8
Learning Objectives
- Managing care for high-risk infants including those with ineffective airway clearance, impaired gas exchange, ineffective thermoregulation, unstable blood glucose, infection, injury, and pain
- Preterm v. Full Term v. Postterm
- Risk factors for complications in the newborn period
Topics
- Defining “complicated” newborn and NICU philosophy
- Nursing care preparation-expected complications
- Nursing assessment variations
- Prematurity versus postmaturity
- Thermoregulation risks
- Feeding and nutrition
- Large for gestational age (LGA) and hypoglycemia
- Hyperbilirubinemia
- Neonatal infection
- Respiratory compromise
- Abstinence
- GI/GU disorders
Complicated Newborn
As you learned in previous chapters, infants are dependent on the functions of the mother and placenta to breathe, eat, eliminate, and protect from infection. Although designed to be an ideal environment, the womb is not always a conducive place to support growth and development. So what exactly does it mean to become a “complicated” newborn? Infants born who do not transition to extrauterine life effectively, encounter post-birth conditions either independently or related to the mothers’ condition, suffer from congenital abnormalities, are pre-term and post-term, or any factor placing them at high-risk fall into a non-normal path. This path ensures their need for closer monitoring, individualized care, specialized testing, and support. As you can imagine, this is a very difficult time for the parents too as their birth and feeding plans are suddenly derailed. Psychosocial support is critical during this time, often requiring a team approach.
NICU Philosophy
Each health care organization develops its own care-related philosophy related to its tiniest patients, however, one consistent theme nationally is to maintain a family-centered care concept. Navigating to a new normal, parents often feel helpless as they embrace the NICU environment. As a NICU nurse, it will be your role to create and maintain a gentle, soothing, and non-intimidating atmosphere. Additionally, parents will require daily education, preparation for discharge, opportunities to bond, and be included in care delivery when feasible.
Nursing Care Preparation-Expected Complications
It is not always possible to be prepared for infant complications, however, there are certain maternal, delivery, and infant or congenital diagnoses that place the infant at risk. These are:
Maternal Factors
- Being younger than age 16 or older than 40 (see Advanced Maternal Age)
- Drug or alcohol use
- Diabetes
- High Blood Pressure (hypertension)
- Bleeding
- Sexually Transmitted Diseases
- Multiple pregnancies (twins, triplets, and more)
- Oliguria and Polyuria
- Premature rupture of membranes (PROM)
Delivery Factors
- Fetal distress or birth asphyxia
- Breech presentation (buttocks first) or other abnormal position
- Infant stools in utero (meconium in the amniotic fluid)
- Nuchal cord (umbilical cord wrapped around the baby’s neck)
- Forcep usage or cesarean delivery
Baby Factors
- Baby born at a gestational age of <37 weeks or > 42 weeks (Quick quiz: Do you remember what term is?)
- Birth weight less than 5 lbs, 8 ounces (2500 grams) or over 8 lbs, 13 ounces (4000 grams)
- Small for gestational age (term infant who weighs less than they should)
- Resuscitation in the delivery room
- Birth defects
- Respiratory distress
- Infections such as herpes, group B streptococcus, chlamydia
- Seizures
- Hypoglycemia
- Need for oxygen, IV fluids, or medication
- Need for special treatment, testing, or blood transfusion
In the event complications are expected, the NICU team will attend the delivery or be close by to intervene. The team includes a Neonatologist, Neonatal Nurse Practitioner, Respiratory Therapist, and often a Pharmacist. Specialized training and certification are needed to care for both normal newborn and NICU patients, which will provide you with the knowledge needed to successfully care for this population.
Nursing Assessment Variations
Recalling the importance of APGAR scoring, ongoing assessments should follow the same level of importance even if the infant appears normal. Complicated neonates are not able to communicate illness, pain, or abnormalities in the same way normal newborns do. Their ability to cry is often an energy expenditure they cannot afford due to other physiological demands. Subtle changes in vital signs, ability to regulate temperature, skin appearance and color, feeding intolerance, and lethargy are all signs requiring further evaluation and physician notification.
Neonatal Vital Signs
Heart Rate Respiratory Rate
- Preterm < 1 kg* 120-160 40-60
- Preterm 1 kg 120-160 40-60
- Preterm 2kg 120-160 40-60
Temperature ranges greater than 97.7 F (36.5 C*) and less than 99.5 F (37.5 C)
*NICU’s embrace the metric system nationally to include g, kg, ml, C, cm, mm
Prematurity and Postmaturity Complications
It may come as a surprise, but infants who deliver post-term (or post-dates) are at increased risk for certain complications similar to infants born preterm. According to the World Health Organization (2018),
- Preterm is defined as any baby born alive prior to the completion of 37 weeks (just before 38 weeks)
- Moderate to late preterm (32-37 weeks)
- Very preterm (28-32 weeks)
- Extremely preterm is any infant born at less than 28 weeks gestation
Caring for a premature infant can be challenging. The greatest indicators of an infant’s health and survival are their gestational age, birth weight, and Ballard score >37 weeks. Complications related to respiratory system maturity, gastrointestinal (GI) and feeding intolerances, and thermoregulation are common. Increased incidence of death and long/short term disability have been linked to low birth weight in particular.
