7
Learning Objectives
- Understand the management of care to the postpartum woman with hemodynamic and circulatory dysfunction, pain, tissue injury, and infection.
- Discuss the care management related to the psychosocial needs of the postpartum client with a potential diagnosis of altered family processes, altered parenting, anxiety, the risk for situational low self-esteem, and grieving.
- Describe assessment for signs and symptoms of postpartum complications including postpartum depression.
OB Hemorrhage
After the delivery of the newborn blood loss is frequently underestimated. The definition of a postpartum hemorrhage is blood loss of >1000 ml after vaginal or cesarean birth. At term, 600-800 ml of blood per minute flows through the pregnant uterus with an average of 5,700 ml of blood in the average adult, up to 30% more in a pregnant client, it would take approximately seven minutes for the pregnant client to bleed out from a postpartum hemorrhage (PPH). Extreme care and intervention needs to be taken when the pregnant client is presenting with a risk for PPH. With every 3-4 percentage drop in hematocrit the assumption can be made that the client has had a 500 ml blood loss. In 2006 it was reported that the incidence of maternal deaths has nearly tripled from 6 per 100,000 in 1996 to 17 per 100,000 annual births. Nationwide, blood transfusions increased 92% during delivery hospitalizations between 1997 and 2005. Several risks are associated with a PPH and should be reviewed to ensure appropriate plans are in place when risks are presented. Some risks associated with a PPH include previous C-section or uterine surgery, multiple gestation, macrosomia (fetal weight of >4kg), high parity (>4 previous vaginal births), prolonged labor especially with oxytocin, history of PPH, placenta previa, low lying placenta, placenta accreta and know coagulopathy. These are some of the risks that can make the incidence higher however, many times a PPH occurs without any known risk factors.
There are a number of reasons that a PPH may occur and are related to the four T’s: Tone, Trauma, Tissue, and Thrombin.
| Cause | Incidence | |
| Tone | Atony | 70% |
| Trauma | Lacerations, hematoma, inversion, rupture | 20% |
| Tissue | Retained placenta, invasive placenta | 10% |
| Thromin | Coagulopathies | 1% |
Early hemorrhage occurs within the first 24 hours after birth and can be caused by uterine atony, lacerations, and hematomas. Uterine atony is defined by a lack of uterine muscle tone or contractions. Uterine atony causes 70% of all postpartum hemorrhage cases and causes can be associated with uterine distention from a large infant, multiple gestation or polyhyramnios, grandmultipartiy, prolonged labor, retained placental parts, oxytocin induction/augmentation, magnesium sulfate, and/or infection.
Lacerations will present with a bright red blood or steady stream of unclotted blood with a firm uterus. The bleeding can be cervical, perineal, or vaginal. Related risk factors for lacerations is a primigravida, precipitous delivery, macrosomic delivery, forceps/vacuum extraction, and/or episiotomy extension. The pregnant client after delivery may experience a hematoma which may be a collection of blood in the vulvar region or vagina due to injury to a blood vessel during spontaneous delivery. It can be caused from prolonged pressure by the fetal head on the vaginal mucosa, forceps/vacuum extraction or precipitous delivery. The symptoms are typically sever pain and pressure in the perineum and it may not always be visible. Careful inspection is needed with the client experiencing this kind of increased pressure after delivery.
Placenta accreta
A placenta accreta occurs when the placenta abnormally implants where it attaches to the myometrium and is inseparable from the uterine wall. Placental accreta is classified as the following:
- Accreta: slight penetration of the myometrium
- Increta: chorionic villi invade the myometrium
- percreta: invades through the myometrium and serosa and occasionally adjacent organs.
The greatest risk with the pregnant client presenting with an accreta is previous C-section. It can be diagnosed prenatally with an ultrasound. A C-section delivery with a hysterectomy is typically planned at 34 weeks at a tertiary care center that has appropriate personnel and a good blood supply. Primary complications are a maternal hemorrhage (AGOG, 2012).
Late Hemorrhage
Late hemorrhage is classified as more than 24-hours post delivery but less then 6-weeks after birth. Typically late hemorrhage is associated with subinvolution and the failure of the uterus to return to a normal size. This may be due to a retained placenta/membranes or an infection. Blood loss with a late hemorrhage may be excessive. If the lochia fails to progress from rubra to serosa to abla complications may be present. Rubra lasting more than two weeks is abnormal. Complications with a late hemorrhage after discharge may not be diagnosed until the postpartum visit at 6 weeks.
Nursing Care with Hemorrhage
The nurse caring for the postpartum client will want to regularly assess the client for signs and symptoms of bleeding. Palpating the fundus for firmness, height, and position is the first assessment that can help identify a PPH. The firmness, height, and position should be documented along with any interventions. In the event of a PPH the nurse will massage the fundus vigorously to help the uterus contract. The nurse will call for immediate assistance and notify the provider. The nurse will immediately assess the bladder for distention and if needed insertion of an indwelling catheter per providers orders. If these interventions do not work, the provider may implement bimanual compression and order uterine stimulants including oxytocin, methergine, hemabate, and cytotec. Additionally the PPH bundle may be implemented where the nurse will want to ensure secondary access with a large bore IV, preparation for blood products, oxygen and warm blankets as needed and begin to assess for signs and symptoms of shock.
