21 Scaphoid Fractures
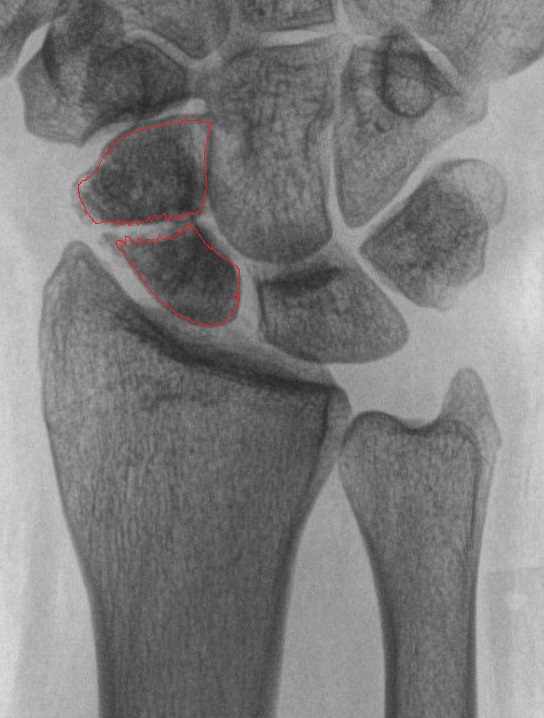
The scaphoid (also known as the carpal navicular) is perhaps the most important of the eight carpal bones. The scaphoid links the carpal bones closest to the radius and ulna, the so-called the “proximal row,” to those articulating with the metacarpals, the “distal row.” Owing to its tenuous blood supply, the scaphoid is particularly susceptible to osteonecrosis (and ensuing post-traumatic arthrosis) after fracture. Unfortunately, the scaphoid is also the most commonly fractured of the eight carpal bones (Figure 1). Fracture is usually caused by a fall on an outstretched hand (a mechanism also associated with distal radius fractures and radial head fractures).
Structure and function
The scaphoid can be morphologically divided into three anatomic regions: proximal third (proximal pole), central third (waist), and distal third (distal pole). A tuberosity on the distal palmar aspect serves as an attachment site for the transverse carpal ligament. Nearly 2/3 of all scaphoid fractures occur at the waist, with 15% occurring at the proximal pole, 10% at the distal pole, and 8% at the tuberosity.

The scaphoid (Figure 2) articulates with the radius and four carpal bones (lunate, trapezium, trapezoid, and capitate). To accommodate so many articulations, 80% of the scaphoid is covered with cartilage.
The scaphoid is supported by the radioscapholunate ligament which stabilizes the scapholunate articulation and acts as a neurovascular conduit. The scaphoid does not have any tendinous attachments.
The scaphoid receives its primary blood supply from the dorsal scaphoid branches of the radial artery, which enter the scaphoid at a point near the distal pole. As such, the scaphoid is perfused in the distal to proximal direction (“retrograde blood supply”).
Because of this retrograde blood supply, an injury to the scaphoid waist (i.e. the middle third of the bone) can interrupt blood supply to the proximal pole. (This is analogous to femoral neck fractures and resulting femoral head ischemia: just as the vessels to the femoral head must traverse the femoral neck, the blood supply to the proximal pole of the scaphoid must traverse the waist).
Patient presentation
Patients with scaphoid fractures will often present with radial sided wrist pain (worsened with gripping or squeezing), variable swelling and limited range of motion. Because scaphoid fractures may occur without bruising or visible deformity, patients may assume a less serious injury and delay seeking evaluation.
During examination, it is important to always compare the injured to the uninjured wrist.
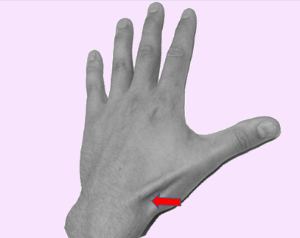
Check if patients have tenderness to palpation of the “anatomic snuffbox” and over the scaphoid tubercle (Figure 3).