Complications
Complications can occur regardless of gestational age. Some risk factors, as mentioned previously, are consequences related to factors associated with delivery, infant, or the mother. The most common risk factors to discuss include:
- Thermoregulation risks
- Feeding and nutrition
- Large for gestational age (LGA) and hypoglycemia
- Hyperbilirubinemia
- Neonatal infection
- Respiratory compromise
- Abstinence
- GI/GU disorders
Thermoregulation Risks
As the cornerstone of neonatal care, thermoregulation serves as a key component unlocking the doors to stress levels, oxygen consumption, and metabolic stability. Maintaining a thermoneutral environment, between 36.5 C and 37.5 C, is the optimum environmental temperature for a preterm infant. At a neutral temperature, a preterm infant will reduce oxygen and energy expenditures, experience decrease levels of stress, and achieve metabolic stability. Why is this important? (hint: brown fat)
The importance of gestational age in the matter of heat generation, or thermogenesis, centers around the production of brown fat. Brown fat or brown adipose tissue (BAT) stores energy, creates heat, and burns calories without the need for shivering. In short, brown fat protects infants from hypothermia. But, what if you don’t have brown fat? Brown fat has been present as early as 20 weeks gestation, however, this is not the norm. A moderate index is present at approximately 29 weeks gestation, with stabilization by 35 weeks. As you can deduce, prematurity, as well as intrauterine growth restrictions, means less brown fat, fewer energy stores (hypoglycemia), less heat generation (hypothermia), increased caloric requirements (altered acid-base balance), and increased oxygen demands (hypoxia). Luckily, artificial environments in the form of isolettes and warmers are used to assist the preterm infant in reaching a thermoneutral environment. You will learn more about growth restriction in later content.
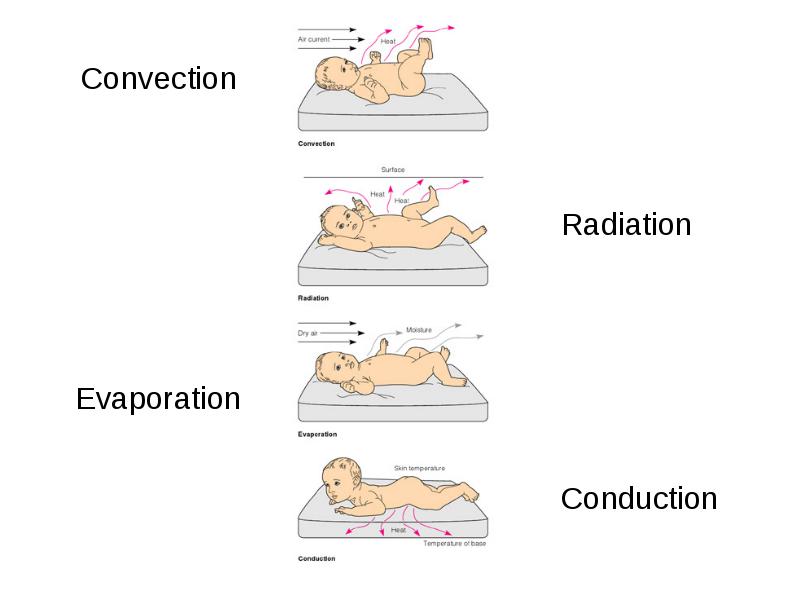
Heat Loss (4 ways an infant can experience loss)
- Radiation-Loss occurs when body heat is transferred to cooler surfaces and objects
- Evaporation-Loss of heat incurred when water is converted to a vapor
- Convection-Loss of heat from the warm body surface to the cooler air current
- Conduction-Loss of heat to a cooler surface by direct skin contact
Relational Rewind
- Cold stress is a cascade of physiological events caused by the infant’s use of chemically mediated thermogenesis in an attempt to increase core temperature. Two specific alterations to thermogenesis occur in the infant suffering cold stress; vasoconstriction of the peripheries, which allows heat to be drawn back to the core and metabolism of brown adipose tissue.
- Heat stress may also be incurred if an infant is exposed to high environmental temperatures, often associated with increased heart rate, increased respiratory rate, and decreasing stability. It is imperative to ensure frequent observation of probe placement when utilizing a thermoregulatory device (warmer or isolette) to avoid a false-low reading if the probe becomes detached, which will result in high heater output.
*NOTE: Rewarming an infant does not go without risk and should be completed slowly by 0.5 degrees C per hour to avoid the potential for seizures.
Feeding and Nutrition
Feeding babies in the NICU is quite different from feeding healthy babies. When babies are sick or premature, they are often not well enough to breastfeed or take a bottle. Premature babies may not be able to suck effectively, or their GI (gastrointestinal) tracts may not be mature enough to digest feedings. Babies who have unstable health, such as altered thermoregulation (mentioned above), respiratory distress, or sepsis are often unable to take regular feedings. Babies with umbilical catheters and those who need help breathing, such as with a mechanical ventilator, may not be able to be fed. This is because of the risk of problems such as aspiration (breathing food into the lungs) or necrotizing enterocolitis (NEC) which we will cover later.
Relational Rewind
Consider: In what ways are thermoregulation, nutrition, and respiration linked? As a nurse caring for a preterm infant, what interventions are needed to prevent or minimize risk factors associated with each?
Large of Gestational Age (LGA)
Large for gestational age is a term used to describe babies who are born weighing more than the usual amount for the number of weeks of pregnancy. LGA babies have birth weights greater than the 90th percentile for their gestational age, meaning that they weigh more than 90 percent of all babies of the same gestational age. The average baby weighs about 7 pounds at birth. About 9 percent of all babies weigh more than 4,000 grams (8 pounds, 13 ounces). It is rare for babies to weigh over 10 pounds. Although most LGA babies are born at term (37 to 41 weeks of pregnancy), a few premature babies may be LGA and appear older than their actual gestational age.
There are multiple causes for an infant to become LGA. They include genetics, maternal weight gain, and maternal diabetes. Diabetes during pregnancy causes the mother’s increased blood glucose (sugar) to circulate to the baby. In response, the baby’s body makes insulin. All the extra sugar and the extra insulin production can lead to excessive growth and deposits of fat, thus, a larger baby.
Relational Rewind
Consider: What happens when insulin is given to someone who doesn’t really need it? (hint: baby after delivery) What nursing interventions and/or monitoring would be needed?
Large for gestational age (LGA) infants are also at increased risk for injury, especially if delivery was long, complicated, or the infant’s size was unexpected. A brachial plexus injury is common under these circumstances and is an unintended consequence requiring medical intervention and testing. When a strong force increases the angle between the neck and shoulders, the brachial plexus nerves might stretch or tear. The injury may also pull the nerve roots of the brachial plexus from the spinal cord. Damaged nerves carry sensation poorly and make muscle movements weak. Upon assessment, you may notice a full or partial lack of movement in the affected arm or the infant may cry with movement or manipulation of extremity. Diagnostic tests should be expected and include x-rays, computed tomography (CT), and magnetic resonance imaging (MRI). Nursing interventions would include parent education and reinforcement of medical treatment such as an arm-sling.
Hypoglycemia
Glucose is essential for brain function regardless of age. Glucose in insufficient amounts can harm the brain’s ability to function and have severe or long-lasting effects such as seizures and serious brain injury. The term Hypoglycemia is used to describe the level of sugar (glucose) in the blood as being too low. In a newborn baby, low blood sugar can happen for many reasons. It can cause problems such as shakiness, blue tint to the skin, and breathing and feeding problems. Although prevention is critical, there may be times when it is not possible due to risk factors. The population affected is both preterm and term infants alike.
Defined-Plasma glucose concentration of <40mg/dl
- Risks Factors :
- Preeclampsia (see complicated antepartum)
- Infant diabetic mother (IDM) (See complicated intrapartum)
- Small for gestational age (SGA)
- Small twin
- Metabolic disorders
- Signs/Symptoms
- Lethargy
- Apathy
- Limpness
- High-pitched cry
- Irritability
- Tremors
- Apnea
- Respiratory distress
- Pallor
- Cyanosis
- Poor Feeding
- Exaggerated Moro reflex
- Treatment
- Early breastfeeding
- PO formula supplementation
- IV fluids of D10W, D12.5W
- Boluses
- Glucagon
- Frequent monitoring
- Corticosteroids (in severe cases)
- Your organization will have its’ own protocol for screening, testing, and treatment
Jaundice-Physiologic versus Pathological
Direct bilirubin –In the liver, bilirubin is changed into a form that the body can get rid of. This is called conjugated bilirubin or direct bilirubin. This bilirubin travels from the liver into the small intestine. A very small amount passes into your kidneys and is excreted in your urine. Since this is a metabolic process, the absence of infant feedings can result in altered excretion (stooling) resulting in bilirubin being deposited in subcutaneous tissue underneath the skin, causing a yellow appearance.
Physiologic Jaundice is a normal process that occurs during the transition from intrauterine to extrauterine life and appears after 24 hours of life. The predominance of unconjugated bilirubin peaks at 4-5 days of age. (key term-conjugated versus unconjugated).
Etiology:
- Infants have a shorter red blood cell lifespan of 90 days compared with 120 days in adults
- Poor hydration from initial inadequate breastfeeding
- Cephalohematoma/bruising
- Slower uptake of bilirubin by the liver
- Inadequate intestinal bacteria
Pathological Jaundice occurs when there are pathological levels of unconjugated and conjugated hyperbilirubinemia present. Also marked by presentation, this type of jaundice will be noted upon assessment within the first 24 hours of life and will last ≥1 week in term infants and ≥2 weeks in preterm infants.
Etiology:
- Prematurity
- Hemolytic disease
- Rh disease
- ABO incompatibility
- Unrecognized
- Cephalohematoma and/or significant bruising
- (increased RBCs to hemolyze)
- Exclusive breastfeeding
- Infection
As a nurse caring for a newborn infant, both term and preterm, you will assess the risk of bilirubinemia with the use of a Bilitool. Diagnostic testing through blood collection is critical to determining intervention levels ranging from phototherapy to an exchange of blood by means of a transfusion. Phototherapy lowers the bilirubin levels in the blood through a process called photo-oxidation. Photo-oxidation adds oxygen to the bilirubin so it dissolves easily in water. This makes it easier for your baby’s liver to break down and remove the bilirubin from their blood. Ultimately, this process eliminates the need for liver conjugation of bilirubin.
