METHOD SPECIFIC INFORMATION AND CONSIDERATIONS
There are many ways to group methods of contraception. When talking about someone’s contraception options, understanding their values and preferences will dictate which options to start with and discuss. (See Contraceptive Counseling above).
Pericoital Methods (Used as-needed, near time of sex)
External Condoms
- Barrier method that prevents sperm from entering the vagina/cervix by covering the penis during vaginal intercourse. Can encourage concomitant use with other methods to further reduce pregnancy risk
- Typical use pregnancy rate: 13%
- Pros: Easily accessible, affordable, and available OTC. Protects against sexually transmitted infections (STIs).
- Cons: Single use. Costly unless free options. Can break or slip, some have latex allergies (non-latex options available). Requires partner cooperation.
Internal Condoms
- Barrier method that prevents sperm from entering the vagina/cervix by creating a barrier in the vaginal canal during vaginal intercourse. Can encourage concomitant use with other methods to further reduce pregnancy risk
- Typical use pregnancy rate: 21%
- Pros: Accessible, and available OTC. Protects against sexually transmitted infections (STIs). Can be placed up to 8 hours before sex and used during menses.
- Cons: single use; can be costly. Can break or slip, some have latex allergies (non-latex options available). Requires partner cooperation
Withdrawal (Coitus Interruptus)
- Withdrawing penis from vagina before ejaculation to prevent sperm from entry.
- Typical use pregnancy rate: 22%
- Pros: No cost and no need for medical devices. Can allow personal control
- Cons: Requires self-control, partner cooperation, and precise timing, making it less reliable. Pregnancy can still occur from pre-ejaculate seminal fluid. No STI protection.
Contraceptive gel (Phexxi®)
- A bioadhesive acidifying vaginal gel; maintains healthy vaginal pH, but is hostile to sperm; placed in vagina up to 1 hour prior to intercourse
- Typical use pregnancy rate: 21%
- Pros: patient-controlled, no partner cooperation required; non-hormonal.
- Cons: requires rx; expensive. Insurance may not cover; appeal if denied.
Spermicides
- Chemical substances designed to kill/immobilize sperm, often used in combination with other methods (e.g., condoms, diaphragms), or embedded within methods (contraceptive sponge).
- Typical use pregnancy rate: 18-29%
- Pros: Non-invasive; and can be used in conjunction with other methods for added protection.
- Cons: May cause irritation, less effective when used alone, does not offer STI protection.
- Considerations:
- Must be inserted 1 hour prior to intercourse. Some formulations require 10 min wait time to dissolve, or can only be used with certain methods.
- Νοոοхyոol-9 (NO9) comes as a cream, film, foam, gel, tablet, or suppository.
Diaphragms / Cervical Cap
- Caya®: one-size, fits approximately 80% of people without fitting
- Milex®: requires fitting / additional provider training, less available
- Works by maintaining a barrier and reservoir of spermicide against cervix
- Range of typical use pregnancy rates, by type & parity (higher failure w/ multiparous cx):
- Diaphragm: 17%
- Cap: 13-16% nullip, 23-32% multip
- Sponge: 14% nullip, 27% multip
- Pros: reusable, minimal complications, patient-controlled
- Cons: Potential side effects from spermicide, especially with frequent use
Contraceptive Sponge (Today ®)
- A non-prescription barrier contraceptive placed in the vagina, infused with NO9
- Typical use pregnancy rates: 12% nulliparas, 24% multiparas
- Pros: Patient-controlled, convenient, spontaneous
- Cons: No STI protection, NO9 can be irritating, especially with frequent use
Fertility Awareness-Based Methods (FABMs)
- Also known as ‘rhythm method,’ ‘calendar method,’ ‘natural family planning,’ and ‘periodic abstinence.’
- All FABMs involve avoiding intercourse and/or use-as-needed (pericoital) methods during the fertile part of the cycle.