The anatomic snuffbox is located in a triangle formed by the extensor pollicis longus tendon, abductor pollicis longus tendon, and the radial styloid. It can be found more easily when the thumb is actively extended. Anatomic snuffbox pain has a sensitivity of 90% and specificity of 40% for detection of scaphoid fractures.
The scaphoid tubercle can be localized on the volar aspect of the wrist (Figure 4). Pain to palpation is a slightly less sensitive but more specific finding for detection of scaphoid fractures.
objective evidence
Plain radiographs are essential for all patients with suspected scaphoid fractures. Standard radiographs include anteroposterior (AP), lateral, oblique and scaphoid views. The scaphoid view is a posteroanterior (PA) view of the wrist, with the wrist positioned in 45 degrees of ulnar deviation and pronated obliquely at 45 degrees.
Because initial radiographs of a scaphoid fracture may appear normal, patients with pain in the snuff box and a fall on the outstretched hand should be immobilized and sent for additional imaging studies.
One approach would be to obtain repeat radiographs in 10 to 14 days. At that point, the absence of fracture line or healing response on x-ray, coupled with an absence of tenderness on exam reasonably excludes the diagnosis of fracture.
Another approach would be to obtain an MRI. This test can detect an occult scaphoid fracture immediately, as well as any other associated injury.
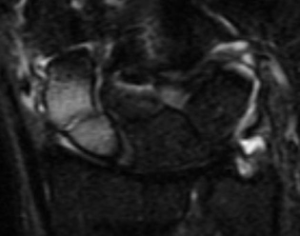
Although bone scans (scintigraphy) can also be used to detect occult scaphoid fractures, MRI has two advantages (Figure 5). First, an MRI can be used immediately. (Bone scans, which assess a biological reaction that takes days to mount, can be falsely negative in the first few days.) Second, as noted, MRI can detect associated injuries as well. (The great sensitivity of MRI can impose costs too, as it may detect a clinically insignificant abnormality as well, prompting unnecessary worry to say nothing of unnecessary treatment.)
Note that MRI is still an expensive imaging modality in many locations. In the United States, at least, the use of MRI is advocated nonetheless, as the true price of MRI is not that much more than plain radiographs. Also, placing a patient in a cast for 10 days while awaiting the second round of radiographs represents a significant delay in treatment if a fracture does indeed exist.
Epidemiology
The scaphoid is the most commonly fractured carpal bone. Fractures of the scaphoid often occur in physically active individuals, and have two to four times greater incidence in men than woman. The most common mechanism of injury is a fall onto an outstretched hand.
The true incidence of scaphoid fractures has been difficult to calculate particularly because many of these injuries are undiagnosed. One estimate is that scaphoid fractures represent 1 out of 100,000 people per year.
Differential diagnosis
The differential diagnosis of suspected scaphoid fracture includes:
- Radial styloid fracture. Here, the tenderness is more proximal; radiographs should make the diagnosis.
- Distal radius fracture. Tenderness localizes to distal radius and deformity may be present; radiographs should make the diagnosis.
- Scapholunate instability. In this condition, the tenderness is more toward the ulnar side of the hand (over the scapholunate ligament) and radiographs should show a gap between scaphoid and lunate (scapholunate dissociation: the Terry Thomas sign).
- Flexor carpi radialis tendon injury. This can be diagnosed by noting pain elicited with resisted wrist extension.
- De Quervain’s disease. A positive Finkelstein’s test may help make the diagnosis.
- Carpometacarpal joint arthritis. Here, radiographs should make the diagnosis, but recall that a patient with arthritis can suffer a superimposed injury.
As noted, fracture of the scaphoid is usually caused by a fall on an outstretched hand, the same mechanism associated with distal radius fractures and radial head fractures. The astute clinician must be mindful of these potentially associated injuries.
