4 Feeding and Eating Disorders
Learning Objectives
- Explain and understand the symptoms of feeding/eating disorders.
- Identify treatment strategies for behavioral addictions.
- Utilize and research SAMHSA Guidelines for identification and treatment of behavioral addictions.
- Utilize DSM – 5 TR for diagnosis and research of criterion to treat behavioral addictions.
Feeding and Eating Disorders
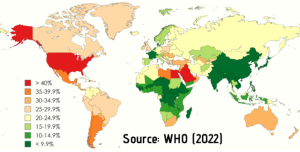
Feeding and eating disorders are “…characterized by a persistent disturbance of eating or eating-related behavior that results in the altered consumption or absorption of food and that significantly impairs physical health or psychosocial functioning” (APA, 2022, pg. 371). They are very serious, yet relatively common mental health disorders, particularly in Western society, where there is a heavy emphasis on thinness and physical appearance. As related to behavioral addiction, eating disorders become problematic when the person cannot control their compulsion to restrict, overeat, or purge food as a way of coping with psychological distress. While there is no exact cause for eating disorders, the combination of biological, psychological, and sociocultural factors has been identified as major contributors in both the development and maintenance of eating disorders. It can be argued that these disorders are related to a person’s inability to regulate normality in eating. Some individuals will over-eat, and eat to excess, while others will restrict their caloric intake. Both behaviors can be addictive in nature as a way for the person to feel in control.
Within the DSM 5-TR (APA, 2022), six disorders are classified under the Feeding and Eating Disorders chapter: pica, rumination disorder, avoidant/restrictive food intake disorder, anorexia nervosa, bulimia nervosa, and binge-eating disorder. All of these eating/feeding disorders are maladaptive and are forms of addictive behaviors.
- For more on eating disorders in general, please visit the National Eating Disorders Association website below:
- https://www.nationaleatingdisorders.org/what-are-eating-disorders
Anorexia Nervosa
Anorexia nervosa involves the restriction of energy intake, which leads to significantly low body weight relative to the individual’s age, sex, and development. This restriction is often secondary to an intense fear of gaining weight or becoming fat, despite the individual’s low body weight. Altered perception of self and an over-evaluation of one’s body weight and shape contribute to this disturbance of body size.
Typical warning signs and symptoms are divided into two different categories: emotional/behavioral and physical. Some emotional and behavioral symptoms include dramatic weight loss; preoccupation with food, weight, calories, etc.; frequent comments about feeling “fat;” eating a restricted range of foods; making excuses to avoid mealtimes; and not eating in public. Physical changes may include dizziness, difficulty concentrating, feeling cold, sleep problems, thinning hair/hair loss, and muscle weakness, to name a few. When the individual loses weight, they view this as an impressive achievement and a sign of extraordinary discipline, while weight gain is seen as an unacceptable failure of self-control (APA, 2022).
The onset of the disorder typically begins with mild dietary restrictions such as eliminating carbs or specific fatty foods. As weight loss is achieved, the dietary restrictions progress to more severe, e.g., under 500 calories/day. Symptoms present in adolescence or young adulthood and rarely before puberty or after age 40. The onset of the disorder typically is preceded by a stressful life event such as leaving home for college.
- For more on anorexia nervosa, please visit the National Eating Disorders Association website below:
- https://www.nationaleatingdisorders.org/learn/by-eating-disorder/anorexia
Bulimia Nervosa
Unlike anorexia nervosa where there is solely restriction of food, bulimia nervosa involves a pattern of recurrent binge eating behaviors. Binge eating can be defined as a discrete period of time where the amount of food consumed is significantly more than most people would eat during a similar time period. Individuals with bulimia nervosa often report a sense of lack of control over-eating during these binge-eating episodes. While not always the case, these binge-eating episodes are followed by a feeling of disgust with oneself, which leads to a compensatory behavior to rid the body of the excessive calories. These compensatory behaviors include vomiting, use of laxatives, fasting (or severe restriction), diuretics or other medications, or excessive exercise. This cycle of binge eating and compensatory behaviors occurs on average, at least once a week for three months (National Eating Disorder Association website; APA, 2022).
It is important to note that while there are periods of severe calorie restriction like anorexia, the two disorders cannot be diagnosed simultaneously. Therefore, it is important to determine the individual’s weight when distinguishing between anorexia and bulimia. If an individual has a significantly low body weight and engages in binge/purging behaviors, the diagnosis is anorexia; if the individual does not have a significantly low body weight and engages in binge/purging behaviors, the diagnosis is bulimia.
