Exchange with the Environment
12 Digestive System
Exchange with the Environment
Introduction to the Digestive System

(Credit: Drhaggis at English Wikipedia, CC BY 2.0)
Which organ is the most important organ in the body? Most people would say the heart or the brain, completely overlooking the gastrointestinal tract (GI tract). Though definitely not the most attractive organs in the body, they are certainly among the most important. The 30-plus foot long tube that goes from the mouth to the anus is imperative for our well-being and our lifelong health. A non-functioning or poorly functioning GI tract can be the source of many chronic health problems that can interfere with your quality of life. In many instances, the death of a person begins in the intestines.
The old saying “you are what you eat” perhaps would be more accurate if worded “you are what you absorb and digest.” Here we will be looking at the importance of these two functions of the digestive system: digestion and absorption.
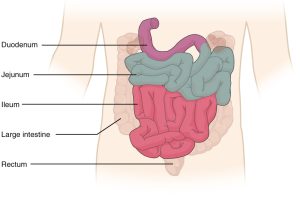
The GI tract starts with the mouth and proceeds to the esophagus, stomach, small intestine (duodenum, jejunum, ileum), and then to the large intestine (colon), and rectum, and terminates at the anus. You could probably say the human body is just like a big donut. The GI tract is the donut hole.
Animals obtain their nutrients through the consumption of other organisms. At the cellular level, the biological molecules necessary for animal function are amino acids, lipid molecules, nucleotides, and simple sugars. However, the food we consume consists of protein, fat, and complex carbohydrates. Our bodies must convert these macromolecules into the simple molecules required for maintaining cellular function. The conversion of the food consumed to the nutrients required is a multistep process involving digestion and absorption. During digestion, food particles are broken down into smaller components, and the body later absorbs these. This happens by both mechanical means, such as chewing and by chemical means, via chemical reactions that use enzymes.
As we said, the digestive system is basically a tube within our body, from mouth to anus. It includes the stomach and intestines, as well as accessory organs such as the liver, gall bladder, and pancreas. The space within any tubular body structure, such as blood vessels or the digestive tract, is known as a lumen. Anything inside the space or lumen of the GI tract is technically described as still being “external” to the body tissues. Thus, the caustic process of digestion is occurring in an “external” tube, and so the “internal” body tissues are not destroyed. The products of digestion are absorbed from this “external environment” into the body’s cells.
The Digestive System in the Big Picture of Human Biology
The digestive system clearly demonstrates several of the core ideas in Human Biology:
- The processes that occur in living organisms follow the laws of physics and chemistry. Both mechanical and chemical digestion are necessary to convert the food we eat into a form that can be absorbed.
- The cell is the basic unit of life; the plasma membranes of cells control the transport and signaling necessary for life. Specialized cells are able to secrete substances into the digestive tract space (called the lumen) to protect the body from this mixture because some of these substances would otherwise digest the body and then absorb specific substances from the mixture into the body.
- Life requires information flow within and between cells and between the environment and the organism. Receptors monitor the composition of the mixture as it moves through the digestive tract, stimulating the secretion of hormones and triggering nerve impulses. Together the endocrine and nervous systems coordinate the release of substances and control the movement from one segment to another.
- Living organisms must obtain matter and energy from the external world. This matter and energy must be transformed and transferred in varied ways to build the organism and perform work. Food in the diet must be broken down into its basic units for absorption, and then these are used to fuel ATP production, build and repair cells and tissues, and participate in other metabolic activities of the body.
- Homeostasis (and “stability” in a more general sense) maintains the internal environment in a more or less constant state compatible with life. In addition to nutrients, the absorption of vitamins, electrolytes, and water is critical to maintaining body homeostasis, with disorders and diseases occurring when malabsorption occurs.
- Understanding the behavior of the organism requires understanding the relationship between structure and function (at each and every level of organization). The concept of increased surface area for efficient absorption in the digestive system best illustrates this.
- Cell-level function is supported by all the tissue structures that make up the different segments and organs of the digestive system.
All life depends upon the proper interactions and supporting functions among interrelated organ systems. In addition to obtaining necessary metabolic substances needed by all other body systems, the digestive system has several mechanisms to protect other systems against pathogens that can enter with things we ingest.
Here is a preview of each of the sections to come:
- Digestive System Structures and Functions will explore how the major organs of the digestive system are able to accomplish the major system-level functions:
- movement through the length of the digestive system
- complementary mechanisms for digestion in different segments of the digestive tract
- structures that enhance absorption
Pay attention to not only what structures are similar and what are unique in the different sections but also to how each contributes to the function of the system as a whole.
- Levels of Organization will examine this structure and function in more detail, progressing through the major levels of organization in the human organism from the chemical and cellular levels to the tissues, organs, and organ systems:
- nutritive and digestive molecules
- cells of the stomach, small and large intestine, liver, and pancreas
- tissue layers and organs that make up the digestive tract, from mouth to anus
- accessory organs that contribute secretions to the digestive tract
Pay attention to the function of cells for both secretion and absorption of specific substances in the different parts of the digestive tract and accessory organs. What these specific cells produce and how they move materials across cell membranes are critical to understanding the function of the system as a whole.
- Homeostasis will delve into how this system contributes to the body’s natural tendency to maintain a stable internal environment:
- how hormones and nerves control and coordinate the digestive system
- what happens when the digestive system malfunctions
Pay attention to how not only is the rate of movement from one section to another controlled, but what is released into the lumen of the digestive tract is controlled based on monitoring of the content of food eaten. Don’t get the endocrine secretion of hormones into the blood for control and regulation confused with the exocrine secretion of substances into the lumen for the digestion and absorption processes. Although both are happening, these are different processes.
- Integration of Systems will investigate which systems are subsets of larger systems and how they function together in harmony and conflict:
- how the digestive system interacts with the other body systems
- how other systems affect the digestive system functions
Pay attention to the relationship between proper movement and secretion for digestion and the subsequent absorption and transport of materials for metabolism. This links the digestive tract and accessory digestive organs to the other systems.
Did I Get This? 12.1
There are two different kinds of secretions associated with the digestive system that need to be understood to avoid confusion when describing how the digestive system functions. Which one of these secretions will be involved in the control of digestion through the blood?
- endocrine
- exocrine
What two body systems regulate and control the proper function of the digestive system?
- endocrine and lymphatic systems
- nervous and cardiovascular systems
- nervous and endocrine systems
All the secretion and absorption functions of the digestive system need to be understood as happening at what level of organization?
- the cell and cell membrane
- tissues
- organs
What structure-function concept is important at all levels of organization for very efficient absorption in the digestive system?
- accessory organ secretions
- increased surface area
- hormonal control of digestion
- enzyme digestion of food
Digestive System Structures and Functions
Learning Objective
The digestive system moves water, nutrients, and electrolytes (ions) from the external environment to the internal environment. Within the digestive system, the gastrointestinal tract is a continuous hollow tube from the mouth to the anus and is continuous with the external environment. All digestive system organs play vital roles either in moving material through the tract, in breaking down food into its chemical building blocks, absorbing these building blocks into the blood, and/or eliminating leftover indigestible materials.
Different parts of the digestive system secrete substances into the space within the digestive tract. These secretions come from both the cells that make up the epithelial lining of the digestive tract and from exocrine accessory organs that have ducts emptying into the tube. Some of these substances assist with the movement of food from one part of the tract to the next (such as mucus) and others with the digestion of the food while it is in the tube (such as enzymes).
In order to be absorbed, digested material has to be moved from the inside of the digestive tract into the epithelial cells lining that line it. Next, it must be moved out of the other side of these cells into the body’s interstitial fluid. Finally, the material must be absorbed by blood or lymph capillaries for transport through the body. This process can happen by active or passive transport. (You may want to review transport across the plasma membrane.) Chemicals secreted into the digestive tract can enhance the absorption of certain substances. Anatomical structures that increase the area of the absorptive surface exposed to the digested substances in the tube will also enhance absorption.
Learn By Doing 12.1
Many different digestive dysfunctions have very similar symptoms. Understanding the biochemical and cellular functions of the digestive system can help in understanding some of the various causes. Celiac disease is a digestive system disorder that is also known as gluten intolerance. Gluten is made up of amino acids and is found in wheat. When the enzyme transglutaminase reacts with gluten in the digestive system, it can cause an autoimmune response that destroys the lining of the small intestine. This causes improper absorption and associated symptoms.
Celiac disease is caused by a problem with which kind of organic compound?
- nucleic acid
- carbohydrate
- protein
- lipid
Hint: Gluten is found in seeds with starch, but it is not in the same organic group as starch.
There is another kind of secretion involved in regulating this whole process, including how long food stays in one section of the digestive tract for the most efficient digestion or absorption. These are endocrine secretions from cells that are part of the digestive organs themselves. These hormones are secreted into the blood, not the digestive lumen, and transported by the blood to target cells of the digestive system organs. In this way, the functioning of different organs within the digestive tract is coordinated. The autonomic nervous system also plays a role in regulating and coordinating the digestive system.
Learn By Doing 12.2
Some people with Panic Disorder have been found to have an inherited metabolic defect that prevents them from producing a digestive system hormone called cholecystokinin (CCK). CCK controls the release of digestive secretions from the liver/gall bladder and pancreas into the small intestine. CCK also acts in the central nervous system, affecting neuron communication in parts of the brain that regulate anxiety and stress. People with this particular genetic condition may experience Gastro-Esophageal Reflux Disease (GERD) or Irritable Bowel Syndrome (IBS), sometimes for years before they ever have a panic attack experience.
Which function of the digestive system would be LEAST directly affected by the lack of CCK?
- elimination of residual indigestible materials
- regulation among different organs of the digestive system
- digestion of food into chemical building blocks
- absorption of building blocks into the body
Hint: All these functions will be affected, but one of them will continue despite the lack of CCK and may even be enhanced in a way that leads to some of the symptoms this person could experience related to the digestive system.
We usually do not think about the digestive system until something goes wrong with it – when we get indigestion, nausea, or diarrhea. We seldom appreciate that the digestive system is a complex string of organs that allows us to transform the food we eat into nutrients that can be used as energy sources or as the building blocks of larger molecules. Each organ of the digestive system performs specific functions, but all these organs work together to digest the foods we eat and absorb the nutrients into our bodies.
Learn By Doing 12.3
Lactose intolerance is a digestive system disorder related to biochemical processes. In this genetic disorder, the person doesn’t produce enough lactase to digest lactose in their diet, so lactose isn’t absorbed in the small intestine. When it moves on to the large intestine, lactose upsets the water homeostasis and bacteria can metabolize it, creating various symptoms.
Lactose intolerance is caused by an insufficiency of the enzyme required to digest which kind of organic compound?
- carbohydrate
- protein
- lipid
- nucleic acid
Hint: Lactose is found in milk products and is also known as “milk sugar”.
The digestive system is generally divided into two main categories: organs of the alimentary canal (aliment = “nourish”) and accessory digestive organs. The alimentary canal, also called the gastrointestinal (GI) tract or gut, is a continuous muscular tube that runs from the mouth to the anus. The internal space of this tube is called the lumen. The GI tract is involved with the digestion of food –its breakdown into smaller fragments – and the absorption of digested food fragments from the lumen through the alimentary canal wall and into the bloodstream. The accessory digestive organs contribute to secretions to the GI tract, but the food doesn’t pass through these organs.
Digestive System Organs
Learning Objectives
- Identify organs of the digestive system based on position and structure.
- Identify the function of each.
- Describe how material moves through the digestive system.
- Explain how mechanical and chemical digestion work together to produce absorbable nutrients.
- Explain how nutrients are absorbed in the digestive system.
Different digestive system organs are responsible for different digestive processes and functions. These functions include extracting nutrients from food and removing waste. The processes by which these occur are called ingestion, peristalsis (the movement of food through the GI tract lumen), mechanical and chemical digestion of the food, absorption, and defecation to remove residues.
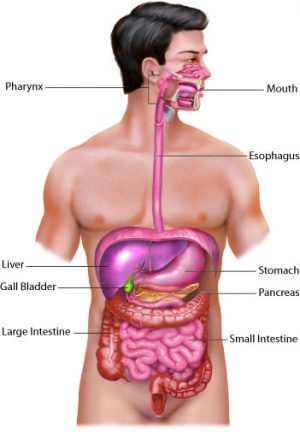
(Credit: Image by Cenveo is licensed under a Creative Commons Attribution 3.0 United States.)
The process of digestion begins in the mouth (oral cavity) with the intake of food. The teeth play an important role in masticating (chewing) or physically breaking food into smaller particles. This action not only decreases the size of the food particles to facilitate swallowing but also increases the surface area for chemical digestion. The enzymes present in saliva (amylase and lipase) also begin to chemically break down food (starch and fats, respectively). The food is then swallowed and enters the esophagus—a long tube that connects the mouth to the stomach. Using peristalsis, or wave-like smooth-muscle contractions, the muscles of the esophagus push the food toward the stomach. The stomach contents are extremely acidic, with a pH between 1.5 and 2.5. This acidity kills microorganisms and activates digestive enzymes. Further breakdown of food takes place in the small intestine where bile produced by the liver, and enzymes produced by the small intestine and the pancreas, continue the process of chemical digestion. The smaller molecules are absorbed into the bloodstream through the epithelial cells lining the walls of the small intestine. The waste material travels on to the colon or large intestine where water is absorbed, and the drier waste material is compacted into feces; it is stored in the rectum until it is excreted through the anus.
Study the table below. It summarizes the major functions of digestive system organs. Subsequent sections of the chapter will discuss these organs and functions in more detail.
| Organ | Major Functions |
| Mouth | Ingests food; Mechanical digestion of food; Salivary amylase begins chemical breakdown of starch; Swallows food and propels it into the pharynx |
| Pharynx | Propels chewed food from the oral cavity to the esophagus |
| Esophagus | Peristaltic waves propel food bolus to the stomach |
| Stomach | Peristaltic waves combine food with gastric juice and move it into the duodenum; Pepsin begins protein digestion; Absorption of some fat-soluble substances (e.g., alcohol, aspirin) |
| Small intestine | Mixes contents with digestive juices for digestion and absorption; Enzymes digest food; Absorbs breakdown products of carbohydrates, protein, fat, and nucleic acid digestion, along with vitamins, water, and electrolytes |
| Large intestine | Gut bacteria digest some food residue and vitamins; Absorbs most residual water, electrolytes, and vitamins produced by enteric bacteria; Propels feces toward rectum; The defecation reflex eliminates feces |
| Accessory organs | Liver: produces bile
Gall bladder: stores and concentrates bile Pancreas: produces enzymes that digests food |
Movement of Material Through the Digestive System
Both voluntary skeletal muscles and involuntary smooth muscles are involved in propelling food material through the digestive system. Skeletal muscles of the tongue are involved in the voluntary first phase of swallowing, but then it becomes an involuntary reflex with skeletal muscles of the pharynx.
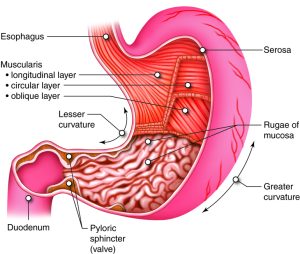
The smooth muscle of the GI tract is arranged in two layers: longitudinal along the length of the tube and circular around the diameter of the tube. Coordinated contraction and relaxation of these two layers creates a wave-like propulsion of the food called peristalsis. Muscles in the esophagus mechanically transport food via peristalsis from the mouth to the stomach. An extra smooth muscle layer in the stomach adds a churning movement within the stomach. Peristalsis continues to propel food through the small and large intestines.
Controlling the rate of food moving from one organ of the digestive tract to the next are specialized circularly arranged skeletal and smooth muscles called sphincters. Sphincters are typically contracted and relax only to allow food to move from one organ to the next. The majority of sphincters along the length of the GI tract are involuntary smooth muscle structures. The esophageal sphincter helps separate the esophagus from the stomach to maintain linear movement and protect the esophagus from the acidic chemicals of the stomach. The pyloric sphincter separates the stomach from the small intestine. There is a physical separation for compartmentalization and to prevent the backward movement of material.
