6
Firoze Manji

Science alone has the power to silence heretics. Today it is the only institution that can claim authority. Like the Church in the past, it has the power to destroy, or marginalize, independent thinkers. … For us, science is a refuge from uncertainties, promising – and in some measure delivering – the miracle of freedom from thought. John Gray, Straw Dogs, cit. Žižek, 2008: 69 (my emphasis)
Where experimental investigation is prohibitively expensive or impossible to do, mistaken assumptions, misconceived paradigms and pathological science can survive indefinitely. Gary Taubes ‘The Case Against Sugar’ 2016
How did it all begin?
Dentistry was never my first love. I had opted at school (in the UK) to specialise in physics, chemistry and biology, not so much because I had particular passions for those subjects, but because I knew I would not have to write essays. I was, I discovered many years later when my daughter was so diagnosed, dyslexic. The same issue informed my decision to study dentistry at university: I knew that I would not have to write long essays. I started the first year – anatomy, biochemistry, physiology — at University College London (UCL). I really enjoyed studying these, especially comparative anatomy, under Alan Boyd. These subjects required you to think.
Not so the second year: we were thrown into the laboratory to learn how to make dentures and had to study material science (well, it wasn’t science, just the technological properties of materials used in dentistry). I was bored. I needed a break. Thanks to Arthur Profit, then Dean, I was given the rest of the year off, and went to Paris in 1969-70 for six months to study at the Sorbonne in the Cours de la civilization française. This was an amazing experience. Paris was still reverberating from the 1968 protests. Living there opened my eyes to literature, art, music and politics. I was keen to return to the UK to see if I could not register for a course in political science or similar subjects, but my parents would hear none of that! I had to complete my studies in dentistry. The thought of returning to UCL and to London depressed me, so I asked Profit to help me get into another dental school outside London. He helped me get a place at Newcastle-upon-Tyne university, and so I began my studies once again in 1970.
The return to dentistry was excruciatingly boring. The first year was spent making and fitting full and partial dentures as well as materials technology. The second year began with learning how to extract teeth, and then scaling and polishing. The rest of the four years was dominated by fillings, drillings, crownings and endodontics. These were interspersed with courses on pathology (at which I excelled), microbiology, and the usual dental curriculum. The striking thing about these years was an atmosphere in which one imagined a large sign over the school proclaiming that ‘dental students are not allowed to think’. We were never encouraged to question: it was assumed that everything that needed to be known was established. Indeed that was the norm, I discovered later, in most fields of dental science.
What I found unnerving was that the course had little to do with health: rather it appeared to be mostly about repair. We were not healing our patients, nor treating then as a whole, as people rather than just patients. Our work was focused primarily on repairing the damage done and perhaps engaging in a healthy dose of iatrogenesis. But most importantly, the ability to qualify as a dentist, or indeed to be eligible to sit the final examination, required that one produced as many fillings, crowns, bridges, S&Ps, endodontics, dentures, as you could possibly do, with a minimum requirement set for sitting the exam. So, you got into the rhythm of thinking that the more restorative interventions you did the better (no matter that the interventions were based on dubious science and were probably causing more harm than good), excellent training for general practice where the more fillings and drillings you did, the more you got paid. Inevitably, the criteria for diagnosing ‘disease’ tended towards the lowest acceptable threshold. We were taught that fissures in molars and premolars were structural weaknesses that could only be resolved by fillings. And some faculty taught that teeth themselves were pretty risky, and people would be much better off with prostheses. Interestingly, at the time I qualified, it was quite customary for many working-class people to be given full dentures as a ‘present’ by their families or loved-ones. Today, implants are all the rage, but mainly the fashion for the rich.
Much of dental education was replete with mythologies. The table below summarizes some of the myths we were made to learn:
| Streptococcus mutans causes caries | The right treatment for caries is fillings | Caries can be prevented only by adding fluoride to drinking water |
| Plaque causes gingivitis | Microorganisms are bad | Inflammation is bad |
| Periodontitis is caused by specific microorganisms | Periodontitis is result of bad behaviour, poor oral hygiene | Periodontitis is main cause of toothloss |
| You must go to the dentist every 6 months | Only dentists can treat dental diseases | Communities must be told how to behave |
Realising that learning by rote was not what I understood to be an ‘education’, I decided I would educate myself. I joined numerous student societies, and went to lectures in different departments whenever the opportunity presented itself. I acted in several plays, chaired the student community action society, and became active in a variety of organisations, especially those involved with Africa. Following the assassination of Amilcar Cabral, the poet, agronomist and revolutionary leader of the movement for independence in Guinea Bissau and Cabo Verde (PAIGC), a group of us decided to organise public education about the Portuguese colonies in Africa. We took over a nearby building where we showed films and had speakers discussing the achievements of the liberation movements. The entry ‘fee’ we asked for was for people to donate a pint of blood! We collected some 120 pints that were then dispatched via East Germany to the Mozambican liberation movement, FRELIMO. Furthermore, living in one of the poorest parts of Newcastle, my real education was provided through participating in local community struggles in my neighbourhood, a run-down working class area with poor housing and few social facilities other than the local pub.
I graduated in 1975 and moved to London where I worked for a year (part-time) in a school dental clinic in east London. The work there was purely fillings, drillings and pullings. We were not encouraged to visit schools or engage in any public initiatives. But the pay was good, so part-time work allowed me to devote the rest of my time to activism, journalism and research. I registered for an MPhil at the University of Canterbury department of politics, but never completed the dissertation I had planned on doing. I then worked for a year in general practice (again part-time) for a year, and was then offered a job as a prison dentist mainly working at Pentonville Prison (but also, from time to time, at other prisons in and around London). During this time, I also worked part-time as an immigration advisor at a community law centre. But I found practising dentistry demoralising as I felt that I was not really a health worker: I wasn’t dealing with health, I was primarily a technician. I was fascinated by the Alma Ata Declaration on Primary Health Care, by the writings on barefoot doctors in China, Mozambique and elsewhere, as well as the achievements of the Chinese revolution described in that amazing book, Fanshen. (Hinton 1966)
Returning to Kenya
The desire to return to Kenya, my home country, began to build up during these years. I should first explain how I ended up in the UK. As a child, I lived under British colonial rule in a country where apartheid laws prevailed. Until independence in 1963, schools were divided by race, with the best schools reserved for whites, technical schools for ‘Indians’, and crap institutions (‘schools’ would be a misnomer) for African people. I was sent to the first and only multiracial private primary school in East Africa for a few years, but as there were no prospects of attending a decent secondary school in Kenya, my parents sent me (as they had done my siblings) to boarding schools in England. I did the rest of my primary and secondary education there. But I always saw myself as Kenyan, and wanted to return home. On a visit to Nairobi, I met with the then Dean of the new dental school at the University of Nairobi, Sopiato Likimani (a former primary school friend). She was keen for me to join the school, but recommended that I study for a postgraduate Master’s degree before returning to Kenya.
