4
Learning Objectives
- Describe the changes in the neonate during the transition to extrauterine life.
- Describe neonatal resuscitation and care immediately following delivery.
- Discuss the gestational age assessment and physical assessment of the newborn.
- Examine the common assessment tools used for screening the newborn.
- Discuss the nursing process as it relates to ongoing care of the newborn.
- Synthesize cultural variations that impact the teaching an learning of newborn care.
For forty weeks the fetus has been weightless, entirely dependent and comfortable in a dark, sound dampened, fluid filled environment. With birth, the newborn moves into a noisy environment where tactile, auditory, visual, and painful stimuli are plentiful and in which it must immediately function independently. The transition to extrauterine life requires the newborn to adapt for a successful transition to extrauterine life. Respiratory, cardiovascular, hematologic, hepatic, thermogenic, gastrointestinal, urinary, behavioral and neurological adaptations occur almost instantaneously and continue to develop over the course of the newborns first year.
Respiratory
The first breath of life is a gasp in response to mechanical, chemical, thermal and tactile events. These events initiate the opening of the alveoli to air and begin the transition from a fluid filled environment to an air-breathing, independent life outside of the uterus. Surfactant contains phospholipids which are critical for alveolar expansion and stability. This begins around 24 weeks gestation and peaks about 35 weeks gestation.
Mechanical
During the last half of gestation, the fetal lungs continuously produce fluid. Fluid expands the lungs almost completely. During labor there is a fetal gasp and active exhalation initiates the removal of fluid from the lungs. During a vaginal birthing process, the fetal chest is compressed, squeezing fluid out of the lungs. At delivery there is a passive inspiration of air that replaces the fluid that is squeezed out. After the first inspiration, the newborn will exhale and cry. The nurse takes into consideration this important mechanical process in helping the newborn expel fluids from the lungs and continuously assesses the newborn during cesarean birth.
Chemical
When the umbilical cord is cut and placental gas exchange ceases, a transitory asphyxia occurs. With the increase of carbon dioxide and decrease in oxygen a hypoxic state initiates impulses that stimulate the aortic and carotid chemoreceptors. This in turn triggers the respiratory center in the medulla and the fetal circulation begins to shift suppling oxygen to the lungs.
Thermal
When the newborn is delivered there is a sudden decrease in ambient temperature that results in chilling of the newborn. The nerve endings of the skin transmit impulses to the respiratory center in the medulla and this results in rhythmic respirations.
Sensory
When the fetus is delivered, it moves from a state of sensory deprivation to a state of sensory overload. The newborn will experience numerous visual, auditory and tactile stimuli. Joint movement appears to stimulation the respiratory center to sustain respirations.
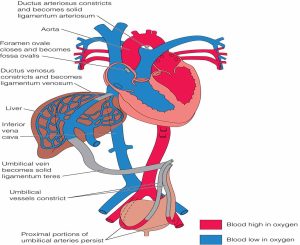
In summary the respiratory adaptations include multiple factors to influence the newborns ability to breath. The fluid in the alveoli must be absorbed into the lung tissue and replaced by air. The umbilical arteries and vein constrict when they are clamped, increasing systemic blood pressure. The blood vessels in the lung tissue relax in response to gaseous distention and increased oxygen. This decreased resistance along with the increased systemic blood pressure results in a dramatic increase in the pulmonary blood flow. Leading to circulatory adaptations to ensure blood flow is appropriate. Beginning with the decreasing flow of through the ductus arteriosus.
Cardiovascular Adaptations
In utero, the special circulatory system involving the placenta bypasses most of the blood supply to the fetal lungs. With delivery and loss of placental circulation, there are marked changes in this circulatory pattern including an increase of pressure in left heart decreasing resistance. In addition, changes to the cardiovascular system include the closure of the foraman ovale (within minutes), ductus arteriosus, and ductus venosus (Mattson & Smith, 2016).
Hematological adaptations occur with a rise initially the first few days but declines during the first two months after birth causing physiologic anemia of the newborn. A decline is due to a decline due to a reduction in red cell survival and decreased production. The normal newborn with good nutritional status can tolerate these adaptations.
