BUILDING AND MAINTAINING YOUR SKILLS
There are many options to consider in developing and maintaining your skills, knowledge and leadership in reproductive health, rights and justice, both during and after training. Support can be identified through help from mentors and existing national networks and organizations.
Gaining and Maintaining Clinical Competency
Medication abortion now accounts for more than 60% of the abortions in the U.S., with 40% of reproductive clinics offering only medication abortion. There has also been an increase in telemedicine consultation and the mailing of medication abortion pills (Jones 2024). Expanding clinical care to include medication management for early pregnancy loss and abortion is vital to providing comprehensive, evidence-based care and an important step in normalizing their use in primary care.
As abortion in the U.S. becomes more restricted, training in telehealth medication abortion may be especially important, and new providers entering care can contribute to access and medication availability. Even if not providing abortion care, supporting and guiding patients before and after their abortions will be critical, especially in restrictive states and/or if care was self managed.
Obtaining abortion training during professional training is helpful, when both credentialing and malpractice are covered under interagency agreements between a training program and a high-volume clinical site. However, there are also opportunities after formal medical and nursing education. The following organizations offer training opportunities throughout this spectrum:
- Medical Students For Choice
- Clinical Abortion Training Centers
- Nurses for Sexual and Reproductive Health: Training Opportunity for RNs, Doulas, Medical Assistants, and Emergency Personnel
- Reproductive Health Access Project (RHAP): Reproductive Health and Advocacy Fellowship
- Repro TLC (formerly Midwest Access Project)
- TEACH Leadership Fellowship and Accelerator Program
- Black Midwifery Fellowship
- Kansas Clinical Family Planning Fellowship
- RADIANT at University of Illinois, Chicago
- MARCH at University or Maryland, Baltimore
- RTEI at Rutgers
- GCSRH at University of Washington, Seattle
Each skill can be delineated into clear steps with observable competencies for learners and trainers-in-training (See Ch 13: Core Competencies). Important aspects of clinical competence in medication and aspiration abortion include person-centered counseling and the ability to identify and triage complications as they arise (Levi 2012). The number of cases to achieve competence and confidence in medication or aspiration abortion will vary between individuals, training environment, and exposure to complications or complex cases.
CONSIDERATIONS FOR ADVANCED PRACTICE CLINICIAN (APC) PROVIDERS
APCs (including NPs, CNMs, PAs) have a long history of providing primary, reproductive, and abortion care, especially in underserved areas (Samora 2007). Despite this, APCs have not traditionally been recognized or widely utilized as abortion providers in the U.S. as they have in many countries, due to outdated policies, classism, white supremacy and entrenched perceptions that have restricted abortion care to physicians. However, this is shifting as evidence continues to support the safety, efficacy, and acceptability of APC-provided abortion care (NASEM 2018). Expanding the role of APCs in abortion care is both a practical and necessary step in addressing access gaps, particularly in communities facing provider shortages. Research has consistently shown that APCs can provide medication and procedural abortion services with competency equivalent to physicians (Levi 2018; see Ch 13: Core Competencies). With additional training opportunities and institutional support, APCs can play an even greater role in increasing access to abortion, miscarriage management, and post-abortion care.