- Identifies fertile days of cycle, by observing physiologic signs (cycle length, cervical secretions, basal body temperature, expected sperm/egg lifespan) (Grimes 2004).
- Wide range of typical use pregnancy rates (~2-23%) (Simmons 2020)
- Pros: body awareness and control, minimal cost and interaction with healthcare system, non-hormonal
- Cons: requires close and careful cycle monitoring and periodic abstention or use of pericoital methods; relies on recognizing patterns with monthly variation, ovulation patterns can be affected by illness or stress
- How to counsel people on the specific FABMs: (RHAP 2021)
- Information Handouts for Patients (RHAP; in multiple languages):
Short-Acting Hormonal Methods
Progestin-only Pills (POPs)
- Available over the counter or as a prescription. Various types now available listed in the table below.
- Typical use pregnancy rate: 7%
- Pros: Fewer medical contraindications than with estrogens. Possible lighter bleeding or amenorrhea. Breast/chestfeeding-friendly.
- Cons: Possible spotting first few months. Possible irregular bleeding.
- Considerations:
- If irregular bleeding is bothersome, add back estrogen if no contraindications
|
POP Comparison Table |
|||
| Medication | Norethindrone
(Micronor, 19 brands) |
Norgestrel
(OPill) |
Drospirenone
(Slynd) |
| Availability | By prescription (typically covered) | Over the counter ($15-20/mo)
Cost-Assistance Program FSA/HSA eligible |
By prescription
(insurance coverage limited) |
| Mechanism | Thickens cervical mucus | Thickens cervical mucus | Ovulation suppression |
| Missed pill window | 3 hour | 3 hour | 24 hour |
| Effects on acne | Increased | Increased | Decreased or less likely to worsen |
Depot medroxyprogesterone acetate (DMPA, Depo-Provera®) Injection
- Typical use pregnancy rates: 4%
- Pros: prevents pregnancy for 3 months at a time; decreased bleeding and pain with periods (amenorrhea 70% by 12 months), decreased risk of endometrial and ovarian cancer; can be injected in a health center or by the patient at home.
- Cons: Slower return to fertility; weight gain (especially if rapid wt gain initially).
- Considerations:
- Duration 13 weeks with flexible administration between 11 – 15 weeks (RHAP Injection Calendar)
- Available in IM for administration by a healthcare professional or subcutaneous (SC) for self-administration.