Hepatic Adaptations
In an adult, the conjugation of bilirubin takes place in the liver and changes it to an excretable form from a lipid soluble pigment to a water-soluble pigment, which then passes through the bile and the bile into the intestines where it is excreted. In the fetus, the unconjugated bilirubin is excreted via the placenta, so the fetus doesn’t need to conjugate bilirubin. The newborn’s liver must start to conjugate bilirubin but has less ability to do so in the first few weeks of life. This increases susceptibility to newborn jaundice (physiologic jaundice). Physiologic jaundice is a normal biological response to the newborn caused by accelerated destruction of fetal red blood cells, impaired conjugation of bilirubin, and increased bilirubin reabsorption from the GI tract. The yellow skin color results from increased levels of unconjugated bilirubin. At birth, the newborn’s total serum bilirubin level is usually < 3 mg/dl. Levels reach 4-6 mg/dl before coloration of the skin and sclera appears. The signs of physiologic jaundice appear after the first 24 hours. This differentiates physiologic jaundice from pathologic jaundice which is usually seen first in the face and progresses down the trunk.
In the adult, several coagulation factors are synthesized in the liver. This synthesis requires the influence of vitamin K, the newborn gut initially has no normal intestinal flora. The bacteria are necessary to synthesize vitamin K. The absence of vitamin K causes a transient coagulation alteration between the second and fifth day of life.
Thermal Adaptations
The full term newborn loses four times as much heat as an adult. More susceptible to hypothermia and cold stress due to less subcutaneous fat, blood vessels closer to the skin than in the adult, and larger surface area to body mass ratio. After initial drying, most of the heat loss is via convection and radiation. Convection loss of heat from the newborn’s skin to the surrounding air. The newborn will lose a lot of heat by convection when exposed to cold air or drafts. Loss of heat through conduction can occur when a newborn lies on a cold surface. Newborns lose heat by conduction when placed naked on a cold table, weighing scale or are wrapped in a cold blanket or towel. Heat loss can occur through evaporation from the newborn’s wet skin to the surrounding air. The newborn can easily lose heat by evaporation after the deliver, after a bath, or from a wet diaper. Last heat loss can also occur through radiation from the newborn’s skin to distant cold objects, such as a cold window. Keeping the newborn dry and warm is a priority for the nurse caring for the mother and newborn. This can be accomplished by drying the newborn immediately after birth and placing them on the mother’s chest for skin to skin contact, covering them with a warm blanket. Additionally, after skin to skin swaddling and keeping their heads covered will reduce heat loss. The flexed posture of the newborn helps decrease the surface area exposed to the environment, thereby reducing heat loss.
Newborns are homeothermic and will attempt to stabilize their core temperature. Newborns have moved from a moist, warm environment to a colder drier environment. This exposure triggers an increase in the metabolic rate of the newborn and heat production. The newborn responds to colder temperatures with a non-shivering thermogenesis. Skin receptors note the decrease in environmental temperature and stimulate the central nervous system to use the stores of brown adipose tissue (brown fat) to provide heat. Brown fat is deposited in the midscapular area, around the neck, and in the axilla’s and kidney areas. It gets its name from its brown color cause by blood supply. Brown fat increases the speed of heat production and oxygen consumption. A normal newborn can usually tolerate this, but complications can arise with newborns that are smaller in gestational age or left without intervention for too long.
Gastrointestinal System
Bowel sounds are present within the first 30-60 minutes, the newborn can successfully, fed during this time. The stomach capacity is 5-7 ml. Since the cardiac sphincter is immature some regurgitation may be noted during the neonatal period. To gain weight , the newborn requires 120 kcal/kg/day. Following birth, caloric intake is often insufficient for weight gain until the newborn is 5-10 days old. During this time, there may be a 5-10% weight loss in term newborns. Between days 1-3 of birth the newborns stomach is approximately the size a cherry and can hold 5-7 ml or 1-1.4 teaspoons at one time, after day 3 up to one week the newborn stomach is about the size of a walnut and can hold 22-27 ml or 0.75-1 oz, after one week it is approximately the size of an apricot and can hold 45-60 ml or 1.5- oz., and after one month the stomach is the size of a large egg and can hold 80-150 ml or 2.5-5 oz. These measurements are helpful in educating a new mother when feeding the newborn. The term newborn usually passes meconium within the first 24 hours after birth. Meconium is formed in utero and contains amniotic fluid, intestinal secretions and shed mucosal cells. Meconium is a thick, black or dark green and tarry in consistence. Transitional stools consist of part meconium and part fecal material and are passed after 24 hours, once the first meconium has passed. Transitional stool may occur up to two days after delivery. A breastfed infant may have stool that is a pale yellow and more liquid than those of formula fed newborns. The frequency of bowel movements varies but ranges from one every 2-3 days to as may as 10 daily.