The material then snakes its way through the small intestine and the iloeocecal sphincter controls movement into the large intestine or colon. The anal sphincter muscle is a skeletal muscle controlled consciously to relax during defecation. There is also a hepatopancreatic (hepato- liver) sphincter that controls the release of accessory secretions from the liver and pancreas into the beginning of the small intestine.
Learn By Doing 12.4
Which sphincter would not have food in some form (bolus, chyme, feces) passing through it when it relaxes?
- hepatopancreatic sphincter
- internal anal sphincter
- lower esophageal sphincter
- pyloric sphincter
Hint: All of these sphincters control the rate of the material moving through the lumen of the tube, but only one of these has a secretion produced by accessory organs moving through the sphincter-controlled opening; all the others have food moving through the sphincter-controlled opening between different organs of the GI tract.
Overview of Digestion
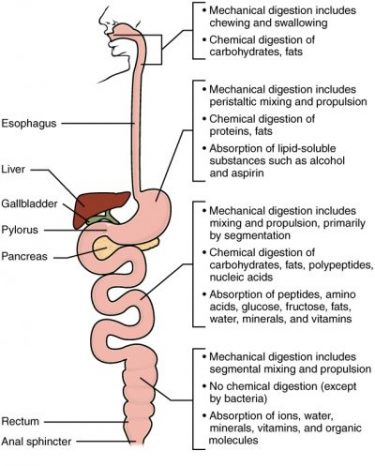
Digestion is accomplished both mechanically and chemically. Mechanical digestion physically breaks food into smaller pieces, increasing surface area for more efficient chemical digestion. Chemical digestion breaks large food macromolecules down into their chemical building blocks, which can then be absorbed through the intestinal wall and into the general circulation.
Food is ingested in the mouth where it begins mechanical digestion from the grinding of the teeth and chemical digestion from enzymes in the saliva. Chemical digestion starts in the saliva and continues in the stomach. In the stomach, the material is broken down into smaller components by chemically strong acids, enzymes, and mechanical churning. However, the small intestine is the site of most chemical digestion and almost all absorption. Enzymes, bile, bicarbonate, and other materials are mixed in from the pancreas and liver to promote chemical digestion and allow enhanced adsorption. Enzymes are responsible for the majority of this chemical digestion. The breakdown of fat also requires emulsification by bile, secreted by the liver and stored in the gall bladder.
Learn By Doing 12.5
Where do the processes of chemical and mechanical digestion begin and end?
- Mouth and stomach
- Stomach and small intestine
- Esophagus and stomach
- Mouth and small intestine
Overview of Absorption
The mechanical and chemical digestive processes that begin in the mouth and continue through the small intestine have one endpoint: to convert food into substances that can be absorbed from the lumen by epithelial cells in the lining of the GI tract and then enter blood or lymphatic vessels. Absorbable substances are the monosaccharides, glucose, galactose, and fructose from carbohydrates; single amino acids, dipeptides, and tripeptides from proteins; and monoglycerides, glycerol, and fatty acids from lipids such as triglycerides.
Digestive System Levels of Organization
In order to get the various materials needed for energy production and anabolic metabolism in all body cells, our body has to import nutrients, water and electrolytes from the environment. However, the substance taken into the space of the GI tract is not always in the form that can be absorbed, so it must first be broken down. Various secreted chemicals are critical to accomplishing this digestion. These ingested macromolecules are digested in different regions of the GI tract, requiring that the mixture of material be moved through the digestive system in a controlled way. Once it has been digested to a more basic chemical structure, the material can be absorbed into the blood or lymph. At that point, the other body systems integrate to distribute these absorbed nutrients, fluids and electrolytes through the body as needed. Any waste material remaining in the GI tract will then be removed from the body by defecation.
To understand these system-level functions, you will be further exploring structures and processes occurring at all levels of organization. Some examples of major digestive structures assigned to their structural level of organization of the digestive system include:
- Organ System level- integration of organs for nutrient and waste movement, digestion and absorption
- Organ level- gastrointestinal tract and accessory organs
- Tissue level– epithelial, connective, and smooth muscle tissues
- Cellular level– mucosa cells, secretory cells, and immune cells
- Molecular level- enzymes of digestion, bile, and the nutritive molecules such as carbohydrates, protein, lipids and nucleic acids.
Rather than consider each of these levels independently in this chapter, we will begin by reviewing the functions of macromolecules and the process by which they are broken down. Then we will journey through the digestive tract, beginning with its shared tissue organization, and investigating the cellular, and molecular specializations of each part of the tract as we go. We will finish the section by summarizing how the organs of the digestive system work together to import materials with the environment, make them available to the rest of the body, and rid the body of undigested materials.
Learn By Doing 12.6
Which would be the correct order from smallest to largest?
- Enzymes, ions, liver, GI tract
- GI tract, stomach, bile, HCl
- Epithelial cells, bile, liver, HCl
- HCl (an acid), Bile salt, secretory cell, small intestine
A Review of Biological Macromolecules
Learning Objectives
- Describe the basic process of enzymatic hydrolysis for nutritive organic compounds.
- Identify the functions of the 4 types of biological macromolecules.
The digestive system breaks down ingested material into absorbable components (nutrients) that the rest of the body can use to maintain adequate function. We require a diverse set of nutrients to support energy production, carry out metabolism, and maintain structure.
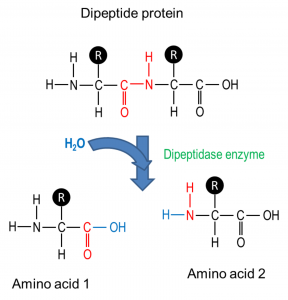
Chemical digestion breaks down large food molecules into their respective chemical building blocks, called monomers, that can be absorbed. The enzymes responsible for chemical digestion are released both by glands found within the gastrointestinal tract and by the accessory glands that secrete molecules into the gastrointestinal tract. It is important to remember that the enzymes of the digestive system are produced and secreted in an inactive form, to be activated only in the lumen, thus preventing the digestion of the cells themselves.
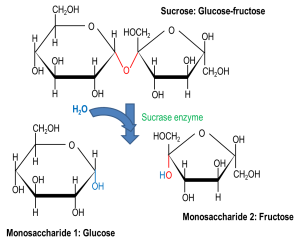
As you learned in the chapter on biochemistry and metabolism, hydrolysis refers to the breakdown of a molecule where the water breaks a covalent bond. Hydrolysis can happen spontaneously, but the breakdown of food into macromolecules and monomers occurs by enzymatic hydrolysis – where an enzyme catalyzes the hydrolysis reaction. Hydro- is part of the name because a water molecule is added to each molecular bond that is broken or -lysed. More specifically, hydrolysis splits a molecule of water to help break chemical bonds in a larger molecule. Usually, an H+ is attached to one of the components and an OH– group to the other. Hydrolysis reactions are important for many other physiologic processes in the body in addition to the breakdown of food molecules.
Did I Get This? 12.2
Why is hydrolysis an important part of the digestion process?
- It builds enzymes that help with digestion.
- It creates the cellular energy needed to fuel digestion.
- It breaks macromolecules down so they can be absorbed.
- It always requires enzymes to build new molecules.
Why would digestive system enzymes be produced in an inactive form and only activated by pH or another enzyme once they are secreted into the digestive tract lumen?
The nutritive organic compounds in our food include carbohydrates, proteins, and lipids. These molecules are digested, then absorbed, and reassembled into macromolecules or used as fuel for metabolism in the body. The process of breaking down these macromolecules involves splitting into smaller molecules using water molecules, thus the name hydrolysis (“hydro” = water; “lysis” = splitting). The reverse reaction, called dehydration synthesis, can build macromolecules from the absorbed building blocks. Enzymes can speed up the rate of these reactions.
(Credit: OLI-CMU, CC BY 3.0)
Carbohydrates
Disaccharides are two monosaccharides bound together and include sucrose (table sugar), lactose, and maltose. Polysaccharides are long chains of monomers and include polymerized glucose in different forms including glycogen, which is the stored form of glucose in our bodies, and starch, a polysaccharide of glucose molecules that comes from plant sources.
In many places around the world, starch accounts for the largest portion of digestible carbohydrates in the diet, with the addition of some glycogen, disaccharides, and monosaccharides. There are other polysaccharides in our diet, like cellulose, but our bodies do not produce enzymes that can break them down, so they are indigestible. While indigestible polysaccharides do not give us any nutrients, they do provide bulk (fiber) that helps propel food through the digestive system. In addition, intestinal bacteria are able to extract some nutrition from these plant fibers and produce vitamins that we absorb.
Example: Lactose Intolerance
Learn By Doing 12.7
Disaccharides that are not processed in the digestive system can cause what dietary condition?
- diarrhea
- constipation
- altered color of stool
- increased amounts of polysaccharides
Why can’t there be a single enzyme to break down the three common disaccharides?
- There is only one enzyme to break down disaccharides; the other enzymes break down starch.
- One disaccharide is too small to be broken down by these enzymes.
- Enzymes are substrate specific.
- Bacterial enzymes are required to break down lactose.
The excess sugars in the body are converted into glycogen and stored for later use in the liver and muscle tissue. Glycogen stores are used to fuel prolonged exertions, such as long-distance running, and to provide energy during food shortages. Additional sugars can be converted into fat and stored under the skin for insulation and can be used as energy reserves.
Proteins
(Credit: OLI-CMU, CC BY 3.0)
We get protein when we eat meat, seafood, eggs, beans, nuts, and soy products. USDA recommends 5 to 6 ounces of protein per day, although children need less. Dietary protein is usually in the form of polypeptides and must be digested into its amino acid building blocks for absorption. Protein digestion begins in the stomach with the enzyme pepsin. Other enzymes in the small intestine break large proteins into smaller peptides and then into amino acids.
Amino acids are then absorbed from the digestive system into the circulatory system where they are delivered throughout the body. Once amino acids have entered cells throughout the body; they are bonded together to make proteins needed for cell function. As a last resort, proteins and amino acids can also be used as energy. They are metabolically converted to glucose before they are used as energy sources.
Learn By Doing 12.8
Digestion of proteins begins:
- In the stomach
- In the large intestine
- In the small intestine
- In the mouth
Lipids and Fats
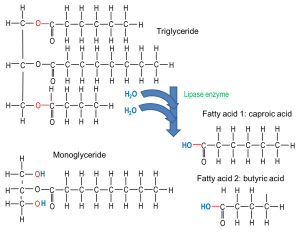
(Credit: OLI-CMU, CC BY 3.0)
Fats add flavor to food and promote a sense of satiety or fullness. Fatty foods are also significant sources of energy, and fatty acids are required for the construction of lipid membranes. Fats are also required in the diet to aid the absorption of fat-soluble vitamins and the production of fat-soluble hormones.
Dietary lipids include fats and oils. While not considered a USDA food group, oils contain some essential nutrients and are recommended as part of a healthy diet, although only in small amounts. Solid fats have more saturated and trans-fatty acids and are considered empty calories when included in a diet because they add calories but are not needed nutrients. Most dietary lipids are in the form of triglycerides, with one glycerol molecule and three fatty acids bound together. Lipids are processed by enzymes secreted from the pancreas (with some enzymes from the stomach and saliva) and are then solubilized for absorption by salts secreted in bile (from the liver). These steps prepare them for absorption in the small intestine. Like proteins, ingested lipids are broken down into smaller parts for absorption and then are either metabolized to make energy or are used to make cellular structures including cell membranes. Lipid absorption is also required for the absorption of some fat-soluble vitamins.
Learn By Doing 12.9
The most common dietary lipids are:
- Triglycerides
- Cholesterol
- Pigments
- Waxes
Nucleic Acids
When we eat any plant or animal foods, we are able to digest the DNA or RNA nucleic acid that was in their cells. The fundamental unit of nucleic acids is the nucleotide, with a phosphate group, a pentose sugar, and one of 5 nucleic bases. The pancreas produces and releases into the small intestine two enzymes to break down either DNA (deoxyribonuclease) or RNA (ribonuclease) into individual nucleotides. Enzymes produced by cells lining the small intestine further digest the nucleotide into its molecular components for absorption.
Learn By Doing 12.10
What type of food are nucleic acids found in?
- DNA and RNA are not nucleic acids.
- DNA and RNA are found in animals only.
- DNA and RNA are found in vegetables only.
- DNA and RNA are found in all once-living things.
While the animal body can synthesize many of the molecules required for function from precursors, there are some nutrients that must be obtained from food. These nutrients are termed essential nutrients, meaning they must be eaten because the body cannot produce them. Essential nutrients include some fatty acids, some amino acids, vitamins, and minerals.
Did I Get This? 12.3
Which of the following macromolecules are used for the functions listed below?
- Carbohydrates
- Proteins
- Lipids
- All of the above
Energy?
Quick energy?
Sustained and stored energy?
Can it be converted for energy as a last resort?
Needed for the absorption of certain vitamins?
Used to make cellular structures?
Tissue Layers of the Gastrointestinal Tract
Learning Objective
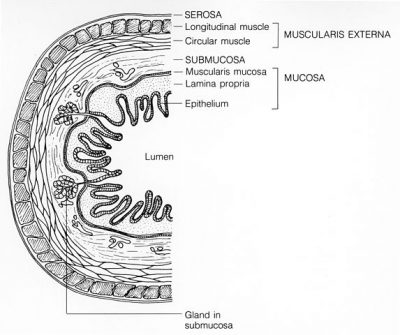
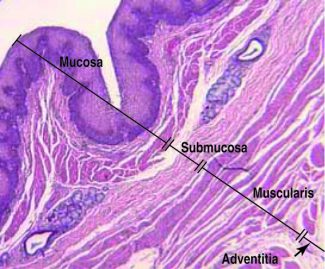
The walls of the GI tract are made of the same four fundamental tissue layers. From the lumen of the GI tract outward, these layers are the mucosa, submucosa, muscularis, and serosa.
Mucosa
The mucosa is a mucous membrane that makes up the inner lining of the GI tract. It has three layers: (1) the epithelium, made of closely packed cells without a blood supply or nerves in direct contact with the foodstuffs that enter the GI tract; (2) the lamina propria (lamina = layer, propria = proper),a layer of loose connective tissue that supports the epithelial cells; and (3) a thin smooth muscle layer called the muscularis mucosae.
Every five to seven days, the harsh chemical and mechanical environment of the GI tract causes epithelial cells to be sloughed off and replaced by new ones. Epithelial cells are interspersed with exocrine cells that secrete mucus and digestive fluid into the lumen (interior space) of the alimentary canal and with endocrine cells that secrete hormones and local signaling molecules. In the mouth, pharynx, esophagus, and the distal portion of the anal canal, the epithelium is primarily non-keratinized stratified squamous epithelium. In the stomach and intestines, it is simple columnar epithelium whose cells participate in secretion and absorption. In addition to connective tissue, the lamina propria of the mucosa contains numerous blood and lymphatic vessels, which transport nutrients absorbed into the GI tract to the liver. The lamina propria also contains many immune cells.
The muscularis mucosae layer is not responsible for the movement of material through the GI tract, but it controls how much surface area is exposed to material in the lumen. Small alterations in the many small folds in the mucous membrane of the stomach and small intestine increase the surface area available for digestion and absorption.
 (Image courtesy of Dr. Allan Wiechmann, University of Oklahoma Health Sciences Center, via OLI-CMU, CC BY 3.0) |
 (Credit: Cenveo, licensed CC BY 3.0 United States) viaOLI-CMU) |
Submucosa
The submucosa binds the mucosa to the muscularis externa. It is composed of loose connective tissue and includes blood and lymphatic vessels (which transport absorbed food molecules) and the submucosal plexus (which is part of nervous system control).
Muscularis
In the mouth, pharynx, and superior and middle esophagus, the muscularis externa contains skeletal muscle that we use for voluntary swallowing. The external anal sphincter is also made of skeletal muscle, giving us voluntary control of defecation. In the rest of the GI tract, the muscularis externa is smooth muscle, which contracts involuntarily to break down food, mix it with digestive juices, and move it along the GI tract. Complementary muscles in longitudinal (along the length of the tract) and circular layers create peristalsis – the wave-like muscular movements to move food from the esophagus to the anus.