On my return to London, I met with Aubrey Sheiham who suggested that I register for the MSc in Dental Public Health. The course was a real eye-opener for me. For the first time I came across people like Aubrey, Newell Johnson, Martin Hobdell and many others who were willing to challenge the shibboleths of the dental profession. They were people who encouraged us to think, to read, to research, to ask questions and to be creative in our approach to the issues of health rather than disease. I became fascinated by the field of epidemiology as a result of this course.
I completed the course in 1980 and in 1981 I returned to Kenya to join the University of Nairobi Dental School as a lecturer in Community Dentistry. My colleague, Jo Frencken, with whom I had done the MSc course, went to Dar es Salaam University at the same time, where I became external examiner for a few years, and we were to collaborate on several research projects.
I was taken aback by the approach to teaching and dental practice that was promoted at the dental school. It was a conventional, British (with some Russian influence from those who had studied on scholarships there) approach: drillings, fillings, pullings, scalings, dentures etc. The main purpose of the curriculum was to reproduce western style dentists. Students frequently complained that lecturers would not turn up at lectures: many faculty members spent their time doing private practice within the school, and almost no research was being undertaken by anyone when I first started. There were several junior staff who were keen to do research, so I organised regular seminars on research methodology and supervised their projects. But teaching was seriously disrupted following the government closing the university on several occasions because of student protests against the appalling food provided in their canteens. Later that same year, an attempted coup against President Arap Moi resulted in the University being closed for several months. This allowed me to spend time doing research.
The months following the attempted coup were amongst the most frightening times of my life. President Daniel Arap Moi, seen until then as a compromise and weak president who sought to balance between rival factions of the elites, began to exert his true character as a despot. Many friends and colleagues were imprisoned and tortured. Some disappeared and others left the country. For at least six months after the attempted coup, there was carnage in the streets: anyone without an ID card would be shot by police without question. My home was raided by local police who came while I was away. Before they came again, I had to get rid of dozens of books and pamphlets that were considered by the regime as potentially subversive. Quite apart from the usual books, I was advised by a lawyer friend that I should hide even the small book entitled ‘The Social Context of Dentistry’! (Davis, 1980)
It became clear to me that being part of the ‘white-coated’ profession in Kenya had distinct advantages. I did not need to apply for licenses to travel outside of Nairobi. I could gain entry to see patients in prison. I was considered ‘neutral’. While clandestinely I helped to bring together and edit a special issue of Race & Class on Kenya (Race & Class, 1983), I realised that to be able to be useful to those under attack by Moi, I had to show that I was professionally engaged as a legitimate lecturer and research at the university in a field that was seemingly ‘apolitical’, my views conveniently hidden under a white coat.
Soon after I started at the dental school, I was struck by how widespread was the prevalence of dental fluorosis in many parts of the country. Together with a colleague from India, KR Nair, who was teaching at the dental school, we published a series of papers on the occurrence of dental fluorosis and on the occurrence and distribution of fluoride in groundwater across the country. At the same time, it was apparent that the Kenya Dental Association, heavily subsidised by a well-known toothpaste-producing transnational corporation, was promoting the use of fluoride toothpaste. I raised the issue of the problem of young children swallowing toothpaste which could increase the ingestion of fluoride (Manji 1982), but was ignored. In January 1982, I wrote a piece for a national newspaper on this issue. Upon seeing the article, the Dean insisted that I go to the newspaper’s office downtown and request that the letter be withdrawn as otherwise my contract with the school was at risk. Reluctantly, I met with the editor of the newspaper who decided that rather than print a withdrawal, he would lead the next day on the issue of the Dental Association’s link with the fluoride toothpaste manufacturer. All hell broke loose. The Dental Association demanded that I attend disciplinary hearings. When I entered the room in one of Nairobi’s biggest and most expensive hotels where the disciplinary hearing was to be held, I saw the managing director of the transnational corporation, one Carl Marx (seriously!), sitting on the panel. I refused therefore to participate. This resulted in threats of being deregistered as a dentist. Meanwhile, smelling a commercial opportunity, one of the toothpaste manufacturers launched a non-fluoride toothpaste into the market. Both sets of commercial toothpaste manufacturers approached me to offer sponsorship of research and other benefits, but I refused such offers.
The controversy eventually led to an agreement that the University would organised an international conference on fluorides and dental fluorosis (Likimani, 1984). I had been in touch with Ole Fejerskov to ask his advice, as I had read several of his publications, especially the outstanding work on the TF-Index that related the clinical appearance of dental fluorosis to the histopathological features, and so included him as one of the invitees.
That was how I first met Ole, an encounter that was to have a major influence on my research and publications over the next decade and the development of a close friendship. Again, here was an individual who was not afraid to raise questions about so many assumptions about dental ‘diseases’ and who insisted that we need to relate what we observe with the biological mechanisms and histopathological evidence to really address these issues.
Becoming a full-time researcher
Following the fluoride conference in Nairobi, I was approached by the recently established state supported Kenya Medical Research Institute (KEMRI) to head up an Oral Health Research Unit, based at the what was then the Medical Research Centre, originally founded by the Dutch Royal Tropical Institute. I started work there at the end of 1983.
Before joining KEMRI, I had developed a thesis proposal for a PhD as an external student at the University of London, which Aubrey Sheiham agreed to supervise. I had also successfully raised funding from the Canadian International Development Research Centre (IDRC) to undertake the PhD research on Sugar Availability, Diet and Dental Caries. As an external student, I had very limited access to Aubrey’s time, so the work on the PhD was largely self-supervised. But I could always rely on Aubrey’s perceptive insights and suggestions. In addition, I owe a huge debt to Ole Fejerskov as he arranged for the library at Royal Dental School in Århus to supply me with all relevant literature that I needed for my research work, including for my PhD research. This was a lifeline because the Nairobi University Library had its funding depleted in the period of structural adjustment programmes and so the most recent journals available in most subjects were dated from the late 1970s. But the research work for the PhD was to take five years to complete, involving as it did several cross-sectional epidemiological studies of caries in children, assessing their diet, and measuring the presence of particular oral microorganisms. I eventually submitted the PhD towards the end of 1988, and was awarded the degree in 1989.