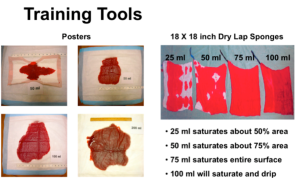
First line of care of the client post delivery is the active management of the third stage by administration of oxytocin 10U IM or 20U IV with the delivery of the infant and placenta. The provider will provide controlled cord traction and the cord clamping will not be delayed beyond two minutes. Once the placenta has been delivered vigorous fundal massage is performed for at least 15 seconds. Blood loss as mentioned earlier is usually underestimated and units have began moving toward measuring a quantified blood loss by weighing all the items where blood is present after delivery. As a visual aid the following picture shows what different amounts may look like visually to the nurse when assessing the client.
Pharmacological management of the client suffering from a PPH should be conducted emergently and if one medication does not work to get the uterus to contract effectively moving to the next can be done. Uterotonic agents utilized to control bleeding include oxytocin, methergine, cytotec, hemabate, and tranexamic acid (TXA). TXA is a fibrinolytic inhibitor, and has been added to the protocol if the uterotonic agents don’t work. Dose is 1 gram very slow IVP over 10 minutes. It may also be given diluted in 50-100 ml IV piggyback. A second dose 30 minutes after the initial dose can be given if bleeding persists. While cryoprecipitate (fibrinogen replacement) works better after administration of TXA, do not delay administration of blood products if needed.
Thromboembolic Disorders
The pregnant client is at higher risk of developing thromboembolic disorders, including superficial and deep vein thrombosis, and pulmonary embolism. Superficial thrombophlebitis often involves the saphenous vein and is a superficial clot with inflammation. It is most common in the third or forth day postpartum. The client will report tenderness of the vein with local heat, a palpable cord, and low grade fever. Deep vein thrombophlebitis (DVT) is more common in clients with a history of thrombosis. It is a formation of a clot in an area that impedes the blood flow in a deep vein and usually located in the lower extremity. It can occur as an obstetrical complication due to preeclampsia and C-section. The client will present with pain and edema in the lower leg and pain with calf pressure. The nurse will also note diminished peripheral pulses in the affected extremity. A pulmonary embolism occurs when a thrombus breaks loose and travels to the lungs, restricting air flow. This occurs most commonly in the postpartum period and will present with dyspnea and chest pain. This can lead to death in thirty minutes if not immediately addressed.
The pregnant client may also present with septic pelvic thrombophlebitis (SPT). SPT is a complication of the reproductive tract where an infection ascends along the venous system in the pelvis. The client may experience abdominal and flank pain with chills. It typically appears during the second to third day postpartum with a fever and tachycardia. The provider will order antibiotics for initial treatment and possibly anticoagulants like heparin. A CT scan will need to be performed for diagnostic measures.
Thromboembolic disorders occur due to Virchow’s triad. Virchow’s triad states that there is a triad of conditions physiologically that increases the risk and includes a hypercoagulable state, venous status, and injury to the epithelium of the vessel. Risk factors that impact the pregnant client include C-section, immobility, obesity, smoking, trauma to the extremities, varicosities of legs, increased maternal age, anemia, history of DVT, and increased amounts of blood clotting factors. To help prevent thromboembolic disorders the nurse can pad the leg rests and minimize the amount of time spent in them, promotion of early ambulation, encourage leg exercises if on bedrest, promote increased fluid intake, provide anti-embolism stockings (SCD’s) in labor and postpartum with the client with a history of varicosities, avoid sitting or standing for long periods, and elevate limbs when sitting but do not gatch bed or use pillow under the knees. The prevention of venous thromboembolism like DVT’s is a Joint Commission Core Measure and preventative measures can be introduced in the care provided by the nurse.
The nurse will assess each client for the signs and symptoms of thrombus by assessing the inguinal area, lower abdomen and legs for any redness, warmth, pain, swelling and/or edema, decreased peripheral pulses, and a palpable cord. If the client presents with thromboembolic disorders the nurse will want to elevate the affected leg, administer analgesics, antibiotics and anticoagulants as ordered. They may also provide warm, moist soaks as ordered. Both heparin and Coumadin are compatible with breastfeeding.
Infections
Any infection occurring in the reproductive system 28 days after delivery is considered a postpartal (puerperal) infection. These include endometrial infections, perineal, vulvar, or vaginal infections, wound and/or incisional infections, mastitis, and urinary tract infections. The postpartal client is at higher risk of infection if they had a C-section, prolonged rupture of membranes, multiple vaginal exams, poor health status such as obesity, anemia, diabetes or history of smoking, internal monitoring, episiotomies & lacerations, group beta strep, vaginal vaginosis, or chlamydia infections, soft tissue trauma/manipulation, retention of placental fragments, lapse in aseptic technique, and forceps/vacuum extraction. Cesarean delivery is the greatest risk factor of endometritis. Symptoms of endometritis include foul smelling lochia, uterine tenderness, fever, malaise, and tachycardia. Causative organisms include Group B strep, Chlamydia, E. Coli, and Staph aureus. The nurse will assess the client vital signs for signs and symptoms with an increased temperature, tachycardia, delayed involution, abnormal lochia, pain, tenderness or inflammation of the abdomen or perineum. Treatment will include antibiotics, adequate nutrition & hydration, rest, and hand hygiene.
