PAIN MANAGEMENT
Pain perception during uterine aspiration is a complex phenomenon influenced by physical and psychosocial elements and can vary considerably between individuals, though uterine aspiration is almost universally painful without medication. Fear of the procedure is predictive of less satisfaction with local anesthesia for pain control (Allen 2024). History of trauma, as well as experiences of structural factors—including systems of oppression and racism—also contribute to pain perception (Pace 2023). Despite similar pain scores, studies show that Black Americans are undertreated for pain relative to White Americans in medical settings (Hoffman 2016), including receiving lower doses of midazolam for aspiration procedures (Pace 2023).
Implicit and explicit biases regarding age, race, body size, substance use disorder, and use of medication for opioid use disorder have been shown to contribute to clinician perception of a person’s pain and subsequent treatment decisions regarding pain management (ACOG 2025, Mende-Siedlecki 2019, Sabin 2020). A meta-analysis on pain management including 20 years of data found that Black patients were 22% less likely to receive pain management than White patients and the size of the difference was sufficiently large to raise quality and safety concerns (Meghani 2012). Intentional efforts are needed to reduce disparities in pain assessment and treatment. Clinicians should work to identify and minimize their own biases, which may include unlearning prior practices and universally prioritizing pain management.
The table below summarizes research on factors associated with pain during uterine aspiration. In the multivariable analyses, no single factor predicted procedure-associated pain (Pace 2023, Singh 2008) and every person deserves a discussion of and recommendation for pain management options.
TABLE 1. FACTORS ASSOCIATED WITH PAIN DURING UTERINE ASPIRATION |
|||
|---|---|---|---|
| Increased Pain | Decreased Pain | Conflicting Results | Not Strongly Associated |
|
|
|
|
Nonpharmacologic Pain Management
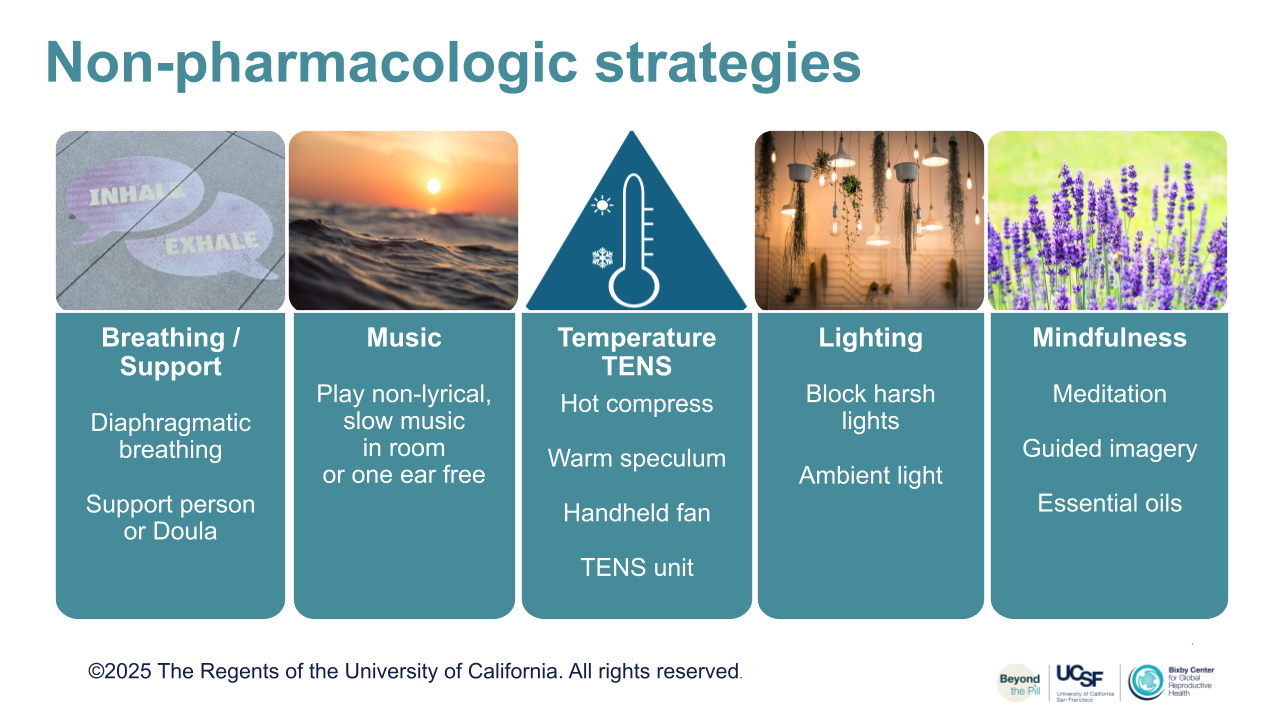
Many people have anxiety about anticipated pain. Abortion stigma also contributes to this anxiety. Establishing rapport and informing the person they are in control during the procedure, can help reduce anxiety over anticipated pain and increase their agency during an experience when they may feel powerless. A multimodal approach to pain and anxiety management can include trauma-responsive care (ACOG 2025, Liu 2021; see Ch 6 section), distraction, an emotional support person, aromatherapy, relaxation exercises, and administration of local anesthesia with cervical block and preprocedural medications (SFP 2018). Supportive verbal communication, including distraction and so-called “vocal local” or “verbicaine,” can play a role in reducing anxiety and pain. Guiding people to take slow, deep, regular breaths can reduce anxiety, avoid hyperventilation, and also increase sense of control. Clinicians can acknowledge the possibility of pain while offering strategies to manage it, such as:
“It is normal to be worried, and some people are surprised that the procedure is faster and more tolerable than expected. Pain can vary, but slow deep breathing helps, and I’ll give you some numbing medicine and be as gentle as possible.”
Using trauma-responsive, neutral language to talk about bodies or medical equipment can increase a sense of safety, empowerment and trust (Ely 2017). Triggering or pain-associated words at the time of stimulation increases pain in a study incorporating functional MRI (Ritter 2019). Encourage the person to release their hips into the table instead of pulling away and tightening; wait for this before placing a speculum. Guided imagery can also decrease anxiety and analgesic requirements for those undergoing a procedure (Gonzales 2010). Consider encouraging people to recall a favorite place or activity during the procedure. Relaxing images or mobiles above the exam table have also been used to decrease pain and anxiety during gynecologic procedures (Carwile 2014). Playing music in the room may be helpful with anxiety and satisfaction, but was not shown to decrease pain, especially with both ears covered (Cepeda 2006, Guerrero 2012, Wu 2012). A heating pad or hot water bottle may be helpful during the procedure, in recovery, and at home, as it has been shown to be beneficial with dysmenorrhea. A support person familiar to the person seeking care can also improve the abortion experience (Altshuler 2021). For additional considerations, see the Contraceptive Pearl (Ti 2022).
Choice of Pain Management Methods
Discussion of pain management options should be reviewed as part of the informed consent process, including the range of possible experiences, available options for pain management, and their risks and benefits. If someone has a strong preference for an option your facility does not offer, an appropriate referral should be provided.
Lactating people should be offered pain control the same as non lactating people and should receive reassurance it is safe. It is acceptable to breast/chest feed once awake if sedation was received. Tramadol and codeine should be avoided in lactating people when possible due to variable metabolism and potential sedating effects on the infant (ABM 2017, ASA 2024, FDA 2024).
Premedication with NSAIDs has been shown to decrease pain during and after the procedure and has few contraindications or side effects (SFP 2018, Ipas 2021). Some people choose NSAIDs in addition to local anesthesia to be more alert, have shorter recovery, and to be able to drive themselves home. Premedication with acetaminophen 1000 mg in addition is supported by evidence outside of abortion (Simpson 2019) and by one study comparing it to lidocaine (Açmaz 2013).
