15 Ankle Sprain
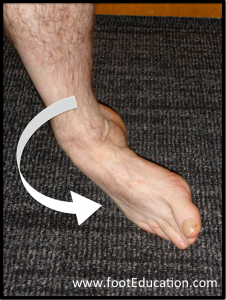
Ankle sprains are among the most common musculoskeletal injuries. Patients typically describe an episode where they “roll their ankle” to one side (often inward, a so called “inversion” sprain (Figure 1) and thereby tear the ligaments on the outside (lateral) ankle. This is contrasted with a less common “eversion” sprain where the foot rolls to the outside and the medial (deltoid) ligament is torn. Patients with sprained ankles can have significant pain and swelling. There is usually a limp, but unlike an ankle fracture, a sprained ankle will usually tolerate some weight-bearing but, in severe cases, not for 7 to 10 days. Although the phrase “it’s just a sprain” may suggest that this is always a minor injury, ankle sprains can in rare cases lead to significant impairment. Expeditious treatment – directed at limiting swelling and regaining motion – helps ensure the best possible recovery.
Structure and function
The ankle joint comprises the articulation of the tibia and fibula with the talus. However, the ligamentous constraints of the ankle also span the subtalar and talonavicular joints as well. The tibia and fibula are held together by the tibiofibular ligaments (anterior and posterior) and interosseous membrane, collectively known as the syndesmotic ligaments. These two bones form a mortise (inverted “U”) into which the talus fits (Figure 2).
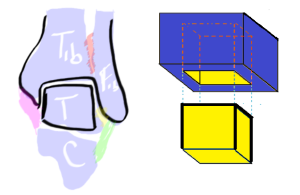
The talus, in turn, acts as a “universal joint” that is connected to the calcaneus, forming the subtalar joint.
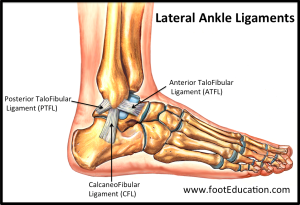
In addition to the syndesmotic ligaments, the ankle joint is stabilized, on the lateral side by the anterior and posterior talo-fibular ligaments and the calcaneofibular ligament, together referred to as the lateral collateral ligaments (Figure 3).
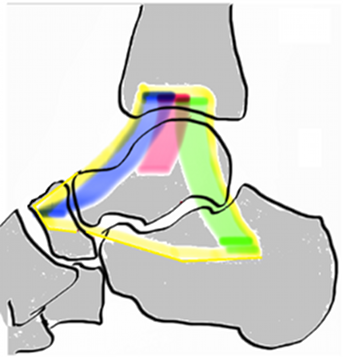
With its three parts, the deltoid ligament serves as the medial constraint of the ankle (Figure 4). The length and tension on these ligaments are vital to their role in the regulation of the coupled motion that occurs between the tibia, talus, calcaneus and navicular. The deeper branch of the ligament is securely fastened in the talus, while the more superficial, broader aspect runs into the calcaneus and navicular. Like the anterior talo-fibular ligament, the deltoid is rarely torn completely but rather becomes stretched (deformed) when stressed.
The anterior talo-fibular ligament (ATFL) is the ankle ligament most often sprained. The ATFL courses from the fibula to the neck of the talus and stabilizes the ankle joint against anterior translation. Inversion of the ankle is resisted by a combination of the ATFL and calcaneo-fibular ligament. The ATFL itself is not a distinct ligament but, rather a thickening of the lateral joint capsule. When it is sprained, the associated interstitial tearing may result in lengthening. This stretching may lead to symptomatic ankle instability.
The calcaneo-fibular ligament (CFL) originates at the tip of the fibula and courses distal and posterior inserting into the calcaneus. Unlike the ATFL, the CFL is a distinct ligamentous structure.
The posterior talo-fibular ligament (PTFL) originates from posterior margin of the fibula and inserts into the posterior talus. The PTFL stabilizes the ankle joint and the subtalar joint. Injuries to the PTFL are rare, unless there is an ankle dislocation or marked subluxation.
