3
Learning Objectives
Upon completion of this module, participants will be able to:
- Understand the relationship between the central, peripheral nervous systems and anxiety
- Explain the function of the basal ganglia in relation to cognitive and behavioral symptoms of anxiety.
- Explain the amygdala and cortex as two pathways to understanding anxiety
- Understand the concept of cognitive fusion and its role in fueling anxiety
- Describe the role that neurotransmitters play in fueling anxiety
Introduction
To fully appreciate the dynamics of anxiety, gaining an understanding of the brain/body connection and the interplay among the body’s complex set of systems is vital for both assessment and intervention. As discussed in module 1, there are several factors that contribute to the etiology and risk for anxiety. Beyond risk factors and etiology, understanding the anatomy and functions of the central (brain and spinal cord) and the peripheral nervous systems (somatic and autonomic nervous systems) is critical to making sense of the anxiety experience. Furthermore, neuroscience has identified that the specific areas of the brain, the prefrontal cortex, and the amygdala, play a critical role in regulating emotion including fear and anxiety (Oler, 2019).
It was once believed that the amygdala held all the power for producing anxiety. While the amygdala plays a role in anxiety, there is now evidence that there are other contributing factors. For example, researchers have found that the size of certain brain parts plays a role in anxiety. A study conducted by Stanford University (2013) discovered that a larger amygdala increases anxiety risk in children and adults. This enlargement makes the amygdala hypersensitive (hyper alert) to possible threats and as a result, triggers false alarms within the brain. Current research is exploring the interplay between the amygdala and an area of the brain known as the bed nucleus of the stria terminalis or the BNST. This is a pea size cluster of neurons which is believed to fuel persistent anxiety (Knight and Depue, 2019).
Remember the basal ganglia (BG) from chapter two? It also plays a role in anxiety production. When the basal ganglia are overactive, people with anxiety may be more likely to feel overwhelmed by stressful situations and freeze or become immobile (sound familiar? fight, flight, or freeze) (Wehrenberg, 2018). This can include physical responses like trembling when nervous or freezing when scared, as well as cognitive responses like becoming tongue-tied. Take social anxiety disorder (SAD) for example. It is said that SAD may be associated with reduced basal ganglia function due to altered dopamine function. This can impair social motor functions like smiling, eye movements, and speech, which can lead to avoidance behaviors.
Beyond the above points, the BG have other influences as well (Marchand, 2010). These include, but not limited to:
Neural Circuits: The basal ganglia are part of neural circuits that connect with the limbic system, which is crucial for emotional processing. This connection influences anxiety-related behaviors.
Neurotransmitters: The basal ganglia have a high density of dopamine and serotonin receptors. These neurotransmitters are known to be involved in mood regulation and anxiety. Dysregulation in dopamine and serotonin systems within the basal ganglia can contribute to anxiety disorders.
Cognitive and Motor Functions: The basal ganglia are involved in the integration of cognitive and motor functions. Anxiety can manifest through both cognitive symptoms (e.g., excessive worry) and motor symptoms (e.g., restlessness or repetitive behaviors), implicating the basal ganglia in these processes.
In the end, it is important to remember that the BG influences anxiety through their role in neural circuits involving emotional processing, neurotransmitter regulation, and cognitive and motor functions.
As stated before, the brain is a complex organ, and we are continuing to learn more about the relationship between the brain and anxiety through ongoing research.
Our current understanding highlights that fear and anxiety are the result of multiple systems at play within different regions of the brain. More specifically, there are two neurological pathways that lead to a fear response (often referred to as a stress response). These pathways travel within the cognitive (prefrontal cortex) and emotional parts (limbic system) of the brain (Pittman and Karle, 2015). This module will introduce readers to the limbic system, two pathways to anxiety, and the role of neurotransmission in the fear response.
**NOTE: As you prepare to read this module, it will be critical that you have read module 2 “Introductory to the Nervous System.”
Limbic System
Prior to jumping into the pathways to anxiety, we will further explore an area of the brain known as the limbic system. The limbic system includes the amygdala, hippocampus, thalamus, and hypothalamus (See image 1). The limbic system is considered the emotional center of the brain, and it plays a vital role in the experience of fear and anxiety. Each part of the limbic system has its own set of functions (See table 1).