Oral anxiolytics such as lorazepam 2 mg have not been shown to be effective in pain reduction but reduce anxiety which is very connected to pain, and may help make people more comfortable (Wiebe 2003). If providing oral benzodiazepines, consider sublingual dosing to overcome the delayed stomach emptying with anxiety.
Others may choose more sedating options to reduce pain, anxiety, and to induce some degree of amnesia. Oral opiate analgesics have shown minimal effect on pain compared to placebo and cause more side effects including nausea (Micks 2012). Moderate sedation with IV fentanyl and midazolam or deep sedation with propofol may be offered in some settings for people who request more analgesia. Some medical conditions, need for cardiopulmonary monitoring, or facility limitations may preclude these options in an outpatient setting (Ipas 2021).
IV Ketamine, an analgesic and sedative that can be administered by multiple routes, is commonly used in outpatient procedures. It has been shown to be non-inferior to fentanyl for patient satisfaction in abortion procedures (Chin 2022, Slomski 2022). It can be used to provide short-term procedural analgesia, sedation, and amnesia by inducing a dissociative state without the respiratory and cardiovascular depression risk associated with IV opioids, and may reduce the overall opioid dose required when used with opioids (Nelles-McGee 2024). It may provide more optimal pain management in settings where continuous cardiorespiratory monitoring is unavailable, as spontaneous respirations and upper airway reflexes are maintained (Nelles-McGee 2024). Lower, subdissociative doses (10-20 mg IV) of ketamine may be used alongside IV benzodiazepine (given first, to avoid inducing a dysphoric emergence phenomenon). Once the critical dose threshold is reached (approximately 0.5 mg/kg), the characteristic dissociative state appears (Rosenbaum 2024). There is no reversal agent available or needed for ketamine; if dissociative dysphoria occurs it can be treated with a benzodiazepine.
Providing Effective Local Anesthesia