Serosa
The serosa is the outermost layer of the GI tract, covering the parts of the GI tract that are exposed to the abdominal cavity. This serous membrane is made up of loose connective tissue and simple squamous epithelium (mesothelium). The serosa produces fluid to lubricate the outer surface of the GI tract so that it can slide against nearby organs. The esophagus has a single layer of tough connective tissue called the adventitia; it does not have a serosa.
The peritoneum is the largest serous membrane in the body and lines the abdominal cavity. The tissue has several components including the mesothelium and an underlying supporting loose connective tissue layer. The connective tissue in turn has two layers: the parietal peritoneum, which lines the abdominal wall, and the visceral peritoneum, which covers some organs and serves as their serosae. The peritoneal cavity is the small space between the parietal and visceral peritoneum that contains lubricating serous fluid.
The peritoneum includes large folds that bind organs to each other and to the abdominal walls. This keeps the organs in the proper place and suspends them when we are upright. Within these folds are blood vessels, lymphatic vessels, and nerves that innervate the abdominal organs. Among the major peritoneal folds is the mesentery. The mesentery attaches the small intestine to the posterior abdominal wall and contains blood and lymphatic vessels, as well as lymph nodes.
Learn By Doing 12.11
Which two layers of the GI tract include nerve endings of the autonomic nervous system?
- mucosa and submucosa
- submucosa and muscularis
- mucosa and serosa
- muscularis and serosa
Hint: These nerves would control the contraction of smooth muscle tissue.
Which two layers are made up of epithelial cells?
- submucosa and muscularis
- muscularis and serosa
- mucosa and serosa
- mucosa and submucosa
Hints: Remember epithelial cells will be on the inner lumen or outer surface of organs.
Which layer is not properly matched with its description?
- Submucosa- contains three layers
- Serosa- superficial layer that is exposed to the abdominal cavity
- Muscularis- responsible for movement in the GI tract
- Mucosa- the inner lining of the GI tract
Describe the role of the peritoneal folds.
The easiest way to understand the digestive system is to divide its organs into two main categories. The first group is the organs that make up the alimentary canal. Accessory digestive organs comprise the second group and are critical for orchestrating the breakdown of food and the assimilation of its nutrients into the body. Accessory digestive organs, despite their name, are critical to the function of the digestive system.
The Gastrointestinal Tract: Oral Cavity, Pharynx, and Esophagus
Learning Objective
- Describe the pathway of the bolus from mouth to stomach, identifying major structures and describing their role in facilitating the process of swallowing.
- Distinguish between the naso-, oro-, and laryngopharnx.
- Explain the process of swallowing, including the changes in the position of the glottis and larynx that prevent aspiration and peristalsis.
(Credit: Cenveo, CC BY 3.0 United States, via OLI-CMU)
The lips, also called labia (“fleshy borders”), encircle the opening of the mouth. Their outer covering is skin, and their inner lining is a mucous membrane. Between these two layers is the orbicularis oris muscle. The cheeks make up the oral cavity’s lateral walls. The outer covering of the cheeks is the skin, and the inner covering is the mucous membrane. This membrane is made up of non-keratinized stratified squamous epithelium; the multiple layers are resistant to abrasion. Between the skin and mucous membranes are connective tissue, fat tissue, and cheek muscles.
Both mechanical and chemical digestion begin in the mouth or oral cavity, which is the point of entry of food into the digestive system. The cheeks, tongue, hard palate, and soft palate frame the oral cavity or buccal cavity. The mouth is involved in both mechanical and chemical digestion. Mechanical digestion consists of mastication (chewing), in which the tongue manipulates food, the teeth grind it, and saliva mixes with it. Mastication turns food into an easy-to-swallow bolus and breaks the food into smaller pieces so that there is more contact area for digestive enzymes.
The cheeks make up the oral cavity’s lateral walls. The outer covering of the cheeks is the skin, and the inner covering is the mucous membrane. This membrane is made up of non-keratinized stratified squamous epithelium; the multiple layers are resistant to abrasion. Between the skin and mucous membranes are connective tissue, fat tissue, and cheek muscles.
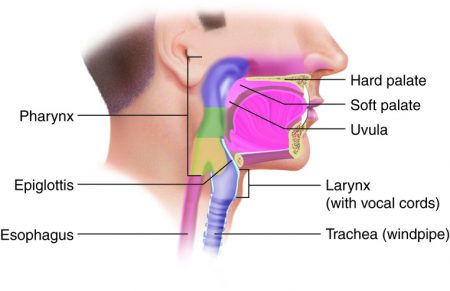
The septum that separates the oral cavity and nasal cavity is called the palate. (Anatomically, a septum (plural, septa) is a wall within a single organ or cavity that separates the space into distinct sides.) The palate, which forms the roof of the mouth, is what allows us to breathe while chewing food. The anterior part of the roof of the mouth is called the hard palate. It is created by the maxillae and palatine bones and is covered by mucous membranes. The hard palate makes up the bony wall between the oral and nasal cavities. The posterior part of the roof of the mouth, the soft palate, is also lined with mucous membranes. This arch-shaped muscular structure forms a dividing wall between the oropharynx and nasopharynx. The uvula (Latin for ‘little grape’) is a cone-shaped muscular process that hangs from the end of the soft palate. It plays a role in the speech and articulation of words. It also plays a role in preventing foods and liquids from entering the nasal cavity during swallowing.
Tonsils are also located in the oral cavity. Made of lymphatic tissue whose function is to monitor material materials entering the body, they form part of the immune system’s first line of defense against pathogens (disease-causing microbes). Most prominent are the palatine tonsils (adenoids). Another set of tonsils, the lingual tonsils, are located at the base of the tongue.
Chemical digestion begins during chewing as food mixes with saliva produced by the salivary glands. The chewing and wetting action provided by the teeth and saliva prepare the food into a mass called the bolus for swallowing. The tongue helps in swallowing—moving the bolus from the mouth into the pharynx. The pharynx opens to two passageways: the esophagus and the trachea. The esophagus leads to the stomach, and the trachea leads to the lungs. The epiglottis is a flap of tissue that covers the tracheal opening during swallowing to prevent food from entering the lungs.
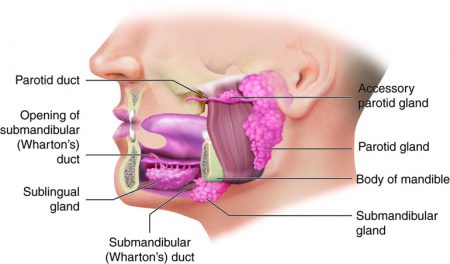
Lying outside the oral mucosa are the three pairs of major salivary glands, which secrete the majority of saliva into ducts that open into the mouth. The parotid glands lie between the skin and the masseter muscle near the ears. They secrete saliva into the mouth through the parotid duct, which is located near the second upper molar tooth. The submandibular glands, which are in the floor of the mouth, secrete saliva into the mouth through the submandibular ducts near the lower central incisor. The sublingual glands, which lie below the tongue, use the lesser sublingual ducts to secrete saliva into the oral cavity.
Example: Mumps, Homeostatic Imbalances of the Parotid Glands
Infections of the nasal passages and pharynx can attack any salivary glands. The parotid glands are the usual site of infection with the virus that causes mumps (Paramyxovirus). Mumps manifests with enlargement and inflammation of the parotid glands, causing the characteristic swelling between the ears and the jaw. Symptoms include fever and throat pain, which can be severe when swallowing acidic substances such as orange juice.
In about one-third of men who are past puberty, mumps also causes testicular inflammation, typically affecting only one testis and thus rarely resulting in sterility. The incidence of mumps has dropped considerably since 1967 when a vaccine was introduced.
Saliva is mainly water, which dissolves chemicals in the food. Only dissolved chemicals can activate the different kinds of taste receptor cells on the tongue, palate, and other parts of the mouth and pharynx. Saliva also contains mucus, electrolytes typically found in blood plasma, as well as some digestive enzymes, metabolic waste products, and immune molecules. Each of these contributes to the various functions of saliva.
Bicarbonate and phosphate ions help maintain the pH of saliva as neutral or slightly basic (average 7.4 pH). This not only helps protect the teeth from acidic substances eaten and plaque bacteria that grow best in an acidic environment but also maintains the optimal pH for the enzyme amylase. Salivary amylase starts breaking complex carbohydrates, like starch, into sugars. This enzymatic activity will stop once the bolus is swallowed and reaches the acidic environment of the stomach.
Mucus in the saliva is composed of glycoproteins and helps moisten the food, so it can be manipulated into a mass for swallowing. It also helps lubricate the movement of food through the pharynx and esophagus by peristalsis. Lysozyme antimicrobial enzymes and antibodies in the saliva help combat pathogens that might enter the body with food or drink. Like the sweat glands, salivary glands play a role in some metabolic waste excretion, so urea and ammonia are also found in saliva.
The table below summarizes the influence that oral cavity structures have on digestion.
| Structure | Action | Outcome |
| Lips and cheeks | Confine food between teeth | Foods are broken up evenly during chewing |
| Salivary glands | Secrete saliva | Moistens and lubricates the lining of the mouth and pharynx Maintains a slightly basic pH Moistens, softens, and dissolves food so we can taste Cleans mouth and teeth Salivary amylase breaks down starch |
| Tongue muscles and Taste Buds | Tongue moves sideways, in and out, and elevates posteriorly | Maneuvers food for chewing Shapes food into a bolus Maneuvers food for swallowing Taste |
| Teeth | Cut, tear, and crush food | Breaks down solid food into smaller particles for swallowing |
| Tonsils | Monitor inhaled and ingested substances for pathogens | Alert the body’s immune system to the presence of disease-causing microbes |
| Uvula | Moves up during swallowing | Blocks entry by food or liquid into the nasal cavity |
Learn By Doing 12.12
Which is not a function of saliva?
- begin the digestion of protein
- moistening to assist in the formation of a bolus
- clean the mouth and teeth
- lubricate tongue and lips for movement during speech
Hint: Saliva is a mixture of fluids, including mucus, water, and enzymes.
Which structure separates the oropharynx and the nasopharynx?
- Soft palate
- Lingual tonsils
- Hard palate
- Labia
Which of the following actively participates in mechanical digestion? (Pick all that apply.)
- Lips and cheeks
- Salivary glands
- Teeth
- Tonsils
- Tongue Muscles
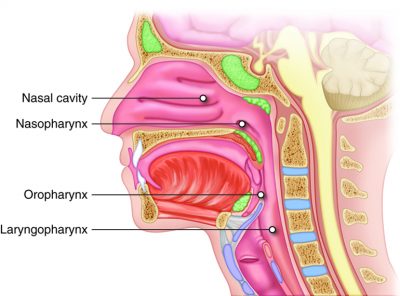
The pharynx (throat) is a funnel-shaped tube that runs from the internal nostrils to the esophagus posteriorly and to the larynx anteriorly. The pharynx has three subdivisions: the nasopharynx, the oropharynx, and the laryngopharynx. The nasopharynx acts as a passageway for air during breathing, while the other two subdivisions participate in both breathing and digestion. Superiorly, the oropharynx is connected with the nasopharynx, inferiorly with the larynx and laryngopharynx, and anteriorly with the mouth.
When swallowed food enters the oropharynx and laryngopharynx, it provokes contractions of the pharyngeal constrictor muscles that help push food into the esophagus. Usually, during swallowing, the soft palate moves back to close off the nasopharynx, while the trachea (“windpipe”) moves up under the epiglottis to cover the glottis (the opening to the larynx or voice box). This effectively blocks off air passages. But we all know what it feels like to have food “go down the wrong tube,” which means it either goes into the nasal cavities or the trachea. When food enters the trachea, our reflex reaction is to cough, which usually forces the food up and out of the trachea and back into the pharynx.
The esophagus is a collapsible tube located posterior to the trachea. This muscular tube is about 10 inches long that connects the mouth to the stomach. The esophageal mucosa is made up of stratified squamous epithelium, lamina propria, and muscularis mucosa. The mucosa near the stomach also includes mucous glands. The stratified squamous epithelium protects against abrasion and erosion from food particles. In the superior third of the esophagus, the muscularis is skeletal muscle; in the middle third it is both skeletal and smooth muscle; in the inferior third, it is smooth muscle. A slight increase in muscle thickness at either end of the esophagus creates two sphincters: the upper esophageal sphincter, made of skeletal muscle, and the lower esophageal sphincter, made of smooth muscle.
Chewed and softened food (i.e., the bolus) passes through the esophagus after being swallowed. Swallowing describes the movement of food from the mouth and into the stomach. It involves the mouth, pharynx, and esophagus and is facilitated by the secretion of mucus and saliva. There are three stages in swallowing: the voluntary phase, the pharyngeal phase, and the esophageal phase.
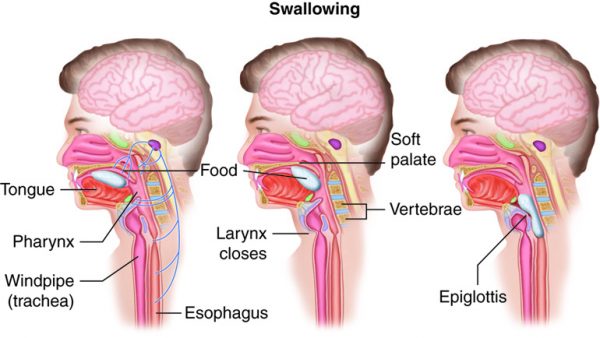
The voluntary phase of swallowing is also called the oral phase or buccal phase. In this phase, swallowing is set in motion when the tongue moves upward and backward against the palate, pushing the bolus to the back of the oral cavity and into the oropharynx. At this point, the two involuntary phases of swallowing begin.
In the pharyngeal phase, stimulation of receptors in the oropharynx sends impulses to the deglutition center (a collection of neurons that controls swallowing) in the medulla oblongata. Impulses are then sent back to the uvula and soft palate, provoking them to move upward to close off the nasopharynx. Sequential contractions of the pharyngeal constrictor muscles move the bolus through the oropharynx and laryngopharynx. Relaxation of the upper esophageal sphincter then allows food to enter the esophagus.
The entry of food into the esophagus marks the beginning of the esophageal phase of swallowing. Peristalsis propels the bolus through the esophagus and toward the stomach. The circular muscle layer of the muscularis immediately superior to the bolus contracts, pinching the esophageal wall, and forcing the bolus forward. At the same time, the longitudinal muscle layer of the muscularis inferior to the bolus also contracts, shortening this inferior area and pushing out its walls to receive the bolus. Waves of peristaltic contractions are unidirectional, moving the food toward the stomach. When the bolus nears the stomach, relaxation of the lower esophageal sphincter allows the bolus to pass into the stomach. During the esophageal phase, esophageal glands secrete mucus that lubricates the bolus and minimizes friction. Peristalsis is completely involuntary even though there is a skeletal muscle in the first 2/3 of the esophagus.
To enter the abdomen, the esophagus penetrates the sheet-like diaphragm muscle. Surrounding this orifice is the lower esophageal sphincter (also called the gastroesophageal or cardiac sphincter). Remember that sphincters are circular muscles that surround tubes and serve as valves, closing the tube when the sphincters contract and opening it when they relax. The lower esophageal sphincter relaxes to let food pass into the stomach, then contracts to prevent stomach contents from backing up into the esophagus. Surrounding this sphincter is the muscular diaphragm, which helps close off the sphincter when no food is being swallowed. When the lower esophageal sphincter does not completely close, some of the stomach contents can reflux (i.e., back up into the esophagus), causing heartburn. If reflux becomes a chronic condition, it is termed gastroesophageal reflux disease (GERD). Untreated GERD can lead to damage to the esophagus as the mucosal layer is eroded by stomach acid.
The esophagus secretes mucus that lubricates food, and it propels food into the stomach. Chemical digestion that began in the mouth continues in the esophagus, but there aren’t any new digestive enzymes secreted. The upper esophageal sphincter controls the movement of food from the pharynx into the esophagus. The lower esophageal sphincter controls the movement of food from the esophagus into the stomach. Rhythmic waves of peristalsis begin in the esophagus and then continue in the rest of the digestive tract organs. The feeling of having a lump in your throat when you are nervous is caused by peristalsis which occurs when there is no food in the esophagus.
