MANAGING COMPLICATIONS
BETWEEN 14 – 18 WEEKS
While overall rates of serious complications remain low with procedural abortion between 14 to18 weeks, complication rates gradually increase with advancing gestation (NASEM 2018, Kapp 2020, Grimes 1984). Between 14 to18 weeks gestation, most complications are similar to those at <14 weeks (SFP 2023; See Ch 6: Managing Complications), with the following nuances:
| COMPLICATIONS | CLINICAL PRESENTATION | PREVENTION AND MANAGEMENT TIPS or OPTIONS | OCCURENCE RATE |
Procedural Abortion > 14 weeks |
|||
| Hemorrhage due to Atony | • EBL > 500 ml = hemorrhage
• Review risk stratification and etiologies (4Ts) |
• Ensure good uterine tone without ongoing blood flow prior to removing instruments.
• If LUS still appears dilated, suggesting atony, immediately provide vigorous bi-directional bimanual massage with ball of gauze in ring forceps in posterior fornix and low abdominal compression by free hand or US probe. • Watch until the tone returns, performing standard 6T management steps and uterotonics • Consider TXA 1000 mg (in 100cc NS) run over 10 mins, and / or Oxytocin 10 units IM, or 20-40 units in 1L NS IV. |
0.07 – 0.4 % |
| Hematometra
(Accumulation of blood in uterus following procedure) |
Immediate:
Delayed:
|
Prompt uterine aspiration of blood offers immediate relief
Uterotonic medications post aspi- ration:
|
1.1 – 2.2 % |
| Hemorrhage due to Arteriovenous malformation (AVM) | • Rare, life-threatening source of profuse bleeding uncontrolled despite usual measures | • Review 6T bleeding management steps See Ch 6. If no resolution, apply tamponade with foley bulb or vaginal packing and transport for embolization/cautery | Rare; case reports |
| Cervical laceration/trauma | Low/Anterior/endocerv tear:
High cervical tear
|
|
0.8% early 2nd trimester with lams + dilation |
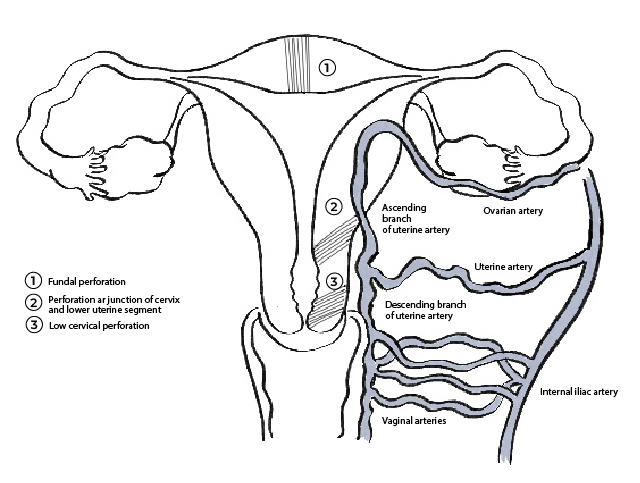
| Uterine perforation
(See Figure 7) |
Instruments pass deeper than expected by gestation and pelvic exam Person may feel sudden sharp pain; may be painlessRisk factors:
|
Stop procedure:
–Indications for transfer include -Free fluid seen on US -Pregnancy tissue outside of uterus in abdomen seen on US -Visualization of bowel in uterus, cannula or collection of POCs -Heavy bleeding diagnosed (from cervix) or suspected (intraabdominal) -VS unstable Inability to complete the procedure after pregnancy disrupted after 13 weeks –Depending on degree of perforation, experienced providers have safely explored uterus and completed procedure under US guidance
