5
Alfonso Escobar
Profesional life
After high school I spent one year of mandatory military service (lieutenant, 1954), after that I begun dental school at the Universidad de Antioquia, in January 1955 full of expectations, having in mind my father´s words the morning of the first day, “in this country every body is a doctor, always be don Alfonso, a gentleman”.
During the two first years we received all the so called basic sciences, some of the courses were given by the medical faculty (anatomy, physiology, microbiology, histology), aldo during the first two years we received dental anatomy (carving teeth from plaster blocks) and the pre-clinic in rerstorative dentistry using extracted teeth. Clinics, after the third semester were organized by departments, system with umpredictable consecuences for the patient, the tooth with the amalgam placed in the morning clinic was extracted in ther afternoon for periodontal reasons, in those days, few if any of the clinical instructor were involved in research, the criteria for selection of the faculty was success in prívate practice: The big innovation at the time was de comprehensive clinic during the fifth and last year of training, in a way is a contradicition because after two years of departamentalized clinics the message was, dentistry is something else, patients come with all kind of problems in need of logical solutions.
This curriculum had the USA classical approach to dental education; some of our clinical faculty were specialists trained there. In the fifities and sixties the Kellogg Foundation gave fellowships to faculty membres willing to do some research and receive training in basic sciences.
By law, in Colombia was mandatory (today is optional), the “rural year”, physicians, dentists and lawyers spent one year working in rural communities paid by the government. excluded from this obligation were trained clinical specialists in a recognized program in a foreign university.
In 1960, right after graduation from dental school I spent one year at the Guggenheim Dental Clinic, port of entry to USA, to many dentists like me, from different parts of the world, it was my first contact with the american way of life. From there I went to Chicago, accepted by Maury Massler as one of his postgraduate students in paediatric dentistry, pure clinical training with intense seminars in emotional growth and developolment, dental caries and pulp biology and so forth, the day I receive my certifícate as paediatric dentist, doctor Massler called me to his office, his words: “Escobar, you are not ready to go back to your country, can you stay with me one more year? I did, and spent the following year attending seminars on dental education, dental research, advance oral histology, and collaborate in an animal study publised in 1967 (1) Being part of that program I was invited to launches organized by Dean Isaac Schour, always with disitnguished speakers from abroad, one of them was a raising figure from Denmark, Jens J Pindiborg, another one, even younger, Leon Silverstone, my eyes were open to a new world of ideas unknwon to me.
Upon completion of the program Massler asked me to stay in the department as a faculty member, I declined the offer, even today I wonder if I made a mistake and returned to Medellin during the summer of 1965, in september of that year I became a faculty member at the dental school in paediatric dentistry, working at the same time in oral micobiology, since that time my interest in cariology and preventive dentistry.
I returned to Medellín in 1965, immediately I begun my academic life as a clinical instructor in paediatric dentistry (dental school, Universidad de Antioquia), the dean at that time gave me the order to choose one basic science as part of my teaching activity, I ended up with another Massler´s former student interested in oral microbiology, since then my involvment in cariology and preventive dentistry. In 1968 (circa) I was selected by the dean to participate in the Danida course at the Royal Dental College in Copenhague, this experience changed my life, for good and for ever. P.O Pedersen was the dean, Professor Erik Kissling was the head of paeditaric dentistry, Arne Bjork in Orthodontics, Ian Jacobsen was the secreatary of the course, Ingolf Moller was another profesor in the course, from my perspective the approach to take care of children through the school dental services was quite different from my experience in Medellín. One of my class mates was Otto Memendez from Guatemala, he, almost 50 years ago, implemented at Universidad San Carlos de Guatemala a program in which last year students from law, medicine, dentistry, architecture, veterinary spent the whole year working in the rural communities, occasionally supervised by instructors.
In 1970, I went back to Denmark as a WHO observer in the Danida course offered this time at the Royal Dental College in Aarhus, one of the speakers was Professor Harald Loe who became my friend of many years, Sven Poulsen was the course secretary, another speakers were Professor Jens Pindborg and Ingolf Moller, at that time Ole was not one of the speakers.
Between 1965 and 1972, three important activities were undertaken by the dental school in Medellin, (1) the creation of the first department of preventive and social dentistry in Latinamerica (2), (2) the salt fluoridation project in rural communities no to far away from Medellín and (3,4) (3) training of dental nurses, similar to the ones in New Zealand,as a result half the faculty resigned in opposition to this approach to take care of the underserve community, unfortunatelly few of them end up in private practice and the program was finally closed down.
From 1972 to 1975 I was a faculty member in the depatment of paediatric dentistry at UIC (College of Dentistry University of Illinois), hired at the same time with two Friends; asked bt yhe head of the department what would we like to do?, one took postgraduate education, the other one undergraduate clinics, I was empty handed, finally I indicated my interest in internationalize the department by organizing the Latinamerican Courses in Social Pedodontics, this program was offer to eager young faculty members interested in research and in the academic life, unable to speak english. The department offered the program 25 years under my coordination, we had over 400 students from all latina amrican countries and from Spain. With the help of another faculty member all lectures were translated from english to spanish. Invited speakers included Harald Loe (Director of NIDR), Paul Keyes, Anders Thysltrup, Leon Silverstone, Michael Newman, Maury Massler, George Gillespie (PAHO), Viron Diefenvach and many others. Participants had financial support from PAHO, Kellogg Foundation, Capes and CNPq (Brasil), some with private funds. By mutual agreetment (the Dean of the dental school, the Head of the department and myself) we decided the offer the last course to former students in the program, during the closing ceremony special recognition was given to those speakers that during 25 years participated in every single course: Paul Keyes, Harald Loe, Viron Difenvack, Indru Punwani (Head of the Department), Allen W. Anderson (Dean of the College, Guillermo Cárdenas, Alfonso Escobar (Program Coordinator).
In 1975 I returned to Colombia and to my teaching activities at Universidad de Antioquia, it was a time of turmoil, to give a lecture was imposible, Cárdenas and my name decorated the toilets, “Cardenas, Escobar, pro-imperialists, out”. We did not give up. At the end of 1976 we were as if we were interested in founding a dental school at another university, private and with excellent reputation, we met with the Rector before Christmas and decided to talk again the following year, but he never called back, instead in January of 1977 a physician who participated in the salt fluoruidation program came to our office to invite ask to explore the possibility of chartering a new dental school and a new medical school. To make the story short, by the middle of the year the “Instituto de Ciencias de la Salud, CES”, was a reality the first group of students in medicine, dentistry and nursing had the first lecture, forty years ago. Since then I have been with CES as faculty member, and former President of our Board of Trustees and of the Executive Comittee, today I belong to both guvernamental bodies. My academic life has been devoted to teaching, not to research.
Maury Massler
During over 50 years of academic life as faculty member at Universidad de Antioquia (1965-1972), University of Illinois (1972-1975); Universidad de Antioquia (1977-1978), Universidad CES of which I am one of the charter members (1978-present) I have had the unique opportunity to meet the giants than in dentistry changed our way of thinking regarding the etiology of the two most prevalent diseases in human, dental caries and periodontal diseases, both associated with the dental bio-film. In a way I was ready for those dramatic changes because I was privileged to have as my mentor and tutor another giant in dentistry, Maury Massler (1912-1990). He took me under his umbrella until 1990.
The first day as a postgraduate student (September 1962, circa), Dr. Massler came into the seminar room at 1:00 pm, sharp, took a look of the new class of pediatric dentists, went to the blackboard and wrote “Learning is a very painful experience”. Months later I was able to understand its meaning. Doctor Massler was in charge of the seminars on emtional growth and develpoment, dental caries, oral histology (mainly dental pulp), and research. He left a permanent imprint in all of us because, he was more interested in teaching us the “why” the “when” and the “what” of things, instead of the “how”. To him a dental auxilliary needs to know how to apply a gel tray with fluoride, we, as future specialists in paeditric dentistry were supossed to know when to apply the fluoride but more important to understand the cariostatic mechanism of fluoride, this is just an example of many other clinical situations. Soon we learned from him what today is called evidence based dentistry, Any time he asked a question and we begun to answer by saying “I believe” immediately we were interrupted by him: “¿I don´t care what your believes are, what is your evidence?”, it was the begining of “Evidence based medicine/dentsitry”, more than fifty years ago.