Even as the policy landscape evolves to permit APCs to provide abortion care, clinical training opportunities remain limited. Historically, APC training programs have not adequately incorporated abortion care, leaving many without access to formalized education and hands-on clinical experience. However, new state-level initiatives are emerging that prioritize APC training and create clearer training pathways for both new and existing providers. (See Organizational Resources Table: Fellowships below)
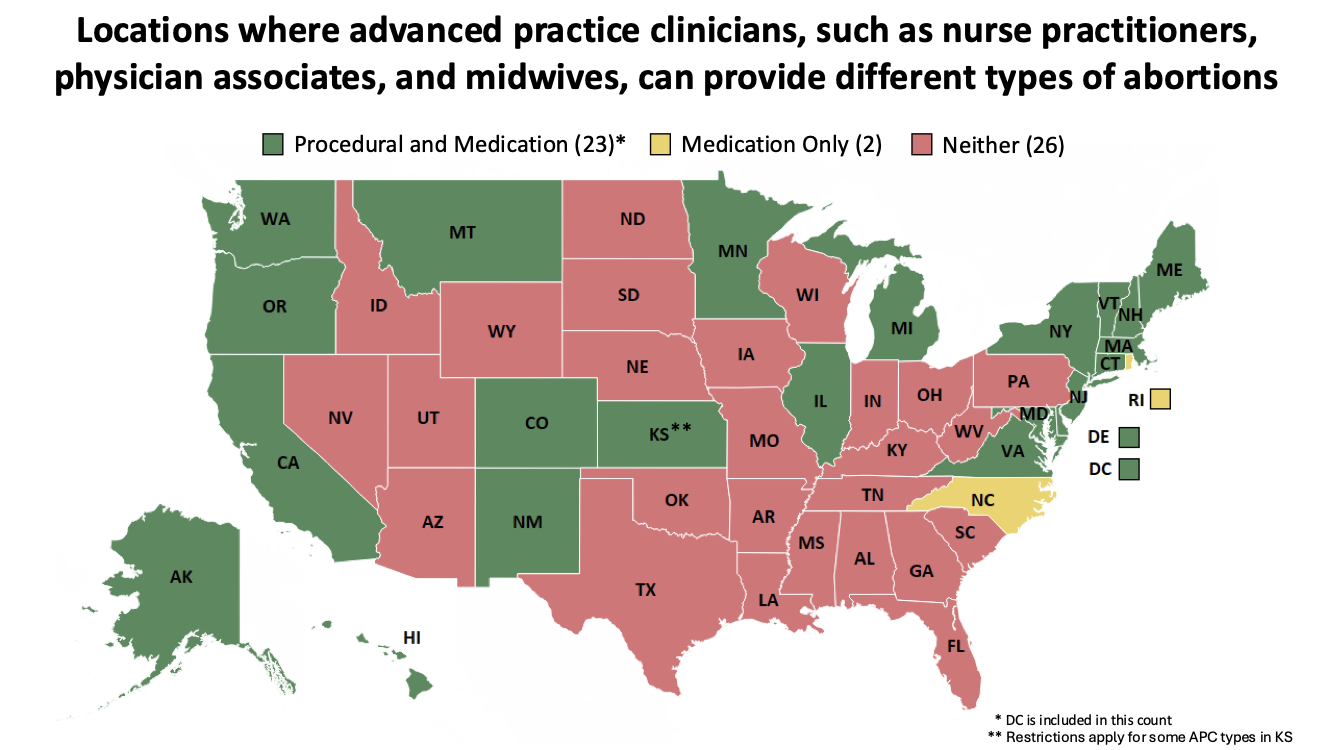
Currently, 23 states plus D.C. allow APCs to provide both medication and procedural abortion care. While 2 states allow APCs to provide medication abortion care only (Jenkins 2025). While these policy changes represent progress, significant barriers remain. State regulations related to physician oversight impose additional burdens on APCs, creating unnecessary legal and logistical challenges that limit their ability to provide care. Legal scope of practice for APCs continues to be shaped by laws restricting abortion provision to physicians, which act as barriers— similar to restrictions in states where even physicians are prohibited from providing abortion care within their professional scope (Jenkins 2023). For more information, see the APC Toolkit Map, NAF CIAC, Guttmacher Interactive Map, the Law Atlas Policy Surveillance Project, ACOG 2023, APHA 2011 and also consider contacting your local Board of Registered Nursing or PA licensing board.
Physicians and administrators can support APC involvement by prioritizing their training, ongoing practice volume and professional development opportunities, and offering resources for clinical advice (see the RH Hotline below),and ensuring guidance on referrals as needed.
Jenkins, J. APC Toolkit: 2025
Building a Strong Knowledge Base
Please consider using the following resources to develop foundational knowledge, review evidence-based practices, and expand understanding:
- Online resources:
- Innovating Education: videos, materials, and resources on abortion, early pregnancy loss, contraception, counseling, and more.
- National Abortion Federation: online courses on abortion, contraception, ultrasound, trans-inclusive abortion care, and values clarification for members, which includes providers, advocates and organizations.
- Reproductive Health Access Project: resources and patient information on abortion, contraception, and miscarriage management.
- Contraceptive Pearls (RHAP): sign up and review previous pearls on contraception.
- Insights (RHAP): sign up and review previous articles on abortion and EPL.
- Nurses for Sexual and Reproductive Health (NSRH): online learning portal for members with educational modules on sexual and reproductive health.
- Partners in Contraceptive Choice and Knowledge: provider and patient resources and webinars.
- AbortionPillCME: See one, do one, teach one medication abortion training.
- Access Listserv: National private discussion group for primary care clinicians and learners to participate in ongoing discussions about reproductive health care provision, training, and advocacy. Membership requires referral by a current participant for security reasons.
- TEACH Curriculum: complete supplemental readings in each chapter, and complete post-tests and evaluation to obtain CE credits.
- RHEDI Resources (now housed at TEACH): list of residencies offering routine abortion training, and other resources related to the training and provision.
- Advancing New Standards in Reproductive Health (ANSIRH): a UCSF based research program offering information related to abortion and reproductive health.
- Provide: an organization that offers free training and technical assistance to organizations around sexual and reproductive health care including abortion care.
- White Coats for Black Lives: a medical trainee-run organization focused on dismantling racism and oppression in healthcare.
- Medical journals:
- Books:
- Reproductive Justice, Loretta Ross and Rickie Solinger
- Radical Reproductive Justice: Foundation, Theory, Practice, and Critique, Loretta Ross, Lynn Robers, Erika Derkas, et al.