Urinary Adaptations
Up to 93% of newborns will void within the first 24 hours and 100% by 48 hours. If the newborn has not voided within 36 hours the provider should be notified and an assessment conducted. Uric acid is a byproduct of the breakdown of purine metabolism and may appear with brick dust color with urination. It is excreted in the newborn as a result of reduced glomerular filtration rate and low intake of fluids, which is very common with breastfed babies for the first couple days of life. Newborns born with female genitalia may present with pseudomenstruation which will be apparent on the diaper and is a let down from the maternal hormones.
Behavioral Adaptations
The normal term newborn assumes a flexed posture and can be hypertonic in symmetry. Diminished tone or flaccidity indicates a problem and should be further assessed and documented. The first period of newborn reactivity is birth to 30 minutes after birth. This period is optimal for bonding and breastfeeding. Next phase is the sleep or inactive phase and is typically after the first 30 minutes. This phase can last as long as four hours. The second period of reactivity lasts four to six hours and during this time the newborn is awake and alert.
Neurologic Adaptations
Newborns can self-quiet using their own resources for comfort and can be exhibited with hand to mouth movements, sucking on the fist or thumb. The newborn has multiple reflexes that are characteristic of an immature central nervous system and include tonic neck (fencing pose), grasping, moro, rooting , and sucking.
Physical Characteristics of the Normal Newborn
Head
The newborn head is large in proportion to the body with an average circumference of 32-37 cms. The head circumference is 2 cm larger than the chest. The head may appear asymmetric because of the overriding of the cranial bones during labor and birth. If not evident visually, upon palpation a ridge can be noted. Ridges develop when one bone slightly overlaps the adjacent one during delivery. The degree of molding is determined by the length of time pressure is exerted on the head. Two fontanelles (soft spots) may be palpated on the newborn’s head both anteriorly and posterior. Fontanelles are the openings at the juncture of the cranial bones. The anterior fontanelle has a diamond shape and is a bit larger. The posterior fontanelle is triangular n shape. Molding can impact the initial size of the fontanelles. When assessing the newborn the nurse will palpate the newborn’s head and feel for both fontanelles. During this assessment the nurse may also notice a caput succedaneum which may be present due to prolonged period of time on the perineum and vacuum delivery. This is a localized swelling of the scalp that crosses suture lines. When the nurse assesses an indentation may occur by pressing on the swollen caput. During prolonged and difficult labor the newborn may also present with a cephalohematoma which is a collection of blood resulting from ruptured blood vessels between the surface of the cranial bone (usually parietal) and periosteal membrane. It does not cross suture lines and may take up to three months to restore to he normal shape. All findings should be documented during the newborn assessment and routine assessments conducted to ensure improvement or deviation from normal.
Eyes
The newborns eyes can fixate on near objects and follow stimuli. They can perceive faces, shapes and colors with a preference to the human face and eyes. The newborn will blink in response to bright lights. With crying they will be tearless. A sub-conjunctival hemorrhage can occur in 10% of newborns.
Nose
The nose of the newborn is small and narrow. Newborns and infants are nose dependent breathers for the first few months of life. Obstructions may be cleared by sneezing. The newborn can differentiate the smell of their own mother within the first week of life. Skin to skin contact and bonding with the mother help with this sense of smell and attachment.
Ears
The ears are soft and pliable upon inspection. They should recoil when folded and released by the nurse assessing the newborn. The top of the ear (pinna) should be parallel to the outer and inner canthus of the eye. Low set ears that are not parallel can be indicative of chromosomal abnormalities which should be reported and assessed further by a provider. The ear and the kidneys are developing during the same period gestationally. This development if impacting one, may have an impact on the other.
Mouth
The newborns mouth should present with pink lips and mucosal membranes. Discoloration such as bluish color can indicate fetal hypoxia and interventions should immediately follow. Touching the lips of the newborn can stimulate the sucking or rooting reflexes. Taste buds are developed and the newborn can discriminate between sweet and bitter flavors. Some variations may be present upon assessment including Epstein's pearls, thrush, or congenital defects like a cleft lip or palate. All these findings will be documented and assessed for any changes or need for further intervention.
Neck
The neck of the newborn is short with skin folds. There should be no webbing of the neck present. The nurse will assess the clavicles. During traumatic deliveries the newborns clavicle could be fractured which can be noted with an asymmetrical appearance of the shoulders.
Chest
The newborns chest should be cylindrical and symmetrical with an average diameter of 32 cms. Some newborns may present with engorged breasts with the possibility to present with both engorged breasts and a whitish secretion. Supernumerary nipples may be occasionally noted and a protruding xyphoid process which is normal. Respirations of the newborn are between 30-60 breaths per minute. The cry should be lusty and vigorous. The heart rate for the newborn should be 110-160 bpm, innocuous murmurs may be present with transition for fetal to neonatal circulation. Most often these may involve the incomplete closure of the ductus arteriosus or foramen ovale.