- DMPA-SC self-administration can be safely taught via telehealth (Burlando 2021), improving continuation, access, and autonomy (Kennedy 2019, Kohn 2017). Availability varies by state and pharmacy.
- Despite concern for decreased bone density after 2 years of DMPA use (FDA label), bone density loss is reversible after discontinuation and limited studies of DMPA do not demonstrate an increased fracture risk (ACOG 2014)
Combined Hormonal Contraceptives (Pill, Patch, Ring)
- Mechanism: ovulation suppression; endometrial thinning, thickening of cervical mucus
Typical use pregnancy rate: 7%- Pros: Decreased dysmenorrhea, PMS, menstrual migraines, acne, gynecologic cancers, ovarian cysts, PID, benign breast tumors, osteoporosis
- Cons: Rare adverse health outcomes: VTE, heart attack, stroke for some risk categories
- Considerations:
- Periods during CHC use is called ‘withdrawal bleeding’ when hormone levels drop during the hormone-free interval, and is usually lighter than regular menses. Hormone-free interval may be shortened (from 7 to 4 days) or removed (see Continuous Contraception below)
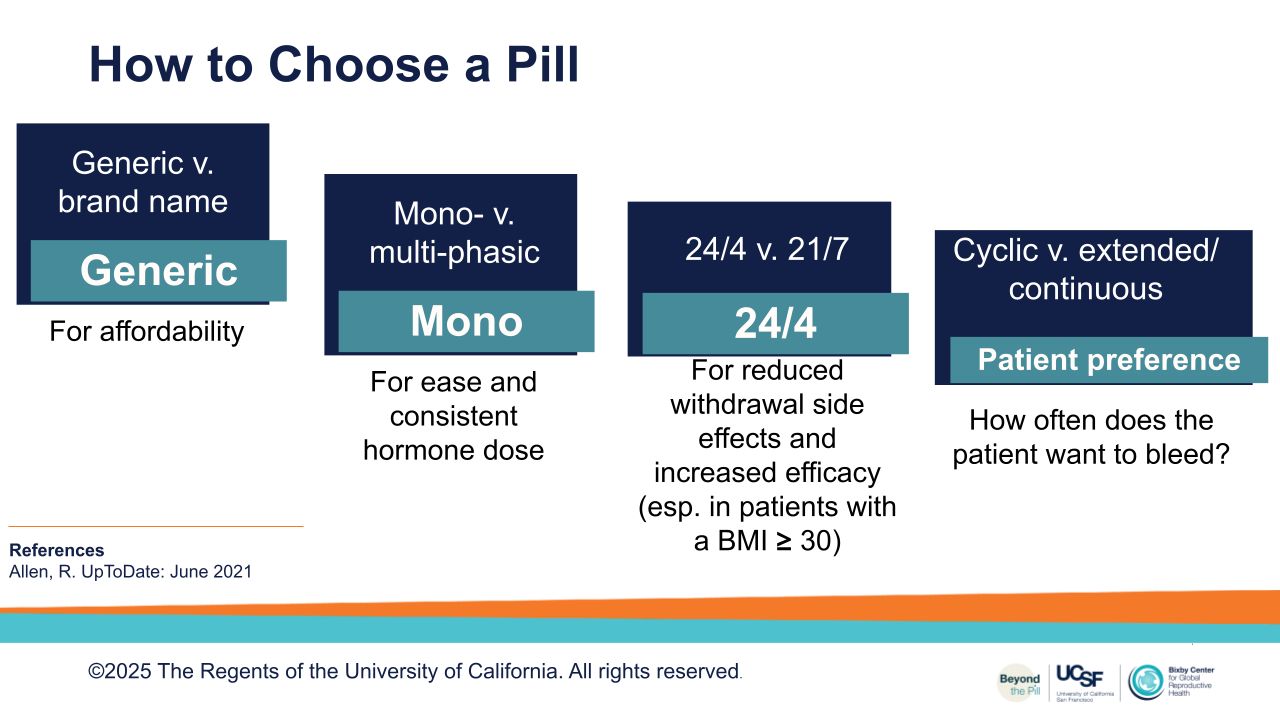
Combined Oral Contraceptives (COC)
- Pros: As above.
- Cons: Spotting first few months
- Considerations:
- Most contain 20-35 mcg of ethinyl estradiol plus one of eight progestins
- Recently FDA-approved pill Nextstellis® with novel estrogen (estetrol –E4).
Vaginal Ring:
- Flexible ring that the user places in the vagina; no fitting required.
- Pros: monthly use
- Cons: Can be inadvertently expelled, leading to failure if unnoticed.
- Considerations:
- Annovera® Ring is FDA approved for 13 cycles
- Use 3 weeks/1 cycle, wash, replace same ring next cycle
- NuvaRing / EluRing is FDA approved for 1 cycle
- Use new ring for 3 weeks/1 cycle, discard, place new ring next cycle
Patch:
- Pros: weekly use; as above
- Cons: can cause allergic skin reactions; only available in one color.
- Considerations:
- Xulane® Patch is a smaller patch with higher dose (Xulane FDA label).
- Twirla® Patch is larger patch with lower dose (Twirla FDA label)
- Patch and Weight:
- Both Xulane® and Twirla® are MEC 2 with higher weight due to increased VTE risk. There is also a concern for decreased efficacy (>198 lb; BMI ≥30).
- However, the concern about patch VTE risk is based on four participants who experienced VTE during a Twirla® clinical trial (Twirla FDA label).
