ULTRASOUND (US) OVERVIEW, METHODS, TIPS & IMAGES
US is not a requirement prior to MAB or uterine aspiration, but can be used when clinical dating is uncertain, to evaluate pregnancy location, and/or to provide procedural support. Use of a transabdominal (TAUS) vs. transvaginal/intracavitary (TVUS) probe depends on patient preference, availability, gestational duration, and sonographer skill. Prior to transvaginal/intracavitary ultrasound, ask and use a person’s preferred anatomic language.
| Transabdominal Probe | Transvaginal/Intracavitary US |
|---|---|
|
|
A limited first trimester US exam must include: (NAF 2024)
- Uterine scan in both longitudinal and transverse planes to confirm IUP
- Evaluation of pregnancy number (singleton or multiple gestation)
- Measurements to document pregnancy dating
- Evaluation of pregnancy landmarks (e.g.yolk sac, embryonic/fetal pole, fetal cardiac activity)
Prior to Ultrasound
- Ask if the patient wants to view the image, keep a copy and/or be informed of the findings (e.g. gestational duration or multiple gestations—in 2-3% of spontaneous pregnancies).
- Inform that limited US only confirms pregnancy duration and location, but is not a diagnostic fetal anatomy scan for detecting anomalies or sex of fetus.
- Consider starting with TAUS, and switching to TVUS if unable to effectively visualize the pregnancy; TAUS is preferred by most people and sufficient to confirm EGD and IUP in most cases (Fu 2018).
- For TVUS, have person empty their bladder [Lee 2025] (collect urine for UPT if no IUP identified), use non-latex probe cover with US gel inside cover, sterile lubricant outside, and offer self-insertion.
- Use clear and simple language when discussing US findings; avoid triggering language that is medically inaccurate (ie “baby,” “heart beat,” etc.).
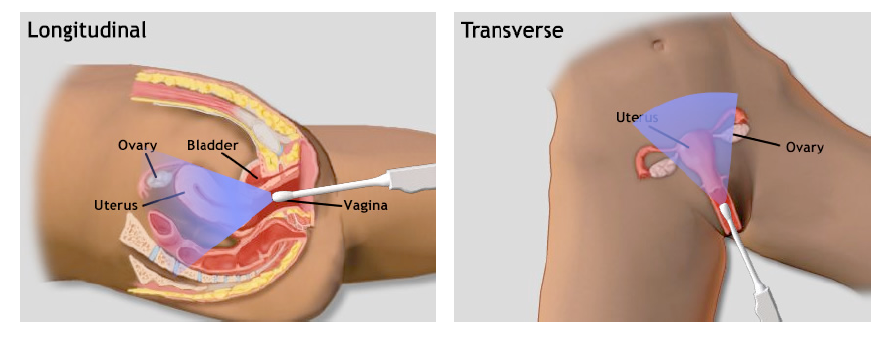
Ultrasound Planes in Early Pregnancy
TVUS planes (Image ARMS 2007)
- Systematically scan in both longitudinal and transverse planes.
- Use longitudinal view to confirm IUP by ensuring that the gestational sac is contiguous with the endometrial stripe. Place the probe marker up (12 o’clock) and scan the uterus side to side to its most lateral aspects (ovaries may or may not be lateral to the uterus). View shows uterine fundus above the cervix with pregnancy inside. Picture below demonstrates an anteverted uterus (fundus on left) with intrauterine pregnancy. Fundus will be on the right side of the screen with a retroverted uterus.
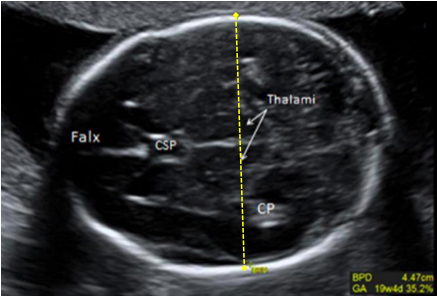
 (Images AIUM Image Library: Obstetrics 2018)
(Images AIUM Image Library: Obstetrics 2018)
- Use transverse view to evaluate for multiple gestations, and to obtain a full image of the uterus. For a transverse view, turn the probe 90 degrees to the patient’s right (counterclockwise or turn notch to 9 o’clock) and scan the uterus anterior to posterior, from fundus to cervix.