If the answer was too long, again, he interrupted us to say: “please be specific”. Her was demanding with the correct se of words, for instance he never allowed the term caries, the correct way was dental caries, becuase caries means rotten, and in that order of ideas he ended his sentence by saying “the branches of a tree can get rotten”.
In his days, literature review has to be exhaustive, one day the topic was remineralization of the enamel, when we presented our results he said, you are missing one important paper from 1910, at that time the author of the article indicated that the best way to remineralize enamel was by having the tooth clean, exposed to the oral fluids.
Today, ther big issue is to inactívate the dental caries process, 50 years ago from day one as his students, we were familiar with active and arrested lesions (He used arrested instead of inactive) (5), and his clinical indication was simple, if you want to arrest an active dentinal lesion, open up the cavity in such way that the mother can clean it, teach her how to have that molar shiny, that way “you will be helping nature do the job for that poor kid”, were his words.
Also, we learned from him that dental caries is an intermittent process characterized by periods of activity (acid production and as a consequence lost of minerals from the enamel surface and from the dentin), and periods of inactivity (no acid production, regain of lost minerals = remineralization). If the laps of time between activity and inactivity was too short, remineralization will never happens, for example in children eatin candies all day long.
“Be gentle to the pulp”, was one of his many admonitions indicating that in reality we were dealing with the pulpo-dentinal organ; adding: to my knolwedge not a single dental material can produce sclerotic and/or reparative dentin, remove the irritants, place a sedative cement, in those days we used zinc-oxide eugenol, to isolate the organ from the outside environment.
“Permanent restorations: there not such a thing, some materials last longer than others”,
Caries control: we were not allowed to place restorations of any type on one tooth at the time, every single lesión and every old restorations were removed before placing amalgamas or steel crowns, no composite at that time.(6) Caries control in my days with Massler, is not different from what 30 years later Anders Thysltrup and Lars Bjorndal, introduced as “stepwise excavation” (7,8) Again doctor Masslar was emphatic, make sure that the tooth is asymtomathic, otherwise you are going to be in trouble.
Six year old kids, thumb suckers, anterior open bite:” Forget the teeth, the problem is in the mind, ask the expert to find out why that kid still sucks his or her thumb” I think this gives an idea of the kind of true “maese”, doctor Massler was.
On the fifth floor corridors of the old dental building, corner of Wood and Polk, he prepared me for life with his counselling, one afternoon in the way home, he asked me “Escobar, what did you learn today”, I tried to answer properly and in order to do so I was taking longer than expected, his immediate reaction was: “If is taking that long to answer a simple question, means that you did not learned any thing today, promise me that fron know on you will learn something new each day”. Even today I complied to that request.
Once in a while he came to the seminar room to tell us “take the train to the loop, my friend xxxx who is the first violinist with the Chicago Orquestra is waiting for you at two o, clock, he will teach you how to listen to a concert, Sir George Solti was his director at that time. Another day was the Art Museaum, and so on.
Some of my friends and colleagues at Illinois called him Maury, today I always refer to him as doctor Massler, which reminds me of my experiences in Denmark. I atended a Danida course in 1968 held at the Royal Dental College, one day I went to present my respects to Pindborg (we met the year before in Medellin), when I came to his office his secretary said: “Will profesor Pindborg be willing to see profesor Escobar who is here? Thirty yers later I returned to the dental school at the Panum Institute to spend some time with Professor Thysltrup, whern I came to his office his secreratry said “Anders, Alfonso is here, can we come in?
TEACHING OF DENTISTRY IN COLOMBIA
The first effort to teach dentistry in Colombia, or at least in Medellín was in 1920 (circa), it was at a private dental college (Colegio Dental), chartered by an orthodontist trained in Philadelphia, since then has been evident the influence of the Northamerican dental schools way of teaching dentistry, influence to be perpetuated by the passing of years. After four years of full time education the dental students at Colegio Dental, received the title of Doctor in Dental Surgery (DDS). In one diploma from 1926 it is possible to read, at the bottom the names of the faculty, mostly physicians who were faculty members at the medical school (Antioquia University) the instruction received was in areas like pathology, oral surgery, general anatomy, bacteriology, chemistry, metallurgy, crown and bridges with orthodontics, prosthesis, operative dentistry, materia medica with anesthesia and histology, dental anatomy and dental histology, morphology, the course enumerated are clear indication of a medical orientation in the teaching of dentistry in those days. Graduates from this institution were able to solve, in the rural áreas, some medical emmergecies (suture of wounds as a result of work accidents) and also to attend deliveries
Few years later the Dental College became affiliated with Antioquia University (Universidad de Antioquia) and in 1946, part of the university as Faculty of Dentistry, today Faculty of Odontology and the degree granted was “odontólogo”, instead of “dentist”.
One of the speakers in this symposium (AE) graduated in 1960 from the dental school (Universidad de Antioquia). At that time, it was possible to study dentistry in three dental schools in Colombia, two in Bogota (National University, chartered in1932, public); and at the Javeriana University, chartered in 1950, private; or in Medellin (Universidad de Antioquia, chartered in 1947 public).
Fifteen years later, in 1975 one new dental school became approved by the government, (Universidad del Valle, public), after that and in rapid succession, Metropolitana (1977), private; CES in Medellin (1978) private; Universidad de Manizales (1979) private; Universidad Santo Tomás, Bucaramanga (1979), private; Universidad del Bosque, Bogotá (1983), private; then the number grew astronomically, one in 1994, three in 1996, four in 1997, one in 1998, three in 1999, one in 2009, 2012, 2014 and 2015 to reach 24, offering 33 programs in the country. Of those, only five are public, financed by the government; the rest are private, and of those, very few, like CES, are not for profit organizations, the rest are business like enterprises, one them, Universidad de Nariño has seven programs in different cities.
Any Institution of higher education in Colombia, in order to be allowed to enroll students and grant degrees require to be registered with the Ministry of Education, all 33 are, but only 10, (four public, six private) went to the complex process of accreditation by the National Council on Accreditation (CAN by the Spanish initial). Two in Medellin, Universidad de Antioquia and Universidad CES.
How different are the curriculums? In general terms the backbone is quite similar in all of them with a clear influence from North America: classical departments and basic sciences as a pre-requisite to start clinical work in patients during the educational process, around the fifth semester (ten semesters, in total); in must dental schools’ integration of clinics takes place during the last semester. CES is one exception in the sense that instead of clinical departments, teaching is organized in areas of integration, and the clinical experience is gained in two main comprehensive clinics, one for the adults, and the other for the child and the adolescent.
Universidad de Antioquia (public) put especial emphasis in public health and the social aspects of dentistry, train community leaders, dental hygienists and lab. technicians; Universidad del Bosque (private) claims the same approach but in reality is more clinically oriented; Universidad del Valle (public), public health; Universidad Nacional (public) goes for an equilibrium between public health and clinical activities; CES (private) strong in the integration of clinical activities from the very beginning. Our first dean (CES) has a profound dislike for specialists in dentistry, in his believe a graduate from our program should be a generalist able to solve up to 75% of oral problems affecting the population, in his opinion generalist were treated by specialists as its auxillairy personnel; at the end this approach was untenable because the Executive Committee of the University requested, that like in the school of medicine, the dental school must offered postgraduate education, today we have speciality programs in paediatric dentistry and preventive orthodontics, periodontology, endodontics, oral rehabilitation, orthodontics, oral surgery and a master of science program in dental sciences. All programs are at least two years, full time on top of fiv years of undergraduate education. The current law won´t allow to reduce the number of undergraduate education to four years.
Strong in research are Valle, Antioquia, Nacional, Javeriana, Bosque and CES.
At the national level, (national state tests related to dentistry), perform better the students from public dental schools, this year the ranking was Valle, Nacional and Antioquia, then CES (private) in fourth place. It is interesting to note that in dental education a healthy patient is considered a poor teaching case, this idea today prevails in many places.