While no local modality has been found to completely block pain during intrauterine procedures, perhaps due to the complexity of the uterine nerve plexus, the cervix is a small area of tissue where a near complete block is possible with enough local anesthesia. Studies also demonstrate that local anesthesia is absorbed into the uterus from the cervix over time. Adding more local anesthesia in areas not reached initially if someone has pain with dilation can be useful.
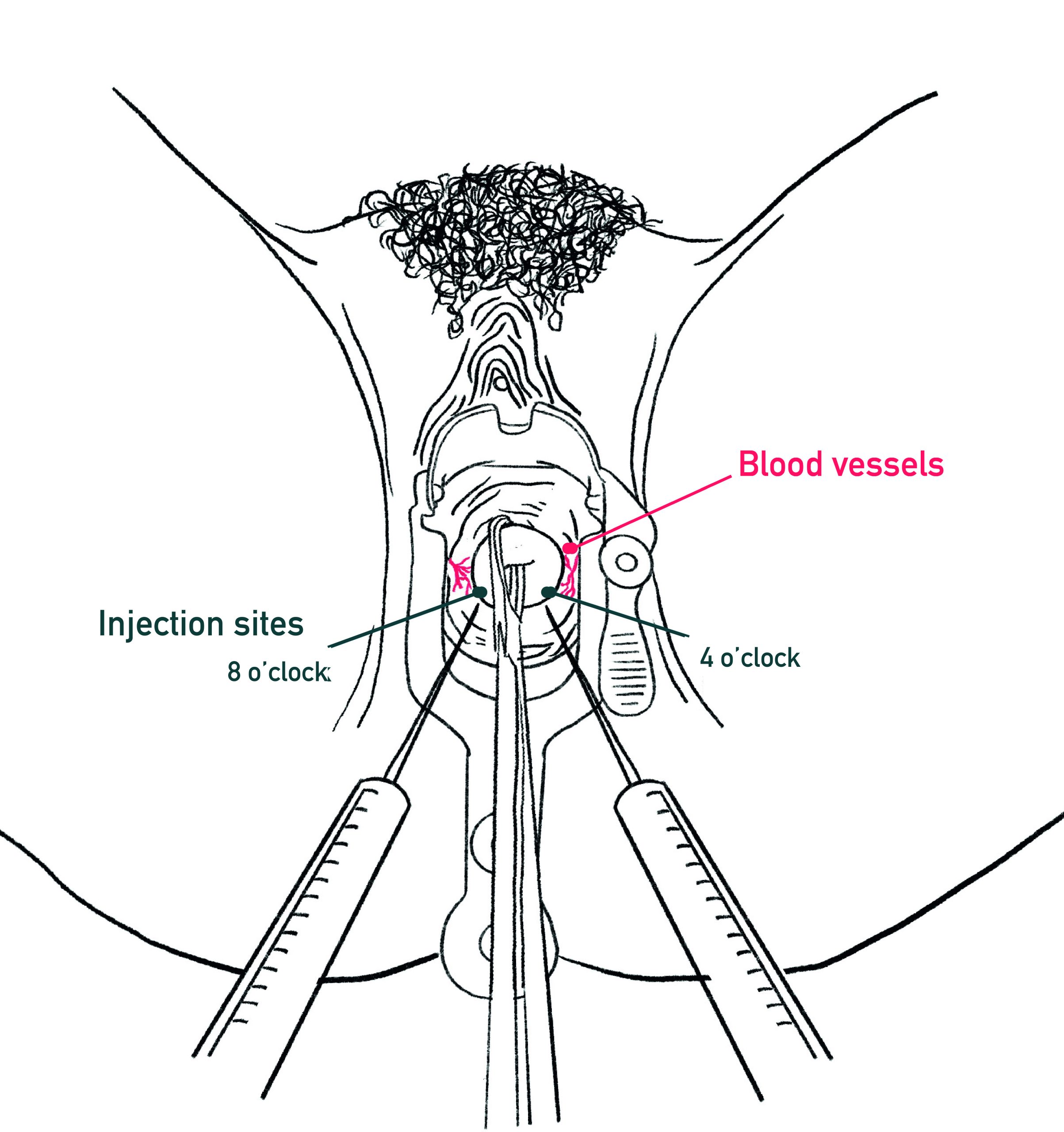
Local anesthesia options include paracervical block (PCB), intracervical block, and cervical topical lidocaine. A PCB impedes nerve impulses and volume causes tissue distention, separating nerve endings, providing some analgesic effect. Below are techniques and pitfalls of PCB preparation and injection, supported by a recent comprehensive review (Renner 2024; unless otherwise noted).
|
|
|
| One approach: inject 2 mL at 12 o’clock for the tenaculum (placed vertically which some prefer), and then 18 ml between 4 and 8 o’clock as depicted above to target paracervical innervation, avoiding vessels at 3 & 9 o’clock. |
- Paracervical block (PCB) can effectively reduce pain during uterine aspiration, though injection can be painful.
- Pain with injection may be improved with: topical lidocaine, slow injection, starting injection superficially, and using smaller gauge needles.
- Tenaculum site intracervical block is mixed, but supported by evidence in other intrauterine procedures (CDC SPR 2024), though topical anesthetic is also effective.
- Pain scores are improved with 20 ml 1% lidocaine PCB compared with 10 ml; may use up to max of 30 ml 1% lidocaine during procedural abortion.
- A 2-site PCB is likely as effective as a 4-point PCB. With a goal to block cervical pain as much as possible, more injections into the stroma may be needed if fewer are unsuccessful. Consider directing injections more medially (rather than the lateral vaginal fornices).
- A 1.5-cm deep injection is as effective as a 3-cm deep injection.