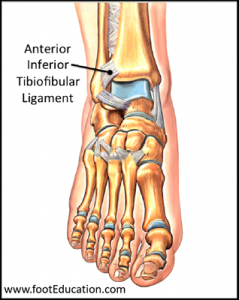
The anterior inferior tibio-fibular ligament is the one injured in a so-called “high ankle sprain.” This ligament is positioned on the anterolateral aspect of the ankle and helps stabilize the mortise (Figure 5). Injuries to this ligament occur when the foot is stuck on the ground and rotates externally. A high ankle sprain can heal with irritating scar formation (hypertrophy–a condition known as anterior-lateral ankle impingement.
The interosseous membrane is composed of strong fibrous tissue that runs between and connects the tibia and fibula. The interosseous membrane along with the anterior or posterior syndesmotic ligaments can be torn in certain patterns of ankle fractures, in which the tibia and fibula spread apart, a so-called diastasis rendering the ankle unstable.
Collectively, the tibio-fibular ligament and the interosseous membrane are called the syndesmosis.
Patient Presentation
Ankle Sprains
Patients with ankle sprains typically describe a twisting episode where they invert (or less often, evert) their ankle. Pain, swelling and difficulty ambulating are common.
A sprained ankle may often have associated redness due to the increased blood flow to this area (Figure 6). Without a history of an injury, this skin appearance may suggest cellulitis (infection of the skin). Physical examination of the acutely injured ankle will reveal swelling over the outer aspect of the ankle. There will be tenderness over the outer front (anterolateral) aspect of the ankle.

It is important to palpate the base of the anterior process of the calcaneus, the 5th metatarsal, the navicular and the Lisfranc joint for tenderness, as the same mechanism that creates an ankle sprain can lead to other injuries there as well.
As swelling and pain decreases, during the recovery period it may be possible to assess for ankle instability. Laxity of the ATFL is assessed with an anterior drawer maneuver (Figure 7). Integrity of the calcaneofibular ligament is assessed by inverting the foot while palpating the lateral talar dome. Either or both of these tests can be obscured by guarding due to pain. The anterior draw test is performed on both the injured and uninjured side to obtain comparison. The examiner assesses the amount of translation of the foot relative to the shin and also the “quality of the end point” (i.e., if a firm stop –a rope snapping to attention–is encountered).
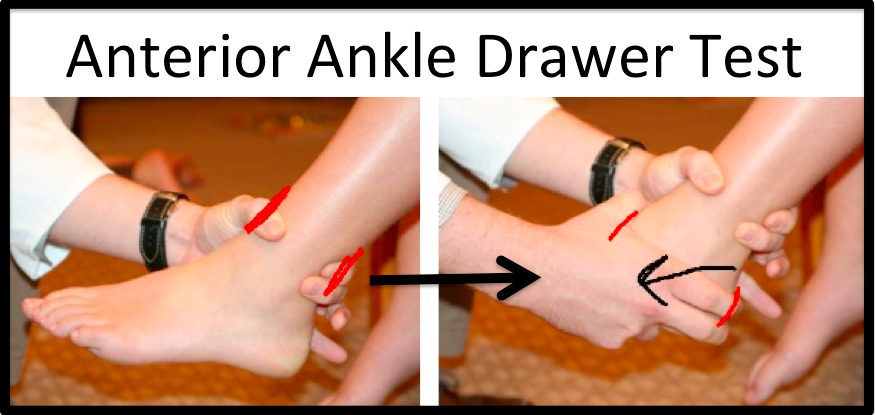
The anterior ankle drawer test is performed with the patient sitting on an exam table, with knees flexed and the foot dangling over the edge of the table. The examiner grasps and stabilizes the shin in one hand and applies anteromedial force to the heel with the other hand, using the deltoid ligament as a hinge.
High Ankle Sprains
So-called “high ankle sprains” are injuries to the syndesmosis, which lies between the tibia and fibula (“high”) above the joint.
