18 Hindfoot Fractures
Structure and function
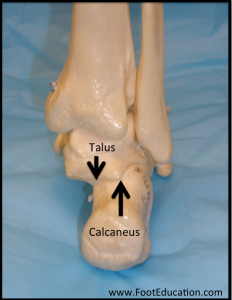
The hindfoot begins at the talocrural (ankle) joint and ends at the calcaneocuboid joint (Figure 1). The bones of the hindfoot are the talus (lower bone of the ankle joint) and the calcaneus (heel bone). The articulation between the talus and calcaneus is called the subtalar joint. The talus does not sit directly on top of the center of the calcaneus, but rather toward the medial-superior edge of the calcaneus (Figure 2).
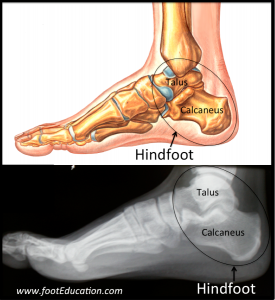
The hindfoot functions to bear and distribute weight to the foot while standing, and to permit complex foot movements in coordination with the ankle joint, especially inversion/eversion and axial rotation.
The talus has a complex architecture, enabling it to function as a “ball-joint” between the leg and the foot. The talus can be divided into three anatomical regions: the head, neck, and body (Figure 3). The head articulates with the navicular anteriorly (talonavicular joint). The neck connects the body and head and is the most commonly fractured part of the talus.
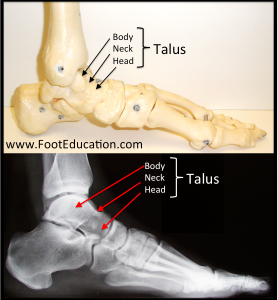
The vascular supply to the body enters at the neck. As such, a fracture of the talar neck may impede perfusion of the talar body. Without perfusion, the bone may die (ie, undergo avascular necrosis). The talar body articulates with the calcaneus inferiorly (subtalar joint) at three separate articular surfaces: anterior, middle, and posterior. There is a small space between these three articulations known as the tarsal sinus.
Motions near the hindfoot include plantarflexion/dorsiflexion at the ankle joint. There is a complex set of motions as the foot moves under the talus at the subtalar and talonavicualr joints. The main elements of this motion is pronation/supination at the subtalar joint; and dorsiflexion and eversion at the talonavicular joint.
Nearly 70% of the talus is covered by articular cartilage. Unlike the calcaneus, which has many insertions and origins of muscles, the talus does not have any muscular attachments. The blood supply to the bone is therefore limited to a “vascular sling” around the talar neck comprising the artery of the tarsal canal (a branch of the posterior tibial artery that supplies the body) and the artery of the tarsal sinus (supplied by branches of the anterior tibial and peroneal arteries to supply the head and neck). This limited blood supply makes the talus prone to delayed healing and avascular necrosis.
The os trigonum is an accessory bone that develops posterior to the talus (Figure 4). It is present in 2.5-14% of people and is bilateral in 60% of these people. For those unfamiliar with this anatomic variation it can be mistaken on x-ray as a fracture of the posterior talus.

The calcaneus articulates with the cuboid anteriorly, but its major articulation is with the talus above it. The calcaneus has three anatomic regions: the anterior process, the body, and the posterior tuberosity. The Achilles tendon inserts at the calcaneal tuberosity on the posterior side of the calcaneus. Near the medial talar articulation is the sustentaculum tali (a horizontal shelf of bone). The calcaneus is likened to a “hard-boiled egg” because its outer cortex is thin and surrounds the softer inner cancellous bone. If damaged, the outer cortex can collapse leading to severe comminution of the underlying cancellous bone.
Patient presentation
Patients with a traumatic fracture involving the hindfoot (talus and/or calcaneus) will have a history of an acute injury. Commonly the injury mechanism is an axial load such as occurs in a fall from a height or a motor vehicle accident. Patients will present with significant swelling and pain. It can be difficult to distinguish a fracture from a sprain with an acutely swollen ankle. A laceration, blood, or puncture wound, often on the medial aspect of the foot, is indicative of an open fracture.
Inability to bear weight is a common sign of hindfoot fractures. Redness, hematoma, and fracture blisters may be present near the heel. Fracture blisters occur when excessive swelling causes the layers of the skin to shear leading to localized blisters. A “Mondor sign” is a hematoma extending distally along the sole of the foot – it is a common finding in patients with a calcaneus fracture (Figure 5).
Hindfoot fractures are often accompanied by other injuries because the extent of axial loading necessary to cause a hindfoot fracture is likely to cause other problems too. Fractures and dislocations of the ankle joint may occur in these settings. Additionally, lumbar spine fractures are seen in 10% of patients with calcaneus fractures.
