PRE-ABORTION PREPARATION
Pre-Abortion Evaluation
- Most evaluation is equivalent to care for those <14 weeks, including:
- Systematic review of health history, relevant obstetric history (previous vaginal deliveries / cesarean / ectopics), medications, substance use, and allergies is recommended (see Ch 3 Pre-Abortion Evaluation).
- Rh status, hemoglobin and/or hematocrit, STI tests as needed (see Ch 3 Pre-Abortion Evaluation),
- Additional information for procedures ≥14 weeks includes:
- US with placental location for everyone ≥14 weeks
- For people with previous uterine surgery/scar and anterior low-lying (< 2 cm from internal os) or placenta previa, screen for PAS with US with doppler flow if possible in clinic setting (by the person with most experience available) (AJOG 2025, Philips 2019).
- For initial placental location, view the uterine-bladder interface in the sagittal plane. Fundal placentation and/or lack of previa is quite reassuring. For specific US and doppler findings of PAS see Adu-Bredu 2022.
- Transvaginal US allows for close evaluation of placentation, particularly in the setting of anterior low-lying placenta or placenta previa.
- People with prior uterine surgery/scar may have a procedure in an outpatient setting, after appropriate exclusion of PAS (NAF 2024).
- For rare PAS, refer to a higher level of care to mitigate hemorrhage risk.
Pre-Abortion Procedures
Patients receiving procedural abortion care at >14 weeks should receive:
- Routine IV access for ease of administration of medications, due to the increased risk of bleeding in later gestations, and greater likelihood of needing IV sedation (NAF 2024).
- Routine antibiotic prophylaxis co-administered with pain medications prior to misoprostol cervical prep or procedure itself, or at insertion of osmotic dilators (SFP 2025, NAF 2024; See Ch 5 Pre-procedure medications).
- Adequate pain management due to greater cervical dilation, procedure time and uterine instrumentation (See Ch. 5 Pain Management).
Cervical Preparation
Adequate cervical preparation is necessary to allow for uterine evacuation, and to minimize prolonged, difficult, or complicated procedures (Grimes 1984, Schulz 1983). Approaches vary by region, training, available resources, staffing, flow, clinical history, and person-centered wait time considerations. Cervical preparation initiated early in the day can facilitate same-day procedural abortion. These recommendations are suggestive rather than prescriptive, as many methods of cervical preparation have been validated as safe and effective, with minimal difference in procedure time and complications (Newmann 2010).
Table 1. Properties of Various Cervical Ripening Agents |
|
| Misoprostol | Prostaglandin E1 analogue providing cervical preparation. Dose range 400-600 mcg (400 mcg most common) PV or BU 30 minutes to 4 hr prior to procedure. |
| Mifepristone | Progesterone receptor antagonist providing cervical ripening and increased misoprostol responsiveness. Dose 200 mg PO 24-48 hrs prior to procedure. Mild increased risk of pre-procedure pregnancy expulsion (Newmann 2010). |
| Synthetic osmotic dilator (Dilapan-S®) | Synthetic osmotic dilator with strong outward radial force; maximum dilation (3-4x original diameter) within 4-6 hours (making them a good option for same day cervical prep). These come in 3 to 4mm diameter by 55 to 65mm length. May shorten as swells, impacting internal os dilation if not adequate length. Expensive. |
| Laminaria | Sterilized seaweed rods with both radial force and some prostaglandin release properties at maximum dilation (3 to 4x original diameter without shortening) within 12 to 24 hrs. Sizes range from 2 to 10 mm in diameter by 60 to 85mm in length. Avoid for people with allergies to iodine and seafood. |
| Foley balloon | Foley bulb placed transcervically, inflated to 30 to 50 mL of normal saline, and taped to the patient’s leg for 4 hours. Maximum dilation of 1.5 to 4 cm achieved. Alternative to osmotic dilators (Ali 2020, Sium 2022). |
Most procedures from 14 to 18 weeks can be accomplished via same-day cervical prep methods (see below). Same day misoprostol alone is usually adequate to achieve cervical ripening for dilation through 16 to 17 weeks (49 or 51 Pratt) (Fox 2014, Nucatola 2008).