While I was at KEMRI, I also became involved in collaborating with other medical researchers, parasitologists, AIDS researchers, biochemists, social scientists, anatomists, microbiologists, and statisticians, and co-authored many papers with them. It was exposure to working with such scientists that fostered in me a questioning approach of not taking for granted the assumptions that prevailed in the dental field. It was also where I developed an interest in statistics and, crazily enough, in mathematics, a subject that I had absolutely hated when I was at school! The person who encouraged my learning of statistics and expanding my understanding of epidemiology was the brilliant statistician, Nico Nagelkerke, a visiting research scientist from the Netherlands. We published many papers together (see bibliography) and became close friends.
In the post attempted-coup period of 1982, the Kenya government began imposing, with the support of the International Monetary Fund and World Bank, as well as with the support of all of the ‘donor’ agencies, a set of policies that became known as “structural adjustment programmes”, policies that were eventually to result in widening the gap between the rich and the poor, vastly increasing impoverishment, privatisation of the public sphere, and concurrent decline in the quality of public health services across the country. One of the policies implemented was the introduction of user fees in all health clinics. Of particular concern was the introduction of user-fees in clinics dealing with sexually transmitted diseases, including HIV/AIDS. I brought together a team of researchers to examine the impact of user fees on attendance at these clinics. We were able to demonstrate a dramatic decline in attendance because people simply could not afford to pay. We documented the decline in detail, while in the public newspapers, there was much public protest against these policies. A few months later, Moi decided to reverse the policies, and user fees were removed, which allowed us to show the change in attendance patters due to user-fees. This research led to the only time I have had a paper published in the Lancet (Moses et al 1992). My work in the non-dental field also led to collaborations with HIV/AIDS researchers with whom I published other papers.
During my time at KEMRI, I undertook a number of epidemiological studies in Kenya (on caries, dental fluorosis, periodontal disease) and in several other African countries including Tanzania, Uganda and Zimbabwe. In Uganda I supervised the first national oral health survey. During this time I also completed my research work for my PhD. (References available on request.)
My interactions with Ole Fejerskov and Vibeke Baelum led to my undertaking research on dental fluorosis. One of the prevailing mythologies of the time, which apparently persists today, was that the most effective way of preventing dental caries was to fluoridate the water supplies. It was held that at 1ppm fluoride, there was little or no risk of dental fluorosis. But I was struck by the fact that in areas where there were low levels of fluoride in drinking water, I was still finding dental fluorosis. Ole Fejerskov and I discussed this (not long after he, Vibeke Baelum and I spent 10 days locked in an apartment writing a book on dental fluorosis (Fejerskov et al 1988).
Ole introduced me to literature on experimental studies indicating that hypobaric rats (conditions mimicking high altitude) developed enamel opacities with relatively low concentrations of fluoride in drinking water (Angmar-Månsson & Whitford, 1982). Given the wide diversity of altitudes to be found in Kenya, the hypothesis that there was an association between altitude, fluoride and dental fluorosis could be tested. I set about undertaking studies in three different communities living at different altitudes above sea level. The findings confirmed the hypothesis (Manji, Baelum & Fejerskov, 1986). When the results were presented at international meetings, deep scepticism was expressed, with accusations that I did not know how to diagnose dental fluorosis. Subsequently, studies in Tanzania speculated, but without any attempt to provide evidence, that our results were due to increased consumption of salt containing fluoride at high altitudes. Our findings have, however, since been confirmed by other studies.
The collaboration with Fejerskov and Baelum led to the establishment of a major study of caries and periodontal diseases amongst rural populations in Kenya with limited access to dental care. For many years, a Dutch research team from the Royal Tropical Institute in Amsterdam had undertaken detailed demographic mapping and health surveys in one part of (what was then known as) Machakos District, all of which provided unique information about the population we were planning to survey (Van Ginneken and Muller 1984). These studies led to a series of publications that helped us gain an understanding of the natural history of both dental caries and periodontal diseases in adults (further details of these studies are covered in Fejerskov’s paper for this meeting, so I won’t repeat them here). We had planned originally to conduct longitudinal studies in this population, but by 1989 I had left KEMRI (to join IDRC as the Regional Representative for Health Sciences in Eastern and Southern Africa), and the project unfortunately did not continue. Nevertheless, the wealth of information that we were able to gather and analyse was quite remarkable. We invited Gunar Dahlen to collaborate with us on the microbiological aspects of periodontal diseases. Newell Johnson joined us together with his team of microbiologists and immunologists (D. Beighton, JM Wilton). It was an exhilarating and exhausting time, but above all, a time of much laughter and enjoyment. (For references, see papers by Gunnar Dahlen, Newell Johnson and Ole Fejerskov for this meeting).
The publications on the patterns of tooth loss (Manji, Baelum & Fejerskov, 1988), caries (Manji, Fejerskov & Baelum, 1989) and periodontal disease (Baelum, Fejerskov & Manji, 1988) were to cause much controversy because they effectively challenged many of the assumptions about the survival of the dentition under conditions of very poor oral hygiene in populations with little or no access to dental care. There was little evidence that periodontal disease resulted in loss of teeth, and progress of loss of attachment was slow despite the context of poor oral hygiene, large quantities of plaque and calculus. Again, these findings have been well summarised in Ole Fejerskov’s paper for this meeting.
One further set of studies was to have profound impact on my thinking. Ole asked me to assist one of his PhD students, Bo Danielsen, to analyse data arising from experimental gingivitis studies that he had carried out in Aarhus (Danielsen et al 1989; 1990). What we found dramatically changed the way I came to understand the nature of the relationship between dental plaque and gingivitis, on which I will comment shortly.
These findings forced me to reflect more deeply on the aetiology of these conditions. I have published a series of papers on the theoretical aspects of the aetiology of these conditions, but the implications of the findings of these papers have not, I believe, been sufficiently recognised, perhaps because the overall story that emerged from these studies have not, until now, been told. They have major consequences, I believe, for deciding on the type of human resources that are required in the future. Let me turn to what emerged from these studies.
Caries, gingivitis and periodontitis as physiological conditions
‘We know now that the microorganisms (the microbiota) that make up the human microbiome are not just unicellular organisms living alongside each other, but instead form highly regulated, structurally and functionally organised communities attached to surfaces as biofilms, with interspecies collaborations as well as antagonisms that contribute to ecologic stability. Bacteria within a biofilm can communicate with each other by producing, detecting and responding to small diffusible signal molecules in a process called quorum sensing, which confers benefit for host colonisation, biofilm formation, defence against competitors and adaptation to changes in the environment. … To date, more than 700 prokaryotic taxa have been detected in the oral cavity, many of which cannot be isolated by common culture methods. Approximately 54% are validly named species, 14% are unnamed (but cultivated) and 32% are known only as uncultivated phylotypes.’ (Kilian et al, 2016, emphases in original).