uterus and control bleeding
|
0.02 – 0.07% |
| Partial or Complete Placenta Previa | People with gestations > 14 weeks with history of c-section and complete previa at high risk for PAS (see below) |
-If possible remove placenta first either with forceps or aspiration. |
0.05% of pregnancies
In setting of previa, 1-5 x higher risk with increasing # c-sections
|
| Placenta Accreta Spectrum (PAS) |
|
• See US and Doppler screening
• Refer people with PAS to multi-disciplinary center, for procedure in an OR with transfusion services and surgical management to mitigate bleeding risk
|
0.07-0.2% of pregnancies
0.3% if previous c-section |
| MAB > 14 weeks | |||
| Retained Placenta after fetal expulsion | Delay in placental delivery after fetal expulsion |
|
12%–33%
|
 |
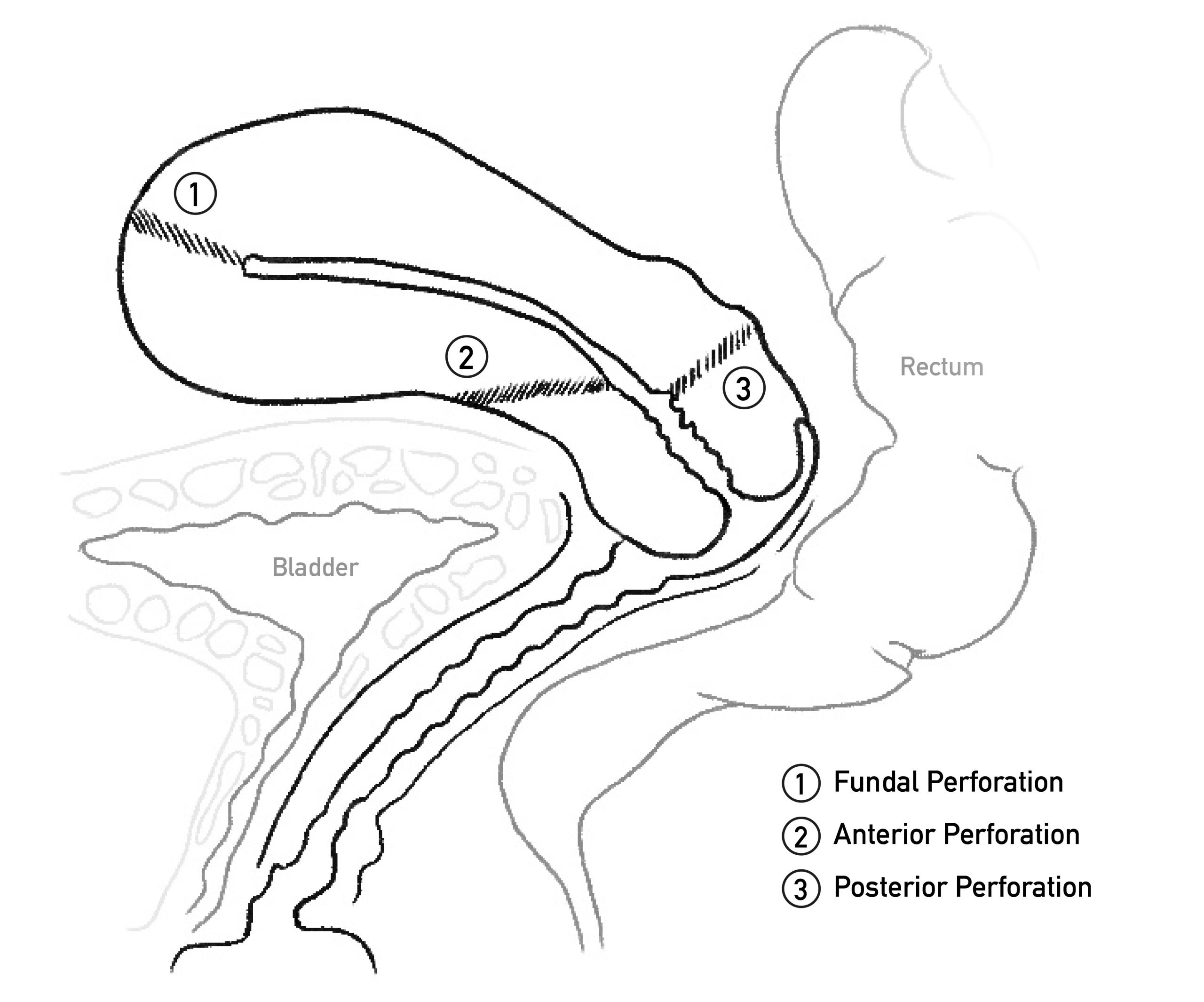 |
Figure 7. Possible sites of uterine perforation: fundal (lateral regions are more vascular than midline), at internal os (often due to overstretching junction of cervix and lower uterine segment, injuring ascending branches of uterine artery), and low cervical perforation (can injure descending branches of uterine artery).
CONCLUSION
With challenges to abortion access globally, providers have an opportunity to consider both traditional methods of training and non-traditional methods of expanding access to care. While in-person training with an experienced provider remains the gold standard for expanding abortion skills, alternate methods of increasing provision may include simulation models and incremental increases in gestational duration using a gradual stepwise approach with informed patient consent. Incremental expansion in gestational duration for both procedural and medication abortion can improve access to abortion, reduce the need for travel and stress, while minimizing fragmentation of care. People with higher-risk pregnancies can be managed or referred to a higher level of care depending on provider skills and regional resources. Depending on legal constraints, providers may use formal or informal referral networks, and/or hotlines for second opinions. Clinicians play an instrumental role in setting the tone of care, helping staff with later abortion values exploration, normalizing the possibility of seeing more complex medical cases, and expanding the services offered.