- Pregnancy landmarks including optimal view for landmark measurement may be found in longitudinal or transverse view.
Ultrasound Landmarks in Early Pregnancy
Seek to identify the pregnancy landmarks that should be visible on the US based on LMP.
| Pregnancy Landmarks by Weeks since LMP | |
| Gestational Sac | 4.5 – 5 weeks LMP |
| Yolk Sac | 5.5 weeks LMP |
| Embryonic Pole | 6 – 6.5 weeks LMP |
| Cardiac Activity | 6 – 6.5 weeks LMP |
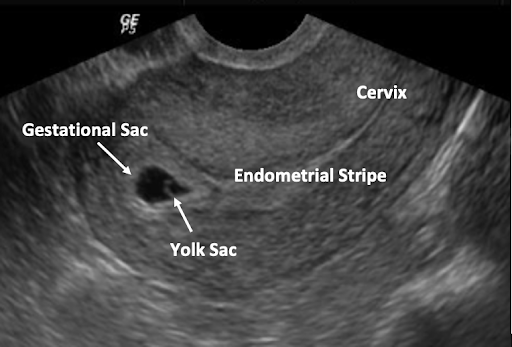
The Gestational Sac (GS)
- GS is the first evidence of pregnancy on US, as early as 4.5 weeks LMP; should always be seen by 5 weeks 5 days LMP by TVUS (Barnhart 2012).
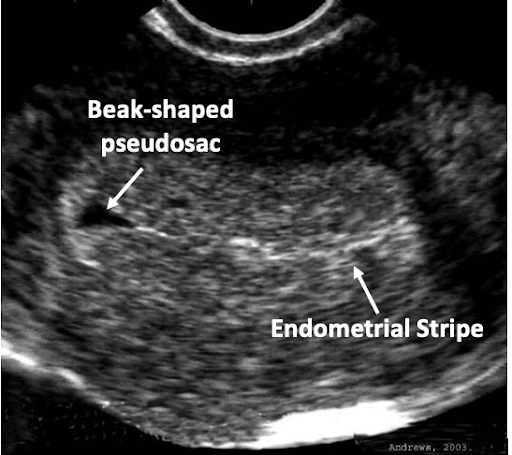
- Although gestational sac cannot definitively be diagnosed until a yolk sac or embryo is seen (Richardson 2015), an intrauterine fluid collection is a probable IUP if there are certain US features and no adnexal masses (Benson 2013, Phillips 2020).
- A true GS should be located in the uterine fundus, be eccentric (not midline) to endometrial canal, be round (or oval) in shape, and have a decidual reaction, demonstrating the FEEDS mnemonic.
- In contrast, an intracavitary collection of blood or fluid that is not a gestational sac (sometimes referred to as pseudosac) typically appears midline in the uterine cavity, lacks an echogenic rim, has pointed or non-curved margins, and may contain internal debris. These collections may be present in ectopic or be visible prior to the GS of an IUP.
- Whenever US scanning of the uterus in a pregnant patient does not identify a definite GS containing a YS or embryo, the adnexae should be evaluated. Detection of a complex or inhomogeneous adnexal mass or saclike structure separate from the ovary is highly suspicious for tubal ectopic pregnancy and warrants further evaluation.
