3
Learning Objectives
- Discuss the psychological adjustments that normally occur during the postpartum period.
- Discuss the nurse’s role in assisting with transition to parenthood as it relates to the parenting process, parental attachment, bonding and acquaintance.
- Describe the physiological changes that occur in the postpartum period as a woman’s body returns to its pre-pregnant state.
- Describe the critical elements of a postpartum-specific assessment
- Identify pharmacological interventions used during the postpartum period.
- Discuss the nurse’s responsibilities related to discharge teaching and preparation for home care
The postpartum period for the client is birth up to six weeks. It is also called the forth trimester or puerperium period of pregnancy. It is a significant time of change both physically and psychologically.
The fourth trimester is a significant time for change and a time for tremendous adjustment. Including an adjustment to the new baby, family dynamics, body image & postpartal discomforts. The Pregnancy Risk Assessment Monitoring System (PRAMS). PRAMS (CDC, 2021), a project with the CDC has monitored and tracked data in conjunction with state departments in regard to the risks associated with pregnancy. The postpartum phase of pregnancy is an important phase as the family begins the transition to the newborn. The postpartum client is still at risk for events related to pregnancy for up to 6-weeks after delivery and should be assessed and monitored accordingly. Additionally, the mother baby nurse should be aware of the educational needs of the family. The mother and baby typically have a short 48-72 hour stay on the unit. PRAMS (2019) has reported a 15.1% average of participants surveyed (n=1834) of postpartum clients reporting depression three months after pregnancy, an increase from 2016 (12.3%). Participants completing the surveys also reported breast feeding issues and concerns, inadequate education, and a need for social support.
Psychological Changes
During the postpartum period the client will experience a number of phycological changes as they adapt to the newborn. Three phases taking-in, taking-hold, and letting-go described by Rubin (1961) in regard to maternal attainment and adjustments to the parental role.
Taking In:
First 1-3 days, passive dependent. During the taking in phase the client has a great need to talk about the labor and birth experience and may be preoccupied with her own needs. Food and sleep are major needs during this phase.
Taking-Hold:
This begins after the third day and lasts up to 10 days or several weeks. The client becomes more independent and is ready to care for self and the newborn. The client begins to display maternal role behaviors and will require a lot of reassurance that she is doing well. This is a time when the mother will want to learn. During this phase the new mother may also experience the “blues”.
Letting-Go:
The letting-go phase begins several weeks after delivery and establishing a new identity with the ability to begin to focus on the family unit. The client may begin to experience resolution of individual role and sexual intimacy.
In addition to the three phases mentioned, attachment behaviors are exhibited during the postpartum period and can be influenced by a number of factors including familial origin, degree of nursing they received themselves, ongoing relationships, stability of the home environment and patterns of communication. During this attachment period both parents may experience different behaviors and are described as fingertip exploration, enfolding, en face position for the birthing client and different levels of engrossment including absorption, preoccupation and interest by the non-birthing family member. Each of the exhibited behaviors help the parents bond with the newborn and begin as a family unit.
During the first few days of the postpartum period there is a typical feeling of well-being and heightened joy by the birth of the newborn. Some women, regardless of ethnic or racial group, may experience a period of time where they feel “blue”. The postpartum blues are common and can occur in up to 50% of women. Causes for postpartum blues are unknown but have been identified with rapid changes in hormone levels and possible unsupportive environments. It is often expressed with sudden episodic tearfulness and rapid mood changes without apparent reason. The client may also experience periods of fatigue and sadness. The blues typically resolve within a couple of weeks, after this period of time the client should be assed further for postpartum depression (Lowdermilk, et al. 2020). During the postpartum period of the pregnancy it is also important to discuss and identify any cultural influences that may have an impact on the care of the client including role of the family and consumption of certain foods.
The nurse will assess the postpartum clients emotional status. This can be done by assessing the adaption to motherhood, assessing for postpartum blues, and the parent-infant attachment behaviors. The nurse will also want to encourage adequate food and fluid intake along with rest.
Physical Changes
Reproductive System
Changes in the reproductive system include changes to the cervix, fundal height, involution of the uterus, and the menstrual cycle.
The cervix will be spongy, and flaccid with minimal resistance. The cervix may also appear to be bruised initially post delivery. In addition the external os may have lacerations. Gradual changes to a lateral slit in comparison to an oval slit.
