Best verbal response
Record “E” if endotracheal tube is in place, and “T” if tracheostomy is in place. |
Oriented x 3 (to person, time, and place) (5)
Conversation – confused (4) Speech – inappropriate (3) Sounds – incomprehensible (2) No response (1) |
- Click the link to get a more detailed overview of GCS: Glasgow Coma Scale
V. Documentation
A sample narrative documentation:
Alert and oriented (x4) to situation, person, place, and time. Behavior appropriate to situation and developmental age. Clear speech and follow verbal commands. Cranial nerves II to XII grossly intact. Pupils Equal, Round, React to Light and Accommodation (PERRLA). Active range of motion all extremities with symmetry strength. Peripheral sensation intact.
VI. Related Laboratory and Diagnostic Procedures/Findings
Depending on the patient’s signs and symptoms from physical examination, some diagnostic tests could be performed. For example, lumbar puncture (spinal tap) is to collect a sample of the patient’s spinal fluids to check if the patient has an infection in the brain or spinal cord or cancer in the brain. Imaging study such as magnetic resonance imaging (MRI) or computed tomography (CT) scan to diagnose a specific neurological disorder. Electroencephalogram (EEG) measures electrical activity in the brain that can be used to diagnose seizures, psychiatric disorders and other conditions of the brain.
A more detailed overview of different neurological diagnostic tests is available at: Neurological Diagnostic Tests and Procedures
VII. Learning Exercise
VIII. Attributions and References
- Biga, L. M., Dawson, S., Harwell, A., Hopkins, R., Kaufmann, J., LeMaster, M., Matern, P., Morrison-Graham, K., Quick, D., & Runyeon, J. Anatomy & Physiology. http://library.open.oregonstate.edu/aandp/chapter/13-3-spinal-and-cranial-nerves/#tbl-ch13_03
- Chandrasekhar, A. (March 28, 2006 updated). Screening Physical Exam. http://www.meddean.luc.edu/lumen/MedEd/medicine/pulmonar/pd/contents.htm
- Doyle, G. R. & McCutcheon, J. A. Clinical Procedure for Safer Patient Care. https://opentextbc.ca/clinicalskills/chapter/2-5-focussed-respiratory-assessment/
- Hacking, C. & Gaillard, F. Radiopaedia.org. https://radiopaedia.org/articles/olfactory-nerve?lang=us. Accessed July 20, 2019.
- Michael Gibson, C., Bahekar, P., & Sharfaei, S. WikiDoc: Glasgow coma scale. https://www.wikidoc.org/index.php/Glasgow_coma_scale. Accessed July 20, 2019.
- National Institute of Neurological Disorders and Stroke. https://www.ninds.nih.gov/Disorders/Patient-Caregiver-Education/Fact-Sheets/Neurological-Diagnostic-Tests-and-Procedures-Fact. Accessed July 20, 2019.
- Orlando, G. (2006). Animation that illustrates the pupillary light reflex. Public domain via Wikimedia Commons. https://commons.wikimedia.org/wiki/File:Eye_dilate.gif
- Psychology Wiki https://psychology.wikia.org/wiki/Level_of_consciousness. Accessed 7/16/2021