Red flags
A fall on the outstretched wrist is itself a “red flag” and should raise suspicion for a scaphoid fracture. When there is tenderness in the anatomic snuff box, even if radiographs appear negative, a scaphoid fracture is even more likely.
Treatment options and outcomes
The patient with tenderness in the anatomic snuff box and negative x-rays should be immobilized in a thumb spica splint (Figure 6) and additional imaging should be obtained. The additional imaging can take the form of either repeat radiographs about 2 weeks after the injury, bone scintigraphy or MRI. This initial immobilization will minimize the chance that a non-displaced occult fracture (i.e., one not seen on x-ray) becomes a displaced fracture, and in turn, minimizes the risk of disrupting the blood supply.
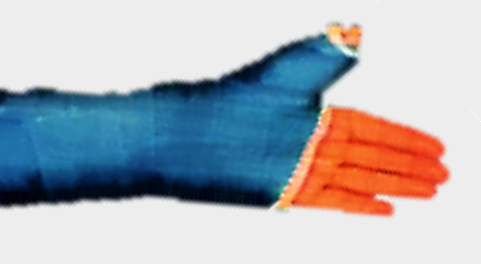
Non-displaced fractures are defined as fractures with less than 2mm of displacement and no fracture site angulation. These types of fractures are treated by immobilization in a long or short arm thumb spica cast for 6 weeks. (The inclusion of the thumb is advised; whether a long arm (vs short arm) cast is needed is perhaps a bit more controversial. Including the elbow will minimize pronation/supination.)
A small (n=25) prospective, randomized study comparing cast immobilization with percutaneous cannulated screw fixation of nondisplaced scaphoid fractures found that screw fixation resulted in faster radiographic union (7 weeks vs 12) and return to military duty (8 weeks vs 15).
Comminuted, displaced or unstable scaphoid fractures benefit from surgical fixation. The precise indications for surgery (that is, how much linear or angular displacement is enough?) are not known.
The favored technique is open reduction internal fixation with screws (Figure 7). The choice of fixation depends on a multitude of factors, such as the location of the fracture, configuration of the fracture, functional concerns, and patient factors.

Most scaphoid fractures treated non-surgically heal without difficulty, with the occurrence of nonunion reported between 5% and 15%.
Scaphoid fractures (especially if not recognized and therefore not treated) can result in post-traumatic arthritis. Once arthritis is evident at the radiocarpal joint there are salvage surgical procedures that can be performed. These include a proximal row carpectomy, scaphoid excision and midcarpal arthrodesis, or a total wrist arthrodesis.
Risk factors and prevention
Scaphoid fractures typically occur in active adolescents and young adults with an incidence two to four times higher in men than in women. The fracture commonly occurs as a result of extreme dorsiflexion of the wrist from a fall.
Short of telling all young, active males to not fall (and getting them to comply!), it is difficult to prevent these fractures. The key point in treating this injury is to prevent non-displaced fractures from displacing, as displacement makes osteonecrosis much more likely.
Miscellany
Scaphoid derives from the Greek word skaphos, which means “a boat.” The English word “skiff” has a similar origin. The scaphoid is also referred to as the carpal navicular (coming from navis, the Latin word for “boat,” from which we get the English word “navy,” for example). Given that there is also a boat-like bone in the foot, it is probably best to refer to the bone in the hand as the scaphoid and the one in the foot as the navicular.
Regardless of length of immobilization after a scaphoid fracture, appropriate physical and occupational therapy is needed after removal of the cast or splint to optimize range of motion and function.
Smoking is strongly associated with nonunion after surgical fixation of the scaphoid.
Key terms
scaphoid, fracture, non-union, avascular necrosis, anatomic snuffbox, scaphoid compression test
Skills
Perform physical examination to recognize occult scaphoid fractures. Be able to explain to patients why immobilization is needed despite “normal” x-rays. Apply a thumb spica splint to temporarily immobilize the scaphoid while awaiting definitive treatment.