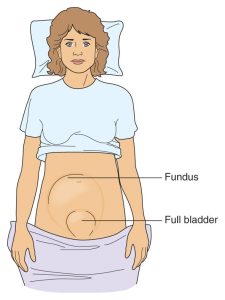
The fundal height of the postpartum client changes immediately after delivery and over the course of several days. A normal fundus is contracted and firm, a boggy uterus is related to uterine atony and is indicative of excessive bleeding. Immediately post delivery fundal massage should be performed to assist with contraction and minimize bleeding. Fundal massage can be done at any time if upon palpation the uterus feels boggy. The postpartum client should be encouraged to empty their bladder often. A full bladder can inadvertently have an effect on the involution of the uterus and create excessive bleeding by not allowing the fundus to contract and displacing the uterus. The fundus should be about half-way between the symphysis pubis and umbilicus immediately after delivery. The first day postpartum the fundus may rise to the level of the umbilicus and will decrease about one-two fingerbreadths (approximately 1-2 cm) each day. The fundus will return to pre-pregnant state by six weeks postpartum, this does however vary among clients and could be impacted by the number of pregnancies. During involution endometrial regeneration is occurring and a sloughing of necrotic tissue occurs with the healing of the placental site. Several factors can impact the progression of involution including a prolonged labor, anesthesia, difficult birth, grandmultiparity, full bladder, incomplete expulsion of the placenta or membranes, infection, and overdistension of the uterus (multiple gestations, polyhydramnios, macrosomia).
The return of the menstruation generally returns in non-breastfeeding women between six to ten weeks and in breastfeeding women at least three months (if exclusively breastfeeding).
Afterpains are similar to but milder than the pain of labor contractions. With the primaparas client the uterus tends to remain contracted following delivery and women feel only mild cramping. With the multiparas client the uterus often contracts vigorously at intervals and causes afterpains that last about three to seven days. Afterpains are more pronounced as parity increases and worsen during breastfeeding due to the release of oxytocin. The client may be treated with warm compresses, and anti-inflammatories. The nurse can encourage intermittent prone positioning. The discomfort is usually decreased by the third day.
Lochia is the discharge of uterine debris following birth consisting of erythrocytes, shredded decidua, epithelial cells and bacteria. It can have a mild musty stale odor that is normal. Assessing the lochia is a priority assessment for the nurse. Always ask the client the last time they changed the peri pad and document the amount of lochia on the pad, the color, and the odor. Assess and document for the presence of any clots or continuous bleeding. Continuous bleeding may be more consistent with lacerations and is typically bright red in color. A scant amount of bleeding is equal to a or <2.5 cm stain of lochia rubra, small amount is equal to or <10cm stain, moderate is equal to or >10cm stain, and a heavy amount of lochia rubra would saturate a pad in 1-2 hours or passing of clots larger than a small lime. TIP 1 ml = 1 gram. Initial lochia and clots are dark red and can be expressed with fundal massage from a boggy uterus.
- Lochia rubra
- First 1-3 days
- Contains blood sufficient to color it red
- May contain a few clots due to pooling in the vagina – may flow heavier when the client gets up.
- Lochia serosa
- Days 3-10
- Pinkish-brown in color; contains serous exudate, blood and leukocytes
- Lochia alba
- White in color; contains leukocytes and reduced fluid content
- Continues until the cervix is closed
- May persist up to 6 weeks in some women
When assessing the fundus in the postpartum client the nurse will need to palpate the uterus through the abdomen at approximately the umbilicus. Ensure the client is in a supine position with her knees slightly lifted and has an empty bladder. When conducting the assessment the nurse should support the lower uterine segment while pushing in a downward motion on the abdomen. Both hands will be used to conduct the assessment while cupping the upper segment of the uterine fundus which should be relative to the umbilicus (above or below). The nurse will assess for the position relative to the midline, is it midline or deviated to the left or right. Next assess for firmness or bogginess of the uterus. Assess for any discomfort or afterpains and promote comfort through repositioning, ambulation, and analgesics if ordered.
Vagina
Post vaginal delivery the vagina may be edematous and bruised with small superficial lacerations. The vaginal mucosa may be thin and dry as a result of estrogen deprivation which can be worse with the breastfeeding client. The vagina diminishes in size postpartum but rarely returns to its pre-pregnant state. Encouraging kegel exercises will help improve tone and strengthen the pelvic floor minimize stress incontinence.