High ankle sprains are less common than lateral ankle sprains, but when they occur they are often more debilitating. They occur from a twisting injury to the ankle when the foot is planted on the ground. These injuries are produced by a sudden change of direction due to an externally applied force, as may be seen from a tackle in a football game. Pain located on the anterolateral aspect of the ankle is the main symptom. However, a high ankle sprain can also occur in combination with an inversion or eversion injury and therefore medial or lateral pain can be present as well.
The “squeeze test,” namely compressing (squeezing) the tibia and fibula together approximately four inches above the ankle joint, can be used to detect a high ankle sprain. This test will tend to reproduce focal symptoms in patients who have had a high ankle sprain. The external rotation test, namely, holding the foot in dorsiflexion and then externally rotating it, will also reproduce focal symptoms when high ankle sprain is present.
Objective evidence
X-rays should be obtained if there is bony tenderness on the posterior aspect of either malleoli or an inability to bear weight (Ottawa Ankle Rules). The x-rays should include the foot if there is tenderness on either the anterior process of the calcaneus, 5th metatarsal or the navicular. X-rays of the knee joint are needed if an isolated medial malleolus is detected on the initial film or if there is widening of the mortise (proximal fibular fracture can occur in combination with ankle injuries and must be ruled out).
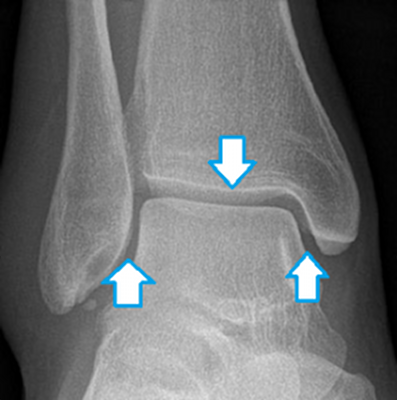
X-rays must be examined to exclude not only fracture but diastasis, namely, an increased distance between the tibia and fibula implying damage to the syndesmosis.
Particular attention should be paid to ensure that the ankle joint mortise is symmetrical: the space between the talus and tibia medially should match the space laterally (Figure 8).
Stress x-rays – imaging the ankle while the heel is pushed towards one side while the leg is pushed in the opposite direction – may be used to assess instability in chronic cases. These films should be used only with great caution in the acute setting as the procedure may displace otherwise non-displaced injuries.
There is typically no role for MRI in acute ankle sprains. An MRI may be indicated in cases of chronic pain after a sprain. An MRI could detect a talar osteochondral injury or extra-articular sources of residual pain such as tendonitis or scarring of the restraining ligaments. Approximately 10% of severe ankle sprains may have associated injuries to the articular surface of the talus. An MRI may also be helpful in identifying an injury to the syndesmosis.
Epidemiology
According to Waterman et al (PMID: 20926721), emergency department data suggest an incidence rate of 2.15 ankle sprain per 1000 person/year in the United States, with a peak incidence rate more than triple that for teenagers between fifteen and nineteen years of age. The overall incidence rate by gender is about the same, though younger males and older females have higher rates than their female and male counterparts respectively. Nearly half of all ankle sprains seen were related to athletic activity.
Differential diagnosis
The key element in the differential diagnosis of an acute ankle injury is discerning what was injured: which bones may have been broken and which ligaments may have been sprained. Note that combination injuries are not only possible but are common.
Bony tenderness on the anterior process of the calcaneus, base of the 5th metatarsal, or navicular suggests a fracture there.
Tenderness coursing up the lateral aspect of the leg may suggest a peroneal tendon injury.
The squeeze test and external rotation test may detect a high ankle sprain (anterior inferior tibia-fibular ligament injury).
Once the diagnosis of an ankle sprain is made, it can be further refined into a grade:
- Grade 1 sprain: the anterior talofibular ligament is injured but not elongated (and thus not prone to cause instability);
- Grade 2 sprain: the anterior talofibular ligament is partially torn resulting in stretching that may destabilize the joint; and
- Grade 3 sprain: a complete tear of the anterior talofibular ligament. Note that instability may be masked by swelling or guarding.