Kernicterus, which is an abnormal accumulation of unconjugated bilirubin in basal ganglia, MUST BE AVOIDED. If not prevented, can cause neurological disorders, deafness, delayed motor skills, hypotonia, and intellectual deficits. (See kernicterus link to EBP article from the American Academy of Pediatrics).

Exercises
Compare Pathological Jaundice and Physiologic Jaundice:
_________________ Jaundice presents as:
- Jaundice appears before 24 hours
- Rise in serum bilirubin by more than 5mg/dl/day
- Serum bilirubin > 15mg/dl
- Jaundice present beyond 14 days of life
- Direct bilirubin >2mg/dl at anytime
_________________ Jaundice presents as:
- First appears after 24 hours of age
- Serum bilirubin < 15 mg/dl
- Jaundice undetectable after 14 days
- Maximum intensity is seen 4-5 days in term and day 7 in preterm
Neonatal Infection and Sepsis
Neonatal sepsis is a blood infection that occurs in an infant younger than 90 days old and is the leading cause of death in neonates. Early-onset sepsis is seen in the first week of life. Late-onset sepsis occurs after 1 week through 3 months of age. Neonatal sepsis can be caused by bacteria such as Escherichia coli (E Coli), Listeria, and some strains of streptococcus. Group B streptococcus (GBS) has been a major cause of neonatal sepsis. However, this problem has become less common because mothers are being screened during pregnancy. The herpes simplex virus (HSV) can also cause a severe infection in a newborn baby. This happens most often when the mother is newly infected.
Early-onset neonatal sepsis most often appears within 24 to 48 hours of birth means the newborn infant contracted the infection from the mother before or during delivery, also known as vertical transmission. The following will increase an infant’s risk of early-onset bacterial sepsis:
- GBS colonization during pregnancy
- Preterm delivery
- Water breaking (rupture of membranes) longer than 18 hours before birth
- Infection of the placenta tissues and amniotic fluid (chorioamnionitis)
- Transplacental transfer (e.g., syphilis)
- Ascending infection
- Ascends into the uterus from prolongs rupture of membranes (ROM)
- Intrapartum exposure (e.g., Herpes simplex virus [HSV])
Other Risk Factors
- All infants are relatively immunocompromised
- Sexually transmitted infections (STIs)
- Untreated Group B Strep (GBS)
- Administration of IV penicillin to GBS positive mothers has greatly reduced the risk of infection among neonates
Can feeding an infant help to reduce the risk of infection?
- Passive transmission of maternal IgA antibodies occurs via maternal colostrum in breastfed infants
- Therefore risk for neonatal infections is greater in bottle-fed infants
Neonatal Group B Streptococcus-most common infection associated with newborns and can cause sepsis, meningitis, pneumonia, and urinary tract infections. Group B Streptococcus (GBS) is gram-positive diplococcus that is a common colonizer of the gastrointestinal and genital tracts. GBS colonization in pregnant women is generally asymptomatic. However, maternal colonization is the primary risk factor for GBS infection in neonates and young infants.

Relevance Rewind
Which type of delivery places the newborn at increased risk for Group B Strep infection? (hint: consider transmission)
- Neonatal Treatment IV-7-10 days dependent on blood cultures
- Ampicillin
- Gentamicin
Warning: Case Presentation Similarity
Sepsis can present with the same symptoms as a congenital heart defect (See PDA). Be thorough in your assessment and prompt with physician notification. Any fever >99.1 F or inability to maintain a temperature >97.6 F (infant is too cold despite efforts to warm <97.6 F) within the first 28 days of life is a medical emergency and requires intervention. Discharge teaching is critical, especially with new parents.
Patent Ductus Arteriosus (PDA)
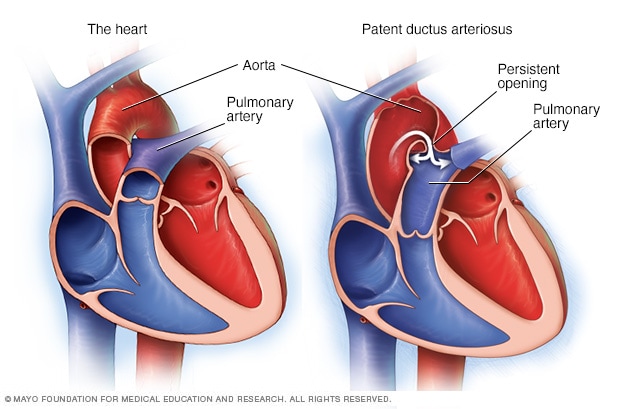
What is a Ductus Arteriosus?
- A large vessel that connects the aorta and pulmonary artery in utero
- An essential part of fetal blood circulation
- In utero, the ductus shunts blood away from the fluid-filled lungs
- After birth, the ductus arteriosus should close and create a normal circulation of blood through the heart.