It is important to assess soft tissue damage in addition to the fracture, as the extent of soft tissue damage will dictate the timing of definitive treatment as well as the prognosis. A comprehensive neurological exam should be performed to look for motor or sensory nerve injury. Anterior and posterior tibial pulses and distal capillary refill should be examined via palpation and/or Doppler to assess for any vascular deficits.

Objective Evidence
Talar Fractures
The presence and location of talar fractures should be evident on plain films, but the talus may be obscured by the ankle mortise, calcaneus, and midfoot.
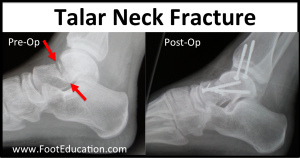
Talar neck fractures, caused by excessive dorsiflexion of the foot against the distal tibia, comprise half of all talus fractures (Figure 6). They are classified, with increasing severity, as nondisplaced; displaced but with an intact ankle joint; and displaced with subluxation/dislocation of both the subtalar joint and ankles joints. A fourth category is designated in there is disruption of the talonavicular joint as well.
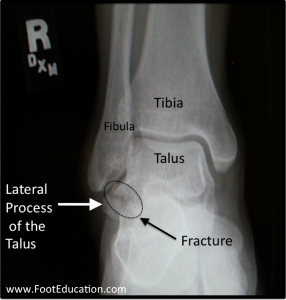
The second most common site of talus fracture is the lateral process – approximately one-quarter of talus fractures occur here (Figure 7). These often occur following axial compression, dorsiflexion, and eversion. They are common in snowboarders.
Fractures of the talar head, body, and posterior process are less common.
Calcaneal Fractures
Calcaneus fractures are more common than talus fractures. They are broadly classified according to whether they involve the subtalar articular surface (intra-articular) or not (extra-articular).
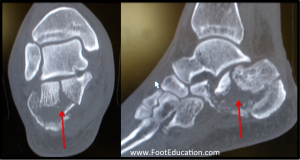
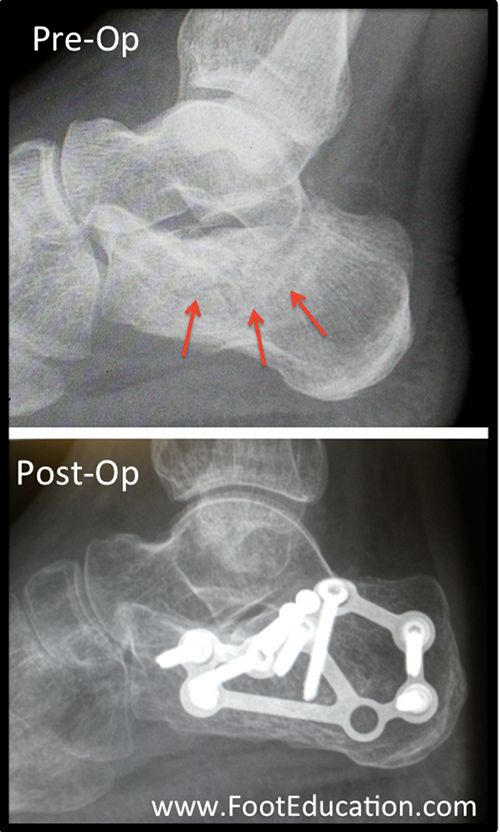
Extra-articular fractures represent only 25% of calcaneal fractures. By definition, they do not involve the subtalar joint or its articular surfaces. Extra-articular fractures typically affect the anterior process, calcaneal tuberosity, calcaneal body, and sustentaculum. Intra-articular fractures are more common (Figure 8). They are also more challenging to treat.
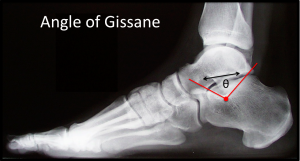
An ankle (anterior-posterior, mortise, and lateral) and foot (AP, oblique, and lateral) x-rays series should be taken. Two angles on the lateral x-ray can be helpful in assessing calcaneus fractures. Bohler’s angle is formed from two lines: (1) a line drawn from the superior point of the posterior calcaneal tuberosity to the highest midpoint of the posterior articular facet, and (2) the highest midpoint of the posterior articular facet to the anterior process (Figure 8). This angle should be 20-40 degrees – a decrease in Bohler’s angle suggests a depressed fracture of the posterior facet. The Angle of Gissane (Figure 9)is formed from the downward slope of the posterior facet and the upward slope directed anteriorly. This angle should be 100-130 degrees – an increase suggests a fracture of the posterior subtalar articular surface.