- Use a harm reduction approach when considering this method: If a person favors the patch, consider that their risk of pregnancy is higher without contraception and VTE risk is higher in pregnancy.
Continuous CHC Contraception to Reduce / Eliminate Withdrawal Bleeding
- Defined as using CHCs in a continuous or extended fashion (skipping placebo weeks) to have longer intervals between bleeding.
- Fewer scheduled bleeds; less estrogen-withdrawal symptoms (Edelman 2014).
- Unscheduled bleeding decreases over time (often 6-12 months) with these regimens.
- Various monophasic OCP and vaginal ring (Annovera® or NuvaRing®) can be used.
- Continuous use of patch is controversial given theoretical increased VTE risk; only 1 study shows efficacy (Stewart 2005).
Long-Acting Reversible Contraception (LARC)
- Typical use pregnancy rates < 1%
- Pros: Highly effective, low-effort maintenance, long acting, improved continuation (Diedrich 2015)
- Cons: pain with insertion (IUD), requires removal sometimes by a healthcare professional. Health system and public health promotion has created incentivization and disproportionate coercion at expense of person-centered counseling (Boydell 2023, Higgins 2016).
- Recommendation:
- Prioritize prompt LARC removal without delay or resistance, advising that removal is possible whenever it is desired and prior to discussing trial or awaiting symptom resolution (Amico 2018). Counsel about IUD self-removal.
- Pros: The copper IUDs available in the US (Copper 380 mm2, and new Copper T175 mm2) are both hormone-free. LNG 52 mg IUD provides symptom management for menorrhagia.
- Cons: Insertion pain is significant for many, and underestimated by providers. (See Appendix A: Pain Management for IUD Placement). Copper IUD can increase or prolong uterine bleeding and worsen dysmenorrhea, although the new Copper T175 mm2 improves bleeding profiles.
- Considerations:
- No association of IUD with increased infertility risk (Hubacher 2001)
- Cu T 380 and LNG 52 mg IUDs can be used as emergency contraception (EC), regardless of weight (Turok 2021, Wu 2010)
- Self-removal is safe; 3 in 10 are successful (Petrie 2024). May improve satisfaction and autonomy (Foster 2014, Raifman 2018) (RHAP: IUD Self-Removal Fact Sheet)
- Routine IUD string checks and follow-up visits are unnecessary and unsupported by evidence (Davies 2014)
- Place any time in cycle if reasonably sure person is not pregnant (CDC SPR 2024)
- Early evidence IUD can be placed any time in cycle with negative UPT (BakenRa 2021)
- No routine antibiotic prophylaxis needed (CDC SPR 2024)
- Back-up method 7 days (CDC SPR 2024), although early evidence suggests not required after LNG-52 mg or Cu IUD placement, more evidence needed (Fay 2021)
- IUD Placement Videos (IERH): https://bit.ly/3O6gF1T
- New Cu-T IUD (2024) placement video: https://bit.ly/4bvkxWt
|
IUD Options for Individual Preferences (Adapted from UCSF Beyond the Pill Program) |
|||
| IUD Type
(Names) |
Cu-T IUD
(Paragard®) |
LNG 52 mcg IUD | LNG 13.5 – 19.5 mcg IUD |
| Desired Bleeding
Pattern |
|
|
|
| Hormone and Cycle Considerations |
|
|
|
| EC |
|
|
|
| Duration |
|
|
|
Contraceptive Implant (Nexplanon®)
A small, flexible rod placed under the skin of the upper arm that releases progestin to prevent pregnancy
- Mechanism of action: prevents ovulations, thickens cervical mucus
- Pros: Minimal placement pain with lidocaine, discrete, prevents pregnancy for up to 5 years.
Cons: High risk of irregular bleeding (CDC SPR 2024), requires an in-office procedure for placement and removal - Considerations:
- Average placement < 1 min, removal < 4 min (Levine 2008). Radiopaque, visible on x-ray.