What happens if it doesn’t close as expected? (Be sure to see “Case Warning” above)
Patent Ductus Arteriosus (PDA) (recall the meaning of “patency”)
- Failure of the ductus arteriosus to close within 72 hours after birth
- PDA in term infants is more likely to be from a functional defect
- PDA in preterm infants is more likely to be from immaturity
Assessment Findings to note:
- Systolic murmur second intercostal space left upper sternal border
- In general, the louder the murmur, the smaller the PDA
- Tachycardia and tachypnea
- Bounding pulses
- Increased demand for O2 and ventilatory support
- Confirmed by echocardiogram
- ECHO: a diagnostic test used to determine patency
- A chest x-ray may show increased pulmonary vasculature, pulmonary edema, cardiomegaly
Treatment
- Wait (if asymptomatic)
- Prostaglandin inhibitor to facilitate PDA closure
- (Indomethacin [“Ind to End”])
- PGE (“P to prolong”) PDA in PDA-dependent lesions
- Diuretics
- Strict I&O – restrict fluids
- Cardiology consult
- Surgical ligation if indicated and not responding to Indomethacin
- Prepare family for possible surgery and post-op care
Respiratory Compromise
Neonatal Respiratory Distress Syndrome (NRDS) is a frequent cause of increased morbidity and mortality in neonates. As a common cause of respiratory distress in a newborn, Respiratory Distress Syndrome (RDS) presents within hours after birth, most often immediately after delivery. NRDS primarily affects preterm neonates due to a deficiency of surfactants of either inadequate surfactant production, or surfactant inactivation in the context of immature lungs. Prematurity affects both these factors, thereby directly contributing to NRDS and the potential need for respiratory support.
- Potential life-threatening lung disorder resulting from underdeveloped alveoli and insufficient levels of pulmonary surfactant
- Alteration in alveolar surface tension
- Atelectasis (collapse of part or all of lung)

Surfactant Deficiency
Have you ever tried to blow up a balloon that is new and has not been stretched? How hard is it to blow up? Correct! It is nearly impossible because the balloon has very high surface tension. However, when you stretch it out, blowing it up becomes less difficult. Why is this? The “stretching” action (similar to surfactant) created the surface tension to be less allowing the balloon to fill with air more easily. (Note: A good way to remember Surfactant is “WD40 of the lungs”~Dr. Burns)
- Pulmonary surfactant is a phospholipid that reduces the surface tension of the alveoli
- What is surface tension?
- The contractive tendency of the surface of a liquid allows it to resist an external force
- Deficiency of surfactant causes increased surface tension, leading to increased work of breathing and alveolar collapse
- Surfactant is produced by alveolar cells within the lungs beginning ~24 weeks and continuing until term
- Intrauterine stress can induce surfactant production early, providing a protective effect against neonatal respiratory morbidity
- Within 72 hours of birth, infants begin producing their own surfactant regardless of gestational age
- Exogenous surfactant (via ETT) to replace surfactant deficiency
Relational Rewind
Consider: Which premature infant would be at greatest risk of experiencing NRDS and why?
A) 24-week preemie with a maternal history of hypertension;
B) 24-week preemie with a maternal history of drug use,
C) 24-week preemie with a maternal history of late prenatal care
D) A&B only
E) B&C only
Other RDS Causes
- Congenital heart defects
- Diaphragmatic hernia
- Absence or decreased pulmonary surfactant
- Pneumothorax
- Atelectasis
- Meconium aspiration
- Pneumonia
- Sepsis
Signs and Symptoms
- Retractions- sternal and subcostal
- Tachypnea- greater than 60 breaths/minute
- Cyanosis- check mucous membranes and skin
- Nasal flaring
- Hypoxemia
- Pallor
- Grunting (babies should never “talk” or make sounds with respirations)
- Acidosis
Nursing Interventions
- Decrease neonatal stress, including cold stress by maintaining a neutral thermal environment
- increased stress also increases O2 demand
- Neonatal care
- Respiratory support including oral and nasal suction
- Cardiac monitoring, O2 sats, ABGs
- Strict I&O
- over-hydration increases cardiac demand, pulmonary congestion, and O2 requirements
- Antibiotic therapy as ordered
Gastrointestinal (GI) and Genitourinary (GU)
A newborn’s ability to eat and digest food is essential for growth and development to occur. Most babies are able to absorb nutrients and have normal bowel movements after being fed. However, issues can occur during fetal development or occur after birth. Inability to void or stool can indicate potentially life-threatening complications related to the GI or GU tract.