From 2001 to 2013 the 24 dental schools graduated 18.380 dentists, an average of 1413 per year, today the total number of dentists in Colombia, with a population of 47 million is close to 60.000, which means one dentist per 783 individuals, far better than the Scandinavian countries. On the average in the country 70% of dental students are females, and 30% males, is very common to see only two or three males among 50 females, this reflects also in the large proportion of female faculty members. 85% of the total number of dentists concentrates in the four main cities of the country, as a consequence in the remote areas the rate show might be 1 dentist per 50.000 individuals.
In Colombia, dentistry as a profession lacks stamina and political power at the level where the decisions are taken (made). The divorce between the dental health policies of the Ministry of Health and what is taught at the dental schools is total to the point of creating ethical problems regarding treatment protocols.
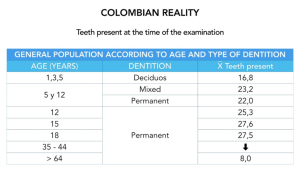
This situation brings into mind another problem, what is the role of the university in society?, it is just to train lawyers, physicians, engineers, dentists?, or should be concerned with the outcome, because in the case of dentistry is nihil as indicated by the recent national study on dental health (ENSAP IV), in spite of all kind preventive efforts the deterioration of the dentition of the Colombian population begins at age 12, losing 0.03; (average) due to dental caries, this figure increase to 3.51 in the 35 to 44 year of age, at age 45 to 64 is 8.89 in the group 65 to 79 is 17.65, this age group ends up with only 8.02 teeth present in their mouth (ENSAB IV, 2015, Colombia).
The profile of the new graduate, defined by each dental school (independently of being public or private, for profit or not for profit) is quite similar, upon graduation, dentists are expected to diagnose, treat and prevent major oral diseases, be socially responsible, permanent learner, internationally minded, educator of his (her) patients, impeccable professional attitudes and habits, high ethical values, leadership and so forth. Once out of dental school, facing the realities of live, trying to make a decent living, dreams are over; soon the new dentist discovers that only two options are available, either private practice or become employed by the private insurance companies or by the public health sector.
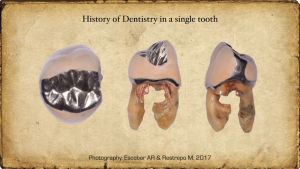
In the first case money lies in designing smiles, placing implants, unnecessarily changing amalgams for resins, bleaching teeth, all kinds of orthodontic appliances very early in the life of children, claiming excellent results with the appliances placed in the mouth when in reality normal growth and development of the craneo-facial structures did the work. The most important professional act in the health sciences, diagnosis, is given free of charge by many dentists, in order to attract patients or offering discounts at cocktail parties; the less trained dentist, the more aggressive. Those in the public sector soon realize that treatment protocols were written by dry finger dentists many times under the influence of the dental industry, unconcerned with the needs of the society. It is a sad reality as illustrated in figure 1. That patient at age 7, more than 60 years ago, had all first permanent molars in good condition, sound. In spite of regular visits to her dentist, every six months, the inexorable deterioration began, through the years the occlusal amalgam became a two surfaces restoration, then three surfaces, almost on a yearly basis, later on endo treatment and a full crown were required, by age 60 the molar was extracted for obvious reasons, today the patienm has an implant that quite provably is going be lost for the same reason that the first amalgam was placed, dental bio-film formation, in other words the technological approach, by the way very expensive, was not the solution to a biological problem. The cycle goes on and on every where in the world. In my opinion this case is a reflection of the way dentistry is tought, in the curriculum restorative treatment has more weight than precention and contro of disease processes.
Historically, in this part of the world, the teaching of preventive dentistry evolved according to the following parameters and chronology; in 1962, in 9 out 17 dental schools in Bolivia, Chile, Colombia, Ecuador, Perú and Venezuela included few hours of public health in the curriculum. In 1962 (circa) in the recently created department of preventive and social dentistry, (dental school, Antioquia University), tried to motivate dental students in social dentistry, public health, in theory the idea was to stimulate prevention as a philosophy of professional life coordinating efforts amongst different departments. The reality was that only 5.6% (306 clock hours) of the entire curriculum where dedicated to achieve such endevour by teaching biostatistics, epidemiology, public health, ecology, sociology, cultural anthropology (2)
About the same time in 44 dental schools in the USA, only six hours of topics related to preventive dentistry were included in the curriculum, in 1968 increased to 28.4 hours, later on 1979 the range of cloack hours varied between 2 and 100 (9) The believe of many clinical instructors on the topic of preventive dentistry was, “let´s dentistry concentrate in dentistry; let´s ecologists solve their problems” (10)
In 1988 In 22 dental schools, out of 56 teachiog of preventive dentistry was scattered in the departments of preventive dentistry, oral biology, general dentistry and restorative dentistry, the average of cloack hours devoted to the topic was 34 (11)
Around 1990 the dental school in Helsinki began to teach dental students how to understand dental diseases from the perspective of the community; additionally, in a unit called infectious diseases of ther teeth, dental caries and periodontal diseases were taught in a comprehensive way (Kerosuro, 2001) (12)
In 1997 the European Academy of Paediatric Dentistry included in the objectives of the teaching od paediatric dentistry the cioncept that dental students must be able to design and implement programs in preventive dentistry (13)
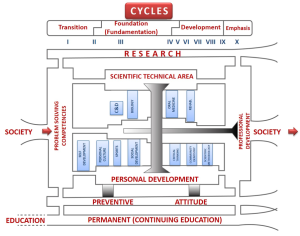
At CES, since 1978 when was chartered, the teaching at the dental school was organized by areas of integration of subjetc matter, classical departments were abolished, as a result clinical training was provided in two main clinics, integrated from the very begining, ione for the child and the adolescent, the other for the adult population (in addition, the clinic to take care of emergencies, orthodontics and oral surgery. The teaching of dental caries and periodontal disease is, and was from the very begining responsability of the scientific-techincal área, module of oral medicine, unit of “diseases of dento bacterial origin”. Preventive dentistry, research and permanent learning constitute the solid bases upon the whole curriculum structure was build. (14) Figure 2.
The perturbing reality is that many faculty members, technically competent lack interest in the social aspects of dentistry. Prevention, in general terms, is irrelevant in the clinic and should be the subject matter of public health. Teaching of prevention is a theorethical course given by faculty members scattered in different departments like periodontology, paediatric dentistric, public health, restorative dentistry, others (Brown, 2007) 15
Past and present perspective
The impact of this enormous task force on the oral health of the colombian population has not been as should be as indicated by the results of the last study of the conditions of oral health in Colombia (ENSAB IV, 2015) (16)
In Colombia, like in many other countries 12 old-year children have a DMF(T) below 3 (Alma Atta and WHO reference value) (17,18,19) but 54.16% at the cavity level are affected by dental caries, if non-cavitated lesions are included 95.13% are affected, being the situation worst in the rural áreas (Figures 3,4).
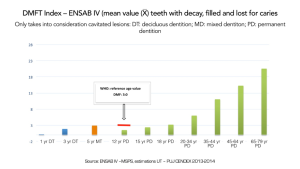
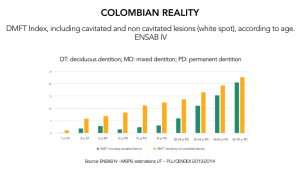
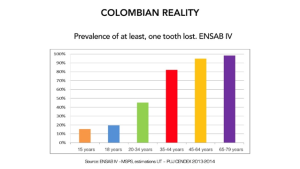
We as a profession feel proud with these figures, ignoring that almost 50% colombian children have the disease, certainly in medicine these figures are unacceptable for any cronic disease. In only six years, at age 18, 75.21% of the population experieices dental caries, reaching 96.26% (COP/T) and 97.01% when the non-cavitaed lesions are included at age 65 and 79. The periodontal condition also deterioretes with age, according to the criterias defined by the AAP and by the Center for the Control and Prevention of Diseases (CDC-Page and Eke, 2007) (20), 61.8% of the population is afeected by periodontitis of different degree of severity; severe periodontitis affects 25.99% at age 65 >; at this age only 9.85% are free of any form of periodontal disease (Figure 5).