Despite years of research and the development of increasingly sophisticated technologies, there has been a signal failure to identify specific causative agents for the development of caries, gingivitis or periodontal breakdown. While more than a hundred years ago, the idea of a non-specific plaque hypothesis prevailed as the ‘cause’ of these conditions, researchers have since turned their attention to looking for the holy grail of the causative agent(s). The main reason for such an approach has been the adoption of a paradigm created by Koch’s postulates in relation to identifying causative agents for disease. Caries, gingivitis and periodontitis were each considered as ‘diseases’, and as such, it seemed legitimate to apply Koch’s postulates to find the criminal(s). The focus of attention was on what specific microorganisms caused demineralisation (caries), inflammation (gingivitis & periodontitis) and loss of attachment (periodontitis).
The problem has been that all the evidence produced by scientists internationally at great expense, merely confirmed that these conditions have a ‘multifactorial’ aetiology, with insufficient information or knowledge about how each of the factors operate either independently or synergistically to cause ‘disease’. What these studies also concluded was that each of these phenomena were characterized by phases of progression and recovery.
Looking for the putative pathogens is like looking for a needle in a haystack. What if the answer lies not in the finding of the needle, but in understanding the dynamics of the haystack itself?
Put it another way, what if we considered these conditions not as diseases, but as dynamic physiological conditions that the result of ‘natural’ processes within the biofilm which are effectively random, some of which encourage progression, others that encourage recovery?
The fact is that all of these natural processes occur in healthy individuals. If we consider these processes ‘pathological, then we would have to conclude that everyone is sick … the prevalence of these conditions being 100%? Such a proposition is, I believe, not particularly helpful. I would argue that they are better understood as physiological processes.
We can develop models for both caries and periodontal breakdown that illustrate that such processes of progression and recovery occur unpredictably in a manner that is intrinsic to biofilm, and requires no extrinsic or pathogenic specific stimulus. And evidence from experimental gingivitis studies in humans confirm also the unpredictable characteristic of the dynamics of inflammation and recovery.
Dental caries
The pH of plaque is not constant. It varies (over time and in extent) in response to dietary stimuli, the actions of salivary and plaque buffers, salivary flow rates, the type and quality of fermentable carbohydrates available, sugar clearance rates, the microbial composition of the plaque mass, opening and closing of the mouth, and numerous other physiological and behavioural factors. All these factors are themselves highly variable or ‘noisy’. In addition, it appears that plaque pH fluctuates even in the absence of obvious external stimuli.
In most studies of the pathogenesis and epidemiology of dental caries, efforts are usually made to control for, minimize the effects of, or sometimes to ignore, the noise (‘error’) which characterizes the complex ecosystem associated with caries, in order to identify the role of particular factors. But, in fact, the noise itself may be considered the subject of interest for enhancing our understanding of dental caries. The noise within plaque generates random fluctuations in the pH close to the enamel surface[1]. The response to the random pH process is also random, but what we observe clinically is the cumulative effect of all these episodes.
In our model (Manji et al, 1991), the caries process behaves like integrated white noise, i.e. as a Wiener process or as what in physics is called Brownian motion (Einstein 1926).
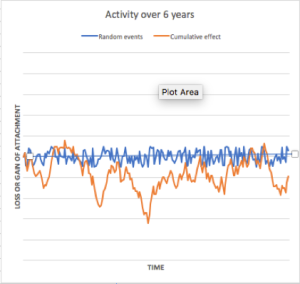
To illustrate what occurs when the effects of random fluctuations are accumulated (‘integrated’), we generated with a computer random numbers (‘pH values’) over a period of time (the magnitude of the values is not important here and may be considered large or small – and the length of period of time is also not important). Fig 1a shows the random pH fluctuations (noise). Fig1b, shows the accumulation of all these episodes – the effect on the mineral tissue. As can be seen, the result of integrating the random numbers is to produce unpredictable, and often substantial, fluctuations in the outcome, i.e., loss or gain of mineral content in response to the accumulated pH fluctuations even though the underlying random fluctuations of pH are on average equivalent to zero. Fig 1c and 1d provide further examples of similarly generated Wiener processes. The differences between these are entirely due to chance as a result of the series of random numbers that happened to be generated in each instance.
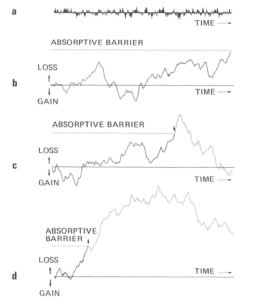
Loss of mineral from the enamel does not occur indefinitely, and once a sufficient degree of demineralisation happens, then a cavity forms – a point of no return to the original contours. In the figures, this point of no return is shown at an arbitrary positioned absorptive barrier.
As we have shown in our paper, what is striking about this model is that it provides a single explanation for two apparently distinct observations in caries epidemiology:
- The effect of fluoride is most pronounced when caries is diagnosed at cavity level, whereas the difference is negligible when demineralisation alone is considered; and
- The changes in the risk of developing caries is greatest in the period immediately after eruption.
Both these features are a function of the Wiener process and are the result of the intrinsic nature of the process.
Let me repeat: the model predicts that de- and re-mineralisation are intrinsic features of the cumulative effect of random processes that occur in the biofilm as a result of natural activities of the multitude of microorganisms. These processes occur in healthy individuals, so they cannot strictly be considered ‘disease’: the closest phrase I can propose is that these are physiological features.