Signs and symptoms of bulimia nervosa are similar to anorexia nervosa. These symptoms include but are not limited to hiding food wrappers or containers after a bingeing episode, feeling uncomfortable eating in public, developing food rituals, limited diet, disappearing to the bathroom after eating a meal, and drinking excessive amounts of water or non-caloric beverages. Additional physical changes include weight fluctuations both up and down, difficulty concentrating, dizziness, sleep disturbance, and possible dental problems due to purging post binge eating episode.
Making Sense of the Disorders
Though anorexia and bulimia share some common features, they differ as follows:
- Diagnosis anorexia …… if significantly low body weight with severe calorie restriction
- Diagnosis bulimia … if body weight is within normal range but displays calorie restriction AND binge-eating episodes
Symptoms of bulimia nervosa typically present later in development – adolescence or early adulthood. Like anorexia nervosa, bulimia nervosa initially presents with mild restrictive dietary behaviors; however, episodes of binge eating interrupt the dietary restriction, causing bodyweight to rise around normal levels. In response to weight gain, patients engage in compensatory behaviors or purging episodes to reduce body weight. This cycle of restriction, binge eating, and calorie reduction often occurs for years before seeking help.
Additionally, those with bulimia are often ashamed of their eating problems and attempt to hide the symptoms. The binge eating occurs in secrecy or as inconspicuously as possible. Common antecedents of binge eating include negative affect; interpersonal stressors; dietary restraint; boredom; and negative feelings linked to body weight, shape, and food.
- For more on bulimia nervosa, please visit the National Eating Disorders Association website below:
- https://www.nationaleatingdisorders.org/learn/by-eating-disorder/bulimia
Binge-Eating Disorder (BED)
Binge-eating disorder is similar to bulimia nervosa in that it involves recurrent binge eating episodes along with feelings of lack of control during the binge-eating episode. The binge-eating episodes are associated with at least three of the following: eating quicker than usual, eating until uncomfortably full, eating large amounts even if not hungry, eating alone, and feeling disgust with oneself or being depressed. Despite the feelings of shame and guilt post-binge, individuals with BED will not engage in vomiting, excessive exercise, or other compensatory behaviors. These binge eating episodes occur on average, at least once a week for 3 months.
Because these binge-eating episodes occur without compensatory behaviors, individuals with BED are at risk for obesity and related health disorders. Individuals with BED report feelings of embarrassment at the quantity of food consumed, and thus will often refuse to eat in public. Due to the restriction of eating around others, individuals with BED often engage in secret binge eating episodes in private, followed by discrete disposal of wrappers and containers.
Making Sense of the Disorders
Though bulimia and BED are similar, they differ as follows:
- Diagnosis BED …… if binge eating occurs WITHOUT compensatory behaviors
- Diagnosis bulimia … if binge eating occurs AND there are compensatory behaviors to prevent weight gain
While much is still being researched about binge-eating disorder, current research indicates that the onset of BED is adolescence to early adulthood but can begin later in life. Those who seek treatment tend to be older than those with either bulimia or anorexia. Binge eating has been found to be common in adolescent and college-age samples and for all, is associated with social role adjustment issues, impaired health-related quality of life and life satisfaction, and increased medical morbidity and mortality (APA, 2022).
- For more on binge eating disorder, please visit the National Eating Disorders Association website below:
- https://www.nationaleatingdisorders.org/learn/by-eating-disorder/bed
Key Takeaways
You should have learned the following in this section of the textbook:
- Anorexia nervosa involves the restriction of food, which leads to significantly low body weight relative to the individual’s age, sex, and development, and an intense fear of gaining weight or becoming fat.
- Bulimia nervosa is characterized by a pattern of recurrent binge eating behaviors followed by compensatory behaviors.
- Binge-eating disorder is characterized by recurrent binge eating episodes along with a feeling of lack of control but no compensatory behavior to rid the body of the calories.
Review Questions
- What does mutually exclusive mean? What does it mean with respect to eating disorders?
- What are the key differences in diagnostic criteria for anorexia, bulimia, and binge eating disorder?
- Define compensatory behavior. What disorder is this found in?
References
American Psychiatric Association. (2022). Diagnostic and statistical manual of mental disorders. (5th ed. Text Revision). Arlington, VA: American Psychiatric Publishing.