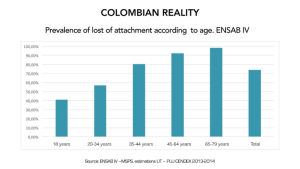
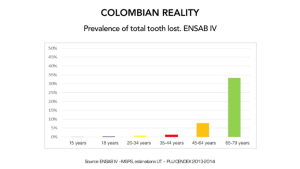
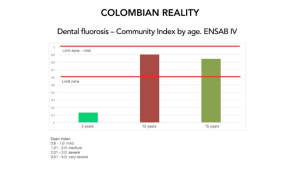
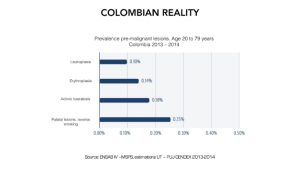
Loosing more than one teeth increses with age, at age 15, the value is 15.78%, reaching 98.90% at age 65 and 79 (Figure 6). Total, edentulism at age 65 and 79 is 32.87%, (Figure 7) compared with 15% USA), 22% (Canada), 54.7% (Brasil). Dental fluorosis is increasing, while in 1998 (ENSAB III) the prevalence was 11.3% (ages 5 and 6, 12 and 15), in 2014 (ENSAB IV), is 59.08% (ages 12 and 15) (Figure 8) regarding the soft tissues four pre-malignant lesions were identified (Figure 9). The nihil impact of a working dental force of close to 60.000 dentists in Colombia is illustrated in table 1.
Since the publication, in Leipzig (1530, circa) of one of the first books containing oral higiene recommendations, dentistry has been concerned and under the influence of different issues as indicated in the Flexner report (1910), for example the foundation of the IADR (1920); the Gies report (1926); water fluoridation in Grand Rapid, Michigan (1945); the foundation of NIDR (1948); the establishment of the departments of preventive and social dentistry in Latinamerica, being the first, the one at Universidad de Antioquia (1960, circa). And of course the transition and incorporation of independent, private dental colleges and schools into the university system (1920, circa).
Historically changes in dental education took place after those in medical education, for example the Gies report (1926) (21) was preceded by the Flexner report of 1910 (22), even today dentistry rejoice planning for the future forgetting the present. Since 1960 (circa) dental education is planning for the future, is true that technology and societal changes are pushing in that direction, but our attitudes keep us clutched to the past.
The main problem, when trying to introduce drastic changes in dental education, to solve questions like what is the best approach to solve the health problems of the society?, is not lack of agreetment upon subject matter, it is the negative attitude of faculty, afraid of lossing power or image (personal ego)
Over the years, those of us involved and concerned with dental education identified the same problems: lack of correlation between basic and clínical sciences, many times dental curriculum is not the reflection of the prevalence of the main diseases affecting the population, students are overwhelmed with numbers, statistics many times with obsolte information. We “educate” our students to be passive receptors of information unable to solve problems by critical thinking. Clinical instruction is centered in the student with minmal requirements to be completed each academic year, instead of centered in the needs of the patient; number of crowns, fillings of dubious quality, endodontic treatments are more important than the holistic approach to solve the problems of the patient and/or those of the community as perceived by them. Technologically dentistry has advanced properly but insensible to the needs and expectations of students, faculty and society.
Forever, curriculum changes are characterized by relocation of courses, modification of cloack hours, many times as a reflection of the Dean´s personal interest or as a result of a new technological toy (tool); few times as a result of the unsolved learning problems of the student or the expectations of the society. Many dental schools are facing budgetary constraints, diminshing numbers of new students, and those interested are not the more qualified. Finnally the government and the insurance companies are the ones dictating how clínical practice should be implemmeted with one objective in mind, increased productivity of dubious quality, numbers of procedures (amalgams, composites, extractions), is what counts, not the needs of the society.
Forseen the future
In order to justify dentistry as a health profession it is necessary to reach consensus, among academitians, in basic issues which guarantee that the dental profesión will contribute to solve the oral health problems of the individual, the familiy and the society they swored to serve. In order to reach that purpose it is not enough to reorganize course content, relocating them or increasing hours. Without any doubt, dentistry is facing, internal and external pressures that reflects the current curriculum design, being education, one of the main considerations in the “mision” of many dental schools, unfortunatelly ignoring the epidemiological profile of the most prevalent oral diseases in the country, and to complete the picture the dental industry is dictating the direction research should takes. (23)
Change has to be the result of a profound critical analysis of the dental profession taking into consideration pressures originated internally, and externally from the society.
Internal factors
- Rigid concepts and inappropiate understanding of the meaning of curriculum flexibility
- The teaching career in many latinamerican dental schools is short due to poor salaries, as a result must of the faculty members are part time or less, many of them from prívate practice. Brazil is one of the exceptions.
- The way dentists are trained, critical thinking is lacking (24)
- Great part of the clinical training is intramural (protected ghetos) that isolate students from the reality of the country where they are going to practice.
- The new technology: multimideia, internet and its tremendous impact in the learning process.
- Lack of integration with medicine, oral health is not part of general health
- The colombian reality is ignored by the health professions, in dentistry restorative treatment is more important than prevention and health promotion.
- Fear to change
Additionally, special mention deserves the exponential growth in all fields of science which might create internal problems in dental schools curriculum design and course contents:
- Pharmacological manegament of behavior in small children; (physical restraint is forbiden in many countries; children are not supose to suffer)
- New diagnostict tools: DNA probes, microbilogical and immunological tests, DIAGNOdent, many others
- CAD-CAM
- New dental materials (bio-compatibility)
- Replacement therapy in dental caries and periodontal disease
- Slow release devices (Fluoride, chlorexidine, antibiotics)
- Saliva, instead of blood samples for many laboratory tests
- Manipulation of inductive substances to produce enamel and dentine
- Genetics and engineering in cranio-facial anomalies
- Guide tissue regeneration in peridontal disease
- All kind of antimicrobial rinses
- Ethical aspects related to handling of VIH patients
External factors
- The impact of the health system in Colombia (Ley 100): less dentists in prívate practice, more dentists working for third party payment
- The impact of the new regulations regarding higher education in Colombia (Ley 30)
- Demographic changes in the population, the number of 60 year-old is increasing.
- The impact of the peace agreements (FARC) on the social, political and economical structure of the country.
- Increased number of high risk groups: uneducated, without work, victims of violence, migration from the rural to the urban areas.
- Top students from secondary schools are not as interested as in the past in dentistry. Quality of the new clases is diminishing
- Needs and expectations of the population are not met
- Changes in the prevalence of dental diseases like dental caries, periodontal disease, bucal cancer, dental fluorosis, dental erosion
- Exponential growth in all fields of knowledge including technological advances for example in informatics (medicine from internet)
- Harmful influence of the dental industry selling all kinds products with dubious benefits
- Dental fees are determined by the health insurances companies not by the profession.
- Complete divorce between what is tought at the dental schools and the way is implemented by the health officials (Ministry of Health).
- Quacks offering dental services (from extractions to full dentures) to the underprivileged mainly in small towns and in rural communities, in those locations the presence of oral health authorities is forbiden by force.
Dental educators keep adressing the same questions, over and over:
- Training in clinical dentistry must be centered in the needs of the dental students (number of clinical requirements), and not in solving the problemas of the patient as perceived by them? Today,the opposite must be the case, as it is proposed during this symposium
- At the university level, what is the role of the dental school in defining finantial priorities?
- How is the Mision of the dental school evaluated from the point of view of society expectations?
- What is the profile of the dentist, required to solve the oral health problems of the society in the 21st century?
- How many clinical specialities do we need? In today´s society what is the role of the general dentist?
- Ideally, dental schools should be training general dentists aware that technology by itself is not the solution to biological problems (placement of restorations is not treatment for dental caries, is a way to replace dental structures lost as a consequence of a process that we called dental caries)
- How far away are we from a dentist socially compromised, medically oriented, able to solve the problems of the patient, its family and the community?
To what extent can we use the above information to solve the oral health problems of the population and not the ones of patients in prívate practice?
For many reasons some of us in this symposium will like to suggest a “scholarized” curriculum characterized by educating students able to think critically, permanent learners as a way to create an academic environement in which the free exchange of ideas is a possibility.