- To avoid deep placement, insert < 30° and view from the side.
- Implant placement video (IERH): https://bit.ly/3HCeFMi
- Pop out removal technique video: https://bit.ly/3GtSBCY
- For difficult or deep removal, contact Family Planning Specialists at some academic centers or others with upper extremity surgical proficiency.
Permanent Contraception
Tubal Ligation
- Requires surgery and permanently blocks, burns, removes, or cuts fallopian tubes
- Typical use pregnancy rate: 3%
- Pros: Permanent and highly effective.
- Cons: Surgery with risks of infection, bleeding, pain, and reactions to anesthesia. Consent waiting period can be a barrier. Some have regret: rates vary from < 10-30%; decreases with age; increases with pre-existing relationship conflict (Danvers 2022). Pregnancy after reversal is approximately 65% and decreases with age (Sastre 2023).
- Considerations: Federal regulations mandate a 30-day waiting period between consent and procedure for those on Medicaid, with exceptions for emergency surgery or premature delivery.
Emergency Contraception
Emergency contraception (EC) refers to methods of contraception used post-coitally (after unprotected or underprotected sexual intercourse) to reduce the risk of pregnancy. May be used as needed or desired, including when other contraceptive methods fail (e.g. broken condom), or after non-consensual sex or assault. EC refers to both pill-based methods as well as IUD placement which requires seeing a healthcare provider.
- Pills work by preventing or delaying ovulation (Salcedo 2023). Levonorgestrel pills are available OTC, online, or with a prescription, increasing access for people of all ages and genders. Ulipristal Acetate pills require a prescription.
- The copper IUD interferes with sperm maturation and motility (Salcedo 2023, Wu 2010). More recently, the LNG IUD was found to be non-inferior to the copper IUD as a method of EC (Turok 2021). Both the copper and levonorgestrel IUDs are thought to create a foreign body reaction in the uterus that prevents pregnancy. Placement of an IUD requires an in-person visit with a provider.
- Typical use pregnancy rates: <1% to 2.1% (see table below)
- Pros: As needed use
- Cons: Requiries access in a specific time frame, pill options may create irregular bleeding/altered menstrual cycle, IUD can be difficult to access without insurance/trained providers, pills are less effective around time of ovulation (Glasier 2011).
- After UPA EC pills, consider delaying the initiation (not re-starting) of hormonal contraception by 5 days due to a risk of decreased prevention of ovulation (ASEC 2016, Salcedo 2023, CDC SPR 2024).
|
Emergency Contraception Methods (Adapted from UCSF Beyond the Pill Program) |
||||
| Method | Levonorgestrel (LNG) 1.5mg Pill | Ulipristal Acetate
(UPA) 30mg Pill |
Copper IUD | Levonorgestrel (LNG) 52 mg IUD |
| Access | OTC or Prescription | Prescription | In-clinic procedure | In-clinic procedure |
| FDA status for EC | FDA-Approved | FDA-Approved | Off label | Off label |
| Mechanism | >Delaying or inhibiting ovulation up to LH surge | Delaying or inhibiting ovulation, after LH surge (thus slightly more effective than LNG EC) | Prevents fertilization
by decreasing sperm motility, egg survival, and fertilization steps |
Prevents fertilization
by decreasing sperm motility, egg survival, and fertilization steps |
| Pregnancy rate | 2.1% pregnancy rate per unprotected act | 1.2% pregnancy rate per unprotected act | < 1% pregnancy rate | Non-inferior to Cu IUD in efficacy (Glasier 2011, Shen 2017, Turok 2021) |
| Weight / BMI | Weight <165*
BMI <25* |
Weight <194*
BMI <30* |
No weight limit | No weight limit |
| Considerations | Effective up to 3 days after UPSIC | Effective up to 5 days after UPSIC
Delay hormonal contraceptive start 5d after UPA |
Place up to 5 days after sex. May place anytime in cycle with a negative UPT. | >Place up to 5 days after sex. May place anytime in cycle with a negative UPT. |
*Use a harm reduction approach: If a patient does not meet the FDA-approved weight criteria and favors ECP, consider that their risk of pregnancy is higher without any form of contraception.