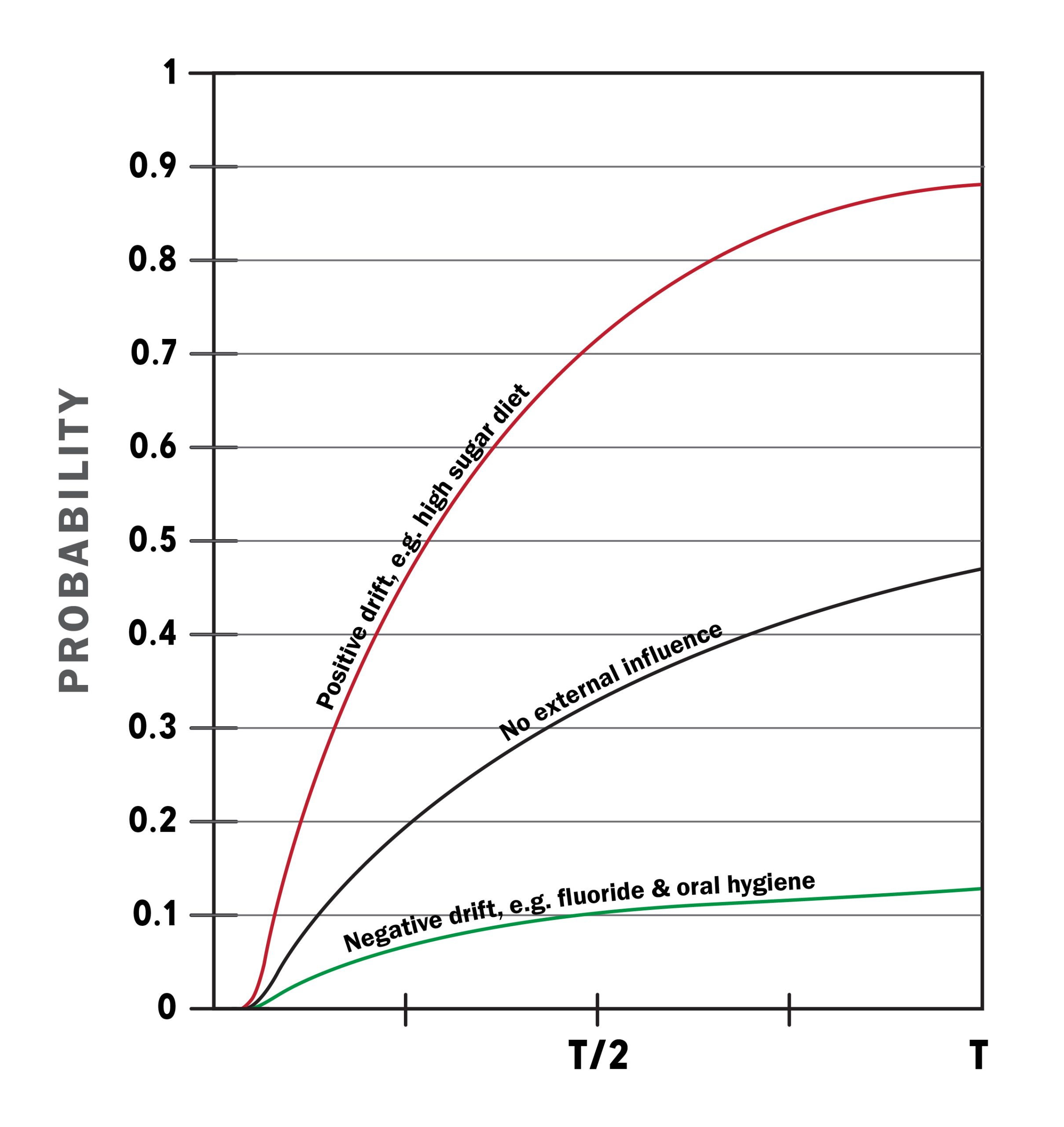
The effects of those factors that encourage demineralisation, such as consumption of refined carbohydrates, or that encourage remineralisation (such as the presence of fluorides) can be built into this model, the former increasing the probability of the absorptive barrier being reached sooner, while the latter reducing the probability of the absorptive barrier being reached. (For further details, see Manji et al 1991.)
From a point of view of intervention, the focus of attention needs to be on encouraging the process of recovery (e.g. topical fluorides), and discouraging the process of demineralisation – influences on sugar intake, being critical. This approach should be the primary intervention, something that restores the conditions in which the probability of the absorptive barrier being breached is reduced.
Periodontal disease
‘There are no clear-cut unique pathogens, while the commensal, parasitic or mutualistic interactions of microbes with each other and with the host should be viewed as a continuum without clear borders. … The literature on the evidence of microbial agents as a primary etiology of periodontitis is essentially barren for prospective cohort studies including validated assessment of exposure in periodontitis-free study populations at baseline. … From an epidemiological perspective understanding periodontitis as a complex inflammatory syndrome characterized by destruction of the supporting tissues of the teeth may provide a better frame for causal inference. The inflammatory model can be understood as the result of the possible interaction of many constellations of causal components where microbial components may be adopted, without this indicating that the researchers are devoted to a single microbial theory of destructive periodontal disease.’ Lopez, Hujoel & Belibasakis (2015)
As with caries, there has been a fruitless search for the pathogens that are responsible for periodontal breakdown. While certain microorganisms are associated with sites with periodontal breakdown, these microorganisms also occur at healthy sites where there is no evidence of breakdown.
Once again, rather than focusing on the needle, attention needs to be paid to the haystack, the biofilm in which vast numbers of microorganisms are going about their daily life of reproducing, excreting, absorbing, metabolising, interacting with each other, and generally having a good time, even in healthy individuals.
We have taken a similar approach to considering the process of progression and regression based on the assumption that the pattern of breakdown of the periodontal tissues is a random phenomenon (Manji & Nagelkerke, 1989). There has been much debate as to whether periodontal breakdown at a given site occurs in a relatively uniform linear fashion or whether the disease progresses in bursts and remissions. These are not contradictory phenomena – they are both compatible with a stochastic (random) model similar to that which I have described above in relation to the development of dental caries.
It is assumed that there are all kinds of biological events created by the multitude of bacteria, immunological responses of the tissues, repair/regeneration of the tissues etc. We assume that these are effectively random (they may not necessarily be random, but given we have little knowledge of the nature all the multiple events, we can treat these as effectively random or at least an approximation). Once again, by accumulating (integrating) the noise, the loss of attachment will behave similarly to the Wiener process / Brownian motion that we applied in the case of caries. The results so generated are shown in Fig 2.
What is important to note here is that these bursts and remissions are generated intrinsic to the process in response to the random ‘noise’ that occurs constantly within plaque. They are not necessarily caused by any extrinsic factor. It is in this sense that I speak about viewing what goes on as being physiological processes.
In each of these examples, the different pattern of loss of bursts and remissions are purely a result of the random numbers generated on a computer, and are merely a function of chance.
Fig 2. Four examples of bursts and remissions of periodontal loss of attachment generated by accumulating random events (orange line). Note: In each case, the average of the positive and negative random events (blue line) over time is set to ZERO. Differences in the pattern of bursts and remissions between the different graphs are entirely due to chance as a result of the random numbers generated by the computer.
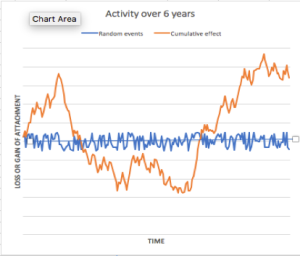
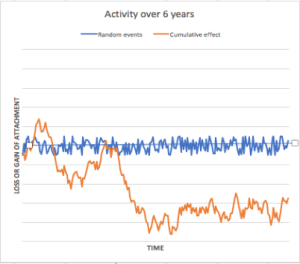
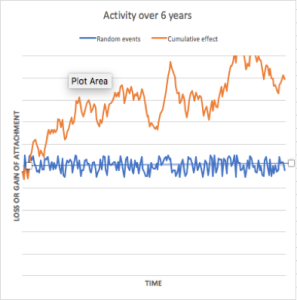
What is interesting in this model is that we can predict, even without the existence of extrinsic factors, not only progression but also recovery. The predominant model of research on periodontal breakdown has focused its attention on the factors that contribute to progression. It intrigues me that relatively little attention is paid to identifying factors that provoke or inhibit recovery. The data that Gunnar Dahlen presents in his paper regarding the findings in populations in Ghana are interesting. To what extent are the findings a reflection of factors that inhibit recovery? The importance of this frame of reference will become clearer when I discuss gingivitis below. But before doing so, let me comment on the recurrent debate about the existence of risk groups (either to caries or periodontal breakdown).