Wound and incisional infections can occur at the site of a C-section incision, perineal lacerations and or episiotomies (rarely become infected). Symptoms are pain/tenderness at the site, redness, warmth, edematous, purulent drainage, fever and in severe cases possibly dehiscence. Local infections may also become systemic. Assess the area for redness, edema, ecchymosis, discharge and approximation (REEDA), and pain. Treatment will be the same with antibiotics, adequate nutrition & hydration, rest and hand hygiene.
Mastitis is an inflammation/infection of the breast connective tissues and usually occurs during lactation. It occurs in up to 20% of breastfeeding clients. The nurse will assess the breasts of the postpartum client for warm, reddened or painful area, axillary lymph node enlargement and flu like symptoms with an increased temperature. The causes of mastitis include milk stasis, plugged ducts, engorgement, fatigue and stress, cracked nipples, and inadequate hand washing. Causative organisms can include staph, E. Coli, Strep, and H. influenza. The nurse will promote adequate nutrition, hydration and rest. Encourage the patient to wear a supportive bra 24 hours per day and perform good hand washing before handline the breast. A culture and sensitivity may need to be collected of the breast milk to identify causative organisms in reoccurring cases.
Urinary tract infections usually occur from ascension of bacteria from the urethra to the bladder. Cystitis may progress to pyelonephritis is untreated. Risk factors for infection include retention of residual urine, decreased bladder sensitivity from stretching or trauma, and contamination of catheterization. The nurse will monitor the client for a temperature and symptoms of a UTI, promote rest and nutrition, teach good vulvar hygiene and encourage the client to increase oral fluids to 3-4 liters/day. Additionally, if ordered the nurse will administer antibiotics.
Psychological Disorders Impacting the Postpartum Period
The client may suffer from psychological disorders in the postpartal period such as postpartum depression and/or psychosis.
Postpartum depression is a major mood disorder and has an incidence rate of 10-15%. The onset is during pregnancy or within 4 weeks of childbirth. Risk factors for PPD include a history of depression or anxiety, lack of support, low socioeconomic status and complicated birth. Symptoms include sadness, frequent crying, insomnia, appetite change, feelings of worthlessness, obsessive thoughts of inadequacy, disregard to appearance, and irritability/hostility toward the newborn. Treatment for PPD may include pharmacological intervention with SSRI (Zoloft, Paxil, Prozac), individual or group therapy, and practical assistance with childcare. Postpartum psychosis presents itself in 0.1% to 0.2% of postpartum clients, it is evident within the first 2 weeks postpartum. Risk factors include previous PP psychosis, history of bipolar disorder, lack of support, and obsessive personality. Symptoms of psychosis include manic episodes, impulsivity, agitation, hyperactivity, insomnia, irrationality, difficulty remembering or making a decision, delusions and hallucinations. Treatment may include hospitalization, antipsychotic medication, ECT, social support, and removal of infant. The nurse caring for a client with either will want to assessment at prenatal and postnatal encounters, note history of previous psych problems, adequacy of coping skills, self-esteem, observe client with baby only and with family, listen for verbalizations indicating potential violence to self or baby, bizarre thoughts, and seek psych referral or social services as needed.
Perinatal Loss and Grief
The death of an embryo, fetus or infant anytime between conception and 28 days after birth, abortion (spontaneous or elective) conception through 20 weeks, intrauterine fetal death (IUFD) also called stillbirth or fetal demise after 20 weeks gestation, and neonatal death which occurs in the first 28 days of life. Common causes of perinatal loss include:
- Preeclampsia/eclampsia
- Diabetes
- Cholestasis of pregnancy
- Abruptio placentae
- Placenta previa
- Asphyxia
- Cord accidents
- Infection
- Congenital anomalies
- Isoimmunization (most common)
However, up to 60% of fetal deaths have no known cause. The first symptom is often decreased fetal movement, an ultrasound will visualize absence of cardiac activity and labor will be induced within a couple of days of diagnosis. Less than 28 weeks with misoprostol (Cytotec) vaginally and term pregnancies usually induced with oxytocin (Pitocin). Women with previous cesarean scars will usually have repeat cesareans if > 28 weeks. After birth, placenta and fetus will be sent to pathology. Often cultures will be taken from placenta. Blood may be drawn from baby for chromosomal analysis. If parents desire, an autopsy will be ordered (parents must bear this cost, which is around $2000). Grief is an individual response to a loss and can be influenced by age, gender, personality, culture and religion, family dynamics. Responses may include: •Physical (SOB, anorexia, fatigue), •Cognitive (denial, confusion, preoccupation), •Emotional (sadness, anger, guilt, bargaining)