Red flags
An inability to bear weight or tenderness in the bone (including the medial and lateral malleoli as well as the 5th metatarsal and navicular) signify a need for radiographs (as per the Ottawa Ankle Rules).
Blood on the skin suggests an open fracture.
Treatment options and outcomes
The initial treatment of an ankle sprain is known by the mnemonic RICE. RICE is used to limit swelling, as too much swelling can significantly increase the patient’s pain and ultimate recovery time.
- Rest: minimize mobilization and activity in the initial recovery period.
- Ice: Apply ice, but not continuously. A regimen of 10 minutes on and 10 minutes off will minimize the risk of thermal injury to the skin.
- Compression: This should be tight enough to decrease swelling but loose enough to allow the foot to be perfused.
- Elevation: To be maximally effective, the foot should be held higher than the thigh, to allow gravity to help drain the edema. Propping the foot in a stool or pillow is not apt to help drain fluid, but may help enforce rest and inactivity.
Non-Steroidal Anti-Inflammatory Drugs (NSAIDs) such as ibuprofen can be very helpful to decrease pain by decreasing the inflammatory response to the injury. However, there is some evidence that suggest that anti-inflammatories may have an adverse effect on ligament healing.
Once the symptoms associated with the initial ankle sprain have started to improve, patients will benefit from physical therapy exercises designed to improve their range of motion, strength and proprioception.
Proprioception is the ability of the brain to sense the position of a joint (ex. ankle) and control its movement relative to the rest of the body. Note that nerves within the ligament mediate proprioception and therefore this sense can be out of kilter following a ligament injury. As the acuity of the injury resolves, patients with seemingly normal ankles on examination (no swelling, no tenderness, no laxity) may still feel unstable if proprioception has not returned to normal. This is referred to as “functional instability.”
“Figure of Eight” exercises are particularly helpful for regaining range of motion and proprioception. Patients should be instructed to imagine that the tip of their big toe is a pen and to then “draw” a figure of eight with the toe slowly, repeating the motion for 30-60 seconds. In the alternatives, patients can “sign” their names in script. It is important that the motion follow a deliberate pattern – and not random waving of the foot – as deliberate motion helps improve proprioception as well.
Proprioception can also be improved by having the patient stand on one foot with eyes closed. Once this is mastered, standing on one foot on a soft surface (such as a pillow or bed) with eyes closed and head moving side to side can further improve proprioception.
Rehabilitation after an ankle sprain can often be completed with a home program, though trained physical therapists may be beneficial in providing initial instruction defining the program.
Surgery is rarely indicated for the treatment of acute ankle sprains. However, patients who have recurrent ankle sprains may be candidates for an ankle ligament stabilization procedure to treat their anatomic instability and restore functional stability.
Most people with sprained ankles fully recover. Even if the ligaments are permanently deformed, the muscles crossing the ankle joint can provide sufficient dynamic stability. However, because ankle sprains are such a common injuries, even a low rate of complications (coupled with a high incidence) may produce a significant number of people with poor outcomes. Ankle injuries associated with chronic anatomic instability may lead to the development of traumatic arthritis.
Risk factors and prevention
Risk factors for ankle sprains include a high arched foot (cavus foot), ligamentous laxity leading to increased inversion, participating in high risk activities (ex. basketball, soccer, volleyball), and a history of previous ankle sprains.
Rovere et al (PMID: 3132864) studied the effectiveness of taping, wearing a laced stabilizer and high-top or low-top shoes among collegiate football for 6 seasons. They reported that the combination associated with the fewest injuries overall was low-top shoes and laced ankle stabilizers.
Miscellany
Ankle sprains from playing basketball represent nearly 20% of all ankle sprains in the US. Football and soccer are the next most implicated sports causing ankle sprains during athletics.
Key terms
Ankle sprain, syndesmosis, mortise, talo-fibular ligament, calcaneo-fibular ligament, deltoid ligament, proprioception
Skills
Recognize an ankle sprain and differentiate between it and other ankle and hindfoot injuries. Apply the Ottawa ankle rules to recognize need for x-rays.