 |
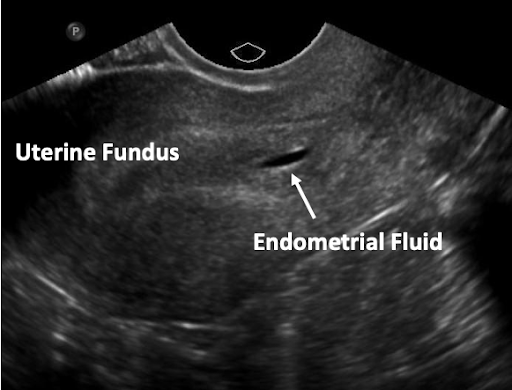 |
| Image: Fjerstad M, et al. CAPS, 2004 | Image: Dr Matt A. Morgan, Radiopaedia.org, rID: 34217 |
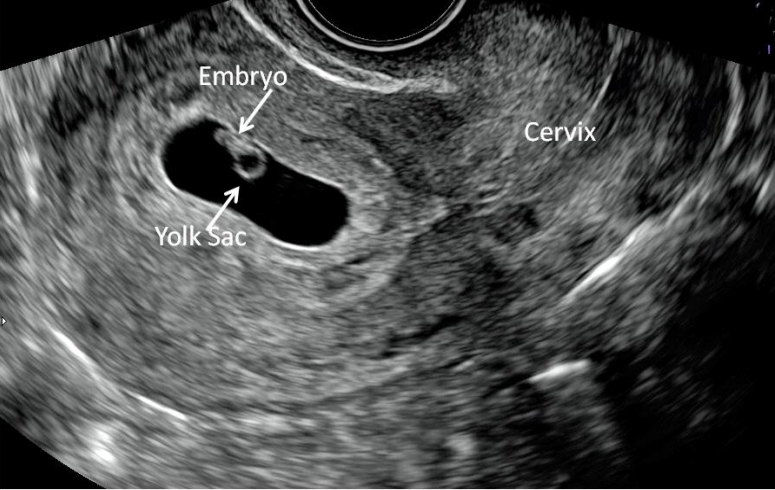
The Yolk Sac (YS)
The YS is the first single US finding that confirms an IUP. The YS is a round echoic ring with an anechoic (dark) center seen within GS. It appears typically at 5 1/2 weeks when the MSD is 5-10 mm. A YS should not be included when taking a measurement of the embryo. The size of the YS is not diagnostic.
Multiple Gestations
Fetal number should be assessed and documented. If a pregnancy plan is undecided, report amnionicity (# of sacs) and chorionicity (# of placentas). Prior to the US, it is helpful to know if a patient wishes to be told of multiple gestations. MAB dosing and procedural abortion will be the same regardless of multiple gestations except for assessing products for completeness after a procedural abortion.
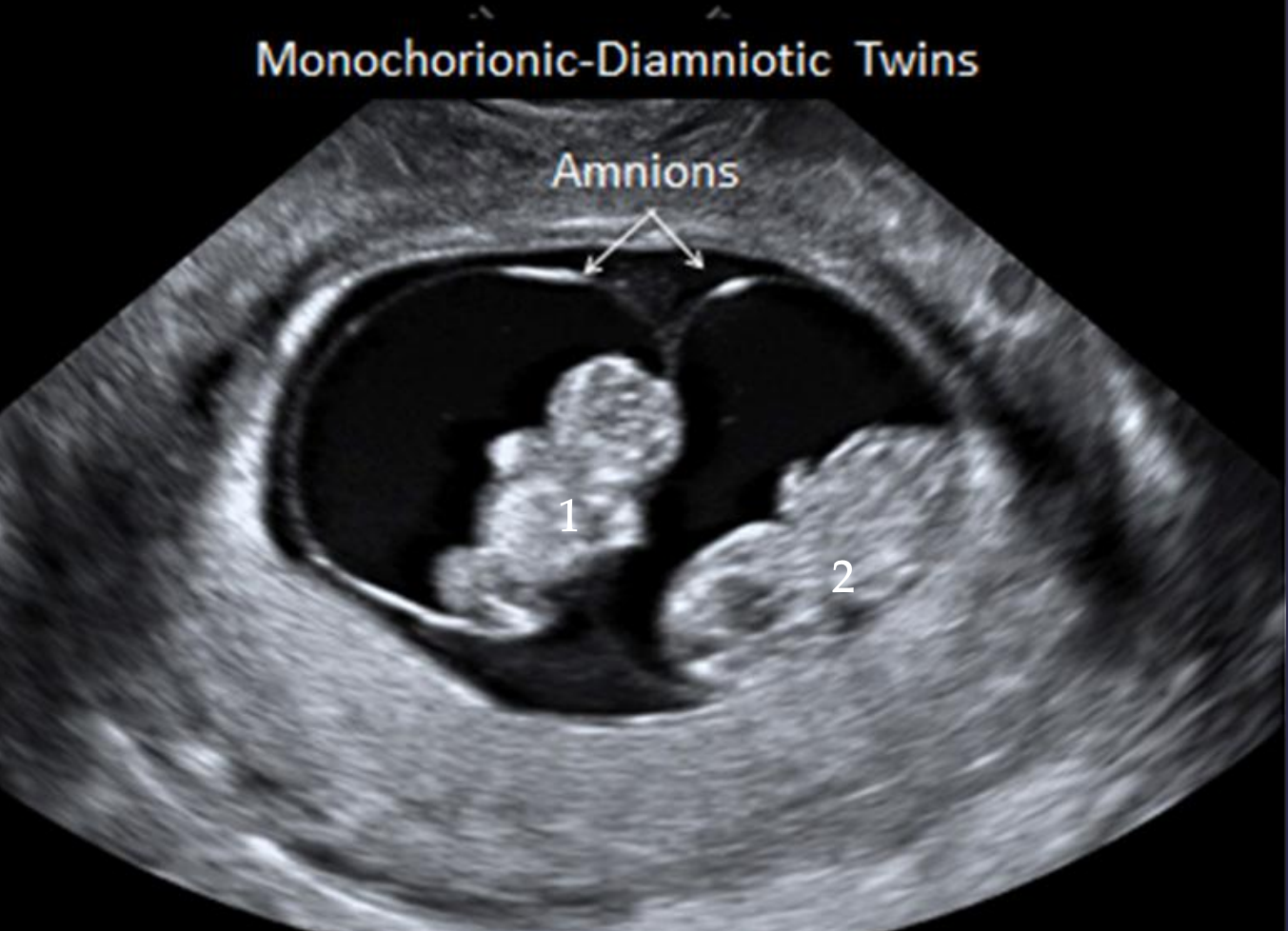 |
 |
Images AIUM Image Library: Obstetrics 2018
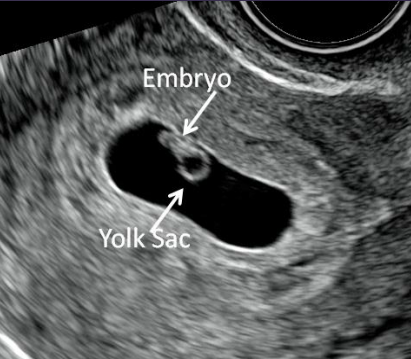
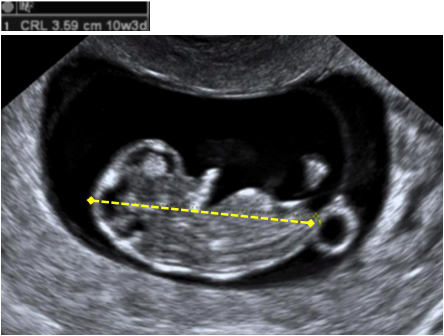
The Embryo and Cardiac Activity
The embryo follows predictable development and its measured size is used to date a pregnancy. The embryo appears at approximately 6 weeks and grows 1 mm per day until 12-14 weeks. See pregnancy dating below using embryonic/fetal measurement. Cardiac activity appears around 6 1/2 weeks.