The table below summarizes important features of esophageal function.
| Action | Outcome |
| Upper esophageal sphincter relaxation | Allows bolus to move from the laryngopharynx to the esophagus |
| Peristalsis | Propels bolus down the esophagus |
| Lower esophageal sphincter relaxation | Allows bolus from the esophagus to enter the stomach |
| Mucus secretion | Lubricates the esophagus, allowing easy passage of a bolus |
Learn By Doing 12.13
Which structure can separate the oropharynx and the nasopharynx?
- Soft palate
- Lingual tonsils
- Hard palate
- Labia
Which of these is not found in the esophagus?
- A skeletal muscle sphincter
- A smooth muscle sphincter
- Mucus-secreting cells
- Enzyme-secreting cells
Which of the following properly describes the phase of swallowing that is under voluntary control?
- The uvula and soft palate move upward to close off the nasopharynx pushing the bolus toward the esophagus.
- Peristalsis propels the bolus toward the stomach.
- The tongue moves upward and backward and pushes the bolus.
The Gastrointestinal Tract: Stomach
Learning Objectives
- Describe the pathway of the chyme through the stomach, identifying major structures and describing their adaptations and role in the various digestive activities.
- Relate the regional cell-level specializations within the digestive system to changing functions along the length of the GI tract.
- Describe how secretions from the stomach facilitate the digestion of food.
- Describe how the stomach uses a combination of mechanical force and chemicals to digest food.
The stomach is an expansion of the GI tract that lies below the esophagus. It is a very mobile structure between the relatively fixed upper and lower ends. The stomach is found between the esophagus to the first part of the small intestine (the duodenum). The stomach’s position and size are always changing. It is about as big as a large sausage when empty and stretches to hold 1 liter of food when full; the stomach has a final capacity of 2-3 liters. One of the digestive functions of the stomach is to serve as a temporary “holding chamber”. This is an important step in digestion because we can eat a meal far more quickly than it can be digested and absorbed in the small intestine. So, the stomach pushes only a small amount of food into the small intestine at a time.
The stomach plays several important roles in chemical digestion, including the continued digestion of starch and the initial digestion of proteins and triglycerides. The stomach is also where the semisolid bolus is converted to a paste-like liquid (chyme) and where some ingested substances are absorbed.
 (Credit: Cenveo, CC BY 3.0 United States via OLI-CMU) |
 (Credit: Cenveo, CC BY 3.0 United States via OLI-CMU) |
Stomach Anatomy
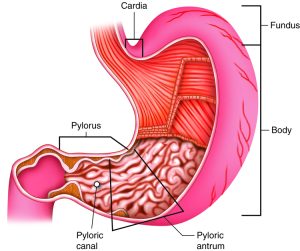
There are four main regions in the stomach: the cardia region, fundus, body, and pylorus. The cardia region is a small area surrounding the opening through which food from the esophagus enters the stomach. Lying beneath the diaphragm, superior and to the left of the cardia, is the dome-shaped fundus, which functions as a temporary storage center for food. Inferior to the fundus is the body, the large central part of the stomach. The funnel-shaped pylorus connects the stomach to the first section of the small intestine. The smooth muscle pyloric sphincter controls stomach emptying. In the absence of food, the stomach deflates inward, and its mucosa and submucosa fall into large folds called rugae.
Adaptations of Stomach Wall
The wall of the stomach is made of the same four tissue layers as most of the rest of the GI tract but with adaptations to the mucosa and muscularis externa for the unique functions of this organ. In addition to the typical circular and longitudinal smooth muscle layers, the muscularis externa has an inner oblique smooth muscle layer that runs diagonally around the organ. As a result, in addition to moving food through the GI tract, the stomach can more vigorously churn and mix food, mechanically breaking it down into smaller particles.
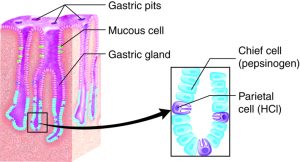
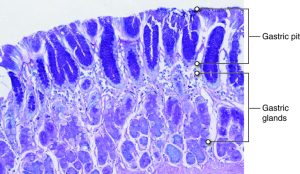
A single layer of epithelial cells forms the innermost layer of the stomach, called the mucosa. The mucosa is marked by millions of depressions called gastric pits (these are lined with epithelial cells). The gastric gland is at the bottom of the pit and produces gastric juice.
 (Credit: Cenveo, CC BY 3.0 United States via OLI_CMU) |
 (Credit: CC BY SA NC 3.0 © 2010 Regents of the University of Michigan, via OLI-CMU) |
Specialized Cells and Molecules of the Stomach
Recall that the primary macromolecule hydrolyzed in the stomach is protein. Digestion in the stomach requires a combination of acid and enzymes. In the gastric glands of the stomach, chief cells secrete the inactive enzyme pepsinogen. Parietal cells secrete hydrochloric acid (HCl). The gastric mucous cells associated with the surface and “neck” of the gastric pit secrete a thick mucus that is more alkaline than the mucus produced by goblet cells found elsewhere in epithelial tissue. This helps provide a protective mucosal barrier from the acid and protein enzymes in the gastric juice.
Protein digestion is carried out by an enzyme called pepsin in the stomach chamber. The highly acidic environment kills many microorganisms in the food and, combined with the action of the enzyme pepsin, results in the catabolism of protein in the food.HCl is responsible for the high acidity (pH1.5 to 3.5) of the stomach contents. The acidity directly kills a lot of the bacteria we ingest with food and helps denature proteins and substances found in plants. The inactive enzyme pepsinogen is modified to become the active protein enzyme pepsin in the presence of gastric juice’s low pH. The low pH of the stomach denatures the salivary amylase that was secreted in the mouth. Therefore, over time, the chemical digestion of starches will decrease in the stomach.
The stomach lining is unaffected by pepsin and acidity because pepsin is released in an inactive form (pepsinogen) that is activated by the low pH. The stomach also has a thick mucus lining secreted by both gastric gland mucosal cells and goblet cells that protect the underlying tissue. It is amazing that cells of the body can produce acids that normally would destroy the cell itself. Strong acids are also produced in cells in the immune system (to break down foreign organisms) and the skeletal system (to break down mineralized bone). High levels of acidity in the wrong places can be very destructive to living cells. Not surprisingly our body has several mechanisms to control pH.
Once the hydrochloric acid is produced in the stomach lumen, this creates a low (acidic) pH that could potentially destroy the cells in the mucosal layer of the stomach. However, there are several structural and functional components that are part of an effective mucosal barrier that protects the stomach cells and prevents the stomach from digesting itself. The thick mucus layer produced by gastric mucus cells has lots of bicarbonate ions(HCO3–) that will combine with hydrogen ions in the lumen. This stable, pH-neutral mucus layer also provides a barrier to the now-activated pepsin enzymes in the lumen as well. The surface gastric epithelial cells under the mucus layer have tight cell-to-cell junctions that prevent the reabsorption of hydrochloric acid from the lumen. Like epithelial tissue elsewhere in the body, these gastric surface cells are replaced continually by gastric stem cells that are stimulated to divide more rapidly if there is tissue damage from the gastric juice. Prostaglandins are chemical messages involved in cell inflammation response to injury. Prostaglandins produced in the stomach stimulate the production of gastric mucus and bicarbonate and promote tissue healing. When the mucosal barrier breaks down, and tissue destruction reaches into the deeper connective and muscular layers of the stomach, this is called a peptic or gastric ulcer.
Example: Ulcers, When the Mucosal Barrier Breaks Down
Aspirin and other non-steroid inflammatory drugs (NSAIDs) are known to increase the risk of gastric ulcers. NSAIDs break down the mucosal layer and reduce the secretion of bicarbonate ions by blocking the formation of prostaglandins. Even when they are enteric-coated to protect the cells from contact, they increase the risk of gastric ulcers.
As described above, the acidity of gastric juice destroys many, but not all bacteria. There is one bacterium, Helicobacter pylori, adapted to live in the stomach mucus layer. Most people have this bacterium in their stomach with no symptoms, but in some people, the bacterium is linked to an increased incidence of gastric ulcers. There is still uncertainty about why only some people are affected this way. The bacterium uses an enzyme to neutralize acid in the mucus layer locally. If the mucus becomes too acidic for the bacterium, it can also induce an inflammatory response that lowers gastric juice acidity. Once the causal link between ulcers and H. pylori was discovered, a new treatment for ulcers was implemented, and the number of gastric ulcers in developed countries fell sharply.
There is evidence to suggest that H. pylori should be considered to be colonizing the stomach, like other GI tract microbes, rather than infecting the stomach because it does have some protective effects. As the incidence of gastric ulcers fell in developed countries due to the use of antibiotics, the incidence of esophageal reflux and cancer increased. Research has shown that the presence of H. pylori is inversely related to the incidence of not only GERD and esophageal cancer but also childhood diarrhea, IBS, asthma, and even tuberculosis. So there are interesting interactions between this bacterium and its human host that need further study.
Regulation within the digestive system is tightly controlled by enteroendocrine cells. Collectively, these cells are found within the organs of the digestive system (entero- inside) rather than in “stand-alone” glands. They release hormones as well as local signaling molecules that regulate the production of digestive chemicals. The main digestive hormone of the stomach is gastrin, which is secreted in response to the presence of food. Gastrin stimulates the secretion of HCl by the parietal cells of the stomach mucosa. Other hormones influence the nervous system for global regulation of digestion. Within the stomach, the enteroendocrine cells are called G-cells.
Learn By Doing 12.14
One of the functions of the mixing waves of the stomach is to break the food up into smaller pieces. Why does this assist with chemical digestion?
- It denatures the proteins.
- It increases the surface area.
- It activates the HCl.
- Chemical digestion is not affected by the size of the food particles.
Inactive pepsinogen becomes modified to active pepsin when:
- exposed to an activating enzyme.
- exposed to low pH levels.
- exposed to high pH levels.
- exposed to a base.
Which drug would be effective in reducing gastric ulcers in someone infected with Helicobacter pylori?
- antibiotics
- antacids
- non-steroidal anti-inflammatories such as aspirin or ibuprofen
Hint: The bacterium is adapted to the acidic environment of the stomach and does not invade the cells themselves, so the drug would come in contact with the bacteria in the stomach.
If the goblet cells stopped their secretions what would happen?
- The regulation of stomach motility would be altered.
- The digestion of proteins would decrease.
- The gastric juice would damage the lining of the stomach.
Why would the digestive system protein enzymes be produced in an inactive form and only activated by pH or another enzyme once it is secreted into the digestive tract lumen?
In summary, the stomach participates in all digestive activities except ingestion and defecation. It vigorously churns food, facilitating chemical digestion. It secretes gastric juices that break down food, and it absorbs certain drugs, including aspirin and some alcohol. (Note that the stomach absorbs no nutritive molecules.) The stomach begins the digestion of protein. It stores food as an acidic liquid called chyme and releases it gradually into the small intestine through the pyloric sphincter two to six hours after eating. Only a small amount of chyme is released into the small intestine at a time. The movement of chyme from the stomach into the small intestine is regulated by hormones, stomach distension, and muscular reflexes that influence the pyloric sphincter.
The Gastrointestinal Tract: Small Intestine
Learning Objectives
- Relate the regional cell-level specializations within the digestive system to changing functions along the length of the GI tract.
- Describe the functions of the different regions of the small intestine.
- Describe how secretions from the small intestines, pancreas and the liver work together to digest nutritive molecules in food.
The word intestine is derived from a Latin root meaning “internal,” and indeed, the small and large intestine together nearly fill the interior of the abdominal cavity. The small intestine is a convoluted tube that begins just distal to the pyloric sphincter of the stomach and then loops through the central and inferior region of the abdomen before ending at the ileocecal valve, where it merges with the large intestine. The small intestine is the primary digestive organ in the body. Not only is it the part of the GI tract where digestion is completed, it is also where the majority of absorption occurs.
Although the small intestine is the longest part of the GI tract, its diameter is about half that of the large intestine, averaging a little over one inch (2.5 cm). When we are alive, the small intestine is more than 3 meters (10 feet) long – the size of a one-story building. Its length provides the expansive surface area necessary for digestion and absorption. However, circular folds, villi, and microvilli add even more surface area. With the loss of muscle tone after death, the folds of the small intestine relax, extending it to about 20 feet in length.
Gross Anatomy of the Small Intestine
The coiled tube of the small intestine is subdivided into three regions. From proximal (at the stomach) to distal, these are the duodenum, jejunum, and ileum.
The duodenum comes first and is the shortest part of the small intestine. It is less than 1 foot of the 10-foot intestine (30 cm of the 3 m). The duodenum receives the stomach contents, pancreatic juice, and bile. Chemical digestion continues in the duodenum. The chyme is mixed with pancreatic juices, which contain enzymes in an alkaline/basic solution rich in bicarbonate that neutralizes the acidity of chyme from the stomach. This result raises the pH and creates an environment that is appropriate for enzymes.
The jejunum is about 0.9 meters (3 feet) long (in life) and runs from the duodenum to the ileum. Jejunum means “empty” in Latin and supposedly was so named by the ancient Greeks who noticed it was always empty at death. This section is responsible for the absorption of a majority of nutrients. No clear demarcation exists between the jejunum and the final segment of the small intestine, the ileum.
The ileum is the longest part of the small intestine, measuring about 1.8 meters (6 feet) in length. It is thicker, more vascular, and has more developed mucosal folds than the jejunum. Vitamin B12 and bile salts are absorbed here as well as materials not absorbed by the jejunum. The ileum joins the cecum, the first portion of the large intestine, at the ileocecal sphincter (or valve). The jejunum and ileum are tethered to the posterior abdominal wall by the mesentery. The large intestine frames these three parts of the small intestine.
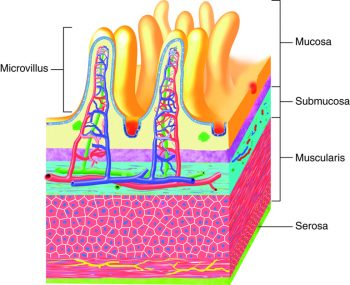
Histology of the Small Intestine
The wall of the small intestine is composed of the same four layers typically present in the alimentary system. However, three features of the mucosa and submucosa are unique. These features, which increase the absorptive surface area of the small intestine by more than 600-fold, include circular folds, villi, and microvilli. These adaptations are most abundant in the proximal two-thirds of the small intestine, where the majority of absorption occurs.
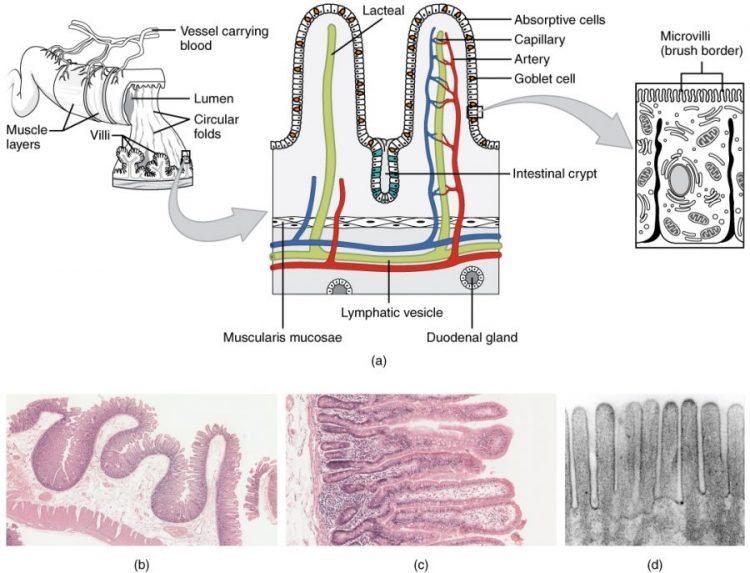
Circular folds
A circular fold (also called a plica circulare) is a deep ridge in the mucosa and submucosa. Beginning near the proximal part of the duodenum and ending near the middle of the ileum, these folds facilitate absorption. Their shape causes the chyme to spiral, rather than move in a straight line, through the small intestine. Spiraling slows the movement of chyme and provides the time needed for nutrients to be fully absorbed.