Some characteristics of this type of curriculum are:
- Integration of research, social service and teaching, taking into consideration the colombian national health plan. Many factors and pressure groups are the driving forces that explained the need to integrate dentistry with different areas in the health system with emphasys in prevention and control of oral diseases, primary care, health promotion, simplified technology cost effective health plans, use of ancillery personnel, “posible” treatments, accesible to the vast majority of the population, instead of the “ideal” plan of treatment, extremely costly, affordable by just a few. Additionally: technological advances in molecular biology, identification of human genome, increased longevity of the population including countries with emerging economies, unsatisfied demands from the underprivileged communities, universities with limited budget, role of government in controlling the health care system, policies from the health insurace companies controlling dental fees, role of the dental industry controlling research and prices of dental products.
- Clinical training in the dental schools must be centered in the needs of the patient, not in the fullfinment of student´s minimum requirements. Students must have early contact with the communities where they are going to practice after graduation from the dental school. In each country is important to define how many and which specialities are needed to solve the community oral health problems of the community.
- Dentistry needs to work hand by hand with society as a whole, including the government, not as an isolated entity The practice of dentistry is evolving from solo practice to salaries paid by the state and/or the insurance companies, such tendency needs to be reflected in the curriculum. Fees are determined by them, not by the profesión, like in the past.
- In dentistry as well as in medicine exists concern regarding the adecuate number of dentists and physicians required by society, seems to me that the role of the university is just to graduate students, unconcerned with their profesional future.
- The most difficult question to answer today is what type of dentist do we need to solve the oral health problems of that pocket of the society living in extreme poverty, unprotected by the health system of the country. Is important to take into consideration that 25% of people, mostly children, accumulatae 80% of the dental problems, i.e, dental caries. Under those circumstances, society, what does requiere?, well trained general practitioners and/or ancillery personnel or specialists in fields like endodontics, radiology, implantas, cosmetic dentistry or even pediatric dentistry?
With the above in mind it might be posible to define the professional profile in terms of (a) its commitment with himself, with the patient as an individual, with the society as a whole, with the scientific community (nationally and internationally), with the dental profession and his/hers alma mater; (b) its profesional attitudes which includes a preventive phylosophy (style) of profesional life, concerned for the healthy individual, inquisitive mind (research orientation), ecologically oriented, profesional attitudes and habits (etics), creativity and lidearship, socially compromised; (c) its level of competency in diagnosis of problems related to oral health, in the manegament oral health projects in science, technology and administration , knowledgable in new technology and in informatics.
The next issue is to define the general characteristics of a curriculum that takes into consideration these factors. First of all has to be dynamic and flexible allowing each student to advance at its own rithm without pre-requisites for the next course; has to be integrated with medicine and with other disciplines in the health science; has to have continuity and integration amongst the different course components, and mínimum number of lectures with ample time for self and group learning. (25)
Upon graduation from the dental school, the graduate must be competent to:
- Diagnose oral health problems of the individual, its family and its community
- Define adequate plan of treatment for each situation according the best available information
- Avoid as much as posible, surgical (mechanical) solutions to biological problems
- Prevent desease before intervention according to the principle, “see, obseve, wait and intervene”
- Use technological develpoments to research health problems in a critical way
- Use simplified technology and equipment in the treatment of patients
- Promote health at the individual and the community level
- To practice dentistry with honesty (moral integrity) and respect for the patient
- To offer each patient different options of treatment, explaining advantages, disadvantages and alternative treatments
- Delegate in well trained ancillary personnel clinical procedures of minor complexity
- Behave as a teacher with each patient and its family
- Be a permanent learner and researcher
- Have a human and humanistic approach in his/hers profesional life
The teacher as passive transmitter of information will give ground to a true maese, able to facilitate learning. A flexible curriculum with this kind of teacher will allow each student to advance and its own rhythm which means that some students might require four years to be competent as a general clinician and others might require less and other more years. (Figure 2)
Conceptual characteristics of this model
- The community as a target. Future dentists must be expert in health, not necesssarily in disease. Health promotion and comprehensive prevention and disease control has to be the primordial philosophy of clinical service to the patient, its family and its community and not the domain of one specific course. (26)
- The curriculum. Has to be the reflection of the more prevalent diseases in the community, with emphasis in health promotion, comprehensive prevention, integration of basic sciences with clinical sciences. Oral health must be contextualized as part of general health. Academically concepts should be discussed going from simplicity to complexity and learning by doing. (27)
- Holistic approach to control and prevention of diseases of the mouth. Prevention must be the protective umbrela in clinical dentistry, should not be an isolated issue belonging to one clinical department, needs to be a phylosophy of profesional life. (12)
- The Colombian reality. This is an important issue to take into consideration, like elsewere in the world colombians are living longer (men 73 years and women 79 years) not necessarily with more teeth, the number of medically compromised patients, immunosuppressed, oral cancer, emotional problems, diabetes or with HIV is increasing, like wise the pattern of the most prevalent clinical problems in the mouth, dental caries and periodontal diseases is changing, the disease process is slow as compared with the past, it allows to less surgical intervention and more therapies oriented to innactivation of the disease process. These circumstances must have an impact on curriculum design and course contents.
- Clinical dentistry. The teaching of clinical protocols, as much as posible, should be implemented in community settings, emergency rooms, hospitals, dental and medical homes and not limited to the intramural clinics in the dental schools.
- Moving from oral health to general health. To achieve this goal dentists must learn how to work with other members of the health team, physicians, nurses, ancillery personnel, administrators of health services of different levels (state, private, mixed), guvernamental dental officers, the profesional associations, others.
- The whole or the totality. The true doctor in dental medicine (stomatologist) must be competent in clinical dentistry, but equally important with impecable profesional habits and attitudes, high moral and ethical values, human and humanistic.
What might be innovative in the teaching of dentistry?
In order to answer, properly, this question we need to take into consideration our main argument to justify this symposium, that is: “current dental education has been unable to solve the oral health problemas of today´s society”
Some general considerations to circumvent this situation might be: (a) integration with medicine in order to train physicians of the mouth; (b) teaching of clinical sciences in context with clinical activities, not as a pre-requisite to iniate clinical work; (d) promoting self study instead of having students as passive receptors of information in lecture halls (e) curriulum oriented to the solution of problems and to the development of abilities and competences, (f) as much as possible extramural activties in the community instead of intramural practice; (g) reduce the number of clincial specialities.
- Curriculum must take into consideration the most prevalent diseaes in the country (region by region), and how is the problem perceived by that particular society?, cultural background, believes, educational level, socio-economical status of the family, are also important issues in this respect
- Curriculum flexibility must allow each student to learn at its own rhythm in order to the develop the adecuate competencies required for clinical practice, for which many of the pre-clinical and clinical courses are of not importance.
- So flexible that students, that according to ther Promotion Committee of the dental school are ready for graduation at the end of the fourth year could start speciality program of their preference during the fifth year or begin the MS or PhD program for those more inclined to be part the academic life (teaching and research).
- On the other hand, curriculum flexibility must allow extra time to those students in need of it to develop the requiered level of competence in clinical practice.
- Even today and as a reflection of the Flexner and Gies report, many dental schools in Latinamerica have curriculum with 80% of the clockhours devoted to preclinical and basic sciences concentrated during the first two years, 17% for clinical activties, mostly after the fifith semester and only 3% for humanistic sciences (including behavioral sciences, social and community work) This model represents the transit from the proprietary, technically oriented, prívate dental colleges (1900 circa), to the dental schools as part of the university system (1950-present, circa). Students keep seeing basic sciences as something mandatory to start clinical activities without any practical value. In their minds is more important the how, than the why or the when.
- Around 1960, dental schools moved from the vertical and horizontal models described in the previous paragraph to the diagonal model with basic sciences concentrated during the first years, progressively declinining at the end of the fifth year, clinical activities were minimal during the first years increasing in intensity toward the end of the fifth year.
- Clinical activties were organized by departments with minimal requirements to be completed by the student, comprehensive clinics were located during the fifth year. The concept of the integrated treatment of the patient came years later. It has been extremely difficult to move away from clinical training devoted to solve the learning problems of the students to one oriented to solve the oral health problems of the patient and/or the community.
