PREGNANCY CONFIRMATION AND DATING
Pregnancy Tests
- High sensitivity urine pregnancy test (HSPT):
- Widely available, inexpensive urine tests available over the counter or in health centers.
- Simple, accurate qualitative test detecting hCG at concentrations of 10-25 mIU/mL.
- Usually positive by cycle day 32-35 (95% of pregnancies).
- May remain positive for 4 or more weeks following an uncomplicated abortion.
- May be used to assess for completion 5-6 weeks after medication abortion.
- Serum quantitative hCG test:
- Available in healthcare settings with an order from a clinician and by self-ordering at labs like Quest and Labcorp.
- Detects serum levels of hCG as low as 2-10 mIU/mL.
- Not used to assess estimated gestational duration (EGD) as range in level is wide & variable for any GD.
- Serial measurements often used to evaluate suspected ectopic, abortion completion (i.e. when products of conception are not visualized following procedural abortion or for medication abortion), or in management of gestational trophoblastic disease (GTD)/molar pregnancy (Horowitz 2021, Soper 2021).
- Other hCG assays with limited availability and use in the U.S.:
- Low sensitivity urine test: detects hCG of at least 1000-2000 mIU/mL (Whitehouse 2022).
- Multi-level pregnancy test (MLPT): a urine test measuring hCG levels within specified ranges (Shochet 2020), rare availability outside research settings.
Last Menstrual Period (LMP)
- Clinicians can confidently use clinical dating or duration (LMP +/- exam) for most people with known LMP to assess eligibility for abortion type and setting.
- First day of LMP alone can accurately provide EGD, with low rates of under- or over- estimation to 11 weeks LMP (+/- 1 week of certainty) (ACOG 2017, Godfrey 2021, Ipas 2023, Kapp 2020, Macaulay 2019, Raymond 2015, Schonberg 2014, Simons 2024).
- In settings with limited US access, LMP maintains high accuracy ≤ 13 weeks (Ipas 2023, Kapp 2020, WHO 2022).
- Additional health history questions (Are you >10 weeks pregnant? Have you missed >2 periods? Are you >2 months pregnant?) may increase the accuracy of gestational duration and sensitivity of self assessment for medication abortion eligibility (Kerestes 2024, Ralph 2021).
- Using health history (including menstrual regularity, recent hormonal contraceptive use, along with LMP dating for medication abortion has high rates of safety and efficacy (Moseson 2022, Upadhyay 2022).
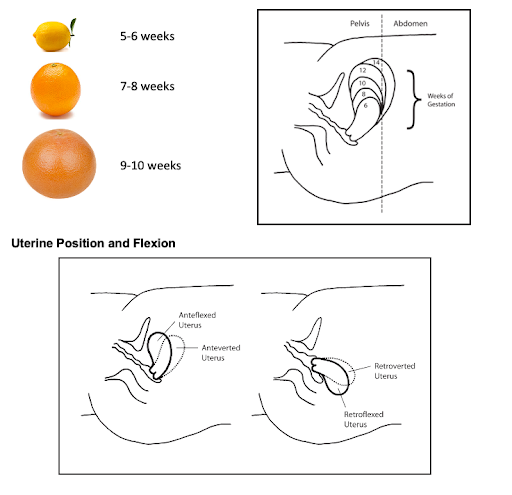
Bimanual Exam
The BME may improve assessment of gestational duration with unknown LMP and may help assess uterine angle for procedural safety (Bialy 2024). While it is important for trainees to become comfortable assessing gestational duration based on exam, trainers and trainees alike must center patient autonomy and preferences as essential components of trauma responsive care. Beyond obtaining consent for the BME itself and trainee involvement in care, it is valuable to consider consent an ongoing process throughout procedural care (Tillman 2020).