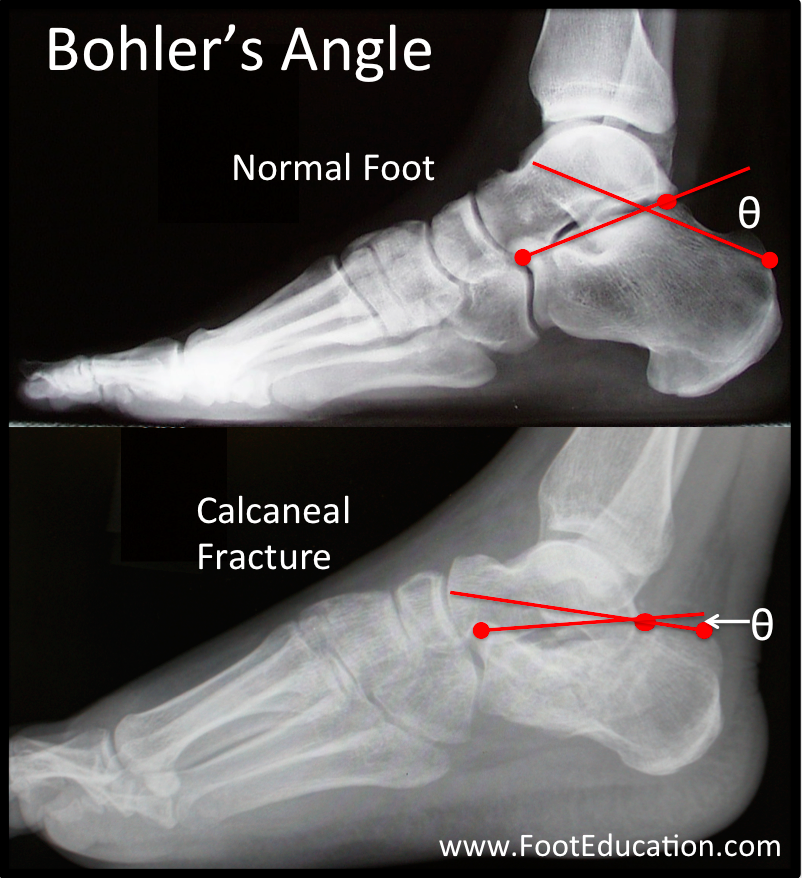
A depressed calcaneal fracture leads to a lower Bohler’s angle (<20 degrees)
“Hawkins sign,” namely a radiolucent line in the subchondral talus (patchy subchondral osteopenia) several weeks following injury on the AP or mortise views of the ankle, is a radiographic indicator of revascularization and absence of avascular necrosis. The radiolucency is the result of bone resorption and is a good sign – it indicates that the bone retained its blood supply.
CT imaging is routinely performed to assess the fracture pattern, degree of displacement, and involvement of articular surfaces since radiographic imaging does not provide sufficient resolution to visualize the articular fragments. Sagittal, coronal, and transverse CT scans are especially helpful for the decisions to perform surgery as well as intra-operative decision-making about technique and needed implants.
MRI is mostly used to detect and quantify the degree of avascular necrosis of talar fractures. It is also used to diagnose osteochondral lesions of the talus.
Epidemiology
Calcaneus fractures comprise 2% of all fractures and 60% of tarsal fractures. The annual incidence is approximately 12 per 100,000 per year, significantly less than ankle fractures (187 per 100,000) which may present similarly. Calcaneus fractures occur 2.4 times more often in males and most often affect men in their 20’s. 72% of calcaneal fractures are due to falls from a height and 19% occur in the workplace. A small minority of calcaneus fractures may be non-traumatic stress fractures due to repetitive axial loading, as seen in military personnel or long-distance runners. Ten percent of calcaneus fractures are bilateral. Ten percent will have associated thoracolumbar spine injuries and another 10% will have a hip fracture.
Talus fractures are the second most common fractured bone in the foot but are rarer than calcaneus fractures, comprising only 0.1-0.9% of all fractures. The most common site of talus fractures is at the talar neck followed by the lateral process. Talus fractures are significant because of their potential for long-term morbidity and complications.
Open fractures occur in approximately 20% of calcaneus and talus fractures.
Differential diagnosis
High-energy impact is necessary to cause hindfoot fractures and this may cause other injuries to the lower limb. These associated injuries can include ankle sprains, ankle fractures, talus dislocations, tibial and fibular fractures, pilon fractures, hip fractures, and injuries to the other tarsal and metatarsal bones. In fact, one-quarter of calcaneal fractures are accompanied by other lower limb injuries. A high-energy axial load can also cause injuries outside the lower limb. One of the most common injuries is a thoracolumbar spine fracture, which occurs in 10% of patients with calcaneal fractures.
Red flags
Hindfoot fractures can be missed in patients who have sustained polytraumatic injuries. Thus an axial load mechanism should be a “red flag” suggesting the presence of a hindfoot fracture, and the presence of such a fracture in one limb should prompt close evaluation of the contralateral side (as it may have been subjected to the same axial load) as well as the spine and pelvis.