Risk groups
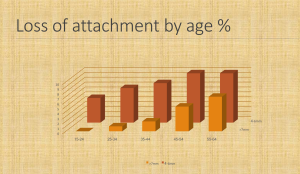
Our cross-sectional studies of caries and periodontal breakdown in adult populations in Kenya showed, as have many other studies, that severe breakdown occurs in a relatively small proportion of individuals in a population. ‘The proportion of surfaces per individual with loss of attachment ≥4 mm or ≥7 mm, and pocket depths ≥4 mm or ≥7 mm, respectively, showed a pronounced skewed distribution, indicating that in each age group, a subfraction of individuals is responsible for a substantial proportion of the total periodontal breakdown.’ (Baelum, Fejerskov & Manji, 1988). Amongst the young, the distribution of caries is also highly skewed, the bulk of the caries occurring in a minority of children.
Several people have drawn the conclusion that the skewness of the distribution of periodontal breakdown demonstrates that there are risk groups in the population, the proportion increasing with age (see for example, Newell Johnson’s paper for this meeting). The following diagram shows the intra-oral pattern of the distribution of clinical attachment loss according to tooth-type and age arising from the Kenya studies. These data indicate that a relatively small proportion of individuals exhibit substantial loss of attachment (≥7 mm).
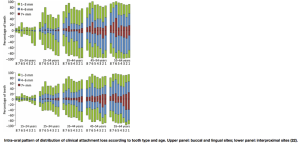
From Baelum, V. Lopez (2013
Let me begin by emphasising that risk should be distinguished from outcome. They should not be confused.
Risk is the probability of an outcome rather than the outcome itself. When tossing a coin, the probability of heads or tails is fixed (e.g. 0.5), but the outcome varies each time you toss a coin. It doesn’t matter if the outcome is the result of intrinsically random events or the influences on the outcome are many and unknown, turning a theoretically deterministic event into an effectively random case.
Risk is not something that exists independent of the knowledge of the person who assesses it. For example, consider two tumours, one benign, the other malignant and fatal. If we are not able to distinguish clinically between these two tumours, for example because of our inadequate knowledge or availability of sufficiently accurate diagnostic tests, and we therefore consider them as a single clinical entity, we would ‘know’ that individuals with such tumours have a 50% probability of dying.
However, once we know how to distinguish between such lesions, then we could state that the those with the malignant type have, if untreated, a zero chance of survival, whereas those with the benign type, have a 100% chance of survival. The risk is different now because of a change in our knowledge.
For both caries and periodontal disease, it is possible to identify two sources of ignorance that may lead to random or unpredictable outcome:
1) ignorance of the exact aetiological mechanisms involved (genetic, immunological, microbial, etc.) – the less we know about the exact mechanism and how they each operate over time, the less accurately can we predict.
2) ignorance about exposition to aetiological factors between time of risk assessment and time of outcome: we would have no idea of the sugar consumption habits, salivary flow rates, salivary buffer capacity, disturbance of plaque from brushing, etc. over time in any individual.
From the above it should be apparent that variations in outcome (levels, distributions, etc.) will say little about variations in risk.
Some argue that if the distribution of the outcome variable is not normal (i.e. it has a long ‘tail’, or is skewed), then it cannot merely be the outcome of a myriad of small unidentifiable effects but, instead, it must be evidence for the existence of at least one major etiological factor which merely needs to be identified. The underlying statistical idea behind this is, perhaps, the central limit theorem which states that the sum of the effects of many small random variables will be approximately normally distributed. However, if effects work multiplicatively, then the result of many small effects will certainly not be normal. Conversely, an outcome variable which is linearly related to an (important) risk factor will nevertheless be normally distributed if the risk factor is itself normally distributed. In short, the shape of the distribution of the outcome variable is completely uninformative (unless, of course everyone has exactly the same outcome!), and the existence of long ‘tails’ or skewness is thus not a priori evidence for the existence of risk groups. The only evidence for the existence of risk factors or groups is by actually identifying them longitudinally.
There is a limit to what can be predicted, even if we have growing amount of information about the possible risk factors involved, owing to the intrinsic randomness or unpredictability of the inputs. (For further discussion, see Manji and Nagelkerke, 1990).
Cross-sectional data shows that in all age groups, a minority experience loss of attachment in one or more sites exceeding 6mm. In the oldest age group in the Kenyan population, the proportion was less than 10%. All we can conclude from such data is that severe loss of attachment appears to progress slowly with age.
Gingivitis
Many experimental gingivitis studies have affirmed that the accumulation of plaque in the absence of oral hygiene results in an increase in the number of sites exhibiting inflammation and bleeding, and the subsequent removal of plaque results in the reduction of gingivitis. But this finding has mistakenly been taken to assume a linear relationship between the presence of plaque and the development of gingivitis. The reality is not only more complex, but more interesting.
In an analysis of experimental gingivitis studies (Danielsen et al, 1989; Danielsen et al 1990), we found that there was no correlation between the presence of plaque at specific sites and the presence of gingivitis at that site. Furthermore, the gingival status of a single site was a poor predictor of its status on subsequent occasions.
When plaque had accumulated, sites were found to convert from non-inflamed status to inflamed status as well as from inflamed status to non-inflamed status. The same was found during the phase of thorough oral hygiene. In other words, there was both a tissue reaction in the form of inflammation but also in the form of recovery.
It appeared that the proportion of inflamed sites converting to non-inflamed status (recovery) was greater than the proportion of non-inflamed sites converting to inflamed status at any given time. The estimated incidence rate remained fairly constant during both the plaque accumulation phase and the oral hygiene phase, whereas the estimated recovery rates was considerable lower during the plaque accumulation phase compared to the oral hygiene phase.
In other words, the rate at which new sites exhibited gingival inflammation remained more or less the same during the poor oral hygiene phase as when the teeth were thoroughly cleaned. However, the plaque accumulation appeared to affect the rate at which the tissues recovered from inflammation.
What these data suggest is that what we term gingivitis could be considered as a physiological phenomenon in which the incidence rates continue to remain constant both during poor oral hygiene and after thorough cleaning. The steady-state prevalences derived from the estimated incidence and recovery rates were quite similar to the actual findings after 14 days of plaque accumulation and the subsequent 10 days of thorough oral hygiene.