- Killing the Black Body, Dorothy Roberts
- Reproductive Justice section of Haymarket Books
- Interrupting Criminalization Resource Documents
- Sister Outsider, Audre Lorde
- You’re The Only One I’ve Told: The Stories Behind Abortion, Meera Shah
- Shout your Abortion, Amelia Bonow, Emily Nokes (Editors)
- The Turnaway Study, Diana Greene Foster
- Policing the Womb, Michele Goodwin
- Choice Words: Writers on Abortion, Annie Finch
- Liberating Abortion, Renee Bracey Sherman, Regina Mahone
- How We Get Free: Black Feminism & Combahee River Collective, Keeanga-Yamahtta Taylor
- Undivided Rights Women of Color Organizing for Reproductive Justice, Marlene Gerber Fried, Elena Gutiérrez, Loretta Ross, and Jael Silliman
- Reproductive Rights and Wrongs The Global Politics of Population Control, Betsy Hartmann
- Relinquished: Politics of Adoption and Privilege of American Motherhood, Gretchen Sisson
- Textbooks:
- Management of Unintended and Abnormal Pregnancy, Maureen Paul
- Contraceptive Technology, Patty Cason
- Radical Reproductive Justice, Whitney Peoples and Loretta Ross
- Procedures in Primary Care, Grant Fowler
- Abortion Pills: US History and Politics, Carrie Baker
- Varney’s Midwifery, EPL and Abortion Chapter, Julia Phillippi and Ira Kantrowitz-Gordon
- Podcasts:
- Reproductive health conferences:
Achieving Diversity, Equity, and Inclusion In Training and Provision
The frameworks of Reproductive Justice and anti-racism (See Ch 1: Reproductive Health through a Justice Lens) should be employed in training to achieve diversity, equity, and inclusion in both training environments and abortion care (BMMA 2020, Ross 2017). The pervasiveness of white supremacy and racism in medicine, and reproductive health specifically, has harmed BIPOC and other intersectionally oppressed communities for generations.
This has sustained white providers in positions of power and decision-making and/or providing abortions for communities with whom they may share little background. For example, recent analysis shows large differences in physician and patient ethnicities (AAMC 2019, Guttmacher 2016).
| Ethnicity | Physicians | Patients |
| White | 56% | 39% |
| Black | 5% | 28% |
| Hispanic | 6% | 25% |
People may prefer providers of the same racial and ethnic background, and although further study is needed, shared racial/ethnic backgrounds may foster better relationships, continuity, and health outcomes (Miller 2022). In order to better meet the health needs of marginalized and diverse populations, we need to increase abortion provider diversity (Ma 2019, Smedley 2001).
Priority should be placed on supporting and training providers of diverse racial, ethnic, and socioeconomic backgrounds, as well as abilities, mirroring and honoring the diversity of patients and communities. Beyond training, space should also be made in leadership positions in order to effectively change the systems we operate and organize in.
Given the hierarchical nature of training environments and historical systemic discrimination in healthcare, support and mentorship should also be provided around navigating power structures and racism. Abortion providers experience additional layers of discrimination given the politicization and polarization of reproductive healthcare which should also be acknowledged and addressed (León 2018).
In addition to cultivating a diversity of providers and a supportive community, it is also important to center anti-racism as a praxis to actively dismantle oppressive structures and reimagine communities that center the priorities of the most marginalized and intentionally shift power and resources, both in the provision of clinical care and in clinical training environments.
Mentorship
Mentorship is a powerful tool in creating a more diverse and enriched abortion provider community. During training, connect with larger communities of reproductive healthcare providers (see Organizational Resources Table below), reach out to faculty who can serve as a reference or connection to other communities, attend conferences, or join the AMSA Mentorship Sprint. After training, consider mentoring a student or trainee, to help fill gaps in training, or lead a project related to reproductive health and justice. Build and maintain relationships with providers whose work you admire and consider reaching out for advice when considering career moves.
Landscape and Limitations
There are many reasons why abortion training and provision is limited, including bans and restrictions, limited funding for training, saturation of providers in urban coastal areas, and government or institutional policies limiting abortion provision to OB/GYNs or fellowship-trained physicians. The SCOTUS decision overturning Roe in June 2022, had seismic impacts on the landscape of abortion training across all states (Vinekar 2024, Dicenzo 2024, Wulf 2023). Access to care, training opportunities, trainee recruitment to specialties, limiting career locations are amongst the changes impacted by this decision (ACOG 2024, Baden 2024, Vachon 2024)
Clinics in provider shortage areas may be more willing to help with credentialing and malpractice, but back-up and security issues may also be more challenging in these locations. For more information on training outside of a program’s standard curriculum or after graduation, see Organizational Resources Table below.