Villi
Within the circular folds are small (0.5–1 mm long) hair-like vascularized projections called villi (singular = villus) that give the mucosa a furry texture. There are about 20 to 40 villi per square millimeter, increasing the surface area of the epithelium tremendously. The mucosal epithelium, primarily composed of absorptive cells, covers the villi. In addition to muscle and connective tissue to support its structure, each villus contains a capillary bed composed of one arteriole and one venule, as well as a lymphatic capillary called a lacteal. The breakdown products of carbohydrates and proteins (sugars and amino acids) can enter the bloodstream directly, but lipid breakdown products are absorbed by the lacteals and transported to the bloodstream via the lymphatic system.
Microvilli
As their name suggests, microvilli (singular = microvillus) are much smaller (1 µm) than villi. They are cylindrical surface extensions of the plasma membrane of the mucosa’s epithelial cells and are supported by microfilaments within those cells. Although their small size makes it difficult to see each microvillus, their combined microscopic appearance suggests a mass of bristles, which is termed the brush border. Fixed to the surface of the microvilli membranes are enzymes that finish digesting carbohydrates and proteins. There are an estimated 200 million microvilli per square millimeter of the small intestine, greatly expanding the surface area of the plasma membrane and thus greatly enhancing chemical digestion and absorption.
Intestinal Glands
In addition to the three specialized absorptive features just discussed, the mucosa between the villi is dotted with deep crevices that each lead into a tubular intestinal gland. The cells that line the crevices produce intestinal juice, a slightly alkaline (pH 7.4 to 7.8) mixture of water and mucus. Each day, about 0.95 to 1.9 liters (1 to 2 quarts) are secreted in response to the distention of the small intestine or the irritating effects of chyme on the intestinal mucosa.
Mucosa-Associated Lymphoid Tissue (MALT)
In addition to adaptations to increase surface area for absorption, the mucosa of the small intestine contains a wealth of mucosa-associated lymphoid tissue (MALT). Most solitary lymphatic nodules are located in the distal portion of the ileum. In addition, groups of lymphatic nodules called Peyer’s patches are present toward the end of the small intestine, possibly because the high amounts of bacteria in that area must be prevented from entering the bloodstream.
Learn By Doing 12.15
During gastric emptying, chyme is released into the duodenum through the ________.
- lower esophageal sphincter
- cardiac sphincter
- pyloric canal
- pyloric sphincter
Match the small intestine section, either duodenum, jejunum, or ileum to the characteristics below:
- Shortest and least mobile, with input from the stomach, liver, and pancreas
Hint: This section receives food from the stomach through the pyloric sphincter. - Longest for increased transit time with continued digestion and absorption of most of the organic compounds
Hint: This is the middle section between the other two. - Location of specialized glands for secretion of bicarbonate-rich mucus
Hint: This would need to be in the section receiving the acidic material directly from the stomach. - Location of most Peyer’s patches for immune response to bacteria that might enter from the large intestine
Hint: This would need to be in the last section, connecting to the large intestine through the ileocecal sphincter.
Why would the last section of the small intestine (ilium) has the greatest concentration of lymphatic tissue for immune response to bacteria?
Hint: Think about the contents of the large intestine.
Mechanical Digestion in the Small Intestine
The movement of intestinal smooth muscles includes both segmentation and a form of peristalsis called migrating motility complexes. The kind of peristaltic mixing waves seen in the stomach is not observed here. If you could see into the small intestine when it was going through segmentation, it would look as if the contents were being shoved incrementally back and forth as the rings of smooth muscle repeatedly contract and then relax. Segmentation in the small intestine does not force chyme through the tract. Instead, it combines the chyme with digestive juices and pushes food particles against the mucosa to be absorbed. The duodenum is where the most rapid segmentation occurs, at a rate of about 12 times per minute. In the ileum, segmentations are only about eight times per minute.
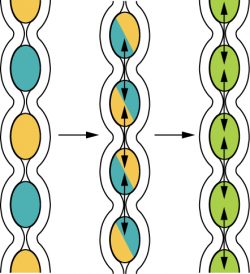
When most of the chyme has been absorbed, the small intestinal wall becomes less distended. At this point, the localized segmentation process is replaced by transport movements. The duodenal mucosa secretes the hormone motilin, which initiates peristalsis in the form of a migrating motility complex. These complexes, which begin in the duodenum, force chyme through a short section of the small intestine and then stop. The next contraction begins a little bit farther down than the first, forces chyme a bit farther through the small intestine, then stops. These complexes move slowly down the small intestine, forcing chyme on the way, taking around 90 to 120 minutes to finally reach the end of the ileum. At this point, the process is repeated, starting in the duodenum
The ileocecal valve, a sphincter, is usually in a constricted state, but when motility in the ileum increases, this sphincter relaxes, allowing food residue to enter the first portion of the large intestine, the cecum. Both nerves and hormones control relaxation of the ileocecal sphincter.
Chemical Digestion in the Small Intestine
The small intestine is the organ where the chemical and mechanical digestion of protein, fats, and carbohydrates is completed. The digestion of proteins and carbohydrates, which partially occurs in the stomach, is completed in the small intestine with the aid of intestinal and pancreatic juices. Lipids arrive in the intestine largely undigested. Lipid digestion is facilitated by bile and the enzyme pancreatic lipase.
Intestinal Juice
The intestinal glands produce intestinal juice, a mixture of water and mucus. Each day, about one to two quarts (1-2 liters) is secreted. Secretion of intestinal juice is stimulated as the small intestine is stretched by the passage of material or the irritating effects of hypertonic or acidic chyme on the intestinal mucosa. The mucus also protects the surface cells from abrasion as the food moves through the lumen. Although the intestinal juice mucus secreted doesn’t have a direct digestive function, it does play an important role as a substrate for digestion.
Extending into the mucus, but embedded in the cell membrane of intestinal cells, are various enzymes. These cell membrane surface enzymes are very important for the final digestion of organic substances before absorption. The wall of the small intestines secrete disaccharidases, which facilitate the digestion of disaccharides (e.g., maltose, sucrose, and lactose) into their respective monosaccharides.
For optimal chemical digestion, chyme must be delivered from the stomach slowly and in small amounts. This is because chyme from the stomach is typically hypertonic, and if large quantities were forced all at once into the small intestine, the resulting osmotic water loss from the blood into the intestinal lumen would result in potentially life-threatening low blood volume. In addition, continued digestion requires an upward adjustment of the low pH of stomach chyme, along with rigorous mixing of the chyme with bile and pancreatic juices. Both processes take time, so the pumping action of the stomach must be carefully controlled to prevent the duodenum from being overwhelmed with chyme.
Accessory Organs and Their Secretions
Learning Objectives
- Identify and discuss the functions of the pancreas and its structures.
- Identify and discuss the functions of the liver and its structures.
- Identify and discuss the functions of the gall bladder.
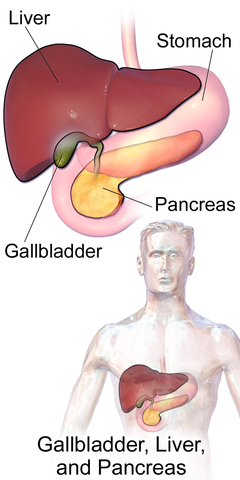
(Credit: BruceBlaus, WikiJournal of Medicine 1 (2). DOI: 10.15347/wjm/2014.010, CC BY 3.0)
Chemical digestion in the small intestine relies on the activities of three accessory digestive organs: the liver, pancreas, and gallbladder. The digestive role of the liver is to produce bile and export it to the duodenum. The gallbladder primarily stores, concentrates, and releases bile. The pancreas produces pancreatic juice, which contains digestive enzymes and bicarbonate ions, and delivers it to the duodenum. Pancreatic juices contain several digestive enzymes (amylase, trypsin, and lipase) that break down starches, proteins, and fats, respectively.
Pancreas
The soft, oblong, glandular pancreas lies transversely behind the stomach. Its head is nestled into the “c-shaped” curvature of the duodenum with the body extending to the left about 15.2 cm (6 in) and ending as a tapering tail near the spleen. It is a curious mix of exocrine (secreting digestive enzymes into ducts) and endocrine (releasing hormones into the blood) functions.
The exocrine part of the pancreas arises as little grape-like cell clusters of cells located at the terminal ends of pancreatic ducts. These cells secrete enzyme-rich pancreatic juice into tiny merging ducts that form two dominant ducts. The larger duct fuses with the common bile duct (carrying bile from the liver and gallbladder) just before entering the duodenum via a common opening. A smooth muscle sphincter controls the release of pancreatic juice and bile into the small intestine.
The pancreas produces about 1.2 to 1.5 quarts (1.1 – 1.4 liters) of pancreatic juice each day. This clear, colorless liquid is mostly water, along with some salts, sodium bicarbonate, and several digestive enzymes. Sodium bicarbonate is responsible for the slight alkalinity of pancreatic juice (pH 7.1 to 8.2). The sodium bicarbonate buffers the acidic gastric juice which has arrived in the small intestine from the stomach, inactivates pepsin from the stomach, and creates an optimal pH for the activity of the digestive enzymes in the small intestine. Pancreatic enzymes are involved in the digestion of sugars, proteins, and fats. The pancreas produces protein-digesting enzymes in their inactive forms. These enzymes are activated in the duodenum. If produced in an active form, they would digest the pancreas (which is exactly what occurs in the disease pancreatitis). The enzymes that digest starch (amylase), fat (lipase), and nucleic acids (nuclease) are secreted in their active forms since they do not attack the pancreas as do the protein-digesting enzymes.
Scattered through the sea of exocrine cell clusters are small islands of endocrine cells, the islets of Langerhans. These vital cells produce the hormones insulin and glucagon.
Liver and Gall Bladder
The liver is the largest internal organ in humans, and it plays an important role in the digestion of fats and detoxifying blood. The liver produces bile, a digestive juice that is required for the breakdown of fats in the duodenum. The liver also processes the absorbed vitamins and fatty acids and synthesizes many plasma proteins.
Although produced in the liver, bile is stored and concentrated in the gallbladder. It enters the duodenum through the bile duct. Bile contains bile salts, which make lipids accessible to water-soluble enzymes. This is accomplished via a process called emulsification, a type of physical digestion. Bile keeps fat droplets from coming back together again, thus increasing the surface area available to lipase.
Bile is another accessory organ contribution to the GI tract lumen. Made by the hepatocytes (hepato- = liver, cyte = cell) of the liver, bile is stored in, concentrated, and released from the gall bladder. Unlike pancreatic juice which is produced and released as needed, bile is produced in small quantities by the liver continuously. The gall bladder stores it for release into the small intestine as needed.
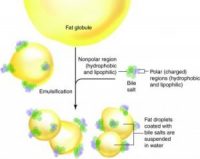
Like saliva, bile is a mixture of water with many substances, including electrolytes, bile pigments, bile salts, and lipids (including phospholipids, lecithin, and cholesterol). The bile pigments include bilirubin and biliverdin, which are waste by-products from the destruction of the hemoglobin in aged or damaged red blood cells destroyed in the liver. These wastes are then eliminated from the body with feces and contribute to its color. In addition, cells lining the bile duct secrete bicarbonate ions into the bile. However, it is the lecithin and bile salts produced from cholesterol that have a digestive function related to dietary lipids.
Recall that phospholipids in the cell membrane have a hydrophilic and hydrophobic portion. Bile salts are also amphiphilic. When they are released into the small intestine as part of the bile, the hydrophobic/lipophilic portion of the molecule is attracted to fat globules in the lumen, while the hydrophilic/lipophobic portion is attracted to the water in the digestive juice mixture. This chemical attraction and mechanical mixing break large fat globules into smaller droplets suspended in the fluid. The bile salts prevent the droplets from rejoining and thus increase the surface area of the lipid exposed to lipase enzymes, but the bile salts don’t actually digest the lipid into fatty acids and monoglycerides. This process is called emulsification.
Example: Emulsification
Once the lipids have been digested, the bile salts are still attracted to the lipid and form small micelles. These micelles come in contact with the small intestine cell membranes, releasing and facilitating the absorption of fatty acids, monoglycerides, and lipid-soluble vitamins. The bile salts are later reabsorbed in the large intestine and recycled through the hepatic portal vein back to the hepatocytes. Soluble fiber in the diet interferes with the reabsorption of these bile salts. As a result, the hepatocytes metabolize new bile salts using cholesterol from the blood, helping to lower LDL cholesterol.
There are also other mechanisms by which both soluble and insoluble fiber affect the body’s cholesterol metabolism and balance. The liver also excretes excess cholesterol in the bile. When the bile becomes supersaturated with such excess cholesterol, one of the three kinds of bile stones may form and obstruct the bile ducts. Not surprisingly, this type of gallstone is often associated with obesity. The absence of bile salts in bile results in a condition called steatorrhea, where fats remain mainly undigested in the feces and can lead to diarrhea and fat malabsorption. This condition can result from liver damage or be a side effect after the gallbladder is removed (cholecystectomy).
To summarize, chemical digestion in the small intestine cannot occur without the help of the liver and pancreas. The liver produces bile and delivers it to the common hepatic duct. Bile contains bile salts and phospholipids, which emulsify large lipid globules into tiny lipid droplets, a necessary step in lipid digestion and absorption. The gallbladder stores and concentrates bile, releasing it when it is needed by the small intestine. The pancreas produces the enzyme- and bicarbonate-rich pancreatic juice and delivers it to the small intestine through ducts. Pancreatic juice buffers the acidic gastric juice in chyme inactivates pepsin from the stomach and enables the optimal functioning of digestive enzymes in the small intestine.
The table below also summarizes the role of the accessory organs in digestion.
| Organ | Function in the Digestive Process | Outcome |
| Liver | Produces bile, which includes bile salts | Bile salts emulsify lipids for digestion and absorption |
| Pancreas | Produces pancreatic juice and sends it to the duodenum via the pancreatic duct | Pancreatic juice contains a variety of digestive enzymes |
| Gall bladder | Stores and concentrates bile | Sends bile to the duodenum via the common bile duct |
| Salivary Glands | Produce saliva | Begin to break down carbohydrates and cleanse the mouth |
Absorption of Nutrients in the Small Intestine
Each day, the alimentary canal processes up to 10 liters of food, liquids, and GI secretions, of which, only about one liter enters the large intestine. Almost all ingested food and drink, 80 percent of electrolytes, and most of the water are absorbed in the small intestine. The entire small intestine is involved in absorption, but most absorption occurs before chyme reaches the ileum. Absorption in the ileum primarily involves the recycling of bile salts. The absorptive capacity of the alimentary canal is amazing. By the time chyme passes from the ileum into the large intestine, it is essentially indigestible food residue (mainly plant fibers like cellulose) some water, and millions of bacteria.
As you’ve learned, the small intestine has a highly folded surface containing finger-like projections called villi. Cells on the top surface of each villus have many microscopic projections called microvilli. The epithelial cells at the surface of these structures absorb nutrients from the digested food and release them to the bloodstream on the other side. Passive and active transport mechanisms are used during absorption. The villi and microvilli, with their many folds, increase the surface area of the small intestine and increase the absorption efficiency of nutrients.
The monosaccharides, amino acids, bile salts, vitamins, and other nutrients are absorbed by the cells of the intestinal lining. Intestinal juice combines with pancreatic juice to provide a liquid medium that facilitates absorption. The intestine is also where most water is absorbed via osmosis. The small intestine’s absorptive cells also synthesize digestive enzymes and then place them in the plasma membranes of the microvilli. This distinguishes the small intestine from the stomach; that is, enzymatic digestion occurs not only in the lumen but also on the luminal surfaces of the mucosal cells. In general, all nutrients that enter the intestine are absorbed, whether we need them or not. Iron and calcium are exceptions; they are absorbed in amounts that fulfill the needs of our bodies.
The absorption of most nutrients through the mucosa of the intestinal villi occurs via active transport mechanisms that are driven directly or indirectly by metabolic energy. These nutrients enter the capillary blood in the villus and travel to the liver via the hepatic portal vein. An exception is certain lipids, which undergo passive absorption via diffusion and then enter the modified lymph duct in the villus (called a lacteal) to be transported to the blood in lymphatic fluid. Substances cannot be absorbed between the epithelial cells of the intestinal mucosa because these cells connect with tight junctions. This is why substances can only enter blood capillaries by passing through the epithelial cells and into the interstitial fluid.
In summary, chyme moves from the stomach to the small intestine through the pyloric sphincter. The small intestine is divided into three parts: the duodenum, the jejunum, and the ileum. It is the organ where the digestion of protein, fats, and carbohydrates is completed. The small intestine is a long tube-like organ with a highly-folded surface containing finger-like projections called the villi. Cells on the top surface of each villus have many microscopic projections called microvilli. The epithelial cells at the surface of these structures absorb nutrients from the digested food and release them to the bloodstream on the other side. Methods of transport discussed in the cell chapter (e.g., active transport) are used during this movement. The villi and microvilli, with their many folds, increase the surface area of the small intestine and increase the absorption efficiency of nutrients.
The chyme is mixed with pancreatic juices. This solution is rich in bicarbonate that neutralizes the acidity of chyme from the stomach, creating an environment optimal for the enzymes found there. Pancreatic juices contain several digestive enzymes (amylase, trypsin, and lipase) that break down starches, proteins, and fats, respectively. Bile is produced in the liver and stored and concentrated in the gallbladder. Bile contains bile salts, which make lipids accessible to water-soluble enzymes. This is accomplished via a process called emulsification, a type of physical digestion. Monosaccharides, amino acids, bile salts, vitamins, and other nutrients are absorbed by the cells of the intestinal lining.
Learn By Doing 12.16
For absorption, some molecules are absorbed without modification (directly), and some are broken down into components before being absorbed in the digestive system. Some molecules are not broken down or absorbed. For each of the molecules below, state if they are broken down, absorbed directly without being metabolized, or not metabolized.
- Lipids:
- Proteins:
- Monosaccharides:
- Water:
- Disaccharides:
- Starch:
- Cellulose:
Hepatocytes are constantly secreting:
- Mucous
- Hormones
- Pepsin
- Bile
Which chemical is produced and secreted into the small intestine to help buffer and maintain high pH for proper enzyme activity?
- Bile Salts
- Bicarbonate Ions
- Mucus
- Intrinsic Factor
Hint: This is produced and secreted in both saliva and pancreatic juice.
Lipases are enzymes that breakdown ________.
- disaccharides
- lipids
- proteins
- cellulose
Where does the majority of fat digestion take place?
- mouth
- stomach
- small intestine
- large intestine
In which part of the GI tract does most chemical digestion occur?
- stomach
- proximal small intestine
- distal small intestine
- ascending colon
Lymph absorbs _________.
- fatty acids
- sugars
- amino acids
- vitamin C
Which of the following is part of the gastrointestinal tract rather than an accessory digestive organ?
- liver
- pancreas
- pharynx
- gallbladder
Hint: The main difference is that all of the GI tract has food in some stage of digestion passing through it, while accessory digestive organ ducts pass substances into the GI tract but don’t have food passing through them.
Large Intestine
Learning Objectives
- Identify and discuss the functions of the large intestine and its structures.
- Describe the role of bacteria living in the large intestine.
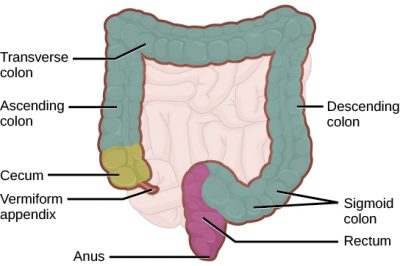
(Credit: modification of work by Mariana Ruiz Villareal, via CNX.org)
The large intestine reabsorbs the water from indigestible food material and processes the waste material. The human large intestine is much smaller in length compared to the small intestine but larger in diameter. It has three basic parts: the cecum, the colon, and the rectum. The cecum joins the ileum to the colon and is the receiving pouch for the waste matter. The colon is home to many bacteria or “intestinal flora” that aid in the digestive processes. The colon has four regions, the ascending colon, the transverse colon, the descending colon, and the sigmoid colon. The main functions of the colon are to extract water and mineral salts from undigested food and to store waste material.
The rectum stores feces until defecation. The feces are propelled using peristaltic movements during elimination. The anus is an opening at the far end of the digestive tract and is the exit point for the waste material. Two sphincters regulate the exit of feces, the inner sphincter is involuntary, and the outer sphincter is voluntary.
Cecum
The first part of the large intestine is the cecum, a sac-like structure that is suspended inferior to the ileocecal valve. It is about 6 cm (2.4 in) long, receives the contents of the ileum, and continues the absorption of water and salts. The appendix (or vermiform appendix) is a winding tube that attaches to the cecum. Although the 7.6-cm (3-in) long appendix contains lymphoid tissue, suggesting an immunologic function, this organ is generally considered vestigial. However, at least one recent report postulates a survival advantage conferred by the appendix: In diarrheal illness, the appendix may serve as a bacterial reservoir to repopulate the enteric bacteria for those surviving the initial phases of the illness. Moreover, its twisted anatomy provides a haven for the accumulation and multiplication of enteric bacteria.
Colon
The cecum blends seamlessly with the colon. Upon entering the colon, the food residue first travels up the ascending colon on the right side of the abdomen. At the inferior surface of the liver, the colon bends and becomes the transverse colon. Food residue passing through the transverse colon travels across to the left side of the abdomen, where the colon angles sharply and immediately inferior to the spleen. From there, food residue passes through the descending colon, which runs down the left side of the posterior abdominal wall. After entering the pelvis inferiorly, it becomes the s-shaped sigmoid colon, which extends medially to the midline.
Example: Colorectal Cancer
Each year, approximately 140,000 Americans are diagnosed with colorectal cancer, and another 49,000 die from it, making it one of the most deadly malignancies. People with a family history of colorectal cancer are at increased risk. Smoking, excessive alcohol consumption, and a diet high in animal fat and protein also increase the risk. Despite popular opinion to the contrary, studies support the conclusion that dietary fiber and calcium do not reduce the risk of colorectal cancer.
Colorectal cancer may be signaled by constipation or diarrhea, cramping, abdominal pain, and rectal bleeding. Bleeding from the rectum may be either obvious or occult (hidden in feces). Since most colon cancers arise from benign mucosal growths called polyps, cancer prevention is focused on identifying these polyps. The colonoscopy is both diagnostic and therapeutic. Colonoscopy not only allows the identification of precancerous polyps, and the procedure also enables them to be removed before they become malignant. Screening for fecal occult blood tests and colonoscopy is recommended for those over 50 years of age.
Rectum
Food residue leaving the sigmoid colon enters the rectum in the pelvis, near the third sacral vertebra. In the final 20.3 cm (8 in) of the alimentary canal, the rectum extends anterior to the sacrum and coccyx. Even though rectum is Latin for “straight,” this structure follows the curved contour of the sacrum and has three lateral bends that create a trio of internal transverse folds called the rectal valves. These valves help separate the feces from gas to prevent the simultaneous passage of feces and gas.
Anal Canal
Finally, food residue reaches the last part of the large intestine, the anal canal, which is located in the perineum, completely outside of the abdominopelvic cavity. This 3.8–5 cm (1.5–2 in) long structure opens to the exterior of the body at the anus. The anal canal includes two sphincters. The internal anal sphincter is made of smooth muscle, and its contractions are involuntary. The external anal sphincter is made of skeletal muscle, which is under voluntary control. Except when defecating, both usually remain closed.
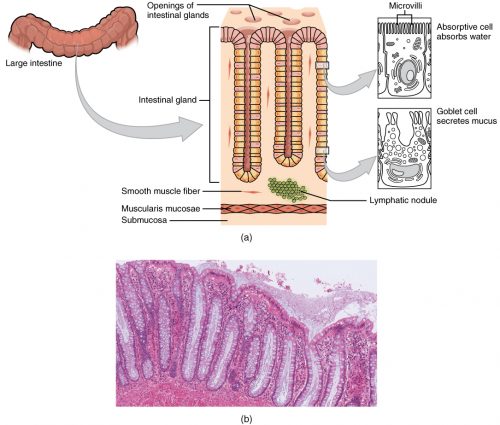
There are several notable differences between the walls of the large and small intestines. For example, few enzyme-secreting cells are found in the wall of the large intestine, and there are no circular folds or villi. Other than in the anal canal, the mucosa of the colon is simple columnar epithelium with many intestinal glands that contain a vast population of absorptive cells and goblet cells. Goblet cells secrete mucus that eases the movement of feces and protects the intestine from the effects of the acids and gases produced by gut bacteria. The absorbing cells soak up water and salts as well as vitamins produced by your intestinal bacteria.
Bacterial Flora
Lysozyme, HCl, or protein-digesting enzymes kill most bacteria that enter the alimentary canal. However, trillions of bacteria live within the large intestine and are referred to as bacterial flora. Most of the more than 700 species of these bacteria are nonpathogenic commensal organisms that cause no harm as long as they stay in the gut lumen. In fact, many facilitate chemical digestion and absorption, and some synthesize certain vitamins, mainly biotin, pantothenic acid, and vitamin K. Some are linked to increased immune response. A refined system prevents these bacteria from crossing the mucosal barrier. First, peptidoglycan, a component of bacterial cell walls, activates the release of chemicals by the mucosa’s epithelial cells, which draft immune cells, especially dendritic cells, into the mucosa. Dendritic cells open the tight junctions between epithelial cells and extend probes into the lumen to evaluate the microbial antigens. The dendritic cells with antigens then travel to neighboring lymphoid follicles in the mucosa where T cells inspect for antigens. This process can trigger a response in the lumen that blocks the commensal organisms from infiltrating the mucosa and setting off a far greater, widespread systematic reaction.
Digestive Functions of the Large Intestine
The residue of chyme that enters the large intestine contains few nutrients except water, which is reabsorbed as the residue lingers in the large intestine, typically for 12 to 24 hours. Thus, it may not surprise you that the large intestine can be completely removed without significantly affecting digestive functioning. For example, in severe cases of inflammatory bowel disease, the large intestine can be removed by a procedure known as a colectomy. Often, a new fecal pouch can be crafted from the small intestine and sutured to the anus, but if not, an ileostomy can be created by bringing the distal ileum through the abdominal wall, allowing the watery chyme to be collected in a bag-like adhesive appliance.
Chemical Digestion in the Large Intestine
Although the glands of the large intestine secrete mucus, they do not secrete digestive enzymes. Therefore, chemical digestion in the large intestine occurs only because of bacteria in the lumen of the colon. Through the process of fermentation, bacteria break down some of the remaining carbohydrates. This results in the discharge of hydrogen, carbon dioxide, and methane gases that create flatus (gas) in the colon. Flatulence is excessive flatus. Each day, up to 1500 mL of flatus is produced in the colon. More is produced when you eat foods such as beans, which are rich in otherwise indigestible sugars and complex carbohydrates like soluble dietary fiber.
Absorption, Feces Formation, and Defecation
The small intestine absorbs about 90 percent of the water you ingest (either as a liquid or within solid food). The large intestine absorbs most of the remaining water, a process that converts the liquid chyme residue into semisolid feces (“stool”). Feces are composed of undigested food residues, unabsorbed digested substances, millions of bacteria, old epithelial cells from the GI mucosa, inorganic salts, and enough water to let it pass smoothly out of the body. Of every 500 mL (17 ounces) of food residue that enters the cecum each day, about 150 mL (5 ounces) becomes feces.
Feces are eliminated through contractions of the rectal muscles. If defecation is delayed for an extended time, additional water is absorbed, making the feces firmer and potentially leading to constipation. On the other hand, if the waste matter moves too quickly through the intestines, not enough water is absorbed, and diarrhea can result. The ingestion of food-borne pathogens can cause this. In general, diet, health, and stress determine the frequency of bowel movements. The number of bowel movements varies greatly between individuals, ranging from two or three per day to three or four per week.
In summary, the main regions of the large intestine are the cecum, the colon, and the rectum. The large intestine absorbs water and forms feces and is responsible for defecation. Bacterial flora breaks down additional carbohydrate residue and synthesizes certain vitamins. The mucosa of the large intestinal wall is generously endowed with goblet cells, which secrete mucus that eases the passage of feces. The entry of feces into the rectum activates the defecation reflex.
Learn By Doing 12.17
Which of the following conditions is most likely to cause constipation?
- bacterial infection
- dehydration
- ulcer
- excessive cellulose consumption
Which part of the large intestine attaches to the appendix?
- cecum
- ascending colon
- transverse colon
- descending colon
What causes intestinal gas or flatulence?
Digestive System Homeostasis
Learning Objective
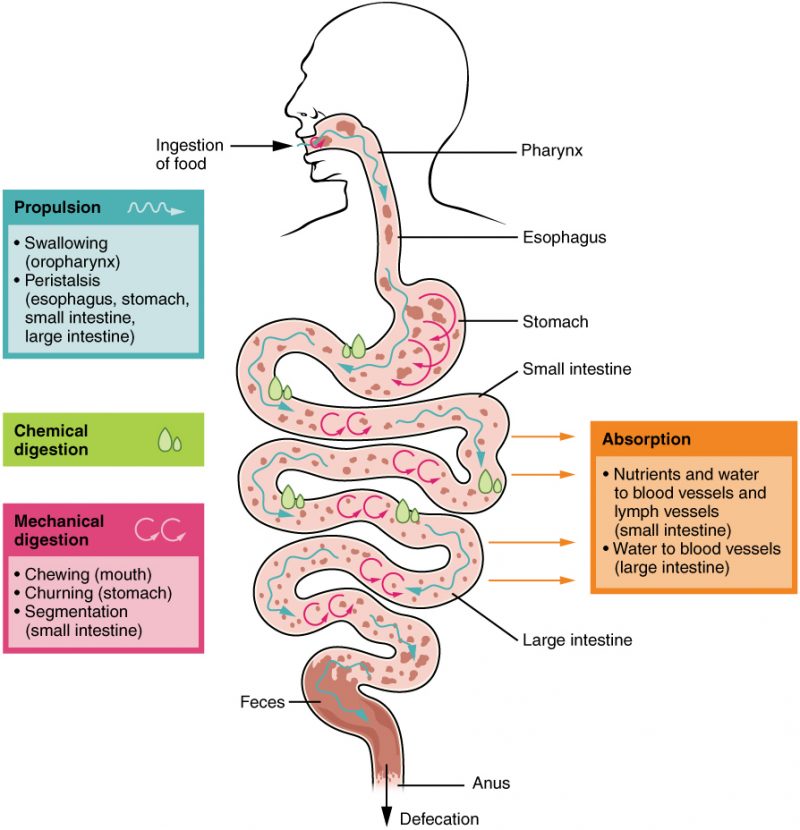
With the exception of oxygen from the respiratory system and sunlight (for vitamin D formation) from the integumentary system, we obtain all of the materials we need for growth and energy from the digestive system. It is through the digestive system that we obtain water, nutrients, and other essential building blocks for metabolism. However, as you know from day-to-day eating habits, the input into the digestive system can change greatly in amount, frequency, and content. It is up to the digestive system to have complex processes in place that help maintain homeostasis at various levels in the body.
Learn By Doing 12.18
In what structure(s) does chemical digestion occur?
In what structure(s) does mechanical digestion occur?
In what structure(s) does nutrient absorption occur?
Hormonal and Paracrine Control of Digestion
Hormonal control (for long-distance regulation) and paracrine control (for short-distance or local, regulation) help maintain processes throughout the digestive system that regulate the secretion of chemicals, mechanical changes, and absorption of nutrients.
A variety of hormones are involved in the digestive process. The main digestive hormone of the stomach is gastrin, which is secreted in response to the presence of food. Gastrin stimulates the secretion of gastric acid by the parietal cells of the stomach mucosa. Other GI hormones are produced and act upon the gut and its accessory organs. Hormones produced by the duodenum include secretin, which stimulates a watery secretion of bicarbonate by the pancreas; cholecystokinin (CCK), which stimulates the secretion of pancreatic enzymes and bile from the liver and release of bile from the gallbladder; and gastric inhibitory peptide, which inhibits gastric secretion and slows gastric emptying and motility. These GI hormones are secreted by specialized epithelial cells, called endocrinocytes, located in the mucosal epithelium of the stomach and small intestine. These hormones then enter the bloodstream, through which they can reach their target organs.
