PREGNANCY OF UNKNOWN LOCATION (PUL) EVALUATION
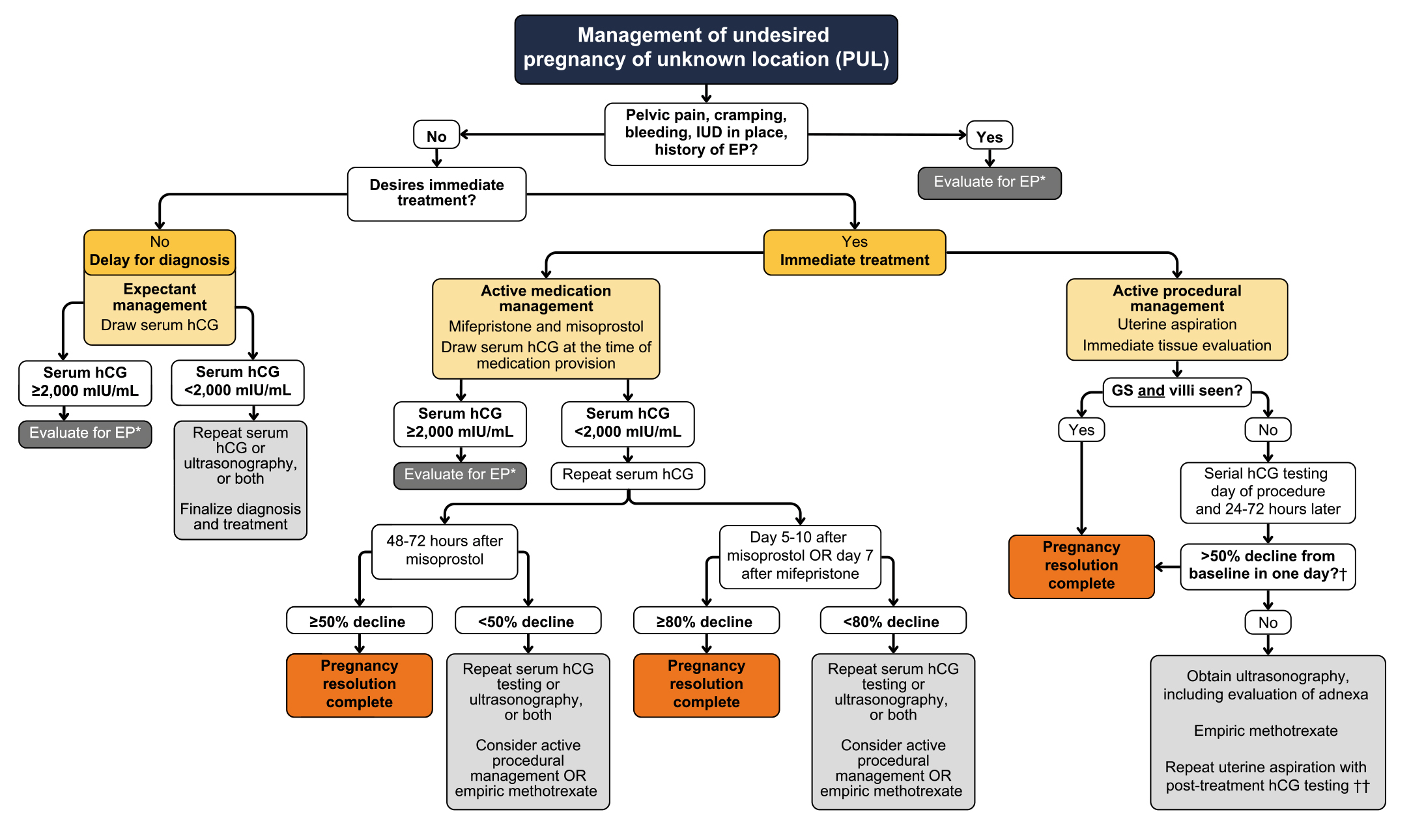
A person with a positive pregnancy test and no visible pregnancy on US is said to have a pregnancy of unknown location (PUL). Most PULs are early viable IUPs, but the differential diagnosis also includes EPL and ectopic pregnancy. Abortion can be provided as a part of a diagnostic algorithm for those not desiring to continue the pregnancy and definitive diagnosis should not delay a desired abortion. People presenting in early pregnancy with symptoms of bleeding and/or pain require evaluation for ectopic pregnancy according to local protocol, available resources, and clinical features. Evaluation may include US, serial hCGs, exam and/or diagnostic aspiration depending on patient preferences and clinical acuity. Referral for formal US and/or emergent evaluation and management may be indicated. As shown in the below table, management options will be influenced by clinical stability, patient preferences, and clinical findings including hCG levels (SFP 2025b).
Management of undesired pregnancy of unknown location. EP, ectopic pregnancy; GS, gestational sac; hCG, beta human chorionic gonadotropin, IUD, intrauterine device. *Includes ultrasonography evaluation of adnexa, initial serum hCG, and repeat hCG in 48 h. Refer to hospital for worsening pelvic pain, presyncope, syncope, or abnormal hCG rise. A suggested normal hCG rise at 48 h is at least 49% if initial value is less than 1500 mIU/mL; 40% if between 1500 and 3000 mIU/mL; 33% if greater than 3000 mIU/mL [42]. †In one study, minimum declines from baseline to day 1, day 2, and day 3 after procedural management via uterine aspiration were 56%, 77%, and 83% [76]. ††Further monitoring with serial hCG testing and expectant management may be considered on a case-by-case basis.