Perineum
The perineum may have bruising and edema present due to the expansion of the soft tissue during delivery. In addition the client may have superficial or significant lacerations that may cause some discomfort. In some instances the provider may have had to cut an episiotomy to assist with the delivery. Lacerations are categorized by degrees from first to fourth degree.
- First degree – limited to the fourchette, perineal skin, and vaginal mucous membrane
- Second degree – involves perineal skin, vaginal mucous membrane, underlying fascia, muscles of the perineal body (central tendon of the perineum that lies between the vagina and the anus)
- Third degree – involves above plus the anal sphincter; may extend up the anterior wall of the rectum
- Fourth degree – same as 3rd degree but extends through the rectal mucosa into the lumen of the rectum
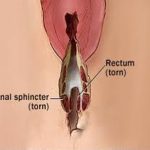
When assessing the perineum if lacerations or episiotomy exist the nurse will assess for redness, edema, ecchymoses, drainage, and approximation (REEDA). The perineum is easiest to view and assess with the postpartum client laying on their side. Ice packs or cold gel packs can be applied for the first 24 hours (10-20 minutes on and 20 minutes off, repeated as needed). Encourage warm showers and/or a sitz bath after the first 24 hours. A peri bottle can be utilized for cleansing. Provide topical anesthetic agents or analgesics as ordered.
The urinary tract may have swelling and bruising of the tissues around the urethra that can impair voiding. During the postpartum phase urinary output is greater due to a diuresis phase that occurs to begin a return to pre-pregnancy blood volume. The postpartum client may be at an increased risk of urinary tract infection due to dilated ureters and renal pelves, and can last up to six weeks post delivery. In addition a decreased sensation of a full bladder may be experienced and exacerbated if the client received an epidural. This places the postpartum client at higher risk of bleeding due to the displacement of the uterus in relation to the full bladder.
A deviated fundus as depicted below may result in an increase in bleeding since the uterus is unable to contract down fully.
Abdomen
The abdominal wall will be soft and flaccid post delivery. The broad and round ligaments have stretched and loosened to accommodate the pregnancy. Both will gradually return to pre-pregnant states. Straie may take on a different color based on the clients skin tone. Diastasis recti may have occurred in the last months of pregnancy and can be corrected with exercises.
Gastrointestinal System
The postpartum client will typically experience hunger and thirst after the delivery of the newborn. It is normal to NOT have a bowel movement two to three days after the delivery. Constipation can result from the bowels being sluggish, narcotics, bedrest and iron supplements. The postpartum client may also be hesitant to have a bowel movement related to an episiotomy, lacerations or hemorrhoids. If the postpartum client had a third or fourth degree laceration, stool softeners and/or laxatives should be provided to avoid constipation and straining which can lead to dehiscence of the tear. Flatulence (gas) can cause distended, taught abdomen and severe pain. Gas may be relieved with ambulation, gentle massage, chamomile or peppermint tea, and antiflatulent medications like simethicone. When conducting the assessment of the postpartum client the nurse will assess bowel sounds, determine status of bowel elimination and passing of gas. Additionally, the nurse will want to assess the concerns of the client regarding bowel movements related to pain, and assess for hemorrhoids to adequately provided comfort measures if needed. Pharmacological interventions including topical anesthetics (proctofoam), witch hazel pads (Tucks), stool softeners and or milk of magnesia. Encourage kegel exercises to help strengthen the pelvic floor. Ice packs can be utilized as well as a non-pharmacological measure.
Breasts
The decision to breastfeed or not to breastfeed should be made prior to delivery. It is best to initiate breastfeeding in the first hour after birth. Initially post delivery, the breasts are soft. As filling occurs the breasts become firmer. Colostrum is secreted after delivery for four to five days and can be expressed by the second day. Milk usually begins to come in on day three or four. Engorgement is caused by an increase in blood and lymphatic fluid (“congestion” or swelling) as well as milk production. During the assessment of the postpartum client the nurse will assess the nipples for cracks, fissures, redness, and soreness. The nurse should also note if the nipples are everted, flat or inverted. Encourage the client to wear a well-fitting bra to help provide support. If the client is not breastfeeding, to support the suppression of lactation a sports bra that is well-fitted, cold compresses and anti-inflammatory medications can be supplied. Cabbage leaves can also help treat engorgement.