- Integration of oral health into general health by means of the common risk factor approach (28,29)
Does the answer lies in curricula oriented, to the solution of clinical problems and/or the development of competencies?
If the important issue is the develpment of clinical competencies, dental education should be oriented to teach the students in what areas they should be (a) competent, (b) informed or have (c) knowledge in some specific topics not requiered for daly clinical activities. It is not a curriculum based upon instructional objectives, it is oriented to motívate the student to independent learning, continuing education and critical thinking. Upon graduation, the new dentist is an apprentice with enough tools to continue to learn from each new clinical problem. (30,31,32,33)
Today, the dental curricula, in the vast majority of dental schools is encyclopedic with course contents organized in countless disciplines. Is a model that can be described in terms of what theachers, teach; students, learn; researchers, research and different kind of committes, discussing and legíslating. It is centered in the teacher, without visión of the future, academically innocuous, only describing the “to be”, instead of the “should be”.
If the goal is to be competent in something the student needs to learn the minimal ability for each clinical task, in order to do so, basic sciences are requied to support clinical activities combined with adecuate profesional habits and attitudes. Itis posible to be competent in something to proper training and accumulated experiences after repeating similar procedures over and over. In order to do so, the general structure of the curriculum must goes from generalities to specificities identifying the most common clinical activties as they ocurre in the daily life of a general practitioner. In this model, classical departments are only the reflection of the administrative structure of the dental school. Teaching could be organized in different categories or “domains”, as they are called, taking into consideration the needs of the population, for example:
- Profesionalism
- Evaluation of the patient and its environment
- Maintenance of good oral health, once is institued
- Health promotion
- Practice adminsttration
- In each domain is necessary to identify “major competencies” required to solve complex clinical problems. The complexity of the task requieres the support of specific abilities to solve the health problems of the patient and its community. The didactic instruction might include lectures, seminars, independent study, group discussions, community activitiers and laboratorios.
As an example: Domain 1: Professionalism
Major competency:
- Ethics
Support activity:
- Honest and confidential relationship with patients
- Recognition of cultural differences and its impact on the oral health care system
Didactic activities:
- Anthropology
- Behavioural sciences
In some way, this approach answers the educational needs of the students, measurable in terms on the ability of the students to solve the oral health problems of the patiernt and its community.
In order to be “competent” to solve the helath problems of the patient and its community, the student has to be able to “solve problems” of any kind. A problema can be define in many ways:
- Every thing that is ignored by the student and is needed to become a dentist
- A question that needs to be clarify
- Group of circumstances that interfere with the achievment of a goal
- Proposal address to obtain a goal through known facts
- Neutral description of certain phenomenons and events among which is posible to find common characteristics
Whenever the student is facing a problem of any kind (for example, a clinical situation), he or she should be able to identify the problem, to explain the circumstances that created the problem, to be able to propose a suitable solution and to develop the abilities and dexterities requiered to do it.
To be competent to perform X task, the dental student must:
- Acquire the basic principles and knowledge required to practice dentistry without supervisión
- With that knowledge the student must be able to evaluate the oral helth situation of the individual, its family and society as a whole.
- Be able to learn how to learn to solve clinical situations of different categories, accumulating experiences from the past.
Is important to understand that the student in his or her daily life is facing problems of different kind: (a) learning problems, which dental education still believes that the best way to solve the situation is by lectures wth the student as a pasive receptor of information, without motivation to be an active member during the educational process. Today´s technological advances available to the students since early infancy demands a complete change in the way to teach clinical dentistry. Few lectures as posible, more community work as a fundamental basis during the learning procees (learning in the field).
(b) knowledge problems, the meaning of this is the erroneous idea of having the so called basic sciences as indenpendent courses during the first semesters of the dental curriculum and not integrated with the teaching of the technological aspects of dentistry, meaning manual skills.
(c) evaluation problems, every single student is evaluated the same way, either by means of multiple questions tests, or by the number of clinical procedures (minimum requirements), in this system no consideration is given to the fact that each student learns in a different way. Students should be evaluated, individually on a daily basis, at CES the promotion committee (PC) plays a very important role in this sense.
(d) manual skill problems; as in the theoretical courses in the lab excercises are evaluated the same way, without consideration of the fact that development of manual skills require more time in some students than in others. Students should be allowed to work independently in order to be competent at the level required by the program. Hand books describing each technique is a must to help the students.
(e) patient´s problems: traditionally patients are considered indinspensable, without them, students won´t be able to complete mínimum requiremtes for graduation. Today the situation is evolving to one devoted to solve the oral health problems of the patient as perceived by them. Clinics in the dental schools are moving away from those centered in the students with specilists as faculty members to those centered in the needs of the patient with general practitiones as clínic instructors.
Daily, dental students are solving problems of different nature, because of that they need to be competents an in need of guidness provided by faculty members not with the answer for each clinical problem but with the appropiate tools to help the student find the correct solution. In time, students will discover that the learning process is more gratifying as a result of deductive reasoning and accumulation of experiences than from memorizing facts of diverse nature. Is a complex situation because in the health sciences clinical problems can have different correct solutions (the so called open problems) while in areas like mathematics problems are “closed” with only one correct answer. Under these circumstances is valid to ask how does the “novice” student learns as compare with the “expert”, the teacher?
The “expert” accumulate experiences from the past, to solve a situation, comparison with similar experiences are used and helps to choose the best alternative. The “novice” starts from zero, lacks experiences, needs or use some basic principles learned in the class room. The students (“novices”), from the very begining need to be introduced to critical thinking, and deductive reasoning, impossible to obtain it from a formal lecture in the class room.
The “heuiristic” approach to learning, is designed to stimulate students to re-search, find, think and analyze through two different approaches to solve a problem: in one; analysis precedes creativity; in the other creativity, precedes analysis. This approach needs to take into consideration that in the health sciences the majority of the situations, are open problems with different correct answers (see above) Open problems requires from the student criticasl thinking, logic reasoning to make subjective decissions (scaring situation for the student), who preferes objectivity. At the end of this process, the student must be confident that his/her decisión is the correct one for the case in hand.
Some of the concepts expresed in previous paragraphs can be sumarized in the following table which compares the traditional approach to dental education with one closes to the “ideal, innovative” solution:
| IDEAL (CES?) | TRADITIONAL |
| Centered in patient needs | Centered in the student/teacher |
| Disease control (prevention) | Restorative treatment |
| Inactivation of the process | Damage repair |
| Accesible treatment (posible) | Ideal treatment, costly, exclusive |
| Generalist | Specialist |
| Patient satisfaction | Requirements |
| Concerned with health | Concerned with disease |
| Community work | Indoors practice |
| Competencies (problem solving) | Encyclopaedic (isolated information) |
| Integration | Isolated courses |
| Basic sciences in context with clinical problems | Basic sciences: clinic pre-requisite |
| Flexibility /individualised | Rigidity, standardised |
| Quality work | Quantity (minumum requirements) |
| Based in the community | Based in clinics and hospitals |
| Research (tutorial) | Lectures |
| Humanist/humanitarian | Technicist |
| Educator | Penalyzer |
| The human being as a whole | Molecule, cells, organs |
| Mouth as part of the body | The mouth |
| Oral health as part of general health | Oral health as part of the |
FROM NOW ON, WHERE SHALL WE GO?