- Buffering lidocaine increases anesthetic cellular absorption and onset, and is used in many specialties. Some studies show decreased pain (SFP 2018, Wiebe 1995).
- No clear wait time between PCB and dilation has been identified, although local anesthetic takes a few minutes to fully work (longer for fibers that transmit dull pain), and waiting may benefit some individuals. The effect of cough technique during injection shows minimal effect with similar procedures (Lambert 2020).
- No evidence suggests one anesthetic is superior; options are reviewed in Table 2 below.
- Saline alone is less effective than lidocaine (Chanrachakul 2001); can be used for those with anesthetic allergy, or to supplement volume of anesthetic blocks.
- Higher concentrations of topical lidocaine (4-10% spray and 5% EMLA) clinician administered show benefit for uterine procedures. Some clinicians test with light stimulation, adding additional anesthesia if needed.
- Pre-procedure self-administration of 2% lidocaine gel is likely to help with speculum, tenaculum and block pain and can be an additional approach to pain control (Conti 2016).
- Some clinicians test with light stimulation, adding additional anesthesia as needed, and ensuring a multi-modal approach to pain management.
Tips to Minimize Systemic Absorption
The most studied dose of injected lidocaine in pregnancy is 200 mg [achieved for example, by giving a 20 ml PCB with 1% lidocaine (10 mg/ml)]. A maximum dose of 300 mg has been found to be safe, but with more systemic side effects (Edelman 2006). With inadvertent IV injection, people may experience perioral tingling, dizziness, tinnitus, metallic taste or irregular/slow pulse. At higher concentrations, they may have muscular twitching, seizure, cardiac arrhythmias, unconsciousness, and even death (Torp 2022).
- Minimize direct intravascular injection by avoiding uterine arteries at 3 and 9 o’clock or aspirating prior to injection
- Minimize excessive anesthetic dosing
- Start superficially, moving the needle while injecting to 1.5 cm and/or aspirate before injecting
- Use a dilute concentration (e.g. using 0.5% lidocaine or diluting with saline)
- Consider a vasoconstrictor (i.e. vasopressin 3 to 5 units) mixed with the anesthetic to slow systemic absorption
| TABLE 2: LOCAL ANESTHETIC PROPERTIES FOR PARACERVICAL BLOCK |
||||
|---|---|---|---|---|
| Generic (Trade) | Potency | Onset | Duration | Max Dose (mg) without episode |
| Bupivicaine (Marcaine) | Strong | Moderate (up to 20 min) | Long (3-6 h) | 175 mg |
| Lidocaine (Xylocaine) | Medium | Fast (4-7 min) | Moderate (1-2 h) (~3 h with epinephrine) | 300 mg |
| Mepivicaine (Carbocaine) | Medium | Fast (4-7 min) | Moderate (3 h) | 400 mg |
| Chloroprocaine (Nesacaine) | Weaker | Fastest (<1 min) | Short (30 min) | 800 mg |
Universal Precautions
To prevent transmission of blood-borne pathogens, universal precautions include:
- Glove and protective eye wear when working with body fluids (i.e. injection, procedure, handling of tissue or contaminated instruments) (CDC 2024).
- Avoid recapping contaminated needles and place sharps immediately in a puncture- resistant container for disposal (CDC 2024).
- For blood exposure, inform a supervisor, and consult National Clinicians’ Post-Exposure Prophylaxis Hotline.
