2
Learning Objectives
- Explain the 5 factors affecting the labor process.
- Identify the characteristics and behaviors associated with the stages and phases of labor.
- Examine the influence of culture on childbirth and discuss the nurse’s role in supporting women through this process.
- Identify non-pharmacological strategies to enhance relaxation and decrease labor discomforts.
- Compare the types of pharmacological pain relief used during labor and delivery.
- Discuss the rationale for common elective and operative intrapartum procedures.
Factors Impacting Labor
- Passenger
- Passageway
- Powers
- Position
- Psychological Response
“Labor and delivery are not passive processes in which uterine contractions push a rigid object through a fixed aperture. The ability of the fetus to successfully negotiate the pelvis during labor and delivery depends on the complex interactions of three variables: uterine activity, the fetus, and the maternal pelvis” (Kirkpatrick, Garrison, & Fairbrother, 2021).
Passenger (The Fetus) – Fetal Head, Fetal Presentation, Fetal Lie, Fetal Attitude, Fetal Position
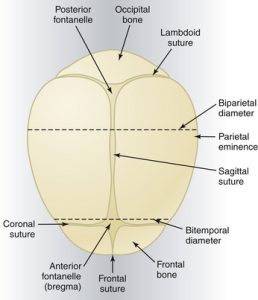
Fetal Head
The fetal head is the largest part of the baby. The biparietal diameter of a term 40 weeks gestation fetus is approximately 9.5 cm. The biparietal diameter measurement is the transverse distance between the the parietal bone protuberance. As seen in the in Figure 1 the fetal head is comprised of several unfused suture lines, and fontanels allowing the fetal head to “mold” as it passes through the birth canal. These suture lines and fontanels can be utilized for assess for the fetal position with in the pelvic inlet during labor.
Fetal Presentation
The fetal presentation is the part of the fetus entering the maternal pelvic inlet first. The possible presenting parts of the fetus are: vertex (occiput), breech (sacrum), shoulder (scapula), brow, face, or chin (mentum). A fetus descending into the pelvis and birth canal can be in a multitude of presentations and would be documented as such as the pregnant client is progressing. Vertex (occiput) is the optimal presentation for a vaginal delivery. Most other positions may cause cephalopelvic disproportion and cause labor to become irregular and lead to surgical intervention via cesarean section (C-section). With breech presentation, whether complete, footling, or frank, delivery typically occurs via C-section.
Fetal Lie
The fetal lie refers to the longitudinal lie of the fetus in comparison to the longitudinal axis of the uterus, in other words the relationship of the spinal column of the fetus to the spinal column of the pregnant client. The lie can be longitudinal with vertex or breech presentation, transverse with a shoulder presentation or oblique. The longitudinal position is optimal for vaginal delivery with singleton fetus (Kirkpatrick, Garrison, & Fairbrother, 2021).
Fetal Attitude
The fetal attitude refers to the position of the fetuses head in respect to the fetal spine. A normal attitude is one of general flexion, where the chin of the fetus is flexed into to the fetal chest. This fetal attitude is optimal for delivery since the fetal head is presenting within the pelvic inlet at the smallest possible diameter (9.5cm). As the head deflexs or changes in flexing or extending of the neck/body concerns arise regarding complications with brow or mentum presentations and “failure to progress” due to malpresentation of the fetal head.
Fetal Position
The fetal position is the relationship of the landmark on the presenting part to the anterior, posterior, or sides of the maternal pelvis. Three notations are used to describe the fetal position and are used to help with maternal positioning during labor. Right (R) or left (L) side of the maternal pelvis, landmarks include occiput for vertex presentation (O), scrum for breech presentations (S), scapula for shoulder presentation (Sc), and mentum for face presentations (M). Additionally the position of the fetal head is also described by which direction the occiput (in a vertex presentation) is in respect to the maternal pelvis. For example, a fetus is vertex (head down) position with the occiput (back of the head) towards the left front of the maternal pelvis, which would be documented as LOA (left occiput anterior), which is the most common position. When the fetus is occiput posterior, which means the fetal occiput is against the pregnant clients posterior, the client may experience a lot of back pain during labor.
The fetal position is also dependent on the fetal station in relation to the pelvic outlet. A fetal station is where the top of the fetal head is in relation to the imaginary line between the ischial spines of the maternal pelvis. The pelvic inlet is the upper border of the true pelvis and is determined by three anteroposterior diameters: diagonal conjugate, obstetric conjugate, and conjugate vera. When the fetus is engaged, the largest diameter of the presenting part (biparietal diameter) passes through the pelvic inlet the fetal head will be at 0 station. In reverse if it is approximately -1 cm from the pelvic inlet the station would be -1 and so forth, if it is +1 cm below the pelvic inlet it would station +1 and forward to +5 or crowning.
Passageway
Bony Pelvis refers to the size and shape of the pelvis. There are four pelvic shapes gynecoid, anthropoid, android & platypelloid. The size and shape of the pelvis can influence labor by hindering the progression and creating obstetrical complications.