Extremities
The normal term newborn has a flexed posture, with fists tightly clenched. Their extremities are short, flexible, and move symmetrically. There should be no extra digits on the hands or feet and the nails extend beyond the fingertips in term newborns. The legs are equal in length with symmetrical skin folds. Asymmetrical skin folds are indicative of hip dysplasia. Some variations that may occur include polydactyly, syndactyly, polysyndactyly, brachial palsy, and club foot. Whenever digits are missing, amniotic bands could be the cause, but should also investigate chromosomal abnormalities.
Abdomen
The abdomen should be cylindrical and soft with no gross distention or bulging. Bowel sounds can be assessed by one hour after delivery. The umbilical cord will initially be white with a gelatinous (Wharton’s jelly) appearance with two arteries and one vein.
Genitals
Female
The appearance of the female genitalia of a newborn is dependent upon the gestational age. The labia majora typically covers the labia minora in a term newborn. Pseudomenstration may also be present as a whitish discharge that is occasionally blood tinged as a result of the withdrawal of maternal hormones.
Male
The appearance of the male genitalia is typically present with the testes descended and pendulous scrotum, also depending on gestational age. The testes and scrotum are assessed for descent. Variations may occur in the with the location of the opening of the urethra which is typically at the end of the penis. In some rare cases a congenital defect can occur called epispadias . Hypospadias, also a congential defect, can also occur. A hydrocele may also be present where fluid fills the sack of the scrotum.
Additionally, in some rare instances the newborn may be born with ambiguous genitalia.
Skin
The newborn may present with variations to the skin tone and appearance. Some of the variations would be noted upon assessment and are all normal findings. Acrocyanosis is a bluish discoloration of the hands and feet and can be caused by poor circulation. It is common at birth and is not concerning unless it persists. It is very common in areas of high elevation due to the decreased amount of oxygen concentration. The newborn is protected in utero by vernix. It is a white cheese like substance made up of sebum and desquamated epithelial cells that are on the fetal skin. It appears by 24 weeks gestation and typically disappears by term. Since this acts as a protective barrier on the newborns skin and aids in bonding with the mother some institutions are delaying bathing. On the term newborn it is typically found within the creases and folds of the newborns skin around the neck and legs. Mongolian spots are macular areas of bluish black or gray-blue pigmentation found on the dorsal area of the buttocks of the newborn. They are more common in dark-skinned newborns, but are also seen in 1-9% of Caucasians. They may appear as bruises so they should be appropriately documented in the charting. Erythema toxicum is also referred to as a newborn rash. It presents with innocuous pink, papular rash of unknown origin with superimposed pustules it appears within 24-48 hours after birth and resolves spontaneously within a few days. Milia are tiny white papules appearing on the face of a newborn as a result of unopened sebaceous glands they disappear spontaneously within a few weeks.
Care of the Newborn
Initial care of the newborn takes place immediately upon delivery by clearing out the airway with a bulb syringe. To suction the airway the mouth is suctioned first followed by the nose as soon as the shoulders are delivered. The nurse will be prepared to immediately dry and stimulate the newborn if the newborn is stable it can be placed on the mother’s chest and abdomen. This skin to skin contact helps provide comfort, warmth and stabilizes the heart & respiratory rates. Vital signs, respiratory and cardiac status, and Apgar’s are all conducted within the first minute. A follow up Apgar is assessed at 5 minutes after birth. If the newborn is not stable they will be taken to the radiate warmer located at the bedside and neonatal resuscitation efforts will be followed.
Ongoing Care of the Newborn
The nurse caring for the newborn should ensure they are maintaining a clear airway and a neutral thermal environment. Assessing the newborn is important multiple times during the shift. The nurse will assess the respiratory system and heart rate. Signs of respiratory distress can present with nasal flaring, intercostal or xiphoid retractions, expiratory grunting or sighing, and tachypnea. The newborn can also present with these signs when attempting to stabilize their temperature. The newborn requires a higher environmental temperature than an adult. An unclothed newborn needs an environmental temperature of 89.6 to 93.2 degrees Fahrenheit. Care of the newborn should take place under the radiant warmer if the newborn needs to be unclothed. After the newborn’s temperature has stabilized, the infant can be placed clothed in an open crib for transport to the mother. Additionally, placing a cap and shirt on the newborn and swaddling can help prevent heat loss as well as provide comfort.