A missed hindfoot fracture should also be suspected if a diagnosed ankle sprain does not improve with routine treatment. Subtle hindfoot fractures such as a fracture of the anterior process of the calcaneus can be caused by the same inversion mechanism that causes sprains, and therefore can be easily misdiagnosed as ankle sprains.
Tenting of the skin with a fracture is a worrisome sign indicative of potential skin necrosis.
Treatment options and outcomes
Initial treatment of hindfoot fractures should focus on reducing swelling and addressing any open wounds. After the fracture pattern has been identified, definitive treatment can begin.
Definitive treatment for hindfoot fractures can be operative or non-operative depending on the part of the bone fractured, the severity of the fracture, and the patient’s risk factors. Non-operative treatment generally involves relative immobilization and no weight-bearing for 6 to 12 weeks followed by progressive weight-bearing. Gentle early ankle and hindfoot range of motion exercises are an important element of non-operative treatment for calcaneal fractures and other stable hindfoot injuries. An attempt to move the hindfoot relatively early in the recovery period will help minimize residual hindfoot stiffness – although some stiffness is inevitable.
Operative treatment generally involves open reduction and internal fixation (ORIF) followed by immobilization, no weight-bearing, and early ROM exercises. There is a window of opportunity for surgery – long enough after the injury such that there is resolution of swelling, yet not too long that too much soft callus has formed.
The risk of complications of talar neck and body fractures is related to the extent of the displacement, degree of damage to the blood supply, and damage to the articular surfaces. A common complication is avascular necrosis of the talar body due to injury to the vascular sling supplying the talus. The risk of avascular necrosis in talar neck fractures is 10% or less if the fracture is not displaced; the risk is close to 100% if there is disruption of subtalar, ankle and talonavicular joints.
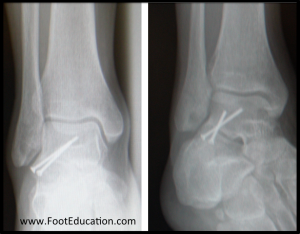
Displaced lateral talar process fractures typically have a better outcome than talar neck and body fractures. They are treated by stabilizing the fracture fragment with screws (Figure 11). If the fractured fragment is small or comminuted, it can be removed.
Extra-articular calcaneus fractures can generally be treated non-operatively unless the fragments are large. In the case of fractures of the calcaneal tuberosity caused by Achilles tendon avulsion, screw fixation may be required to prevent displacement by the force of the Achilles.
Non-displaced calcaneal fractures are treated non-operatively and either non-operative or surgical fixation may be indicated for displaced calcaneal fractures (Figure 12). Effective surgical treatment of a displaced calcaneal fracture is a highly technical procedure. Surgical fixation has not been shown to be superior to non-operative treatment in multiple comparative studies when considering all patients and reviewing all outcomes. The potential benefits of surgery including better range of motion, improved function, and less posttraumatic subtalar arthritis are offset by the higher wound complication and infection rates in the surgically treated patients. It has been shown that surgical fixation has optimal results in young, female patients who are not receiving worker’s compensation. Smokers, diabetics, older patients, patients with vascular disease, and those receiving worker’s compensation tend to do less well.
Risk factors and prevention
Because most hindfoot fractures occur in the setting of acute injury, such as falls or motor vehicle accidents, prevention mostly centers on avoiding such accidents. However, certain health conditions can also predispose people to hindfoot fractures. For example, diabetes mellitus and low bone mineral density are major risk factors for hindfoot fractures.
Hindfoot fractures can also be sports-related. Snowboarders are 17 times more likely to sustain fractures to the lateral process of the talus compared to the general population. Additionally, running with minimalist footwear has been implicated in calcaneal stress fractures.
Miscellany
Calcaneus fractures are called “lover’s fractures” because they are the injury a cheating spouse would sustain if jumping from an upstairs bedroom window to escape trouble.
Talus fractures were historically referred to as “Aviator’s astralgus.” In the early 20th century, plane crashes at sub-lethal speeds were common, resulting in high-impact injuries to the foot including talus fractures. Nowadays talus fractures are mostly caused by falls and motor vehicle accidents, so this term is mostly obsolete.
Key terms
Talus fracture, Calcaneus fracture, Osteonecrosis, Os trigonum, Mondor sign, Hawkins sign, Bohler’s angle, Aviator’s astralgus
Skills
Develop a differential diagnosis of possible foot injuries resulting from high-energy axial loading such as a fall or motor vehicle accident. Recognize the classic signs, symptoms, and history of hindfoot fractures. Identify and differentiate between calcaneus and talus fractures on plain radiographs. Use radiography to calculate Bohler’s and Gissane’s angles. Classify calcaneus fractures according to Sanders Classification using coronal CT images. Determine the appropriateness of operative vs. non-operative management depending on whether fractures are displaced and the patients associated risk factors.
