PREGNANCY OPTIONS COUNSELING TECHNIQUES
Adapted from: RHAP Options Counseling 2023 & Perrucci A. Options Counseling 2012
When providing pregnancy test results, be prepared to encounter and respond empathetically to the full range of reactions a person may have. Some people will be surprised while others are expecting the result. People may feel a spectrum of emotions, including sadness, happiness, guilt, conflict, or no emotion related to their pregnancy. It is important to avoid assuming that an abortion itself will be a sad experience. Some expressions of sadness may be about related life circumstances, with ultimate feelings of relief (Rocca 2015). Relief is the most common emotion expressed 1 week and 5 years post-abortion, and the overwhelming majority continue to feel it was the right decision for them (Rocca 2020).
Our role in options counseling is to listen, present options, and provide appropriate decision support, as needed (Perrucci 2012). When providing positive pregnancy test results:
- Be explicit: “Your pregnancy test came back positive, which means you are pregnant.”
- Avoid assuming how someone will react.
- Allow time for processing the information.
- Use open-ended questions like,“How do you feel about this result?”
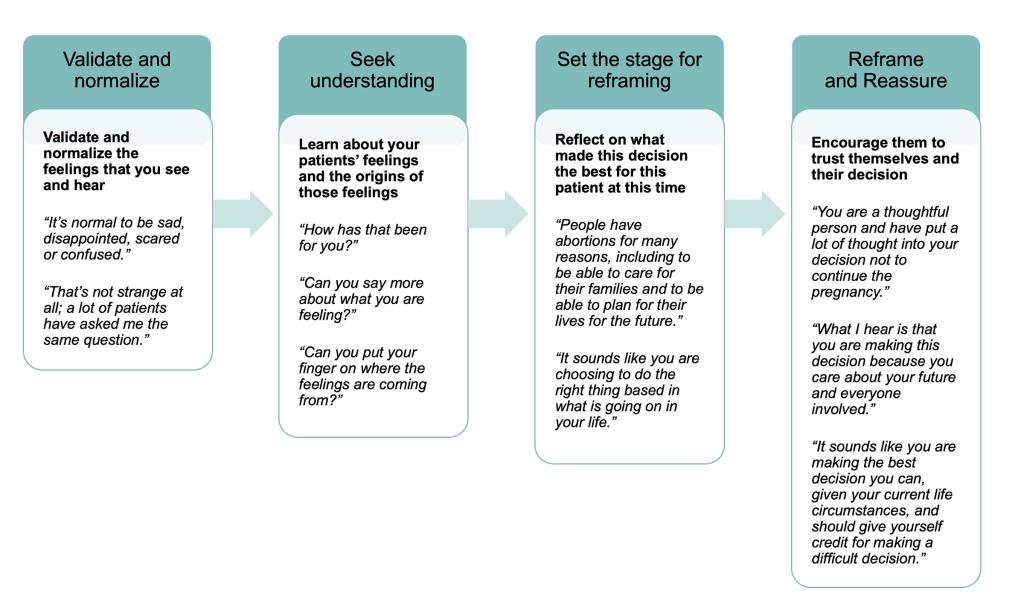
Image: Counseling Framework (Perrucci 2012) which may assist in your counseling conversations.
When Someone Is Sure of Their Decision
When the decision to continue the pregnancy or have an abortion is clear, a person won’t need full options counseling, and you can move to planning the next steps. Although you may use language like “choice,” a person’s pregnancy outcome may not be experienced as a choice but the only mechanism of upholding bodily autonomy and/or safety. In a society in which support for parenting is limited at best, the decision to end a pregnancy also may not feel like a choice.
When Someone Is Undecided
For those who are less sure, offer information on all pregnancy options, including any time constraints on when they need to decide in order to have access to each option. People were significantly more satisfied with their pregnancy counseling experience when their provider non-directively discussed all options, including abortion, which stands in contrast to regulations that restrict discussion of all options (Nobel 2022).
Ask questions (such as those in the counseling framework above) in a non-directive manner, and provide reassurance. These conversations can take time, so be creative within the constraints of a busy clinic, or schedule extra time for pregnancy test visits for this reason.
Another exercise for people who are unsure is to invite them to imagine their lives now and in a few years and how they might feel depending on the outcome of this pregnancy. “How would each outcome change, affect, or support your goals?”
| Continuing Pregnancy | Ending Pregnancy | |
| Pros: | ||
| Short Term | ||
| Long Term | ||
| Cons: | ||
| Short Term | ||
| Long Term |
When Counseling Someone Who Has Received a Prenatal Diagnosis
When presenting someone with a prenatal diagnosis, it is important to use neutral, compassionate, and non-judgmental communication strategies. Many people report receiving prenatal diagnoses in a tone insinuating that potential disability is inherently a tragedy and abortion was their only option (Wright 2008). It is also important to recognize that parenting a disabled child in an ableist society can feel overwhelming or beyond the capacity of an individual. Providers should consider the following:
- Use neutral language focused on the person’s desired pregnancy outcome.
- Provide scientifically accurate information about the condition, including both positive aspects and challenges related to the condition.
- Offer concrete examples of the effects of the condition on activities of daily life.
- Provide resources like local and national support groups, and printed fact sheets to assist in a fully informed decision (Wright 2008).
- Avoid assumptions about potential quality of life if the pregnancy is carried to term. Likewise, avoid assumptions about available resources, which are often more limited than people who are not disabled or not parenting a disabled person might believe.
- If appropriate, share the following resource on Ending a Wanted Pregnancy.
- Utilize the same communication principles if someone changes their mind after a prenatal diagnosis.
When Someone Has Religious, Spiritual, or Moral Conflict
People of all religious and spiritual backgrounds have abortions, and clinicians do not need a specific background to explore what this conflict means for them. People may experience moral conflict for multiple reasons. Some may have been raised to believe life begins at conception and that abortion is an act of murder. Others may feel that higher power(s), family, or others may not forgive their decision. The counseling framework above can help explore a person’s beliefs and options for spiritual reconciliation and healing. Suggesting readings (such as faith-based resources), discussions with clergy, a supportive religious group, or other counselors may be beneficial.
Additional resources:
- Catholics for Choice
- Religious Community for Reproductive Choice
- Faith Aloud
- Abortion Explained: Religion and Spirituality (We Testify)
- Sacred Choices: A Right to Contraception & Abortion in 10 World Religions (Maguire 2001)
- A Guide to Emotional and Spiritual Resolution After Abortion
Considerations for Counseling Minors
Pregnant minors, like others, deserve a supportive, nonjudgmental space to explore their options. Adolescents often face unique barriers to care, including legal restrictions, stigma, and a lack of safe or trusted adults to confide in. While most states allow minors to consent to STI testing and contraceptive care, many have parental involvement laws for abortion care (Allison 2024). Be informed about your state-specific policies, and connect minors with resources for judicial bypass, abortion funds, and doula networks or accompaniment networks as needed.
Many professional organizations emphasize the importance of confidential, adolescent-centered care that affirms autonomy and fosters trust (AAP 2022, ACOG 2017). In order to provide this kind of care, clinicians should reflect on their own biases about how an adolescent should proceed. Minors may vary in their knowledge and decision-making needs, and our role is to provide accurate, developmentally appropriate information without making assumptions about their emotions or circumstances (Rocca 2020). Encourage trusted adult involvement when possible—while affirming a minor’s right to confidentiality—to help ensure they feel supported in their choices. Further, providers should be supportive of the minor’s ultimate choice no matter the provider’s personal feelings about whether the decision is prudent.
Additional Resources: