
An Overview of the IMPACT Research Program
IMPACT was a five-year research program that provided an opportunity to build upon Local Innovation Partnerships (LIPs) and research to co-create models of care to enhance access to health care for vulnerable populations. LIPs were formed to represent communities with complex challenges to the delivery of primary health care. Set in three Australian states (New South Wales, South Australia and Victoria) and three Canadian provinces (Alberta, Ontario and Québec), IMPACT began by creating learning networks of decision makers, researchers, clinicians and members of vulnerable communities in the six local health regions.
Through this program, we aimed to transform primary health care organisations to improve access to appropriate care for vulnerable populations resulting in reduced unmet need, avoidable emergency department visits and avoidable hospitalisations for vulnerable populations. Our program had four main objectives:
- To develop a network of partnerships between decision makers, researchers, clinicians, and members of vulnerable communities to support the improvement of access to primary health care for vulnerable populations;
- To identify organisational, system level CBPHC interventions designed to improve access to appropriate care for vulnerable populations and determine the potential effectiveness and scalability of the most promising organisational innovations;
- To support the selection, adaptation, and implementation of organisational innovations that align with our regional partners’ local populations’ needs and priorities; and
- To evaluate the effectiveness, efficiency, and further scalability of these organisational innovations.
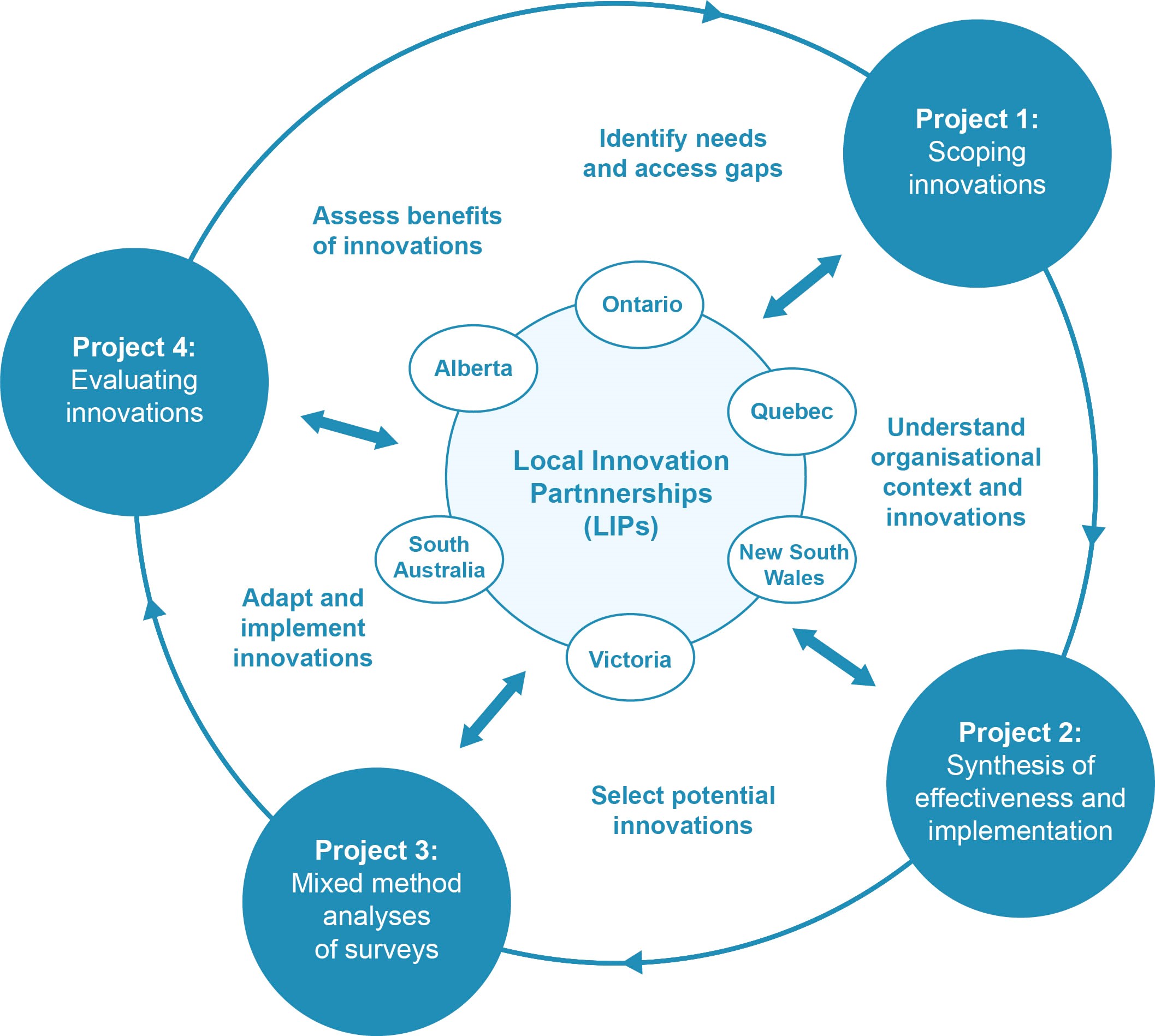
The program was based on a mixed methods approach in which qualitative and quantitative methods were combined in order to achieve the various objectives of the program. The IMPACT program of research involved four interconnected projects over five years:
- Project 1 – Scoping of organisational innovations
- Project 2 – Syntheses of effectiveness and implementation
- Project 3 – Mixed method analyses of surveys
- Project 4 – Implementation and evaluation of organisational innovations
How the projects are related to the LIPs
Critical to the achievement of IMPACT’s objectives was the engagement and creation of meaningful partnerships between researchers, decision-makers, care providers, and community representatives. Engagement and partnership was operationalised within the LIPs. Evidence generated from IMPACT’s four projects and from the activities undertaken within the LIPs informed each other.
Project 1 was based on the scoping of international innovative organisational interventions to optimise access to CBPHC for vulnerable populations. The results from Project 1 provided IMPACT’s LIPs with an understanding of the breadth of current innovative organisational interventions in CBPHC access and contextual elements related to their implementation, and the LIPs informed Project 1 to help ensure that the range of the scoping review captured the aspects of organisational interventions deemed relevant by their partners. Each LIP then developed contextually relevant interventions based on the following sources of information: local problem finding, community assessment, past experience, existing interventions, and realist reviews.
Following the scoping of organisational innovations, and in collaboration with each LIP, project 2 was based on conducting realist reviews on promising organisational interventions in different contexts to produce 6-8 potential innovative interventions for future consideration by the LIPs. This project provided knowledge about the effectiveness and potential scalability of interventions within the LIPs.
The scoping review and realist review (projects 1 and 2) allowed us to generate hypotheses about the organisational interventions that might be associated with access to CBPHC for vulnerable populations. Project 3 helped us generate an understanding of key contextual factors likely to influence access-related interventions. In order to achieve this, quantitative data from international, national, and selected provincial/state level surveys was reanalysed to assess the equity of access to CBPHC. We studied the association of access to CBPHC and vulnerability to identify jurisdictions that have had success in dealing with this issue and organisational innovations that might be associated with access. While this work was being done, each LIP documented need and mapped existing interventions for vulnerable populations. LIPs also had the opportunity to learn from each other and received emerging evidence from the empirical research program.
The last project of this research program included adapting, implementing, and evaluating promising organisational innovations. Project 4 aimed to: 1) adapt and implement the selected organisational intervention in the LIPs; and 2) evaluate the interventions developed with our partners.
The Interventions
Alberta
Local partners provided health services at pop-up events held in the community
New South Wales
Health checks and a web portal provided health information and service referrals to enhance patients’ ability to self-manage Type 2 diabetes
Ontario
Lay, bilingual navigators integrated into primary care practices supported patients to reach community resources
Quebec
Volunteer guides discussed the health and social needs of patients before their first appointment with a primary care physician
South Australia
Assessed the Dandelion project, which responded to the needs of residents of aged care facilities
Victoria
A health brokerage service matched patients from social service organisations to primary healthcare providers
IMPACT was supported through joint funding from the Australian Primary Health Care Research Institute, the Canadian Institutes of Health Research and the Fonds de recherche du Québec – Santé.
For more information and additional resources visit our website at www.impactresearchprogram.com
the consequence of the interface between the five dimensions of consumer ability and five dimensions of service accessibility (Levesque, Harris & Russell, 2013)
Access is a consequence of a dynamic process. See proposed primary health care model (Levesque et al., 2013 & Obrist et al., 2007).
Contextual and demographic factors are assumed to influence the service and consumer dimensions and need to be measured/monitored in each partnership.
The 5 dimensions of accessibility of services:
1) Approachability;
2) Acceptability;
3) Availability and accommodation;
4) Affordability;
5) Appropriateness.
The 5 dimensions of ability of consumers:
1) Ability to perceive;
2) Ability to seek;
3) Ability to reach;
4) Ability to pay;
5) Ability to engage.
Access to community-based primary health care is indicated by first-contact accessibility (primary indicator of access): The ease with which a person can obtain needed community-based primary health care (including advice and support) within a time frame appropriate to the urgency of the problem (Haggerty et al., 2007).
At a population level, access to community-based primary health care is indicated by assumed outcomes of poor access (secondary indicator of access): high rates of emergency department visits, avoidable hospitalizations and emergency department presentations for Ambulatory Care Sensitive Conditions.
groups whose demographic, geographic, economic and/or cultural characteristics impede or compromise their access to community-based primary health care services
organisations whose main function is to deliver at least primary care
In Australia: private general practices (delivering care in clinics, community services and homes), community-managed health sector (varying models for primary health care delivery; including Aboriginal Controlled Community Health Organisations).
In Canada: Clinics that provide comprehensive primary care services. These include the new primary care models established under the recent reforms (such as Family Health Teams, Groupes de médecine de famille, Primary Care Networks) as well as the traditional family practices, and community health centres.
Not limited to a particular profession within those services.
Excludes meso-level primary health care organisations whose main function is not delivery of primary health care (i.e. Medicare Locals in Australia).
community-based primary healthcare
a novel set of behaviours or routines implemented through planned and coordinated actions (based on Greenhalgh, 2004)
Excludes innovation aimed at individual practitioner behaviour changes (e.g., clinical practice, treatment innovation) if they are not intended to address one of the dimensions of service accessibility
Excludes innovations aimed at community members (e.g., general health literacy strategies)
Requires action to be planned and coordinated
May include behaviours or routines provided off-site or externally that improves accessibility of the community-based primary health care organisation (e.g., routine access to telephone translation services).