Yuzpe Method is combined OCPs taken < 72 hr after UPSIC; repeated in 12 hr. Has much higher typical pregnancy rate (15-45%), with more side effects than other ECPs, but important when there are barriers to access and privacy.
Weight and EC
- LNG ECP may be less effective with weight ≥ 165 lb / 75 kg (BMI ≥ 25).
- UPA may be less effective with weight ≥ 198 / 90 kg, BMI ≥ 30; thought to be more effective than LNG ECP across weight ranges.
- While efficacy of LNG EC pills and UPA EC pills is decreased in people with increased weight (Glasier 2011), it remains MEC 2. However, people over 198 lb / 90 kg made up less than 3% of the study population, so these data should be interpreted with caution (FDA Label). No one should be discouraged or restricted from using EC based on weight (Kardos 2019). After counseling, all options should be offered (Festin 2017).
Evidence that IUD and LNG EC Pills (ECPs) are not abortifacients
- Neither IUDs nor LNG ECPs will disrupt an implanted pregnancy or cause an abortion. IUD can prevent fertilization and implantation (Salcedo 2023, Turok 2021).
- Post-IUD tubal flush studies find no fertilized eggs (Ortiz 2007).
- Post-IUD transient hCG elevations not found (Wilcox 1987).
- LNG ECPs prevent ovulation by blocking LH surge, inhibiting follicular development and egg release. UPA delays ovulation, including after LH surge started. This extended activity likely explains UPA’s greater efficacy (Turok 2024).
- LNG EC taken after ovulation has similar conception rates vs. placebo. No effects on fetal development, miscarriage, stillbirth, or subsequent menses (Endler 2022).
- Although UPA (at higher dose) + Miso was found to be effective for abortion, when used alone, UPA does not affect an established pregnancy. Efforts to limit UPA as EC are detrimental, since it is effective up to 5 days after UPSIC, while LNG is effective up to 3 days. Additionally, UPA is more effective than LNG for people with larger bodies (Winikoff 2025).
Contraception After Abortion
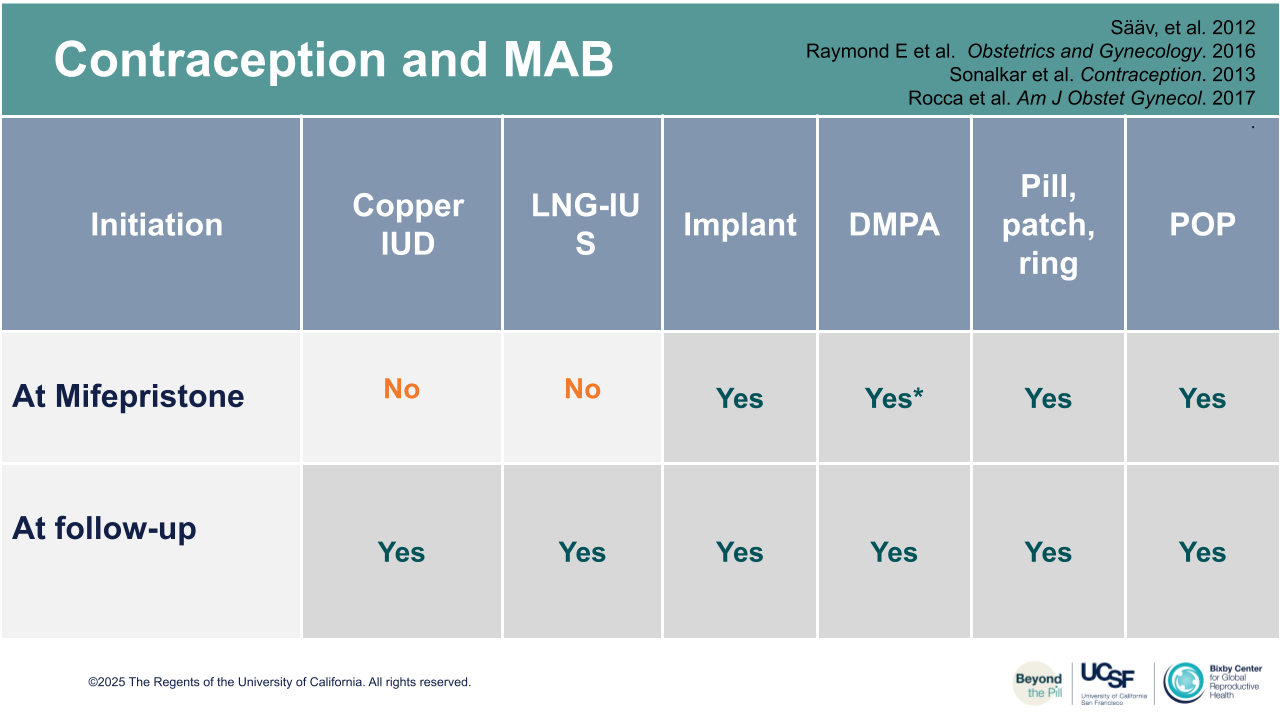
All methods can be initiated at the time of procedural abortion.
Most methods can be initiated at any time of medication abortion, with the following considerations:
- Barrier methods: as soon as the patient resumes intercourse.
- Combined hormonal contraceptives: may start at any time (Tang 2002).