Respiratory and Cardiovascular Systems
Maternal hypervolemia occurs immediately after delivery as result from the circulation being redirected from the placenta. There will be an initial rise in the systolic and diastolic blood pressure which will return to normal. It is not unusual to experience bradycardia (50-60 bpm). Diuresis and diaphoresis in the first few days will occur to help decrease extracellular fluid. This can result in a 3 kg weight loss. Cardiac output will decrease by 30% in the first two weeks. Hemoglobin and hematocrit will fluctuate in the first few days because of the changes in the blood volume. A 3-4% point drop in the hematocrit is equal to 500 ml blood loss. As extracellular fluid is excreted, hemoconcentration occurs with a rise in hematocrit along with a shift of interstitial fluids leading to a decrease in values. A non-pathologic leukocytosis occurs during labor and in the early postpartum period. White blood cell counts of 20,000-30,000 may be normal. Pregnancy associated activation coagulation factors continues increasing the risk for thromboembolism during the first six weeks. Conditions that may increase the risk include hypercoagulability, Cesarean delivery, immobility, obesity, cigarette smoking, varicose veins and trauma to the extremity. The nurse will conduct a head to toe assessment on the postpartum client including auscultation of the heart and lungs, and vital signs. During the assessment the nurse will also assess for deep vein thrombosis by looking for any swelling in the lower extremities (leg or calf), pain that may worsen with standing or walking, and warmth and redness in the leg.
Thermoregulation may be impacted post delivery. It is not uncommon that the postpartum client presents with an slight elevation in their temperature up to 24 hours after birth of 38° C or 100.4° F. This can be due to exertion and dehydration of labor. Additionally, the temperature may increase 24 hours breast milk comes in.
Postpartum Specific Assessment BUBBLEDE
BUBBLEDE.
- B – Breast
- U – Uterus
- B – Bowel
- B – Bladder
- L – Lochia
- E – Episiotomy/Lacerations/incision
- D – Deep Vein Thrombosis check
- E – Emotional State/Edema
Neurologic System
Headaches are common due to fluid shifts, use of spinal or epidural anesthesia, and stress. They are present in approximately 40% of postpartum clients (Lowdermilk, et al. 2020). Postpartum chill occurs immediately after delivery. The definite cause is unknown. Theories of why the postpartum client may experience chills include sudden release of pressure on pelvic nerves, fetal-maternal transfusion, maternal adrenaline, and epidural anesthesia. Interventions to help comfort the postpartum client include warm blankets, meperidine can also be utilized.
Pharmacologic Interventions
Pain Medications may be ordered for the postpartum client and include but are not limited to: Non-opioid/opioid combinations (e.g. Norco). This is hydrocodone and acetaminophen in varying dosages (e.g. 5 mg hydrocodone and 325 mg acetaminophen). Give no more than 3000 mg acetaminophen in 24 hours. Motrin—doses range from 200 to 800 mg q 4 – 6 hours (max dose is 3200 mg in 24 hours)
Vaccinations that may be administered after delivery include: Rubella or MMR (Live virus vaccines), administering just after childbirth is an advantage since the woman should not become pregnant for at least one month following the injection. Tdap (Tetanus, Diphtheria, acellular Pertussis). The CDC recommends this vaccine during the third trimester of EACH pregnancy to protect the newborn. If not given during pregnancy, it is given postpartum (but this is not ideal)
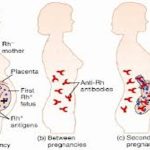
Rh Immune Globulin (Rhogam or Rhophylac) is administered to Rh-negative women with Rh-positive babies to prevent sensitization from a feto-maternal transfusion of Rh positive fetal red blood cells. It is given within 72 hours postpartum (IM or IV). This may also be administered to clients that have experienced an abortion (spontaneous or clinical). The Rh factor is present on the surface of erythrocytes of most of the population and when present, the individual is Rh positive. Those individuals without this factor are Rh negative, if the Rh negative individual is exposed to Rh positive blood, an antibody-antigen response occurs and the individual is sensitized. Subsequent exposures to Rh positive blood during pregnancy can result in hemolysis in the fetus (erythroblastosis fetalis). This exposure can occur during pregnancy, delivery, abortion, amniocentesis, CVS, or any bleeding episodes during pregnancy, prophylactic Rh immune globulin is given at 28 weeks gestation and and within 72 postpartum when the woman has an Rh positive baby and has not been sensitized.