Greater same-day dilation can be achieved with the placement of one to several synthetic osmotic dilators (Dilapan-S®) with or without misoprostol. Some people, such as minors or a person with a history of multiple prior c-sections or uterine anomalies, would benefit from same day cervical preparation with osmotic dilators alone. Osmotic dilators, when placed in the closed cervix, absorb moisture from the tissues and swell, opening the cervix due to slow progressive action (Socha 2023). To minimize “hourglassing” and to aid in removal – consider placing a “keyhole” dilator in center of the set, extruding more from external os, OR using a combination of synthetic osmotic dilators (which stretch more with traction to remove) and laminaria (which undergo less radial expansion during same-day prep) (see Figure 9 and Tables 1 & 2 for specific types and considerations).
 |
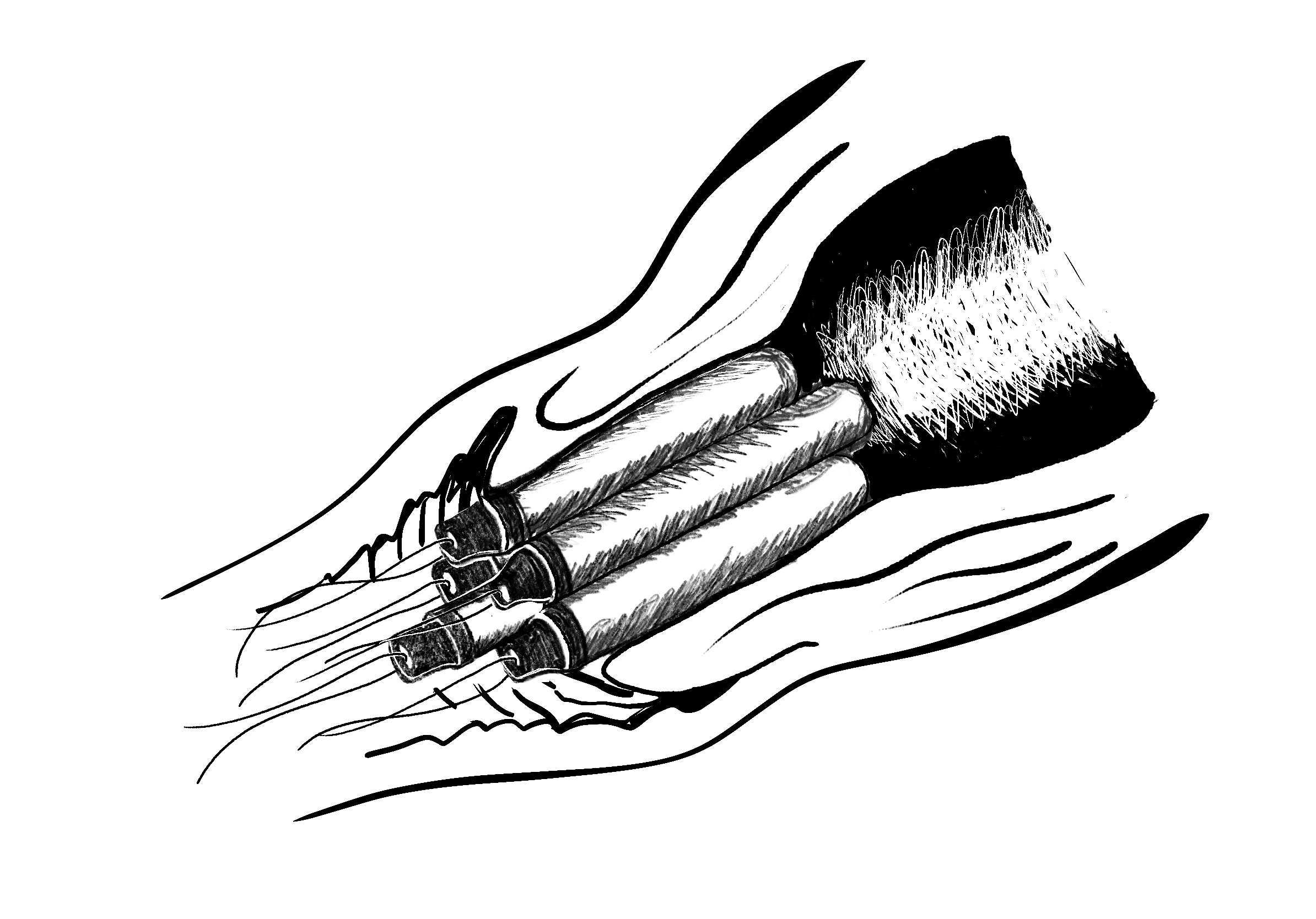 |
Figure 5a: Correct osmotic dilator placement, through external and internal os, ensures uniform dilation. 5b: A“keyhole” dilator in center of the set, which extrudes more from external os than the others, helps minimize “hourglassing” and aids in removal.
Although rarely needed for procedural abortions up to 18 weeks, two-day procedures can be planned, using cervical preparation with mifepristone and/or osmotic dilator placement on day 1, followed by the option of adding misoprostol on the procedure day.
Table 2. Options for Cervical Preparation¹,2 |
||
| Gestational Duration | Same Day Cervical Prep |
Overnight Cervical Prep3 |
| 12w – 15w | Misoprostol: 400 – 600 mcg PV/BU for 30- 90 min or
(Dilapan-S®) +/- miso |
|
| 16w | Misoprostol: 400 – 600 mcg PV/Buccal for 90 min – 3 hour or (Dilapan-S®) +/- miso | Day 1: 200 mg Mifepristone PO only OR Day 1: Mife +/- (Dilapan-S® +/- Laminaria) +/- Miso (on day 2) |