On the basis of these experimental gingivitis studies, it was not possible to say whether or not the presence of inflammation could lead to further periodontal breakdown. The cross-sectional epidemiological data from Kenya suggest that the ubiquitous accumulation of plaque and poor oral hygiene and the presence of bleeding amongst populations with little access to dental care is not associated with periodontal breakdown and loss of teeth. However, it is quite possible that since plaque reduces the tissues’ ability to recover from inflammation, over a period of time there will be bursts and remissions in periodontal breakdown unpredictably, just as the transition to and from gingival inflammation is unpredictable. But what is of critical importance is that plaque appears not so much implicated in causing inflammation as in inhibiting the tissues ability to recover.
Implications for oral health care
The literature on oral health care planning is replete with arguments that are based on how to control the over-production of dentists (in order that they can protect their market power?), or what kind of cadre can be developed that obviates the need for dentists to carry out the most tedious routine tasks, or reduce the cost of providing care.
Dentistry owes its origins to the artisanal class of barbers who, in many parts of the world, were responsible for extracting teeth and carrying out circumcisions. It was only when ether’s anaesthetic powers were discovered that dentists, seeking approval from the medical profession, were able to establish their own profession while imposing restrictions on the ability of those who had been their professional ancestors to continue to engage in oral interventions (Davis 1980). Furthermore, the dental profession has always sought recognition, acceptance and admission by the medical profession, and current discussions about the future of dentistry continues to hark back to the need for dentists to become part of the hallowed medical professions, despite the fact that the majority of the work done by dentists today is cosmetic, technical and in many cases iatrogenic.
Moreover, the substantial literature on dental public health that speaks about what Third World countries should do is most often written by Westerners. Even if dressed up as ‘not making the same mistakes as we have’, such literature frequently has implicit in its arguments that there can be one kind of healthcare for ‘us’ (i.e. Westerners), and quite another for ‘them’ (those barbarians!). There is frequently the assumption that because Western societies have a long history of producing dentists, it is difficult to bring about change, while Third World countries are assumed to have no history, rather mimicking Hegel’s and other Enlightenment philosophers’ viewpoint that places like Africa have no history!
Much of dental public health planning and discussions about the need for different cadres (therapists, hygienists, etc.) are informed by a perspective that takes for granted the ‘sanctity’ of the profession itself. It is informed by self-interest, rather than considerations of the conditions that the community faces, an understanding of the biological (and physiological) processes involved, as the basis for deciding both what kind of personnel is required, and what kind of training is needed, or more importantly, what interventions are needed.
If, as I have argued in this paper, the three major phenomena that the majority of dentists are concerned with —dental caries, gingivitis and periodontitis- are physiological conditions, rather than ‘diseases’, then it seems to me that a radical rethink is needed if the aim is to improve the health and well-being of the community rather than to improve the financial health of members of the profession.
If severe loss of attachment is a phenomemon seen in a minority of the population, and if periodontal ‘disease’ is not the principal cause of tooth mortality, then interventions related to periodontal conditions would not appear to be a major priority. Perhaps there may be only aesthetic and social reasons for encouraging oral hygiene in relation to periodontal conditions. Our studies suggest that scaling and polishing of teeth has little value in terms of ensuring the longevity of the dentition, but may be considered as cosmetic interventions.
In any case, the evidence suggests that gingivitis and periodontal conditions are characterized by phases of progression and recovery. The same is true for dental caries. The fundamental requirement has to be to design public interventions that promote the process of recovery, that prevent those factors that inhibit recovery, and hinder the process of progression.
For caries, pain relief and reconstruction to achieve a functional dentition is clearly necessary where lesions have been allowed to reach the pulp. In all other cases, we should be looking at how we can intervene non-mechanically to encourage recovery of the lesions by encouraging remineralisation. But restoration has to avoid iatrogenesis. This requires a major rethinking of dental practice.
No serious healthcare system can accept the way in which the sugar industry has sought both to encourage dependence on their products as well as suppression of information about the negative impact of refined carbohydrates on the health of the individual, in particular the consequences for obesity and diabetes, let alone the damage done to the dentition. Public awareness, exposure and media coverage, similar to that which was done in relation to the tobacco industry, is needed. Gary Taubes’ recent book, The Case Against Sugar, should be mandatory reading for all health professionals to really understand the way in which the sugar industry operates, and how obesity and diabetes are growing health problems especially amongst the most impoverished in urban areas where access to alternatives to high refined carbohydrates is generally limited.
Main implications
- Microorganisms in biofilm are commensals – there is no need to blame ‘immigrants’. Periodontitis, gingivitis and caries are all produced by commensals, and so it would be misleading to refer to these as infectious diseases.
- Postulate: events in plaque are effectively random.
- Cumulative effect of noise leads to progression and recovery without the need to postulate that they are caused by changes in microbial composition. Changes in microbial composition may well occur as a result of changes in the tissues caused by unpredictable progression and recovery of the tissues.
- Response of tissues unpredictable at any given moment but can be positive or negative
- It is not possible to “prevent” caries, periodontitis or gingivitis, but they all can be controlled — i.e. probability of negative outcome can be reduced
- Caries, periodontitis and gingivitis are all associated with physiological processes occurring in plaque/ biofilm
- Plaque appears not so much to ’cause’ breakdown as to cause delays in the recovery of tissues
- Inflammation is the host response to injury. It’s a ‘good thing’!
- The primary task of the oral health professions should be to ensure that people retain a functional dentition for life. Interventions that are made to ensure that outcome should be based on an understanding of the underlying biological processes, primarily to reverse the processes that lead to destruction of the dentition and promote those that encourage recovery.
- Oral health professions need to be proficient at analysing the political and economic factors that contribute to conditions unfavourable to the maintenance of good health, and proficient in advocating policies that limit the ability of corporations to profit from causing ill-health (just as the medical profession has done so against the tobacco and pharmaceutical industries). Thus, for example, the sugar and related industries need to be amongst the primary targets of the profession. Alliances should be formed with health professionals engaged in advocating social policy related to obesity and diabetes. Similarly, analysis of the influence of privatized policies, corporate policies and insurance company policies on what is treated and how.
- Billions are spent every year to promote people to eat substances containing sucrose, fructose syrups, and other refined carbohydrates, and in many communities, access to healthy foods is limited both by cost and availability. The medical & dental professions tendency to blame the victim for the disruptions to their metabolism has to be challenged.
- The professions should be held accountable to the public by demonstrating their success in promoting recovery of the oral tissues. The incidence of restorations, endodontics, extractions should be considered as markers of failure, and annual targets should be set to reduce their occurrence.