Image from AIUM Image Library: Obstetrics 2018
IUP of uncertain prognosis
If a patient does not desire to continue the pregnancy, there is no reason to delay an abortion to await confirmation of viability, however some people may prefer a repeat ultrasound at a later date for confirmation. Person centered care may require prioritization of diagnosis as opposed to intervention and timing of definitive care may be impacted by numerous non-clinical factors. If US findings are diagnostic of or concerning for EPL, document appropriately: the diagnosis may impact the type of care available in legally restricted settings, and/or insurance coverage. If the patient desires to continue the pregnancy, and findings are suggestive of EPL, repeat US in 7-10 days (see Ch. 8: EPL Classification and Terminology for US diagnostic criteria).
Pregnancy Dating by US
Gestational Sac Measurement and Calculation of Gestational Duration:
Mean sac diameter (MSD) is used for dating before the embryo is visible. Measure 3 dimensions in 2 planes (from inside double ring to inside double ring):
- Longitudinal Plane: Length (L) & Height (H)
- Transverse Plane: Width (W)
Calculate the Mean Sac Diameter (MSD): MSD = (L + W + H)/3
Calculate Gestational Duration (GD): GD (in days) = MSD (in mm) + 30
 |
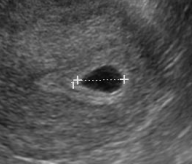 |
| Length and height measured in longitudinal view. | Width measured in transverse view. |