Appendix A: Instruments and Supplies for Abortion > 14 weeks(Beyond standard equipment for aspiration < 14 weeks) |
|
| Appendix B. Dilation, Cannula Size, and Recommended Forceps by Gestation | |||
| Gestation | Dilation | Cannula | Recommended Forceps |
| < 14w | 14 Denniston
43 Pratt |
14 curved
May follow with smaller cannula |
None
(If needed Ring, Hern, Van Lyth) |
| 14w-14w6d | 43-45 Pratt | Either 14 curved or
12 curved w/ forceps May follow with smaller cannula |
None
(If needed Ring, Hern Van Lyth) |
| 15w – 15w6d | 45-47 Pratt | Either 15 curved or 12 curved w/ forceps
May follow with smaller cannula |
None or Small finks (or Ring, Hern Van Lyth) |
| 16w – 16w6d | 49 Pratt | Either 12, 14 or 16 curved w/ forceps
May follow with smaller cannula |
Small Finks (or Regular Finks or Sophers) |
| 17w – 17w6d | 49/51 Pratt | Either 16 curved w/ forceps or 12 curved and forceps
May follow with 8 flexible |
Small finks (or Regular Finks or Sophers) |
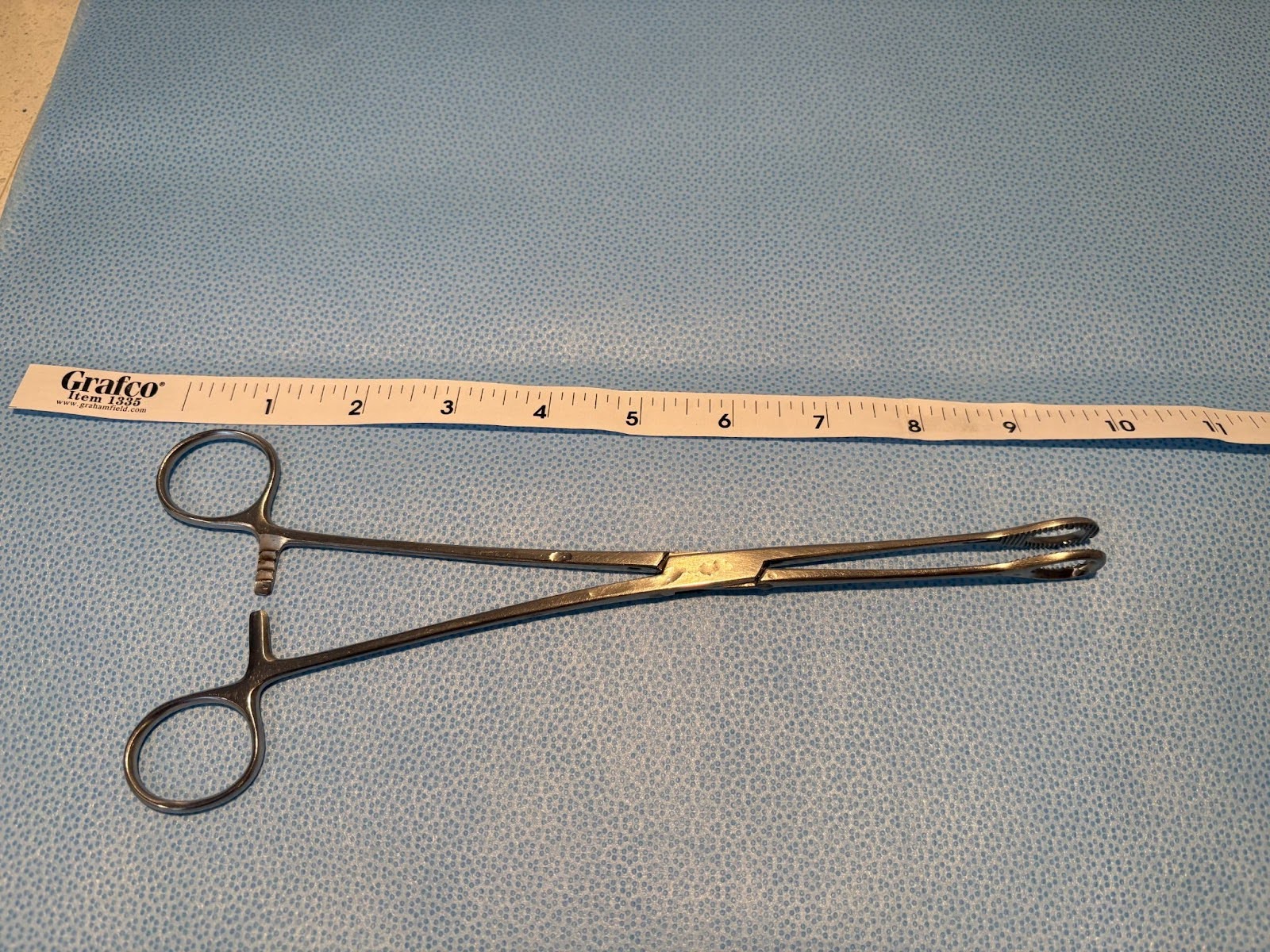
*Pros/Cons of surgical instruments are personal. Instrument choice is often dependent on provider preference, availability of instruments, patient anatomy, and gestation duration. Generally it is good practice to use the smallest forceps that will comfortably complete the procedure (smaller head and larger teeth is ideal). Nuances (such as presence/absence of locking or ratcheting mechanism, curve of handles, and size of handle rings) become personal preferences with practice and exposure. Photo credit: Drs. J. McDonald and S. Mischell