- The secondary task of oral health professionals is emergent care: relief of pain, management of trauma, diagnoses of soft-tissue pathologies, and where justifiable from the point of view of health, interventions to establish a functional dentition.
- All other pre-occupations of oral health professionals should be considered fundamentally cosmetic, except where there is an evidence-based rationale that the interventions are essential for the maintenance of health or required because of severe disfigurement.
- If this the basis for what oral health professionals should be doing, then a profound overhaul of the curriculum is required. A significant proportion of interventions required to ensure health can be undertaken by community-based workers who are provided with basic training. The remaining tasks would require relatively few dentists and cosmeticians.
- Health is a democratic right. The ability of live a healthy and productive life is fundamental. The existence of private health care always results in a two-tier healthcare system. But worse, the provision of care that is inevitably driven by the rate of profit means that treatments tend towards those procedures that provide the greatest returns, procedures that are not always coincident with achievement of health.
- As a democratic right, health is achievable only by enabling communities to exercise agency in ensuring that the conditions for good health pertain. Democracy presupposes citizens playing a role as agents not as recipients or objects of the actions of the dental profession.
Too much of the work we have hitherto been trained to undertake is based on questionable scientific evidence. Our task in establishing dentistry on an ethical basis is to be willing to fight the truth decay that has so long been associated with dentistry. Otherwise, dentistry becomes a refuge from uncertainties, promising – and in some measure delivering – the miracle of freedom from thought.”
To sin by silence, when we should protest,
Makes cowards out of men.
“Protest” by Ella Wheeler Wilcox (November 5, 1850–October 30, 1919)
Bibliography
Angmar-Månsson B, Whitford GM. Plasma fluoride levels and enamel fluorosis in the rat. Caries Res. 1982;16(4):334-9.
Baelum V, Fejerskov O, Manji F. Periodontal diseases in adult Kenyans. J Clin Periodontol 1988;15:445-52.
Baelum, V. Lopez, R. Periodontal disease epidemiology – learned and unlearned? Periodontology 2000; 2013. 62:37-58.
Danielsen B, Manji F, Nagelkerke N, Fejerskov O, Baelum V. Effect of cigarette smoking on the transition dynamics in experimental gingivitis. Journal of Clinical Periodontology. 17(3):159-64, 1990
Danielsen B; Manji F; Nagelkerke N; Fejerskov O; Baelum V. Transition dynamics in experimental gingivitis in humans. Journal of Periodontal Research. 24(4):254-60, 1989
Davis P: The Social Context of Dentistry. London: Longwood, 1980
Einstein, Albert (1926) Investigation on the theory of Brownian movement, London: Methuen, 1926.
Fejerskov O, Manji F, Baelum V, Moller IJ (1988): Dental Fluorosis: A Handbook for Health Workers. Copenhagen Munksgaard.
Hinton, William: Fanshen: Documentary of Revolution in a Chinese Village. London: Penguin, 1966
Kilian M, Chapple, I. L. C., Hannig M, Marsh P. D., Meuric V., Pedersen A. M. L., Tonetti M. S., Wade W. G. and Zaura E.: The oral microbiome – an update for oral healthcare professionals. British Dental Journal 221 (10) 657-66, 2016
Likimani, S. (ed.) (1984). Fluorosis research strategies. Proceedings of Workshop, Nairobi: University of Nairobi
Lopez, R. Hujoel, P & Belibasakis GN (2015) On putative periodontal pathogens: an epidemiological perspective, Virulence, 6:3, 249-257
Manji F: Is fluoride toothpaste appropriate for Kenya?. East African Medical Journal. 59(7):499-501, 1982
Manji F, Bælum V, Fejerskov O (1986): Fluoride, Altitude and Dental Fluorosis. Caries Research 20 (5) 473-480
Manji F, Fejerskov O, Nagelkerke NJ; Baelum V. A random effects model for some epidemiological features of dental caries. Community Dentistry & Oral Epidemiology. 19(6):324-8, 199
Manji F, Bælum V, Fejerskov O. Tooth mortality in an adult rural population in Kenya. J Dent Res 1988; 67:496-500.
Manji F, Fejerskov O, Baelum V. Pattern of dental caries in an adult rural population. Caries Res 1989;23:55-62.
Manji F, Kapila S (1986): Fluorides and fluorosis in Kenya. Part III: Fluorides, fluorosis and dental caries. Odontostomatol Trop [reference to be inserted]
Manji F, Kapila S: Fluorides and fluorosis in Kenya. Part II: The occurrence of dental and skeletal fluorosis. Odontostomatol Trop 9 (2) 71-74 1986;
Manji F, Kapila S. Fluorides and fluorosis in Kenya. Part I: The occurrence of fluorides. Odontostomatol Trop. 1986 9(1):15-20;
Manji F, Nagelkerke N. What can variations in disease outcome tell us about risk? Community Dentistry & Oral Epidemiology 18(2):106-7, 1990
Manji F; Nagelkerke N. A stochastic model for periodontal breakdown. Journal of Periodontal Research. 24(4):279-81, 1989;
Manji F: Excessive fluoridation in Kenya. British Dental Journal. 153(5):168, 1982 Sep 7.
Moses, S.; Manji, F.; Bradley, J. E.; Nagelkerke, N. J. D.; Malisa, M. A.; Plummer, F. A. Impact of user fees on attendance at a referral centre for sexually transmitted diseases in Kenya. Lancet 1992. 340(Aug. 22):463-466
Nagelkerke NJ Manji F. The effect of measurement errors in confounders on adjustment. International Journal of Epidemiology. 18(3):732-3, 1989
Nagelkerke NJ; Plummer FA; Holton D; Anzala AO; Manji F; Ngugi EN; Moses S. Transition dynamics of HIV disease in a cohort of African prostitutes: a Markov model approach. AIDS. 4(8):743-7, 1990
Nagelkerke, N. J. D., Manji, F.; Muttunga, J. Epidemiology and statistics in diarrhoea research Ottawa: IDRC, 1990
Nair KR, Manji F, Gitonga JN: The occurrence and distribution of fluoride in groundwaters of Kenya. East African Medical Journal. 61(7):503-12, 1984;
Race & Class: Special Issue on Kenya 24 (3) 1983
Žižek, Slavoj, In Defence of Lost Causes. London: Verso. 2008: 69
Van Ginneken, JK and Muller AS (eds) (1984): Maternal and Child Health in Rural Kenya: An Epidemiological Study. London: Croom Helm
For further bibliographic references for research in Kenya, see the essay by Ole Fejerskov in this volume.
- The noise can be considered effectively random (or an approximation) under conditions where we do not have information or knowledge about the role of each of the factors involved in causing rises and falls of pH – see later in my discussion about periodontal breakdown. ↵