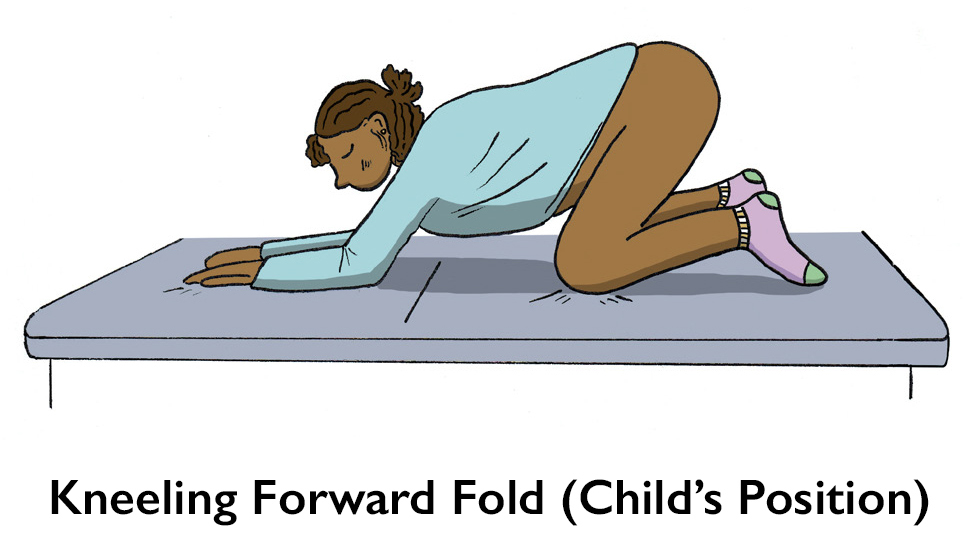
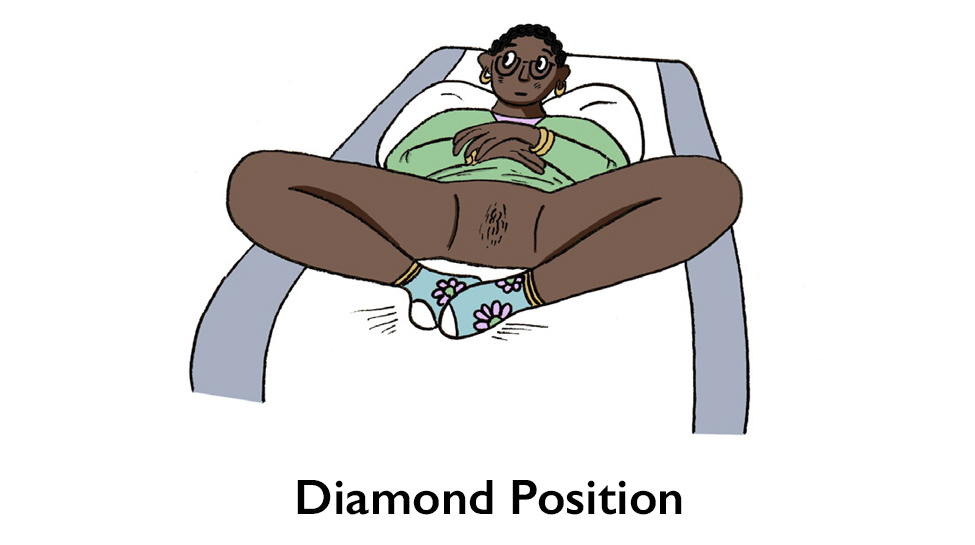
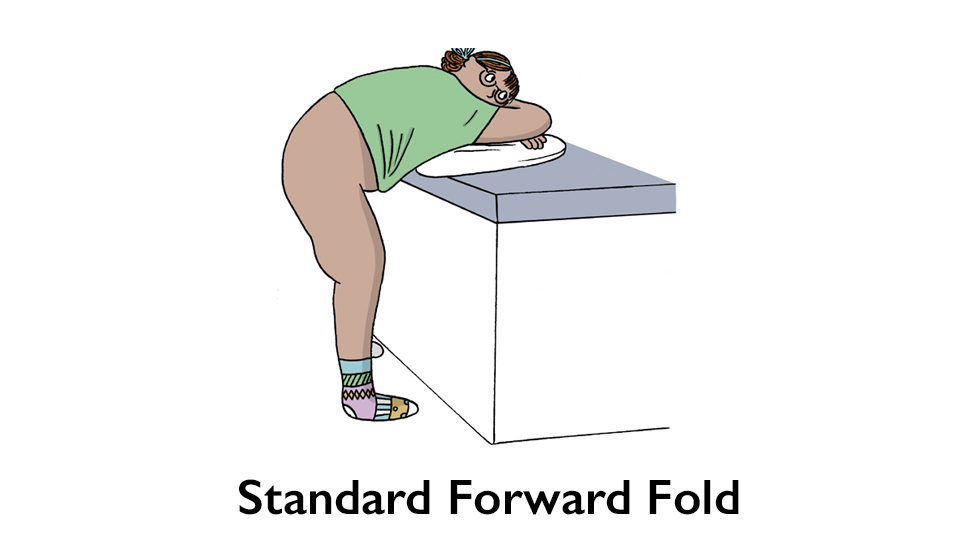
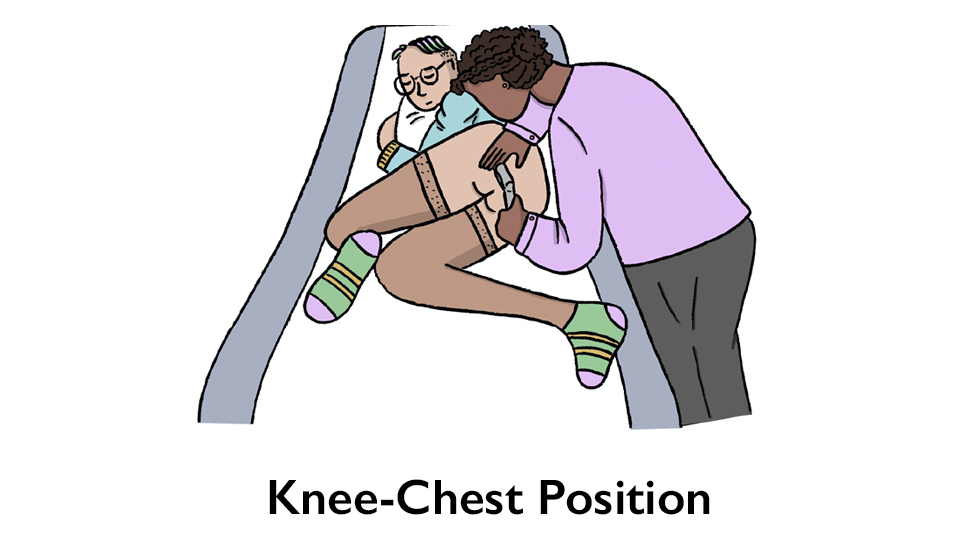
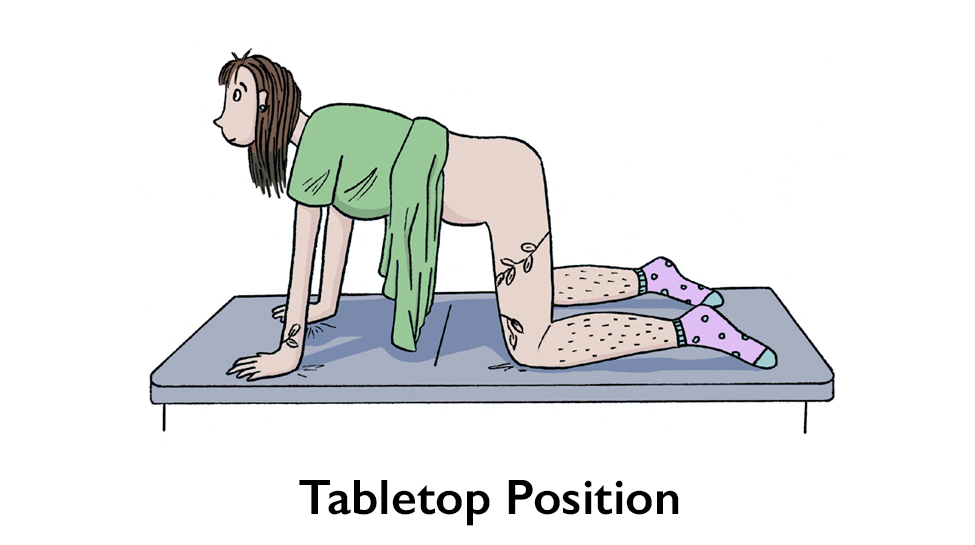
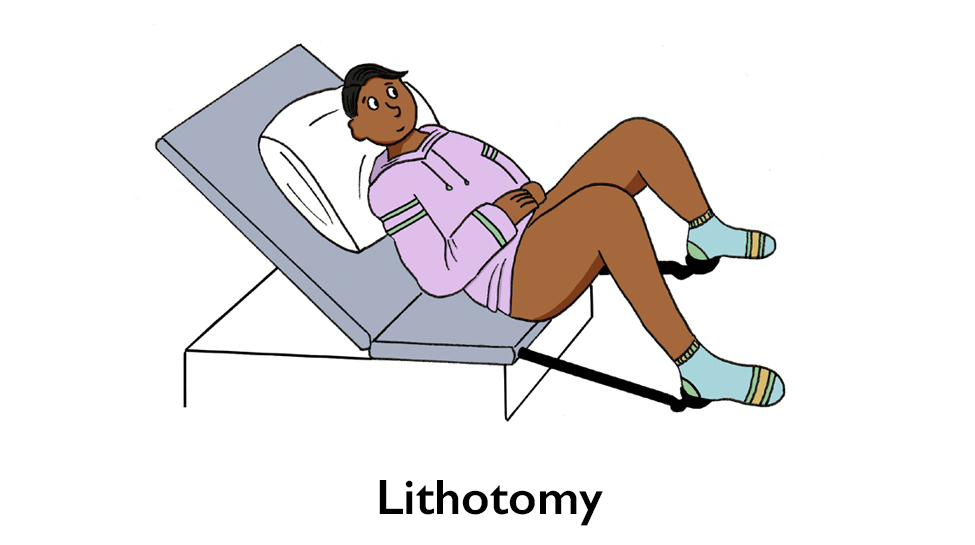
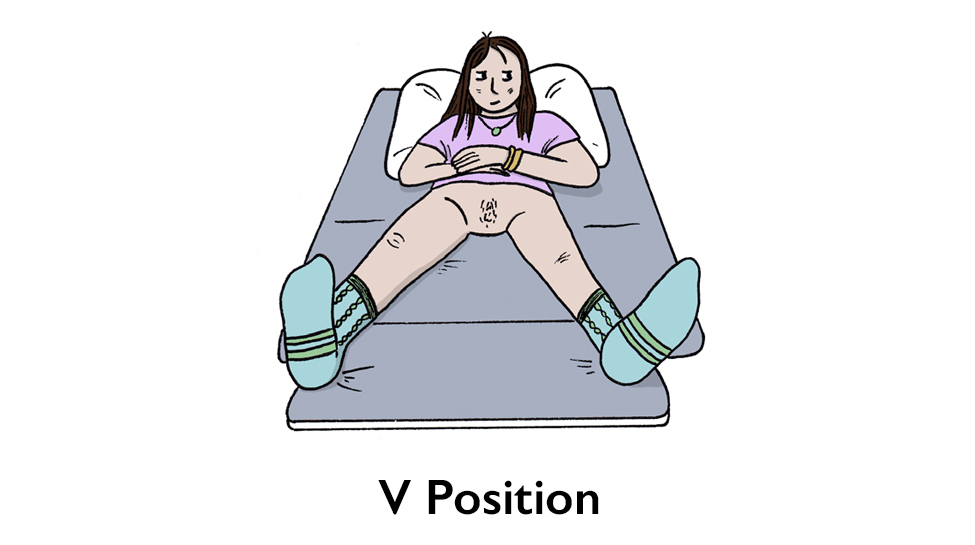
Alternative Exam Positions
Multiple exam positions are available to help facilitate person-centered care (RHAP 2025). Consider variables including mobility, availability of support people or adaptive equipment, duration of exam/procedure, trauma history, and patient preferences. While various positions can be used for pelvic exams, intrauterine procedures usually necessitate lithotomy or modified lithotomy position to provide mobility of the speculum and instrument angles. Note: covers/drapes not shown to better demonstrate positions.