Neural Control of Digestion
Neural innervation of the GI tract is provided by the enteric nervous system and by the autonomic nervous system. The enteric nervous system is intrinsic to the digestive tract and is often called the third branch of our nervous system. It contains around 100 million motor neurons, sensory neurons, and interneurons that run from the esophagus to the anus.
Many enteric nervous system neurons are part of the reflex pathways responsible for controlling secretion and motility in response to GI tract stimuli. In these pathways, enteric nervous system sensory neuronal axons synapse with neurons of the enteric, central, or autonomic nervous system, either activating or inhibiting the activities of GI glands and smooth muscle.
The autonomic nervous system provides parasympathetic and sympathetic innervation to the GI tract. In general, parasympathetic nerves increase GI secretion and motility by stimulating neurons of the enteric nervous system, and sympathetic nerves decrease GI secretion and motility by restricting the activity of enteric nervous system neurons. When we are angry, frightened, or anxious, sympathetic innervation of the GI tract is stimulated, slowing digestive activity. Many people feel ‘butterflies’ in their stomachs (or regurgitate) when they are nervous.
Dysfunctions of Digestion Homeostasis
As an example of homeostasis maintained in the digestive system, we will consider the homeostasis of water. In the introductory units, we covered all of the important functions that water plays in our bodies. We get water from drinking liquids and from most of the foods that we eat. Water is necessary for the normal functioning of most of our tissue systems including cardiovascular fluids (blood). We lose water by exhalation (respiratory system), urination (urinary system), and feces in the digestive system. A fraction of water is retained in the digestive system to maintain movement, and water is both absorbed and secreted in the large intestine.
Diarrhea is a gastrointestinal disorder characterized by frequent watery stools. Diarrhea can occur secondary to a number of problems, including bacterial or viral infection of the gastrointestinal tract. The most common causes of these infectious diarrheas are infections with Escherichia coli or Vibrio cholera bacteria or from Rotavirus. In the large intestine, 98% of digestive system water is reabsorbed along with electrolytes and nutrients. Bacterial or viral infection interferes with the processes that control fluid reabsorption, leading to frequent, watery stools.
Infectious diarrheal disease usually occurs in older infants and children, particularly in situations where safe sources of drinking water are not available. Most children can recover from these gastrointestinal infections. However, diarrhea can lead to the loss of substantial body fluids, sodium, chloride, and other electrolytes. The loss of just 10% of body fluids can prevent the maintenance of blood pressure. Diarrhea leads to 2.2 million deaths per year throughout the world, most in children in developing countries.
Cholera is a severe diarrheal disease caused by the Vibrio cholerae bacterium. This bacterium produces a toxin that binds tightly to cells of the large intestine and prevents water absorption. Simply providing water to cholera victims does not prevent dehydration but adds to the volume of diarrhea. Proper treatment solutions contain water, salts, and glucose since all of these are responsible for the absorption of fluids.
Another example of alterations in digestive system homeostasis is age-related changes that can affect virtually every aspect of functioning. Taste buds become less sensitive, so food isn’t as appetizing as it once was. A slice of pizza is a challenge, not a treat when you have lost teeth, your gums are diseased, and your salivary glands aren’t producing enough saliva. Swallowing can be difficult and ingested food moves slowly through the alimentary canal because of the reduced strength and tone of muscular tissue. Neurosensory feedback is also dampened, slowing the transmission of messages that stimulate the release of enzymes and hormones.
Pathologies that affect the digestive organs—such as hiatal hernia, gastritis, and peptic ulcer disease—can occur at greater frequencies as you age. Problems in the small intestine may include duodenal ulcers, maldigestion, and malabsorption. Problems in the large intestine include hemorrhoids, diverticular disease, and constipation. Conditions that affect the function of accessory organs—and their abilities to deliver pancreatic enzymes and bile to the small intestine—include jaundice, acute pancreatitis, cirrhosis, and gallstones.
Did I Get This? 12.4
How do diarrheal diseases influence water homeostasis?
- Bacteria toxins prevent water absorption in the large intestine.
- Virus toxins prevent water absorption in the small intestine.
- Bacteria toxins stimulate the small intestine to excrete excess water.
- Bacteria toxins stimulate the large intestine cells to excrete excess water.
Integration of Systems, Digestive System
In addition to serving as a nutritive input for all of the body systems, the digestive system interacts with all of the systems of the body.
| Body System | Digestive System Support | Digestive System Benefits/Effects |
| Cardiovascular | Provides nutrients for the formation of plasma protein and blood cells; the liver detoxifies the blood, produces plasma proteins, and destroys old red blood cells; Hydration levels to help maintain blood pressure | Blood vessels transport nutrients from the digestive system to other parts of the body; blood supplies digestive organs |
| Endocrine | The stomach and small intestine produce hormones | Endocrine hormones help regulate secretion in digestive glands and accessory organs; insulin and glucagon control glucose storage in liver |
| Lymphatic | Provides nutrients for lymphoid organs; stomach acidity blocks entry of pathogens | Lacteals absorb fat; Peyer’s patches block entry of pathogens |
| Muscular | Provides glucose for muscle action; liver metabolizes lactic acid buildup after muscle activity | Smooth muscle contraction creates peristalsis; skeletal muscles support and protect abdominal organs; Skeletal muscles aid in swallowing and voluntary sphincter control |
| Nervous | Provides nutrients for neurons | Nerves innervate smooth muscles responsible for digestive tract movements |
| Reproductive | Provides nutrients for reproductive organs and fetal development | During pregnancy, digestive organs are crowded, causing heartburn and constipation |
| Respiratory | The shared pharynx allows breathing through the mouth | In the lungs, gas exchange provides oxygen to and excretes carbon dioxide from the digestive tract via the vascular system. |
| Skeletal | Provides calcium and other nutrients for bone growth and repair | Bones protect and support digestive organs; hyoid bone helps deglutition |
| Integumentary | It provides nutrients required by the skin, hair, and nails | The skin helps protect digestive organs and provides vitamin D for calcium absorption |
| Urinary | The liver synthesizes urea; the digestive system excretes bile pigments from liver | Kidneys convert vitamin D to its active form, allowing calcium absorption; Urinary water loss influences water available for saliva formation and chime production |
Did I Get This? 12.5
Which of the following systems is not involved in acquiring required materials from the environment?
- Respiratory system
- Digestive System
- Urinary System
- Integumentary System
Identify the system(s) responsible for each of the following:
- Transport of absorbed nutrients to tissues
- Coordination of smooth muscle activity in the gastrointestinal tract
- Absorption of lipids
- Production of vitamin D
- Absorption of oxygen
*
“Learn By Doing” and “Did I Get This?” Feedback
Did I Get This? 12.1
There are two different kinds of secretions associated with the digestive system that need to be understood to avoid confusion when describing how the digestive system functions. Which one of these secretions will be involved in the control of digestion through the blood?
- endocrine
Correct. The various endocrine hormones secreted and transported in the blood will coordinate the movement of food through the GI tract as well as the secretion of exocrine substances into the lumen.
- exocrine
Incorrect. These substances, such as enzymes, are secreted into the GI tract lumen and not into the blood.
What two body systems regulate and control the proper function of the digestive system?
- endocrine and lymphatic systems
Incorrect. The lymphatic system helps protect from any pathogens that might enter the digestive system but doesn’t regulate the digestive system’s function. - nervous and cardiovascular systems
Incorrect. The cardiovascular system does transport but doesn’t produce chemicals that control the digestive system’s function. - nervous and endocrine systems
Correct. Both of these systems produce chemical messengers to coordinate proper system function and homeostasis.
All the secretion and absorption functions of the digestive system need to be understood as happening at what level of organization?
- the cell and cell membrane
Correct. This is the level where substances are moved between the “external environment” of the GI lumen and internal body fluids. - tissues
Incorrect. This is an important structural level to study because they make up the different organs of the digestive system, but most physiology happens at a different level. - organs
Incorrect. This is an important structural level to study because the different organs of the system function together, but most physiology happens at a different level.
What structure-function concept is important at all levels of organization for very efficient absorption in the digestive system?
- accessory organ secretions
Incorrect. This will directly enhance digestion necessary before absorption can occur, but not the process of absorption. - increased surface area
Correct. The various structural features that increase the surface area exposed to the substances in the GI tract will enhance the amount of absorption that can occur while the food passes through the tube. - hormonal control of digestion
Incorrect. This will coordinate the digestion and movement of material through the GI tract but not the process of absorption. - enzyme digestion of food
Incorrect. This will directly enhance digestion necessary before absorption can occur, but not the process of absorption.
Learn By Doing 12.1
Many different digestive dysfunctions have very similar symptoms. Understanding the biochemical and cellular functions of the digestive system can help in understanding some of the various causes. Celiac disease is a digestive system disorder that is also known as gluten intolerance. Gluten is made up of amino acids and is found in wheat. When the enzyme transglutaminase reacts with gluten in the digestive system, it can cause an autoimmune response that destroys the lining of the small intestine. This causes improper absorption and associated symptoms.
Celiac disease is caused by a problem with which kind of organic compound?
- nucleic acid
Incorrect. All cells have DNA and RNA, but gluten is not a part of nucleic acid. - carbohydrate
Incorrect. Starch is a carbohydrate and gluten is not in the same group as starch. - protein
Correct. Gluten is a protein that stimulates this immune response in some people, so they have to avoid all wheat and related products.
- lipid
Incorrect. Seeds have lipids in the form of oils, but gluten is not a lipid.
Learn By Doing 12.2
Some people with Panic Disorder have been found to have an inherited metabolic defect that prevents them from producing a digestive system hormone called cholecystokinin (CCK). CCK controls the release of digestive secretions from the liver/gall bladder and pancreas into the small intestine. CCK also acts in the central nervous system, affecting neuron communication in parts of the brain that regulate anxiety and stress. People with this particular genetic condition may experience Gastro-Esophageal Reflux Disease (GERD) or Irritable Bowel Syndrome (IBS), sometimes for years before they ever have a panic attack experience.
Which function of the digestive system would be LEAST directly affected by the lack of CCK?
- elimination of residual indigestible materials
Correct. Material in the digestive lumen can still be moved for elimination; however, with improper digestion and absorption, now some material that should have been digested and absorbed will be included with the residual material, possibly leading to symptoms such as diarrhea. - regulation among different organs of the digestive system
Incorrect. This hormone plays an important role in coordinating the functions among the different parts of the system. - digestion of food into chemical building blocks
Incorrect. This will directly limit the proper release of digestive secretions from the accessory organs and make digestion within the tract less efficient. - absorption of building blocks into the body
Incorrect. If the material in the lumen is not being digested fully into the form that can be absorbed, the absorption will be less efficient.
Learn By Doing 12.3
Lactose intolerance is a digestive system disorder related to biochemical processes. In this genetic disorder, the person doesn’t produce enough lactase to digest lactose in their diet, so lactose isn’t absorbed in the small intestine. When it moves on to the large intestine, lactose upsets the water homeostasis and bacteria can metabolize it, creating various symptoms.
Lactose intolerance is caused by insufficient enzymes to digest which kind of organic compound?
- carbohydrate
Correct. Lactose is a disaccharide of glucose and galactose. - protein
Incorrect. The enzyme lactase is a protein, but the lactose it digests is not. - lipid
Incorrect. Milk does have “milk fats”, but lactose is not one of the triglycerides. - nucleic acid
Incorrect. The sugars ribose and deoxyribose combine with a nitrogen base to form nucleotides, but lactose is related to nucleic acid.
Learn By Doing 12.4
Which sphincter would not have food in some form (bolus, chyme, feces) passing through it when it relaxes?
- hepatopancreatic sphincter
Correct. The hepatopancreatic sphincter controls the emptying of bile and pancreatic juice into the duodenum, but no food passes through it. - internal anal sphincter
Incorrect. The internal anal sphincter controls the emptying of the large intestine to outside body. - lower esophageal sphincter
Incorrect. The lower esophageal sphincter connects the esophagus to the stomach. - pyloric sphincter
Incorrect. The pyloric sphincter connects the stomach to the small intestine.
Learn By Doing 12.5
Where do the processes of chemical and mechanical digestion begin and end?
- Mouth and stomach
Incorrect. Both of these structures do promote chemical and mechanical digestion but the stomach is not the last place this occurs. - Stomach and small intestine
Incorrect. The stomach and the small intestine do both perform chemical and mechanical digestion these processes begin in the mouth. - Esophagus and stomach
Incorrect. The esophagus does not produce any enzymes for chemical digestion. - Mouth and small intestine
Correct. Chemical and mechanical digestion begins with saliva and chewing in the mouth. These processes end in the small intestine with the brush border enzymes and the peristaltic waves.
Learn By Doing 12.6
Which would be the correct order from smallest to largest?
- Enzymes, ions, liver, GI tract
Incorrect. Enzymes are proteins that are macromolecules and are bigger than an ion. - Incorrect. This order would be from largest to smallest. The stomach is part of the GI tract so is smaller than it.
GI tract, stomach, bile, HCl - Epithelial cells, bile, liver, HCl
Incorrect. Epithelial cells are larger than bile which is a macromolecule. - HCl (an acid), Bile salt, secretory cell, small intestine
Correct. HCL is a small acid, then bile salts are larger macromolecules that have a steroid structure, secretory cells are larger than just macromolecules, and the small intestine is an organ that is larger than a single cell.
Did I Get This? 12.2
Why is hydrolysis an important part of the digestion process?
- It builds enzymes that help with digestion.
Incorrect. Hydrolysis may be catalyzed by enzymes, but it does not build them. - It creates the cellular energy needed to fuel digestion.
Incorrect. Although hydrolysis will release some energy during digestion, cellular energy is produced inside individual cells. - It breaks macromolecules down so they can be absorbed.
Correct. Hydrolysis is the process that breaks macromolecules into smaller parts that the small intestine can absorb. - It always requires enzymes to build new molecules.
Incorrect. Hydrolysis is involved in the breaking of chemical bonds and can happen spontaneously.
Why would digestive system enzymes be produced in an inactive form and only activated by pH or another enzyme once they are secreted into the digestive tract lumen?
Our Answer: If they were produced inside the cells and tissues in an active form, enzymes could begin to digest the cell and tissue structures of the organism before they were secreted into the digestive tract.
Learn By Doing 12.7
Disaccharides that are not processed in the digestive system can cause what dietary condition?
- diarrhea
Correct. Sugars in the large intestine increase the water content of the stool, causing diarrhea. - constipation
Incorrect. Sugars in the large intestine increase the water content of the stool causing diarrhea. A decrease in water content causes constipation. - altered color of stool
Incorrect. There are numerous digestive issues that alter the color of stool, but sugar content is not one. - increased amounts of polysaccharides
Incorrect. Humans do not produce polysaccharides from monosaccharides in the digestive system.
Why can’t there be a single enzyme to break down the three common disaccharides?
- There is only one enzyme to break down disaccharides; the other enzymes break down starch.
Incorrect. Starch is broken down by amylase and is not a disaccharide. - One disaccharide is too small to be broken down by these enzymes.
Incorrect. The shape of an enzyme’s active site rather than the size of the substrate determines if an enzyme can facilitate digestion. - Enzymes are substrate-specific.
Correct. Each enzyme can only catalyze a specific reaction, so each disaccharide would need a different enzyme. - Bacterial enzymes are required to break down lactose.
Incorrect. If the enzyme for lactose is missing, bacteria will break down these molecules for energy and cause conditions such as diarrhea.
Learn By Doing 12.8
Digestion of proteins begins:
- In the stomach
Correct. Digestion of proteins begins in the stomach with the enzyme pepsin breaking them down into polypeptides. - In the large intestine
Incorrect. Digestion does not occur in the large intestine. - In the small intestine
Incorrect. Protein digestion finishes in the small intestine as trypsin hydrolyzes polypeptides into amino acids. - In the mouth
Incorrect. Salivary amylase begins starch digestion in the mouth.