Development Related Complications
If we consider the various stages of fetal development, the structure of organs occurs prior to a woman even being aware she is pregnant. Birth defects can occur naturally due to errors, can be genetically linked, a result of infection, or be an unintended consequence of external factors such as maternal medication, drug use, lack of prenatal care, or other lifestyle choices. Below is a list of the most common GI/GU birth disorders (pictures included) :
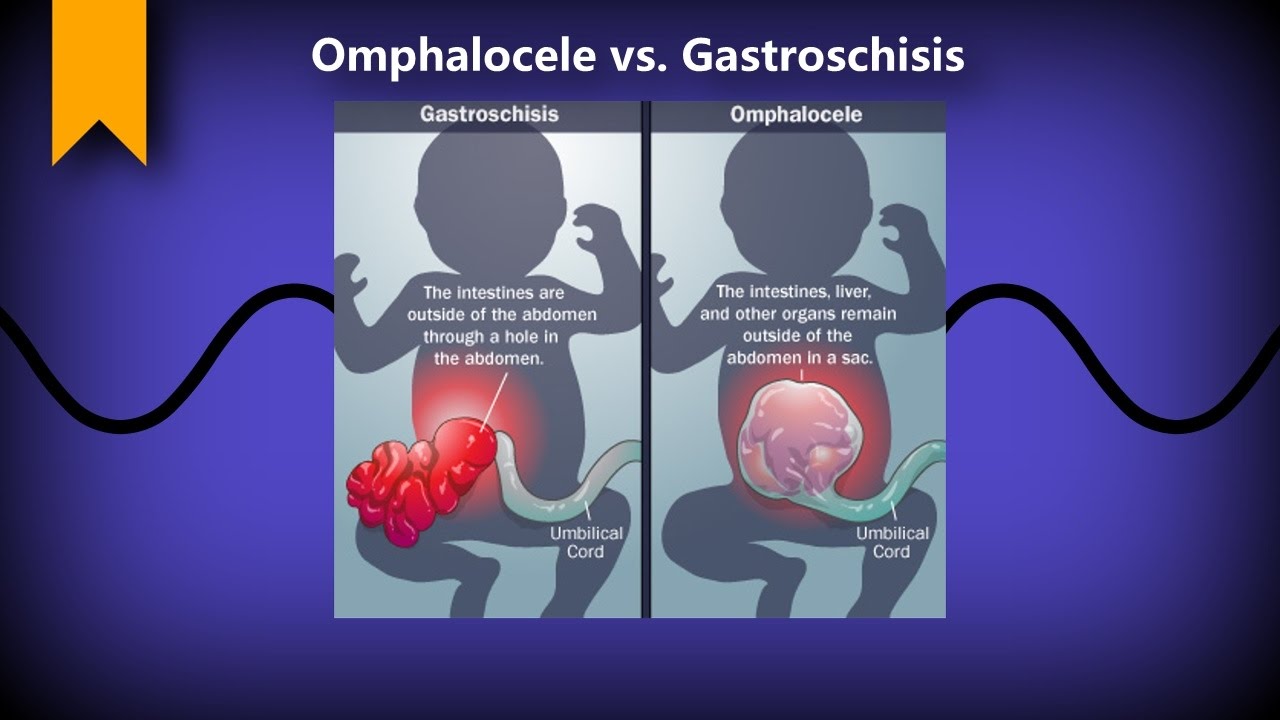
- Abdominal Wall Defect
- Omphalocele
- Gastroschisis
- Anal Atresia (Imperforate Anus)
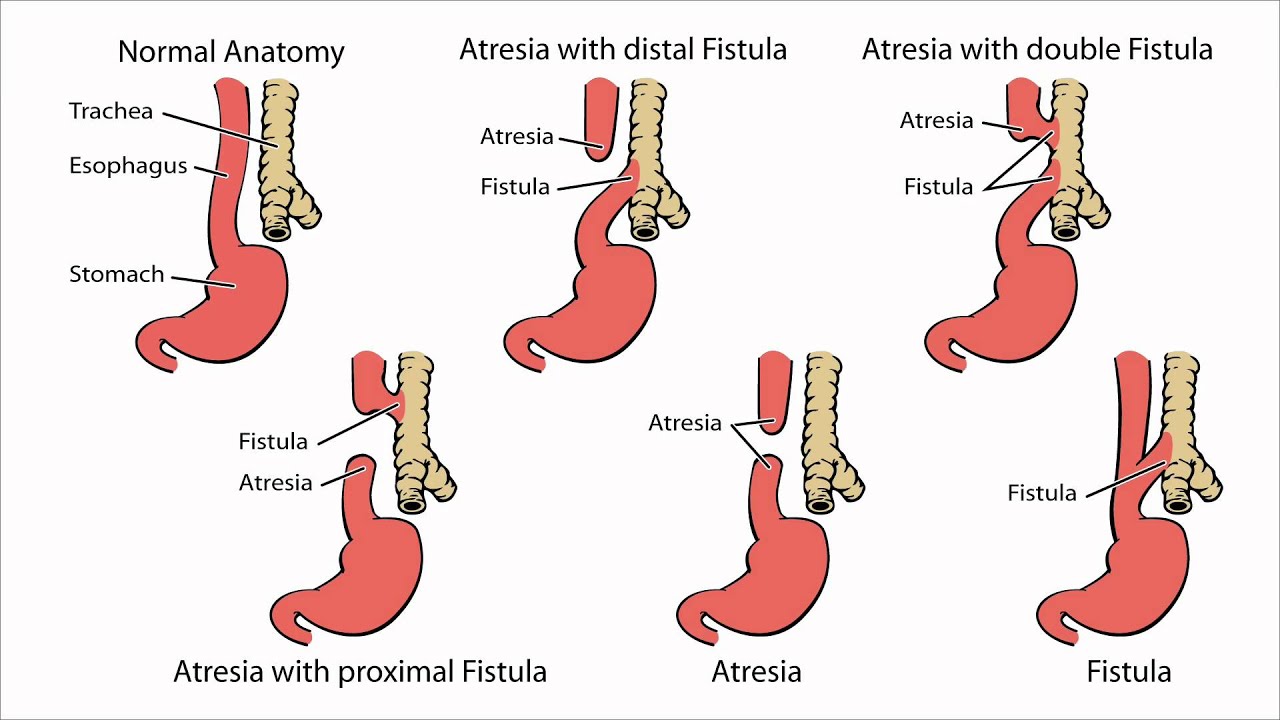
- Esophageal Atresia
- Hirschsprung disease
- Intestinal Malrotation
The digestive organs may be incompletely developed or abnormally positioned, causing blockages, or the muscles or nerves of the digestive tract may be defective. Symptoms depend on the location of the defect but may include crampy abdominal pain, abdominal swelling, and vomiting. The diagnosis usually is based on imaging tests and other tests and surgery is usually required. While nursing care varies among organizations, identification of a GI/GU problem through a keen awareness of symptoms and thorough assessment will determine the infant’s outcome. This is especially critical for infants requiring surgical intervention and treatment.