- Favorable pelvis for vaginal birth:
- Gynecoid (50%): rounded, wide with a deep sacral curve, wide and round pubic arch, all inlet and outlet diameters are adequate.
- Antropoind (24%): oval, long anteroposterior diameter, adequate but short transverse diameter, inlet and outlet adequate. Favors occiput posterior fetal position.
- Unfavorable for vaginal birth:
- Android (23%): heart shape, male-type pelvis, anteroposterior and transverse diameters are adequate, but other measurements make both the inlet and outlet inadequate. Favors occiput posterior.
- Platypelloid (3%): flat, transverse oval shaped, short anteroposterior diameter, wide pubic arch, both inlet and outlet are inadequate.
Soft Tissue refers to the cervix, lower uterine segment, vagina and perineum. To adequately progress the lower uterine segment must thin, the cervix dilate & efface, and the vagina & perineum must distend.
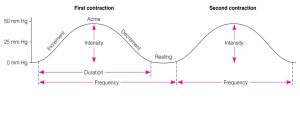
The Power
“The powers refer to the forces generated by the uterine musculature. Uterine activity is characterized by the frequency, amplitude (intensity), and duration of contractions” (Kirkpatrick, Garrison, & Fairbrother, 2021). Monitoring and assessing for uterine contractions can be conducted with palpation, electronic monitoring using an external tocodynamometer, or internal pressure catheter. External palpation and tocodynamometer of the uterus is appropriate to assess uterine contractions by monitoring and measuring the external wall of the uterus. Both are qualitative and only “show” a contraction occurring not the strength of the uterine contraction. To assess uterine activity the provider assesses for the frequency, duration, and intensity of the contraction. As discussed by Kirkpatrick, Garrison, & Fairbrother the definition of adequate uterine activity remains unclear, typically contractions that appear adequate, if using an external monitor, with 3-5 contractions within a 10 minute period of time. In active labor this will correlate with a uterine contraction approximately every 2-3 minutes and depending on the duration and intensity cervical change will occur. More then 5 contractions in a 10 minute period is classified as tachysytole and should be documented. Tachysytole can lead to uterine rupture and fetal compromise and fetal hypoxia, documentation that an absence of fetal stress, noted by absence of decelerations, is recommended. Intrauterine pressure catheters (IUPC) are used with caution due to the risk associated with placement. The pregnant client becomes at higher risk of infection. With placement hemorrhage can occur if misplaced causing placental disruption and/or uterine perforation. The use of an IUPC occurs to gain more adequate, quantitative, measurement of uterine contractions. Since the IUPC is a direct measurement of pressure within the uterus with contractions a more adequate picture of contractions can be gathered. The Montevideo unit (MVU) “a measure of average frequency and amplitude above basal tone (the average strength of contractions in millimeters of mercury multiplied by the number of contractions per 10 minutes)” (Kirkpatrick, Garrison, & Fairbrother, 2021). Adequate measurement is between 150-350 MVU for adequate labor.
If uterine contractions are adequate, labor should progress appropriately as exhibited by cervical dilation and effacement. In some instances this does not occur and could be related with cephalopelvic disproportion (CPD). Many instances can cause CPD some of the following could be instances as to why labor is not progressing, the size of the fetus (macrosomia), pelvic shape, or fetal position.
Cardinal Movements
Cardinal movements are described as the movement of the fetal head as it descends through the pelvic canal. There are seven cardinal movements, (1) engagement, (2) descent, (3) flexion, (4) internal rotation, (5) extension, (6) external rotation or restitution, and (7) expulsion (Kirkpatrick, Garrison, & Fairbrother).
Signs of Labor
Prior to labor starting there can be some preceding signs that occur. They include Braxton-hick contractions, lightening (engagement), weight loss (1-3.5 pounds), sudden burst of energy, rupture of membranes (ROM), loss of mucus plug, and backache.
False labor (practice labor) may occur prior to true labor and consists of contractions that might be regular, but they do not change in frequency, duration, or intensity and no cervical change occurs. False labor can be frustrating and exhausting for the pregnant client, during this time the client may need support, comfort measures and education from the nurse. True labor is defined by an increase in frequency, duration and intensity of regular uterine contractions. The uterine contractions do not go away with a change in activity. The contractions are usually felt low in the abdomen and wrap around toward the back. There is a change in the cervix with dilation and effacement. This cervical change is the hallmark of true labor and they usually occur together. Cervical dilation is the widening of the cervical os and cervical canal. As the uterus contracts the musculature composition of the uterus pulls the cervix up and around the fetal presenting part. The contractions, pressure from the presenting part and the release of hormones (relaxin, oxytocin, & prostoglandins) help with cervical changes. The effacement or thinning of the cervical wall, which is typically 2cm in length, is the drawing up of the internal os and the cervical canal into the uterine wall sides. Examination of the cervix is conducted digitally and is a sterile examination by the nurse or healthcare provider. This digital exam is somewhat subjective in nature due to the structure and composure of the examiners hand, generally 1cm is equal to the index finger and 2 index fingers is equal to 3cm.