PUL Diagnosis
Ultrasound
- Discriminatory zone is the hCG level at which an IUP should be seen on US; a range of values have been cited in the literature and this level can vary based on probe type (TVUS vs TAUS), ultrasound machine characteristics, multiple gestations, use of assisted reproductive technologies, and other factors. A higher discriminatory zone should be used when a patient plans to continue the pregnancy to avoid potential interruption of a viable IUP (Larraín 2024).
- While some older studies have cited discriminatory zone values between 1000 and 2000 mIU, more recent studies have demonstrated that an intrauterine GS will be detected at an hCG level of 3510 to 3994 mIU per mL with 99% probability (Connolly 2013, Park 2023).
- A GS is rarely visualized in an early pregnancy <5 weeks from LMP, and therefore not expected. Follow-up US in 7 days with ectopic precautions is appropriate management for PUL <5 weeks, if not managed with diagnostic aspiration or medication abortion.
- Historically, a “doubling” of hCG every 48 hours was used as an indicator of a healthy developing IUP, more recent and larger studies show a broader range of normal particularly as pregnancies progress. hCG trends must be considered in the context of other considerations (multiple gestations, assisted reproductive technologies, variation between labs) as well as clinical findings (Larraín 2024). hCG rise over 2 days for normal pregnancies varies based on the initial level: for values <1500, 1500-3000, and >3000 the 2 day minimal rise is approximately 49%, 40%, and 33%, respectively (Barnhart 2016). The doubling time calculator may be helpful when assessing hCG trends.
- The rate of hCG increase and trends may be unpredictable, especially at low levels. Typically need 3 serial hCGs to establish a trend, ideally on days 0, 2, and 4 or 7.
- The minimum rate of decline expected for EPL depends on the initial hCG at presentation and is less predictable than rates of increase; slower rates of decline seen with lower starting hCG levels (Larraín 2024).
- Among people diagnosed with ectopic pregnancies:
- Most (90%) of ectopic pregnancies will present with hCG levels less than 3994 mIU per mL (Park 2023).
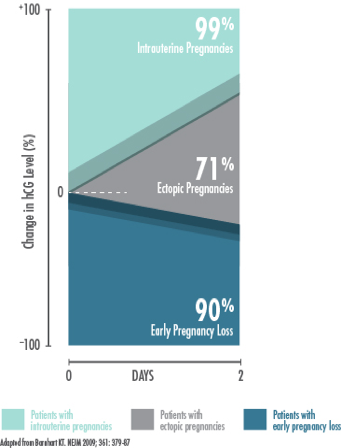
- Rate of hCG rise with ectopic is usually slower than expected for a viable IUP: the majority had serial hCG rise below normal range for a viable IUP (i.e. level rose < 35-53% in 2 days).
- For those with declining hCG, the rate of decline is usually slower than that expected for EPL.
- 21% of ectopics have a hCG rise similar to viable IUP and 8% have a decrease that is normal for EPL (Silva 2006).
- Use caution when following those in early pregnancy with possible symptoms of ectopic pregnancy, i.e. intermittent bleeding/spotting, pelvic pain.
- A “normal” rise or fall in levels is not sufficient to exclude ectopic and must be used in conjunction with other clinical data including symptoms, exam, US, and/or diagnostic aspiration.
PUL Diagnostic and Management Options
A person-centered approach, prioritizing desired pregnancy outcome, can be safely used to guide decision-making and approach to managing a PUL (Flynn 2020, Larraín 2024). Management options may be impacted by patient preference, available resources, breastfeeding status (in case of methotrexate), legal considerations, risk of criminalization, and need to travel for follow-up care.
Management options for those planning abortion include:
- Medication Abortion: <9 weeks MAB protocols may be safely used; clinicians should provide ectopic precautions & trend serum hCG with close follow-up to confirm completion (Brandell 2024, Goldberg 2022, SFP 2025b). Clinicians should not await visible pregnancy on US prior to MAB initiation. While mifepristone and misoprostol have not been confirmed to treat ectopic pregnancies, they will not cause harm nor interact with treatments for ectopic, should additional management be needed.
- Diagnostic Uterine Aspiration: can be offered at the same visit as PUL identification, providing a quicker diagnosis and resolution which may be desirable for some (Borchert 2023). If pregnancy tissue (GS or villi) is found in aspirate, an ectopic pregnancy is ruled out. If GS and villi identified, management is complete. If no pregnancy tissue or only villi is identified, review ectopic precautions, collect and trend hCG with repeat hCG in 24-48 hours until able to confirm diagnosis of completed abortion or ectopic pregnancy. Treatment or referral for ectopic pregnancy is warranted if symptoms develop (heavy bleeding, severe pelvic pain, shoulder pain or dizziness) or if hCG does not drop by at least 50% in 24-48 hours. Consider local resources when escalating care (i.e. avoid referral to hospitals with restrictive policies (if possible).
- Methotrexate (MTX): MTX (50 mg/m2 IM) can be effective in treating early ectopic pregnancy when the diagnosis of IUP or EPL cannot be confirmed (persistent PUL) if criteria are met. Managing a persistent PUL with MTX or uterine aspiration is more likely to result in a successful pregnancy resolution compared to expectant management (Barnhart 2021). Success is determined using serial hCG testing, clinical exams and progression of signs and symptoms (Seeber 2006). Lactating individuals should be advised to avoid breastfeeding for 24 hours after each dose of methotrexate (“pump and dump”).
Management for those planning to continue pregnancy:
- Serial hCG and/or US to continue evaluation for diagnosis of IUP, EPL or ectopic.
- If EPL or ectopic is conclusively diagnosed, offer appropriate management and/or referral (see Chapter 8 “Management Options For EPL”) or PUL / Ectopic Pregnancy Workup and Management Protocols.