| 17w | Misoprostol: 400 – 600 mcg PV/Buccal for 2 – 4 hour or
(Dilapan-S®) +/- miso |
Day 1: 200 mg Mifepristone PO, Day 2: misoprostol ORDay 1: Mife + (Dilapan-S®) +/- Laminaria, +/- Miso (on day 2) |
| 18w – 19w | Misoprostol: 400 – 600 mcg PV/Buccal for 4 hour and (Dilapan-S®) +/- lams for 4 hours or transcervical catheter until dilation achieved | Day 1: 200 mg Mifepristone PO, Day 2: Misoprostol ORDay 1: Mife + (Dilapan-S®) +/- Laminaria, +/- miso (on day 2) |
|
¹Some providers consider shorter wait times after misoprostol dosing for history of prior vaginal delivery and no prior cesarean delivery. ²>18 weeks, the use of adjunctive Mife and/or Miso should be strongly considered along with osmotic dilator insertion/transcervical catheter when cervical preparation in less than 24 h is needed (Ralph 2019). ³>Travel and logistics, as well as clinical setting, should be incorporated into decisions about cervical prep timing. Most procedures can be accomplished with same-day cervical prep options for gestational durations <18w. |
||
Deciding whether people may leave the health center area after cervical preparation is initiated will depend on each health center and abortion seeker. Pain management, anxiolytics, and antiemetics should be offered as needed. Consider allowing the person to leave the health center during cervical prep wait time if the person:
- is comfortable and experiencing no more than scant bleeding
- has normal vital signs
- has no IV in place
- has not received opioids or benzodiazepines
- has no history of cesarean delivery or current placenta previa.
While use of misoprostol > 14 weeks in people with a history of previous cesarean section slightly increases the risk of uterine rupture, the risk is < 0.3% in a systematic review (Goyal 2009). This risk may be acceptable to both patients and providers.