11 Rheumatoid Disorders of the Foot and Ankle
Rheumatoid arthritis (RA) is an autoimmune chronic inflammatory condition where the body’s immune system attacks the joints and causes inflammation of the joint lining (synovium). Typically RA is a symmetrical polyarthritis, affecting multiple small joints of the hands and feet bilaterally, and more than 90% of RA patients develop symptoms in the foot and ankle over time.
Structure and function
Diarthrodial joints, which include the type found between the bones of the feet, are lined by the synovium. The synovium produces a synovial fluid to lubricate the joint, reduce friction, and help absorb shock. Normal synovial tissue has thin monolayer of cells containing monocyte-derived cells that remove debris, cells that produce hyaluronic acid, and fibroblasts that produce lubricin.
Pathophysiology of rheumatoid arthritis
Rheumatoid arthritis is an inflammatory disease of the synovium, often affecting the small joints of the hands and feet (MTP, PIP, DIP joints). The etiology of RA is likely an interplay of genetics, environmental triggers, and immune response leading to an autoimmune attack on the body’s own tissue. In brief, the synovial membrane is infiltrated by macrophages, lymphocytes, plasma cells, and granulocytes. Macrophages secrete matrix metalloproteinases and other proteolytic enzymes that damage the synovial tissue. Plasma cells release rheumatoid factor (RF) and other immunoglobulins that perpetuate the inflammatory response.
Patient presentation
A typical patient will likely be female, aged 40 to 60 presenting with pain, stiffness, swelling, and limited range of motion in the joints, prototypically those of the wrists and hands. Initial involvement in the feet occurs in 15% of cases. The stiffness seen in RA is most often worst in the morning, and may last one or two hours. The morning stiffness is due to a build-up of extracellular fluid in and around the joint. Other signs and symptoms are systemic and include loss of energy and appetite, dry eyes and fever. A dry mouth and firm lumps beneath the skin (so-called rheumatoid nodules) may also be seen.
In the lower extremity, RA more commonly affects the forefoot; the midtarsal joints are next most likely to be involved. The forefoot is involved twice as often as the hindfoot.
The changes that occur to the forefoot in patients with RA span a combination of bunions, claw toes, and metatarsalgia. These changes occur because the inflamed synovium causes the associated joint capsule to become lax leading to deformity or even dislocation of the involved joint. Hallux valgus can be quite severe and the big toe commonly crosses over the second toe. Calluses can also form on the ball of the foot when midfoot bones are pushed down from joint dislocations in the toes (MTP joints). As a result, callosities and even ulcers on the plantar forefoot can form from the abnormal pressure.
In the midfoot, RA can weaken the ligaments that support the midfoot causing collapse of the arch. Bony prominences can appear on the arch. Rupture of the tibialis posterior tendon can occur, and if it does, the talonavicular joint and subtalar joints sublux and the hindfoot drifts into valgus, leading to midfoot hyperpronation and a marked acquired adult flatfoot deformity (fallen arch).
Objective evidence
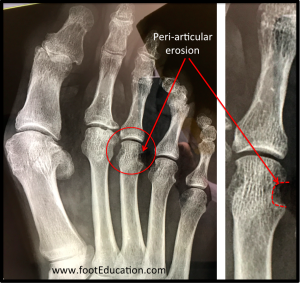
Radiographs may show soft tissue swelling, subchondral bone erosions, osteopenia, joint space narrowing, bony destruction, and the classic finding of peri-articular erosions. Osteopenia starts in the metaphyseal region underlying collateral ligament attachments and becomes more generalized as the disease progresses. Inflamed synovium can wear away the bone at the point where the collateral ligaments attach creating characteristic peri-articular erosions (Figure 1). Cartilage destruction occurs when the inflamed synovium extends into the joint itself growing on top of the cartilage (pannus). This leads to destruction of the cartilage over time and narrowing of the joint on plain x-rays. Mal-alignment, displacement, and ankylosis of the joint mark end-stage rheumatoid disease.
Synovial fluid: Aspiration and analysis of the synovial fluid is important for distinguishing RA from non-inflammatory and infectious arthrosis. The fluid in patients with RA will be sterile, with increased neutrophils and increased protein but decreased viscosity. Obtaining a fluid sample from small joints in the feet in early stages can be very difficult and not clinically practical in many cases.
Epidemiology
RA is the most common of the inflammatory arthritides affecting about 1% of people, with female:male ratio of 3:1. The peak incidence is at age 50, and symptoms most commonly develop between age 40 to 60.
Differential diagnosis
RA of the foot can present with findings that may suggest other conditions including:
- Crystal induced arthritis(gout/pseudogout): usually involves the knee, the metatarsal-phalangeal joint of the big toe, and the heel, and can be diagnosed with an aspiration of the joint fluid.
- Osteoarthritis: usually seen in older patients and affects weight-bearing joints asymmetrically. Pain worsens with prolonged use of the joint. Can be distinguished with x-rays.