- Maintain hydration and temperature
- Provide D5W and/or albumin for hypovolemia
- Place infant in a sterile bag up to and covering the defect
- Initiate gastric decompression by insertion of a nasogastric tube to prevent distension of lower bowel and impairment of blood flow
- Position to prevent trauma to defect
- Prevent infection and trauma to defect
- Administer broad-spectrum antibiotics
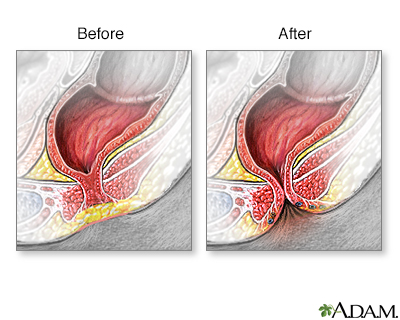
Anal Atresia (Anorectal Malformation)
- Absence of stool. There is no passage of stool within a day or two of birth.
- Passing of stools in other openings. The infant may pass stools through another opening like the urethra in boys or vagina in girls.
- Swollen belly. The newborn could not pass out stools, resulting in a swollen belly.
- Absence of anal opening. The opening of the anus is missing or not in its usual place; in girls, this may be near the vagina.

Non-Developmental Complications
Necrotizing Enterocolitis (NEC)
Necrotizing enterocolitis (NEC) is primarily a disease process of the gastrointestinal (GI) tract of premature neonates that results in inflammation and bacterial invasion of the bowel wall. Despite advances in the care of premature infants, NEC remains one of the leading causes of morbidity and mortality in this population. It occurs in 1-5% of all neonatal intensive care admissions and 5-10% of all very low birth weight (<1500 g) infants. Although research has presented an interesting array of potential contributing factors, the precise etiology of this multifactorial disease process remains unknown.
Believed to have risen predominantly from ischaemic injury to the immature GI tract, many factors are likely to be involved and diagnosis is reliant on clinical presentation Some plausible causes may be related to the introduction and advancement of enteric feeding, alterations in the normal bacterial colonization of the GI tract, bacterial translocation, and activation of the cytokine cascade, decreased epidermal growth factor, increased platelet-activating factor, and mucosal damage from free radical production. Clinical manifestations of NEC may be vague, including increased episodes of apnoea, desaturations, bradycardia, lethargy, and temperature instability. There may also be GI-specific symptoms such as feeding intolerance, emesis, bloody stools, abdominal distention, loops of bowel, tenderness, and abdominal wall discoloration. Your frequent and keen assessment of the infant is critical.
Medical treatment typically consists of bowel rest and decompression, antibacterial therapy, and management of other hematological or electrolyte imbalances. Increased respiratory and cardiovascular support is sometimes needed. In neonates who do not respond adequately to medical management, or if pneumoperitoneum is present, surgical intervention may occur. Time is of the essence in beginning antibiotics upon diagnosis for the best chance of recovery and survival.