There are four stages of labor classified numerically 1-4. The first stage is compromised of three phases, latent phase, active phase, & transition, and begins when contractions begin up to 10 cm dilation. The second stage begins with complete dilation until birth, the third stage is the birth of the placenta, and the fourth is from when the placenta is delivered until 1-4 hours. During the fourth stage the uterus continues to contract to control bleeding at the placental side of attachment along the uterine wall.
As the nurse it is important to assess the pregnant client and offer support during the three phases of the first stage of labor. Certain characteristics, maternal behaviors, and knowledge of the anticipated length of each phase can assist in the delivery of care and are described further below:
- Latent phase
- Characteristics: Beginning of cervical dilatation and effacement, no evident fetal descent, uterine contractions increase in frequency
- Contractions : irregular, Q 3-30 minutes, duration 20-40 seconds, mild intensity
- Maternal behaviors: able to cope, happy that labor has started, energetic, nesting
- Typically lasts: 8.6 hours in nulliparas, 5.3 hours in multiparas
- Nursing support: encourage patient to stay at home (where she can move freely, eat, drink, and rest) until contractions become more frequent and intense
- Active Phase
- Characteristics: dilatation from 6 to 8 cms; fetal descent (1.2-1.5 cm/hr)
- Contractions: Q 2-5 minutes, lasting 40-60 seconds, moderate intensity, firm to palpation
- Maternal behaviors: anxiety, decreased ability to cope, time to go to the hospital
- Typically lasts: 4.6 hours in nulliparas, 2.4 hours in multiparas
- Nursing support: encourage mobility, hydration, urination, relaxation—these are the things that promote labor progress
- Transition phase
- Characteristics: dilatation from 8 to 10 cms, progressive fetal descent increases 1-2cm/hr
- Contractions Q 1.5-2 min, lasting 60-90 seconds, strong intensity
- Maternal behaviors: withdraws, terrified of being alone, but does not want to be touched or talked to—BUT DON’T LEAVE HER!, may lose focus, or beg for drugs, may have urge to push but should control through panting/blowing—important NOT to push against an incompletely dilated cervix—can lead to cervical tears and hemorrhage!
- Typically, transition is not longer than 3 hours in nulliparas, 1 hour in multiparas
- Nursing support: help mother stay focused; LOTS of encouragement here—she will soon be ready to push!
During the second stage of labor pushing begins leading to delivery of the newborn. The second stage may present differently from the nulliparas (first pregnancy) client to the multiparas (previous pregnancies). For the nulliparas client the second stage may take up to three hours, in contrast to the multiparas client where it can be much shorter 0-30 minutes. Contractions are typically 1.5-2 minutes apart and last 60-90 seconds and are much stronger in intensity. The pregnant client in latent phase or laboring down and active phases (pushing) of the second stage should not start pushing until the cervix is completely dilated and the baby’s head is as low as +1 station. The sensation and urge to push as the fetal head presses on the pelvic floor comes from the activation of the Ferguson’s reflex. In most instances pushing down feels good and the pregnant client may express a sense of control since starting labor. They may have a burning sensation in the perineum as the tissue stretches that is often referred to as the ring of fire. During pushing the client often uses closed-glottis pushing, which can trigger the Valsalva maneuver. This can increase intrathoracic pressure and cardiovascular pressure which in turn reduces cardiac output and placental perfusion. The client may experience a light headed feeling and it could cause fetal hypoxia. Close management to ensure breathing between contractions is important to minimize these effects. During this phase of labor it is significant that the nurse continue to closely monitor fetal heartrate, maternal blood pressure, & heartrate every 5-15 minutes. Assistance with positioning can help ease discomfort and delivery and it is important for the nurse to help coordinate the pushing efforts, comfort measures and encouragement through positive reinforcement.
The third stage of labor is delivery of the placenta and products of conception, including the amniotic sac. Delivery of the placenta usually occurs within 5-30 minutes after the delivery of the infant. Prior to delivery of the placenta the provider may notice a gush or trickle of blood, lengthening of the umbilical cord, and a rise of the fundus in the abdomen. The client may bear down slightly to help with the delivery while they continue to bond with the newborn and experience skin to skin contact. The nurse is responsible at this time to help assist the provider to ensure the fundus is contracting adequately to minimize post-partum bleeding by administering IV oxytocin per the providers order and delivering vigorous fundal massage as soon as the placenta is delivered. Both aid in uterine contraction to help prevent and minimize bleeding.
During the fourth stage, 1-4 hours after birth, of labor the mother may experience shaking “postpartum chill”, which can be supported with blankets and reassurance. This is a physiologic readjustment phase for the client and the cause is unknown for the “chill”. The bladder is often hypotonic and the uterus should remain contracted (midway between the symphysis pubis and the umbilicus). The client may have a number of behaviors and feelings after the birth of the infant including relief, exhaustion, excitement, hunger and thirst. The nurse can support the client by providing snack and drink along with assessment of VS, perineum, and fundus every 15 minutes. They can also encourage breastfeeding and bonding during what is considered the “Golden Hour”.