Is easy to agree in what needs to be change, the main obstacle are faculty members afraid of loosing power or status. More than fifty years ago dental educators agreed on aspects that requiered inmmediate attention: lack of correlation between basic and clinical sciences; excesive information given to the students in the class room, many times obsolete and without practical use; students were trained to be pasive receptors of information, unable to think critically; clinical instruction only took into consideration the amount of amalgams, crowns or extractions required for graduation, the patient was a guinea pig to that end; comprehensive clinics from the very begining, even today are scarce and many times present during the last year of clinical training; undergraduate students are unable to manage properly medically compromised patients or pharmacological handling of behavior; community work is scarce; prevention and control of deasese represents in the best of the cases less than 10% of the total of curriculum hours; lack of flexibility, every single student is measure equally ignoring that students learn at different rates; technological advances are far more important than community sensibility. (34,35,36)
In order to introduce those changes dental educators proposed curriculum by objectives; problem based learning and development of competencies, lately independent learning but without consensus among dental educators; as a consequence we keep moving back and forward from one model to the next. (37,38,39) Training the proper personnel is not the only problem that dentistry is facing today, questions like how to obtain better care, mantain people and communities healthy in an affordable, cost-effective way needs to be answer in light of the fact that the prevalence of oral diseases, mainly dental caries and periodontal desease are decreasing in the population because of the success of appropiate preventive programs of different order including fluoride therapy, systemic and /or topical, promotion and education of the individual about good oral higiene practices. The question here is, who is succeeding? The dental profesión per se, or the dental industry with its aggresive campaigns?
As indicated in this document in Colombia the dental work force, per capita is ingreasing (over 45.000 dentists for a population of 45 million people), to dangerous levels. The treatment provided by these dentists focuses on restoring the damage caused by past dental caries experience and/or periodontal disease. But if both diseases are decreasing, what will dentists being doing in 20 years?, considering the possibility of reduced demand, an increased number of dentists, and the fact that in some countries a great amount of preventive and maintenance care is provided by non-dentists; under these circumstances how will the profession be organized?, there is a movement to integrate dentistry and general health, promoting greater dentist-physician interaction in patient care as use to be in some european countries last century.If this integration takes place will be dentists be considerad as colleagues by physicians? In the mind of some dental educators the concept of “physicians of the mouth” (stomathologists) is growing, to reach that end point is mandatory for expanded baseline knowledge in medical sciences during pre-doctoral training in stomathology. The future of dentistry resides in the capacity to answer the question: what can be done to properly serves the oral health needs of the population. Dentistry to survive needs proper adaptation to a changing environment. Not an easy task.
Colombian universities: re-inventing them-self or disappearing
Presidentes (rectors) of some of the leading colombian universities like Andes and Rosario, in Bogotá, coincide saying that without modernization and innovation in teaching methodology the near future is uncertain. Today, some academic programs are unable to trained people able to solve many of the problems of modern society, in general, they are not talking about dentistry. For generations students receive the same type of education in the class room, same topics by the same professor who many times is not able to respond correctly to sound arguments from part of the students. The encycolopedic way of teaching of the past 100 years has to give space to the new technological information.
Virtuality is a reality and the class room has to be re-invented, interacting with adecuate space inside the physical university structure. On the other hand, is pertinent to ask how to trained leaders by internet?, it is posible?, is also valid to ask how to learn and how to work in groups?
Another interesting debate is to define if higher education should be oriented to give the students proper tools (advance technology), instead of adequate course content. Modern education must guarantee that the students not only have access to appropiate tools, but also profesional attitudes and habits to solve the complex problems of a changing world. Active learning is replacing the enlightened teacher. Different topics can be approach by developmnt of competencies in sciences, mathermatics, technology (robotics) which will allow students to move from pure entertainment to learning. In order to change society students of the future must be experts in bio-tehnology, nano-technology and digital solutions.
In Colombia, is a must in education, bilingualism, good knowledge in mathematics, science, technology, bio-engineering, creativity, communication, leadership and group work. Those claiming for change are aware that the idea of incorporating new thechnoly means that every thing from the past has to be avoided. Is true that we need to be disruptive but at the same time conscious that each society has different challenges. We are observing changes in the industry, in the government, in society as a whole, then the way of teching has to change as well. And at the end, are the students who will promote and demand changes. Change is around the corner, and won´t be easy, the new generation of students will demand it.
How is this way of thinking going to be influenced by the new definition of health recently proposed by the FDI (2016)?
“Oral health is multi-faceted and includes the ability to speak, smile, smell, taste, touch, chew, swallow an convey a range of emotions through facial expressions with confidence and without discomfort and disease of the craniofacial complex. Further attributes include that it is a fundamental component of health and physical and mental wellbeing. It exists along a contiuum influenced by values and attitudes of individuals and communities; [it] reflects the physiologic, social, and psycological attibutes that are essential to quality of life; [it] is influenced by the individual´s changing experiences, perceptions, expectations and ability to adapt to circumstances”. (40)
Additional considerations
In this presentation the emphasis resides in posible ways as to how to achieve, the what and the why, objectivelly to be described by other speakers during the following presentations.
Like medicine years ago, dentistry today is at a cross-road (41), accepting, not by every body, that the current educational model is strictly oriented to train excellent clinicians for private practice, tecnically competent to design smiles, place implants, use orthopedic appliances in the mouth since infancy; higly expensive modalities of treatment, consequently affordable by only a few (¿5% in Colombia?) forgetting that the oral health needs of the population are not met.
In most dental schools students are passive receptors of information, unable to understand the concept, only memory matters to pass the test and proceed with the following topic. Critical thinking, independent and deductive learning are a rarity if ever exists; the teacher gives the answer instead of possing questions to be solve by the student; in daily life, outside the class room the student is face with the need to solve problems of all kinds, as simple as to decide what to order in the cafetería or as complex of the ones in the clinic or in the lab.
Education in the health sciences, medicine, dentistry, nursing, paramedics is under the influence of external demands that need to be to take into consideration by educators. Patient are demanding better treatment at affordable fees, private practice is vanishing, the new graduates are force to work in a group practice or for a salary paid by the government or by one of the many insurance systems available in each country.
Research and the new technological developments have a tremendous impact in all areas of clinical and teaching activities. All of us, here, in this beautiful auditórium agree that a drastic changes are badly needed in dental education, however outside during the coffee brake the reaction is quite different and the status quo goes on and on, why?
Dental caries and periodontal diseases are cronic, intermitent, accumulative in nature with age and as a result of both processes many individuals end up loosing teeth. A different consideration might be to consider loosing teeth as part of the aging process, the same way that humans loose hair, hearing and sightseeing deteriorates, arteries get harder, memory fades away. (42) At any rate, in Colombia, the efforts to obtain at age 12, a DMF(T) < 3 and almost 50%, free of dental caries, are lost with the passing of years as indicated by an increment in the prevalence of dental caries, 52.81% at age 20 to 34; 64.73% at age 35 to 44; at age 65 to 79 decreases to 43.47 as a result of the amount of lost teeth at this age. An interesting consideration is that those individuals that today are in the age group of 40 to 55 year old represents the cohort that has been analyzed in four studies realized in Colombia since 1995. Unfortunatelly for this age group not adequate measures were implemented to control risk factors and progression of the disease process, as a consequence, frecuency and severity of the disease remained unchange at age 35 to 44 and 65 > Instead of more healthy teeth present in this individuals, the contrary is the real situation. Who should be blamed? Dental education, policy makers at the local and central government, ¿or both?
Conclusions
In my opinión to expect that dental schools in the near future, move away from training dentists to practice, either for a salary within the health system or in private clinical settings is an imposible dream. Faculty members are afraid to change, and clinical practice is more profitable to design smiles, place implants, than to work in the communities solving accumulated needs. The dental industry will assit to perpetuate private practice by offering new products of dubtious quality to the public and to private practioners anxious to grasp what appears in the market. Political and economical interests precludes any possibility of closing dental schools, on the contrary, the corruption that is destroying our society will facilitate the opening of new ones.
Under this circumstances, what can we do, in the short term? Start by changing teaching methodology, for example reducing as much as posible the class room lectures, promoting self and group learning via new technology; implementation of curriculum flexibility to the point that each student can progress in the development of required competences according to its capacities; basic sciences must be integrated to the clinical teaching; instead of so many hours devoted to the repetition of the same subject matter, more time must be allowed to behavioral sciences, health promotion; clinical practice must be learned in community settings, not only in the dental school clinics.
In order to close the gap, between what we teach at the dental schools and the oral health care policies implemented by the public sector, it is desirable to create working committees integrated by faculty members, public health servants (Minsitry of Health), members of the insurance companies, and researchers from the dental industry. The main responsability of this committee must be to formulate policies oriented to really serve the needs of the underprivileged segment of the population. ACFO (colombian association of dental schools) can play a very important role in this enterprice.