Learn By Doing 12.9
The most common dietary lipids are:
- Triglycerides
Correct. Triglycerides consisting of a glycerol molecule and three fatty acid chains are the most commonly eaten lipid; think about saturated and unsaturated fats. - Cholesterol
Incorrect. Although cholesterol is a lipid, it is not the most commonly eaten type of lipid. - Pigments
Incorrect. Although some pigments are lipids, they are not the most commonly eaten type of lipid. - Waxes
Incorrect. Although waxes are lipids, they are not the most commonly eaten type of lipid.
Learn By Doing 12.10
What type of food are nucleic acids found in?
- DNA and RNA are not nucleic acids.
Incorrect. DNA and RNA are nucleic acids. - DNA and RNA are found in animals only.
Incorrect. DNA and RNA are found in all cell types. - DNA and RNA are found in vegetables only.
Incorrect. DNA and RNA are found in all cell types. - DNA and RNA are found in all once-living things.
Correct. DNA and RNA are nucleic acids that are found in all cell types.
Did I Get This? 12.3
Which of the following macromolecules are used for the functions listed below?
- Carbohydrates
- Proteins
- Lipids
- All of the above
Energy? All of the above is correct. After the carbohydrates have been used, other macromolecules such as lipids can be broken down for energy. Proteins can also be used in this capacity although they usually are not in healthy individuals.
Quick energy? The correct answer is carbohydrates. Simple carbohydrates such as glucose and fructose can be used as quick energy because they are broken down quickly into ATP through cellular respiration. Lipids can be used for energy only after the simple carbohydrates have been used. Proteins are broken down for energy as a last resort.
Sustained and stored energy? Lipid is the correct answer. Carbohydrates such as starch and glycogen can store energy, but lipids store it more efficiently. Proteins can be broken down for energy as a last resort but have many functions other than storing energy. Lipids can be used for energy and can store the most energy because of their many hydrogen-carbon covalent bonds.
Can it be converted for energy as a last resort? Protein is the correct answer. Simple sugars are regularly used as energy while fats are regularly used as long-term energy sources. Proteins can be converted for energy as a last resort.
Needed for the absorption of certain vitamins? Lipid is the correct answer. Lipids and fats have surfactant properties so they can non-polar vitamins can dissolve in them. Carbohydrates are polar molecules and are not able to solubilize the hydrophobic vitamins. Some proteins are needed for the transport of vitamins and other hydrophobic materials. However, in the digestive system, it is primarily the lipids that solubilize the hydrophobic vitamins.
Used to make cellular structures? All of the above is correct. Structure is one of the main functions of proteins. The cytoskeleton consists of different proteins, but they are not the only macromolecules used to make cellular structures. Lipids are structural for plasma membranes, but they are not the only macromolecules used to make cellular structures. Carbohydrates are used to make cell walls in plants and parts of extracellular matrix in animals, but they are not the only macromolecules used to make cellular structures.
Learn By Doing 12.11
Which two layers of the GI tract include nerve endings of the autonomic nervous system?
- mucosa and submucosa
Incorrect. The submucosa has nerve endings, but the mucosa does not. - submucosa and muscularis
Correct. The submucosal nerve endings control the movement of muscularis mucosa for moving mucosa structures such as villi and glands, and the nerve endings in the muscularis control the movement of the circular and longitudinal smooth muscle for peristalsis. - mucosa and serosa
Incorrect. The serosa supports major nerves and blood vessels but doesn’t include nerve endings, and neither does the mucosa layer. - muscularis and serosa
Incorrect. The muscularis has nerve endings, but the serosa does not.
Which two layers are made up of epithelial cells?
- submucosa and muscularis
Incorrect. The submucosa is made of loose connective tissue while the muscularis is made of smooth muscle. - muscularis and serosa
Incorrect. The muscularis is made of smooth muscle. - mucosa and serosa
Correct. The innermost layer of mucosa and the outermost layer of serosa are both epithelial tissues. - mucosa and submucosa
Incorrect. The submucosa is made of loose connective tissue.
Which layer is not properly matched with its description?
- Submucosa- contains three layers
Correct. The submucosa is a binding layer that contains nervous system components. The mucosa consists of three layers. - Serosa- superficial layer that is exposed to the abdominal cavity
Incorrect. The serosa is exposed to the abdominal cavity. - Muscularis- responsible for movement in the GI tract
Incorrect. The muscularis layer contains smooth and skeletal muscle to move food through the digestive system. - Mucosa- the inner lining of the GI tract
Incorrect. The mucosa is the inner lining of the GI tract that consists of three layers.
Describe the role of the peritoneal folds.
Our Answer: The peritoneal folds bind the abdominal organs. This holds the organs in their places and suspends them when we are upright.
Learn By Doing 12.12
Which is not a function of saliva?
- begin the digestion of protein
- moistening to assist in the formation of a bolus
- clean the mouth and teeth
- lubricate tongue and lips for movement during speech
Which structure separates the oropharynx and the nasopharynx?
- Soft palate
Correct. The enzyme amylase in saliva only begins the digestion of carbohydrates; the lipase will only become active when it reaches the stomach pH.
- Lingual tonsils
Incorrect. This is an important function, as seen if you try to swallow something very dry like crackers without anything to drink. - Hard palate
Incorrect. The fluid helps clean as well as protect teeth because a dry mouth can result in more cavities. - Labia
Incorrect. This is an important function, as seen if you get a dry mouth because you are nervous about giving a speech in front of the class.
Which of the following actively participates in mechanical digestion? (Pick all that apply.)
- Lips and cheeks
No: Although they confine food to the area used for mechanical digestion, the lips and cheeks are not actively involved in the process. - Salivary glands
No: Salivary glands produce molecules involved in chemical digestion but do not actively participate in mechanical digestion. - Teeth
Yes: The teeth break down solid food into smaller particles for deglutition (swallowing). - Tonsils
No: The tonsils are part of the immune system. - Tongue Muscles
Yes: The muscle of the tongue maneuver food for chewing.
Learn By Doing 12.13
Which structure can separate the oropharynx and the nasopharynx?
- Soft palate
Correct. The soft palate is an arch-shaped muscular structure that divides the oropharynx and nasopharynx. - Lingual tonsils
Incorrect. The lingual tonsils are located at the base of the tongue and have an immune function. - Hard palate
Incorrect. The hard palate creates the bony wall between the oral and nasal cavities. - Labia
Incorrect. The labia are the lips that surround the opening to the mouth.
Which of these is not found in the esophagus?
- A skeletal muscle sphincter
Incorrect. The upper esophageal sphincter is a skeletal muscle sphincter. - A smooth muscle sphincter
Incorrect. The lower esophageal sphincter is a smooth muscle sphincter. - Mucus-secreting cells
Incorrect. There are mucus-secreting goblet cells to help lubricate the bolus. - Enzyme-secreting cells
Correct. There are no enzyme-secreting cells because no digestion originates in the esophagus.
Which of the following properly describes the phase of swallowing that is under voluntary control?
- The uvula and soft palate move upward to close off the nasopharynx pushing the bolus toward the esophagus.
Incorrect. The pharyngeal phase which pushes the bolus into the esophagus is under involuntary control of the deglutition center of the medulla oblongata. - Peristalsis propels the bolus toward the stomach.
Incorrect. The esophageal phase which uses peristalsis to propel the bolus toward the stomach is involuntary. - The tongue moves upward and backward and pushes the bolus.
Correct. The oral phase or buccal phase of swallowing is voluntary and occurs as the tongue moves the bolus toward the oropharynx.
Learn By Doing 12.14
One of the functions of the mixing waves of the stomach is to break the food up into smaller pieces. Why does this assist with chemical digestion?
- It denatures the proteins.
Incorrect. The chemical HCl denatures proteins. This acid unfolds proteins. - It increases the surface area.
Correct. By breaking down the food into smaller pieces, the enzymes of chemical digestion are able to more efficiently digest food. - It activates the HCl.
Incorrect. HCl is an acid that is already in its active form. - The chemical digestion is not affected by the size of the food particles.
Incorrect. The larger the molecules the smaller the surface area to volume ratio and the less effective the digestive enzymes are.
Inactive pepsinogen becomes modified to active pepsin when:
- exposed to an activating enzyme.
Incorrect. Pepsinogen is an enzyme that is activated by a change in the environment, not by another enzyme. - exposed to low pH levels.
Correct. The stomach secretes acid and pepsin needs to be active in an acidic or low-pH environment. - exposed to high pH levels.
Incorrect. The stomach secretes acid and pepsin needs to be active in an acidic or low-pH environment. - exposed to a base.
Incorrect. The stomach secretes acid and pepsin needs to be active in an acidic or low-pH environment.
Which drug would be effective in reducing gastric ulcers in someone infected with Helicobacter pylori?
- antibiotics
Correct. By killing the bacteria linked to the formation of gastric ulcers, the ulcers are able to heal. - antacids
Incorrect. These would reduce the acidity of the gastric juice temporarily but not affect the bacteria. - non-steroidal anti-inflammatories such as aspirin or ibuprofen
Incorrect. These would inhibit the symptoms of inflammation but not affect the bacteria.
If the goblet cells stopped their secretions what would happen?
- The regulation of stomach motility would be altered.
Incorrect. Gastrin regulates stomach motility. - The digestion of proteins would decrease.
Incorrect. Pepsinogen, when activated to pepsin, digests proteins. - The gastric juice would damage the lining of the stomach.
Correct. Without the protective layer of alkaline mucus produced by the goblet cells of the gastric epithelial the acidic gastric juice would damage the stomach.
Why would the digestive system protein enzymes be produced in an inactive form and only activated by pH or another enzyme once it is secreted into the digestive tract lumen?
Our Answer: If produced inside the cells and tissues in an active form, enzymes could begin to digest the cell and tissue structures of the organism before they are secreted into the digestive tract.
Learn By Doing 12.15
During gastric emptying, chyme is released into the duodenum through the ________.
- lower esophageal sphincter
- cardiac sphincter
- pyloric canal
- pyloric sphincter
Match the small intestine section, either duodenum, jejunum, or ileum to the characteristics below:
- Shortest and least mobile, with input from the stomach, liver, and pancreas
Duodenum: Food enters through the pyloric sphincter, while bile and pancreatic juice enter through the hepatopancreatic sphincter. - Longest for increased transit time with continued digestion and absorption of most of the organic compounds
Jejunum: In addition to length, the plicae circulares, villi, and microvilli also increase surface area for efficient absorption while chyme is in the small intestine. - Location of specialized glands for secretion of bicarbonate-rich mucus
Duodenum: Bicarbonate-rich mucus helps neutralize the acidic chyme entering the stomach. - Location of most Peyer’s patches for immune response to bacteria that might enter from the large intestine
Ileum: This section connects to the large intestine at the ileocecal sphincter and contains lymphatic nodules called Peyer’s patches.
Why would the last section of the small intestine (ilium) have the greatest concentration of lymphatic tissue for immune response to bacteria?
Our Answer: Bacteria live in the large intestine and could enter the ilium through the ileocecal sphincter. The chyme entering the duodenum has just come from the acidic environment of the stomach which will kill most bacteria.
Learn By Doing 12.16
For absorption, some molecules are absorbed without modification (directly), and some are broken down into components before being absorbed in the digestive system. Some molecules are not broken down or absorbed. For each of the molecules below, state if they are broken down, absorbed directly without being metabolized, or not metabolized.
- Lipids: broken down
- Proteins: broken down
- Monosaccharides: absorbed directly without being metabolized
- Water: absorbed directly without being metabolized
- Disaccharides: broken down
- Starch: broken down
- Cellulose: not metabolized
Hepatocytes are constantly secreting:
- Mucous
Incorrect. Mucous is secreted by goblet cells in the epithelial layer. - Hormones
Incorrect. Hormones are produced by endocrine glands and by special cells of the GI tract. - Pepsin
Incorrect. Pepsin is the active form of pepsinogen which is secreted by the stomach. - Bile
Correct. Hepatocytes secrete bile to assist in lipid digestion and absorption.
Which chemical is produced and secreted into the small intestine to help buffer and maintain high pH for proper enzyme activity?
- Bile Salts
Incorrect. Bile salts emulsify lipids but don’t affect the pH of the GI tract contents. - Bicarbonate Ions
Correct. Bicarbonate ions in both saliva and pancreatic juice help maintain a slightly alkaline pH for the many enzymes that don’t function at low pH.
- Mucus
Incorrect. Mucus forms a mucosal barrier that protects the tissues from stomach acid, but it doesn’t buffer the pH of the stomach contents. - Intrinsic Factor
Incorrect. Intrinsic Factor is produced in the stomach and assists in proper absorption of vitamin B 12 in the small intestine, but doesn’t affect the pH.
Lipases are enzymes that breakdown ________.
- disaccharides
- lipids
- proteins
- cellulose
Where does the majority of fat digestion take place?
- mouth
- stomach
- small intestine
- large intestine
In which part of the GI tract does most chemical digestion occur?
- stomach
- proximal small intestine
- distal small intestine
- ascending colon
Lymph absorbs _________.
- fatty acids
- sugars
- amino acids
- vitamin C
Which of the following is part of the gastrointestinal tract, rather than an accessory digestive organ?
- liver
- pancreas
- pharynx
- gallbladder
Learn By Doing 12.17
Which of the following conditions is most likely to cause constipation?
- bacterial infection
- dehydration
- ulcer
- excessive cellulose consumption
Which part of the large intestine attaches to the appendix?
- cecum
- ascending colon
- transverse colon
- descending colon
What causes intestinal gas or flatulence?
Our Answer: Through the process of fermentation, bacteria break down some of the undigested carbohydrates. This results in the discharge of hydrogen, carbon dioxide, and methane gases that create flatus (gas) in the colon. Roughly 1.5 liters are produced per day.
Learn By Doing 12.18
In what structures does chemical digestion occur?
mouth, stomach, and especially the small intestine
In what structures does mechanical digestion occur?
mouth, stomach, and small intestine
In what structures does nutrient absorption occur?
small intestine
Did I Get This? 12.4
How do diarrheal diseases influence water homeostasis?
- Bacteria toxins prevent water absorption in the large intestine.
Correct. The bacterial toxins bind to the cells and prevent the water from being absorbed into the cells of the large intestine. - Virus toxins prevent water absorption in the small intestine.
Incorrect. Diarrheal diseases result from the large intestine, not the small intestine not being able to absorb water. - Bacteria toxins stimulate the small intestine to excrete excess water.
Incorrect. Diarrheal diseases result from the large intestine, not the small intestine not being able to absorb water. - Bacteria toxins stimulate the large intestine cells to excrete excess water.
Incorrect. The toxins do not cause excess water to leave the cells; it prevents them from taking it up.
Did I Get This? 12.5
Which of the following systems is not involved in acquiring required materials from the environment?
- Respiratory system
Incorrect. The respiratory system acquires oxygen which is needed for energy production. - Digestive System
Incorrect. The digestive system takes in the majority of the material we need from the environment. - Urinary System
Correct. The urinary system is responsible for maintaining salt and water balance but does not bring in any new material into the body
- Integumentary System
Incorrect. The integumentary system absorbs sunlight which is used to produce Vitamin D.
Identify the system(s) responsible for each of the following:
- Transport of absorbed nutrients to tissues
Cardiovascular System - Coordination of smooth muscle activity in the gastrointestinal tract
Enteric and Autonomic Nervous System - Absorption of lipids
Lymphatic System - Production of vitamin D
Integumentary System - Absorption of oxygen
Respiratory System
Media Attributions
- 240px-Chocolate_cruller_doughnut
- D_M2_12Labeled
- 2426_Mechanical_and_Chemical_DigestionN
- carb_digestion
- protein_digestion
- lipid_digestion
- 573px-Mucosa
- D_M2_16
- D_M2_17
- D_M3_20B-1
- D_M3_21
- D_M3_23
- D_M3_25
- D_M3_26b
- D_M3_26a
- D_M2_11
- D_M3_28
- 2417_Small_IntestineN
- 2418_Histology_Small_IntestinesN
- 2419_Segmentation
- 240px-Blausen_0428_Gallbladder-Liver-Pancreas_Location
- D_M1_10
- Figure_16_02_03
- 2421_Histology_of_the_Large_IntestineN