Continuum of Sedation Level
Various approaches to pain management may be offered, depending on the clinical situation and resources. Below is a short summary of the levels of sedation, examples of medications used, and the associated risks. Note that ketamine produces a dissociative state that does not fall into the classic sedation continuum (ASA 2002).
|
TABLE 3: CONTINUUM OF LEVELS OF SEDATION WITH DIFFERENT ANESTHESIA |
|||||
|---|---|---|---|---|---|
| Level of Sedation | Example | Responsiveness | Airway | Spontaneous Ventilation |
Cardiovascular Function |
| Minimal (Anxiolysis) | Oral lorazepam and/or hydrocodone |
Normal response to verbal stimulation |
Unaffected | Usually adequate / May be affected | Unaffected |
| Dissociative | Ketamine | Dissociation
Eyes may remain open |
Unaffected | Unaffected | Usually maintained |
| Moderate “Conscious Sedation” | Fentanyl +/- Midazolam |
Purposeful response to verbal or tactile stimulation |
No intervention required | Usually Adequate | Usually maintained |
| Deep* | Propofol or higher doses of meds used for moderate sedation | Purposeful response to repeated or painful stimulation | Intervention may be required | May be inadequate | Usually maintained |
| General Anesthesia* | Propofol or other medications | Unarousable even with painful stimuli | Active airway management required | Frequently inadequate | May be impaired |
*These methods require licensed anesthesia clinicians (CRNA/anesthesiologist) to administer and monitor
Adapted from Continuum of Depth of Sedation: Definition of GA and levels of Sedation / Anesthesia, ASA 2024.
Monitoring Guidelines
- During moderate sedation, a person trained to monitor cardiorespiratory and level of consciousness must be present, other than the clinician.
- Moderate sedation may lead to deep sedation with hypoventilation, so the following respiratory support and monitoring should be provided (ASA 2024):
- Pulse oximetry should be used to enhance monitoring
- IV access should be maintained
- For people with severe systemic disease that could impact sedation or respiration, consider a higher level of care
- Some sites use routine oxygen administration based on limitations of O2 saturation monitoring (Al-Halawani 2023).
- When moderate sedation is used, monitoring must be of a degree that can be expected to detect the respiratory effects of the medications being used.
- The practitioner administering deep sedation or general anesthesia must be certified according to applicable local, hospital, and state requirements.
Consent Considerations Prior to Sedation
Informed consent should be completed prior to initiating sedating medications. If the individual is drowsy or unable to answer orientation questions, consider having them rest and reevaluate for capacity to provide consent. Substance use disorder history and use of MAT medications do not alter the informed consent process; in fact withdrawal symptoms may impede proper consent.
It is also important to use verbal consent throughout the procedure as is recommended with trauma responsive care.
Techniques for evaluating if someone is able to consent for a procedure include asking orientation questions and having them repeat information back after reviewing it, with the following key considerations of medical decision making capacity. Patients shouldmust be able to:
- demonstrate an understanding of risks, benefits and alternative options
- demonstrate an appreciation of benefits and risks
- show reasoning in making a decision
- communicate their choice
- See unique considerations see Ch 2: Considerations for Counseling Minors, and for people with intellectual disabilities or who are non-verbal, see Ch 2: Ensure Capacity to Consent.
Logistical Considerations of Sedation
Pre-sedation
While patients have traditionally been asked to be NPO (nothing per os) prior to surgical procedures with deep sedation to prevent aspiration of gastric contents, multiple studies support removing the fasting interval prior to procedural abortion with light to moderate sedation. Removing the NPO requirement decreases unpleasant symptoms (nausea, vomiting, dehydration) without an increase in anesthesia-related complications (SFP 2021, Cansino 2021, Wiebe 2013). Individuals do not have to be NPO for fentanyl and midazolam at doses usually used for moderate sedation, although 6 hours of NPO may still be required prior to deep sedation (NAF 2024, Wiebe 2013, Wilson 2009).
Post-sedation
People who receive moderate to deep sedation or ketamine need to be monitored in an adequately staffed and equipped area before they can be safely discharged from care. Until return to a responsive level of consciousness, periodic monitoring of oxygenation, ventilation, and circulation is recommended (Cansino 2021). Consider providing precautions with driving or performing potentially hazardous activities for up to 24 hours following moderate to deep sedation or ketamine administration. Use of ride share or taxi services are reasonable options for transportation home when an individual does not have a ride, or does not want others (family, friends) to know about their appointment.