At the level of the university, the schools of medicine, dentistry, nursing, nutrition, physioterasphy and allied health sciences, must work together to integrate oral health as part of general health. Concept that can be implemeted by means of a “health family demostration program” in which a family or group of families, ideally in a rural community, are assigned to a group of students (one from each participating school) who will assume the responsability to keep healthy the family group after restoring health in those affected by disease. The common risk factor approach must be the conductoig line to successfully achieve this purpose.
A final dream, universties with schools of health sciences, offering a two- three year core curriculum to future physicians, dentists, nurses, orthodontists, cardiologist, urologist etcétera. The concept behind is that in the future it is not necessaery to go five, six years to medicne or dentistry if the expectations are, to be, for example a cardiologist, a family doctor ora n oral surgeon. Only working together Ministry of Health, Ministry of Education the profesional associations and the Universioty is might be posible to achieve this dream.
References
-
Binns WH, Escobar A Deffects in permanent teeth following pulp exposure of primary teeth. J of Dent for Children Vol XXXIV, pp 4-14.
-
Restrepo D. (1963) La enseñanza de la odontología preventiva y social en facultades de odontología de América Latina. Boletín de la Oficina sanitaria Panamericana (OPS) 55(3): 312-321.
-
Mejia VR, Velez AH, Espinal TF, Hernandez AN. Fluoruración de la sal en cuatro comunidades colombianas. Boletín Oficina Sanitaria Panamericana 77(4): 295-299, 1974
-
Panamerican Health Organiztion. Salt fluoridation studies in four Colombian communities. Resolution 2/15 Washington DC, 1963.
-
Sarnat H, Masler M (1965). Microstructure of active and arrested dentinal caries. J of dent res 44(6): 1389-1401
-
Massler M. Control of caries: A new concept. The New Zealand Dent j. (58): 69-73, 1962
-
Bjorndal L, Thysltrup A. A practice based study of step-wise excavation of deep carious lesions in permanent teeth: a 1-year follow-up study. Community Dental Oral Epidemiology 1998; 26:122-8
-
Bjorndal L, Larsen T, Thysltrup A. A clinical and microbiological study of deep caries lesions during stepwise excavation usuing long treatment intervals. Caries Res 1997; 31:411-17
-
Blackerby PE. Department of social dentistry. A review in Social dentistry; seminar proceedings. Washington DC; government printing office, 1965
-
Ayers C, Williams D, Lausten L. A survey of prevention in dental education. Journal of Dental Education, Vol 4(9): 515-576, 1979.
-
Spolsky VW, Brown JP, Hudepohl N, Garcia R, Heushew M, Clarck C, Olney C. The teaching of caries prevention in US and Canadian dental schools No. 82 at www.dentalcare Accessed Sep 5, 2006
-
Kerosuro E, Ruotoistenmaki J, Murtomas H. Report on the development of a new dental curriculum at Helsinki. European Journal of Dental Education, 2001; 5: 23-30
-
European Academy of Paediatric Dentistry (EAPD). Curriculum guidelines for education and training in paediatric dentistry. Inter Journal Paed Dent, 1997; 7: 273-281
-
Escobar A, Vélez LF. Teaching of cariology at the College of Dentistry, University CES, Medellín, Colombia. CES Odontología, 2014, 27 (2): 105-120.:
-
Brown JP (2007) A new curriculum framework for clinical prevention and population health, with a review of clinical caries prevention teaching in US and Canadian dental schools. J of Dental ed 71(5): 572-578
-
ENSAB IV. IV Estudio Nacional de Salud Bucal. MINSALUD, Bogotá, 2015
-
World Health Organization (1978) La Declaration d´Alma-Ata WHO 2-2
-
World Health Organization & UNICEF (1978) Primary Health Care: Report of the International Conference on Primary Health Carer, Alma-Atta, USSR, 6-12
-
Labonté R, Sanders D, Packer C, Schaay (2017): Is the Alma Ata visión of comprehensive primary health care viable? Findings from an international Project. Global Health Action 7:1, 24997
-
Page R, Eke P (2007) Definitions for use in population-based surveillance of periodontitis. Journal of Periodontology, 78: 1387-1399.
-
Gies WJ, Pritchett HS (1926) Dental education in the United States and Canada: A report to the Carnagie Foundation for the advancement of teaching. Carnegie Foundation for the Advancement of Teaching, no. 19.
-
Flexner A. The Flexner report on medical education in the United States and canada. (1910), New York, NY, Carnegie Foundation, col. 58.
-
Bertolami CN (2001) Rationalizing the dental curriculum in light of current disease prevalence and patient demand for treatment; form vs content. Journal of Dental Education 65(8): 725-735.
-
Hendrickson WD, Audriew SC, Chadwick K et al. (2006) Educational strategies associated with development of problema-solving, critical thinking and self directed learning. Journal of Dental Education. 70(9): 925-936.
-
Kerosuto E, Ruotoistenmäki J, Murtomaa H. (2001) Report on the development of a new dental curriculum at Helsinki. Eur Journal Dent Edu, 5:25-30
-
Petterson EO. (1973) The development of community dentistry in dental educational curricula; activities and resources of departments. Journal of Public Health Dentistry 33 (4): 238-244
-
Baelum V, Van Palestein Helderman W, Hugoson R, Yee R. A global perspective on changes in the burden of caries and periodontitis: implications in dentistry. Journal of oral rehabilitation 2007 34:872-906
-
Sheiham A, Watt RG. The common risk factor approach: a rational basis for promoting oral health. Community Dental Oral Epidemiol 2000, 28: 399-406
-
Watt RG, Sheiham A. Integrating the common risk factor approach into social determinants framework. Community Dent Oral Epidemiol 2012; 40: 289-296
-
Rohlin M, Peterson K, Svensater G (1988). The Malmö model, a problema based learning curriculum in undergraduate dental education. European Journal of Dental Education. 2(3): 103-114.
-
Bassir SH, Sader-eshkerazi P. (2014). Problem based learning in dental education: a systematic review of the literature. J of Dental Education. 78(1): 98-109.
-
Carracio C, Wolfsthal SD, Englander R, et al. Shifting paradigms: from Flexner to competencies. American Medicine. 77(5): 361-367
-
McCann AL, Babler WJ, Cohen PA (1998). Lessons learned from the competence-based curriculum initiative at Baylor College of Dentyistry. Journal of Dental Education. 62(2): 197-207.
-
Jenny J, Frazier PJ. Departments of community dentistry as viewed by teachers of clinical practice, basic science, and community dentistry (1974) Journal of Public Health Dentistry 34(3): 161-173.
-
Allan J, Barwick TA, Cashman S, Cawley JF, et al. Clinical prevention and population health. Curriculum frame work for health professions. (2004) American Journal Preventive Medicine. 27(5): 471-476.
-
Lange BM, Dunning DG, Graham S. The changin role of prevention in dental education. (1990) Journal of Dental Education 54(9): 567-569.
-
Manogue M, Mc Loughlin J, Christersson C, Delap E, Lindh C, Schoonheim-Klein M, Plasschaert A. Curriculum structure, content, learning and assessment in European undergraduate dental educatio – up date 2010. European Jouranl Dental Education (2011): 133-141
-
Piskorowsky WA, SJ, Stefenac. Influence of community-based dental education on dental student´s preparation and intent to treat underserved populations. (2012) Journal of Dental Education 76(5): 534-539.
-
Brown JP. A new curriculum framework for clinical prevention and population health, with review of clinical caries prevention teaching in U.S. and Canadian dental schools, (2007) Journal dental education 71(5): 572-578.
-
Editorial. A new definition for oral health developed by the FDI World Dental Federation opens the door to a universal definition of oral health. International Dental Journal 2016; 66:322-324
-
Field MJ, Jeffcoat MR (1995) Dental education at the crossroads: a report by the Institute of Medicine. The Journal of the American Dental Association. 12(2): 191-195.
-
Fejerkov O, Escobar G, Jossing M, Vaelum V. A functional natural dentition for all – and for life? The oral health care system needs revisión. (2013) Journal of Oral rehabilitation. 40(9): 707-722.