- DMPA Injection: may start at any time, may be provided IM in a health center or SQ for home use if available. Advise that injection at time of mifepristone is associated with a slightly increased rate of continuing pregnancy on the order of 1-3% (Raymond 2016).
- Implant: placement at time of mifepristone enhances patient satisfaction without increasing MAB failure rates (Raymond 2016).
- IUD: placement at follow-up visit after confirming MAB completion; may have slightly increased risk of expulsion (Sääv 2012).
- Permanent contraception: consents must be signed (30-180 days prior to procedure in the U.S. for patients with public insurance), refer and offer an acceptable bridge method.
- EC: offer and dispense or prescribe for future use.
DMPA with mife shows slight increase risk of continuing pregnancy risk (< 3%), without increased need of uterine aspiration or increased 6-month repeat pregnancy rate. Increased satisfaction” (Raymond 2016).
Contraception for People Who Create Sperm
Methods requiring cooperation of a sperm-producing partner are listed above and include external condoms, spermicides, and withdrawal. Additionally, vasectomy is an option for sperm producing individuals.
Vasectomy / Permanent Contraception
- Surgical procedure that involves separating and sealing both vas deferens, the tubes carrying sperm from the testes to the penis, as a means of permanent contraception, typically by cutting or cauterizing.
- Typical use pregnancy rate < 1%
- Pros: Highly effective, office-based procedure with no known impact on sexual performance. More effective and safer than tubal procedures. Can be done in an ambulatory care setting without general anesthesia.
- Cons: Surgical risks include infection, pain, and bleeding. Requires a backup method for 3 months before confirming success. Reversal is difficult and not always successful (Hollingsworth 2007).
- Considerations: Obtain a ѕеmеn analysis 3 months postoperatively (Sharlip 2012). The person should have had at least 20 ejaculates since the time of vаѕесtоmy
Additional Contraceptive Forms Under Investigation for People Who Produce Sperm
- Pills: typically focusing on blocking sperm production or reducing sperm motility.
- Contraceptive injections: injection of hormones to reduce sperm count.
- Contraceptive implants: typically releasing hormones to suppress sperm production.
- Reversible inhibition of sperm under guidance (RISUG): polymer gel injected into the vas deferens to block sperm flow.