When the newborn is delivered and stabilized a number of medications are administered per provider orders and with parental consent. To help prevent bleeding an injection of vitamin K is given prophylactically. It is given via intramuscular injection in the vastus lateralis (middle third) with a 25-gauge, 5/8″ needle. To prevent infection of the eye prophylactic eye treatment is conducted with the instillation of erythromycin ointment in the lower conjunctival sac of each eye. This treatment is conducted to treat Neisseria gonorrhoeae and Chlamydia trachomatis. In some states this is required by law and could be considered a Class B misdemeanor. Other medications that may be given for the prevention of infection is the Hepatitis B vaccine. It is also given via IM in the vastus lateralis and requires parental consent. The nurse will also provide umbilical cord care and assess for bleeding and infection. The cord should be kept clean and dry. Some facilities advocate the use of a drying or antimicrobial agent however this is no longer evidence based and can cause skin irritation.
The nurse will help to initiate the first feeding upon delivery by placing the newborn skin to skin with the mother. Mothers who are breastfeeding should be encouraged to breastfeed within the first hour and during the first period of reactivity to help promote long term breastfeeding. The formula fed newborn is typically fed within five hours. Both parents should be involved in the feedings to help facilitate bonding.
Metabolic screening will take place in to test for several inborn errors of metabolism and congenital disorders, phenylketonuria and congenital hypothyroidism, are performed in all 50 states. The American Academy of Pediatrics recommends that states test for core panel of 29 treatable congenital conditions. Tests must be done no sooner than 24 hours after initiation of feedings, with a second test repeated between 1 week and 1 month.
Hearing loss is found in 1-3% per 1000 infants. An initial hearing screen is completed before discharge with follow up scheduled if it is failed. Some infants fail for other reasons other than hearing such as amniotic fluid or vernix in the canals. Ideally treatment should occur with early intervention before 6 months of age.
Prior to discharge the critical congenital heart disease (CCHD) screening is conducted. This screens for heart defects that might otherwise not be detected through prenatal ultrasound or newborn physical examination. If the infant is undiagnosed with CCHD and discharged they may suffer cardiac collapse and death within the first few days or weeks of life. The CDC estimates 1200 newborns with a CCHD could be identified each year with the utilization of the screening. The screening is done through pulse oximetry, typically after the infant is 24 hours of age. Leads are placed on the right hand and either foot. Pulse oximetry is targeted to detect the following cardiac defects: hypoplastic left heart syndrome, pulmonary atresia, tetralogy of Fallot, total anomalous pulmonary venous return, transposition of the great arteries, tricuspid atresia, and truncus arteriosus.
A screen result would be considered positive if:
- Any oxygen saturation measure is <90%
- Oxygen saturation is <95% in both extremities on 3 measures, each separated by 1 hour.
- There is a >3% absolute difference in oxygen saturation between the right hand and foot on 3 measures, each separated by 1 hour.
Any screening that is > or equal to 95% in either extremity with < or equal to 3% absolute difference in oxygen saturation between the upper and lower extremity would be considered a negative result. (Kemper, et al. 2011).
In some instances the parents will chose to circumcise the newborn born with male genitalia. The care of the newborn during and after the procedure is important to minimize bleeding and infection. The type of instrument utilized is depending on the provider and could include the gomco clamp, mogan clamp or plastibell. The nurse will help provide comfort during the procedure by swaddling and giving Sweetease. Observe for bleeding every 30 minutes up to 2 hours. Pertoleum jelly and gauze will be placed at the site following the procedure, except the Plastibell, with reapplication during each diaper change until the wound is healed. The first void after the procedure needs to be documented and assessed. Once healing begins to take place the parents may note a yellowish granulation of the tissue which is normal.
white bumps under the skin that are opaque, whitish-yellow cysts or lesions that can form on the newborns gums or roof of the mouth. Epstein's pearls will go away on their own and should not cause concern.
Fungal infection
extra digits
webbing of the digits, can be mild or severe where all digits are completely fused
Combination of extra digits and webbing
damage to the brachial nerve which usually occurs with shoulder dystocia, Erb's palsy is damage to the upper portion of the brachial nerve.
congenital defect that can be distinguished from positional deformity by simply trying to reposition the extremity. If it moves easily it is positional.
a rare condition caused by strands of the amniotic sac that separate and entangle digits, limbs, or other parts of the fetus. This constriction can cause a variety of problems depending on where strands are located and how tightly they are wrapped.
the urethra is on the dorsal side, top, of the penis.
Opening of the urethra is on the ventral, underside, of the penis.