- Systemic lupus erythematosus: characterized by the “butterfly rash” on the face, photosensitivity, joint pain in the hands and feet, and presence of antibodies against double-stranded DNA.
- Scleroderma: joint inflammation, compression syndromes (carpal tunnel is often an initial symptom of scleroderma).
- Psoriatic arthritis: distinguished by nail and skin changes.
- Lyme disease: check patient’s history of presence in endemic regions and order appropriate blood tests as necessary to diagnose.
- Reiter’s syndrome(reactive arthritis): asymmetrically involves the heel, sacroiliac joints, and large joints of the leg. Also associated with urethritis, conjunctivitis, iritis and painless buccal ulcers.
- Ankylosing spondylitis: though this involves the spine, it’s possible that RA-like symmetrical, small-joint polyarthritis might also occur in AS.
- Hepatitis C: may induce Rheumatoid factor auto-antibodies, and can cause RA-like symmetrical small-joint polyarthritis.
- Acute rheumatic fever: migratory pattern of joint involvement (usually asymmetric), with history of antecedent streptococcal infection.
- Gonococcal arthritis: migratory pattern involving tendons around ankles and wrists, with history of antecedent gonococcal infection.
Red flags
RA can be systemic. Consider the diagnosis of RA as a red flag to prompt an evaluation of problems elsewhere. As a systemic disease RA can affect blood vessels, nerves, and tendons throughout the body. Patients with extra-articular manifestation are more likely to have a high RF titer, more severe disability, and increased mortality rate.
Treatment options and outcomes
There is currently no cure for RA. Medical treatments focus on controlling the disease and preventing progressive loss of function of the joints. As many of the symptoms of RA stem from the resulting joint deformity or loss of articular cartilage, early aggressive treatment is very important.
NSAIDs and corticosteroids (oral or injections) are used to alleviate inflammation and vasculitis. There are now a series of disease modifying anti-rheumatic drugs (DMARDs) that slow progression and improve symptoms, function, and quality of life. Common DMARDs include Methotrexate and biologic agents such as etanercept, infliximab and adalimumab that offer a more specific approach by targeting the pro-inflammatory cytokine TNF.
In the case of flare-ups of the foot and ankle, considerable relief can be gained from the use of appropriate footwear and insoles. Stiff soled comfort shoes with a soft accommodative orthotic and a wide toe box can be very helpful in patients with RA. An orthotic and/or a rocker soled shoe can support RA involvement of the midfoot (arch) and ankle. Some patients may benefit from the use of ankle bracing or even use of a removable walking cast boot.
In cases of an acquired adult flatfoot deformity (collapse of the arch) secondary to an RA induced posterior tibial tendon dysfunction a surgical reconstruction may be indicated. When RA affects the posterior tibial tendon, early synovectomy of the tendon sheath relieves discomfort and can delay or prevent rupture. When posterior tibial tendon rupture has occurred, transfer of the flexor digitorum longus tendon to the distal posterior tibial tendon stump combined with a subtalar fusion or a medializing calcaneal osteotomy may be necessary.
Foot surgery in the RA patient needs to be tailored to the specific deformity. For example, talonavicular arthritis is common in RA patients. These patients often do well with a fusion of the talonavicular joint using a bone graft. This can alleviate the pain from this joint and provide the foot with a stable medial beam, thereby helping to prevent the calcaneus from taking a fixed valgus position.
If RA of the forefoot has severely progressed with dislocation of many of the MTP joints one option is the Hoffman procedure -a procedure that removes all of the metatarsal heads in the foot. The bony prominence of the metatarsal heads are removed shifting the weight-bearing surface to the bottom of the foot. This MTP joint sacrificing procedure should be performed only in advanced disease, as it is quite destructive and non-anatomic. This procedure is usually reserved for the lesser (2-5) MTP joints only and is often combined with arthrodesis (fusion) of the 1st MTP (big toe) joint (Clayton procedure).
Patients with significant RA involving the hindfoot will often develop marked pain and associated deformity. These patients may benefit from a triple arthrodesis. This procedure realigns and fuses the talonavicular, subtalar, and calcaneocuboid joints. Fusion allows the deformity to be corrected, improves stability of the hindfoot, and eliminates pain from the arthritic joints thereby allowing for easier weight-bearing. A potential complication is that other joints of the foot may develop arthritis over time as they will be subject to more stress after a triple arthrodesis.
Risk factors and prevention
Risk factors include HLA-DR4 haplotype; female gender; smoking history; and periodontal disease. While alone it has not been associated with increased risk of developing RA, obesity has been linked to poorer prognosis and response to treatment modalities.
Miscellany
Synovium is partially derived from the word ovum, Latin for egg, because of the yolk-like consistency of synovial fluid.
Key terms
Synovitis, morning stiffness, inflammatory arthritis, rheumatoid factor, ACPA, HLA-DR4, symmetrical polyarthritis, claw toes
Skills
Recognize RA and distinguish it from osteoarthritis. Analyze synovial fluid and distinguish inflammatory vs non-inflammatory, and infectious vs non-infectious arthritides. Assess joint damage in radiographs.