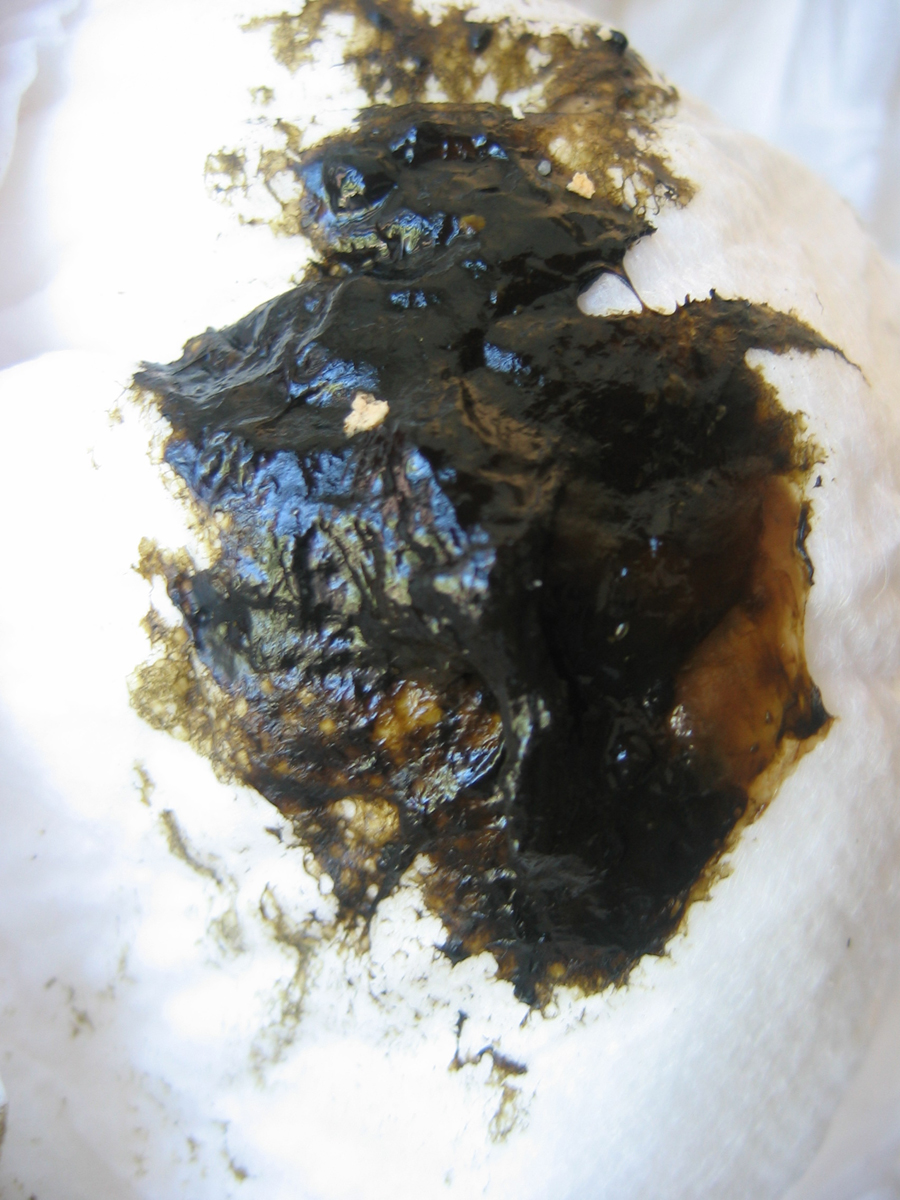
Meconium Aspiration Syndrome (MAS)
We have previously discussed the protective aspect of intrauterine stress in relation to respiratory distress, however, another outcome of such stress can be less protective and can be life-threatening. Meconium, or fetal feces, usually represents the first stool passed after birth. Unlike later feces, meconium is composed of materials ingested during the time the infant spends in the uterus: intestinal epithelial cells, lanugo, mucus, amniotic fluid, bile, and water. If under stress in utero, the fetas can pass meconium into the amniotic fluid. This is caused by the relaxation of the rectal sphincter due to fetal hypoxia in utero and can occur in breech and normal births w/o evidence of asphyxia. As a complication, a fetus can aspirate the meconium-stained amniotic fluid (MSAF) in utero and/or at the time of delivery resulting in obstruction of lower airways, reduced surfactant production, or pneumonia. Your actions as a nurse will include assisting with resuscitative measures, ongoing respiratory assessment, and respiratory support.
Neonatal Abstinence Syndrome (NAS)
Neonatal abstinence syndrome (also called NAS) is a group of conditions caused when a baby withdraws from certain drugs he’s exposed to in the womb before birth. NAS is most often caused when a woman takes opioids during her pregnancy. But it also can be caused by antidepressants (used to treat depression), barbiturates, or benzodiazepines (sleeping pills). When taken during pregnancy, they can pass through the placenta, which is responsible for supplying nutrients and oxygen through the umbilical cord, and cause serious problems for the baby.
Opioids include:
- Codeine
- Hydrocodone (name brand Vicodin®)
- Morphine (name brands Kadian®, Avinza®)
- Oxycodone (name brands OxyContin®, Percocet®)
- Tramadol
- The street drug heroin
Signs and Symptoms
Depending on the drug, most symptoms begin within the first 3 days after birth but can appear earlier. Some infants have experienced symptoms weeks after birth and can have lasting effects for up to 6 months. Symptoms include:
- Body shakes (tremors), seizures (convulsions), overactive reflexes (twitching), and tight muscle tone
- Fussiness, excessive crying, or having a high-pitched cry
- Poor feeding or sucking or slow weight gain
- Breathing problems, including tachypnea
- Fever, sweating, or blotchy skin
- Trouble sleeping and lots of yawning
- Diarrhea or throwing up
- Stuffy nose or sneezing
Nursing Care
Your nursing care for an infant experiencing withdraw includes obtaining a comprehensive prenatal medical and drug history, especially with respect to polydrug
abuse, monitor lab (Serum glucose, Serum calcium/magnesium, Urine test for toxicology, and Meconium drug analysis), Observe S/S with a NAS scoring sheet or Finnegan Neonatal Abstinence Scoring Tool (FNAST) and follow the Eat, Sleep, Console (ESC) algorithm.