Image 1: Limbic System
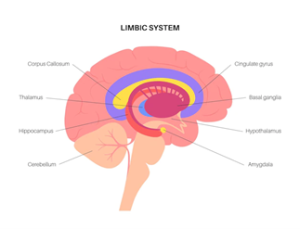
(Source: The Limbic System, freepik)
Table 1: Limbic System Parts and Functions
| PART | FUNCTION |
| Thalamus | The thalamus sits on top of the brainstem. Its primary function is that of a router. It receives information from your senses, sorts out that information and decides where to send it within the brain. It typically sends information to the limbic system and/or the cortex. Sensory information routed through the thalamus tend to be sights and sounds. However, smell bypasses the thalamus and goes directly to the olfactory system and amygdala. |
| Amygdala | It is most known for processing fear and detecting threats. It acts as a guard and prepares us to protect ourselves by activating other brain/body parts. The amygdala helps process and regulate both positive and negative emotion. It works closely with the hippocampus as it attaches emotion to memories. Stimulation of the amygdala can lead to a stress response (fight, flight, or freeze) which is linked to anxiety and fear. |
| Hypothalamus | The hypothalamus’s primary role is to keep the body stable and in balance (also known as homeostasis) and it does so with the release of hormones (i.e., stress hormones). It acts as a switchboard between the endocrine and nervous system. It assists in regulating temperature, hunger, sex drive, and sleep. |
| Hippocampus | The hippocampus has many functions but is most known for its role in learning and memory. This is where memories are processed, organized, retrieved, and stored. It takes data and facts and sends it to the thinking part of the brain- the cortex. |
Click the video link below to learn more about the limbic system
Pathways to Anxiety
It is helpful to think of the brain in three distinct parts each with their own set of responsibilities; survival, emotional, and thinking brain (LeDoux, 1998), (See table 2). Each of these components contribute to the experience of fear, anxiety, and stress. However, there are two primary pathways to anxiety that create a chain-like reaction thus triggering an emotional and physiological response. The two pathways occur via the amygdala and the pre-frontal cortex. While there are two specific pathways, I want to note that the amygdala plays a role in both, resulting in the activation of stress response.
Table 2: Brain Components Broken Down
| Survival Brain |
|
Heart rate Breathing Movement Sleep/wake cycle Body temperature
|
| Emotional Brain |
|
Deals with emotions (and attaches emotions to memories) Assesses for threats and danger Activates the fear and stress response
|
| Thinking Brain |
|
Problem-solving Organizing Planning Language/communication |
Pathway 1: The Amygdala
The amygdala contributes to several functions within the brain. One of its primary functions is to respond to fear and detect real/perceived threats. You can think of it as an alarm system with a guard that is continuously scanning the environment for potential danger. If potential danger is detected, the alarm system is automatically activated thus producing a fear response. At this juncture, the body prepares itself to engage in self-protection which is known as the stress response. This response triggers what is known as flight, fight, or freeze (while fawn is another type of stress response, it is mostly linked to PTSD). In general, this type of survival response is normal and what keeps us protected. However, when the threat has subsided and a person experiences chronic activation of the fear response, it can lead to disordered anxiety (Pittman and Karle, 2018). In short, the stress response should be activated when needed, and de-activated when not needed. This is not always the case for people with problematic anxiety.
Another common metaphor used to describe the amygdala is that of a smoke detector. Before reading on, write down things that you believe could set off a smoke detector. Perhaps you included the following in your list: low batteries, smoke from cooking, dusty/dirty, or malfunctioning. What do you typically do when your smoke detector goes off? Is the first thing you do call 911? In most cases the answer is no because we have context of what is happening. You most likely try a few things to address the alarm such as replace the batteries, open a window, turn on a fan, or clean the detector. Our brain and body respond to anxiety like a smoke detector responds to its trigger. In many cases, the threat or danger is a false alarm. Those with anxiety often have an overactive amygdala thus experiencing consistent false alarms. When activated, the amygdala goes into self-protective mode (i.e., fight/flight/freeze, activation of hormones including cortisol and adrenaline).
The amygdala pathway is often referred to as the “low road” (LeDoux, 2000). When the brain receives sensory messages of danger or threat via the thalamus it automatically sends this information to the amygdala, thus bypassing the thinking part of the brain (pre-frontal cortex). Once the emotional response is activated, the amygdala sends out an emergency SOS notifying other brain parts to prepare for defense (LeDoux, 2000). It is at this point that bodily changes are initiated for protection and defense. For instance, the body releases the stress hormone cortisol as well as adrenaline. Again, these chemicals make the body stronger for defense. For example, a person may start to notice an accelerated heartrate, rapid breathing, increased energy, and dilated pupils.
Because the fear response activation happens so quickly and on an unconscious level, people are often confused as to what triggered this level of response. For example, if a person describes feeling anxious for no apparent reason and that it came out of the blue, the anxiety experience is most likely the result of the amygdala pathway. Does this sound familiar? This is reflective of a person who may experience panic attacks. To determine if the anxiety response is amygdala based, it is important to assess what was happening before the onset of symptoms (Pittman and Karle, 2015). For example, if there was a specific situation, event, or location that initiated the stress response, it is most likely amygdala based (i.e., fear of open spaces such as the beach).
It is our brains unconscious mechanism that manages our fear and stress response. This pathway of anxiety often feels like it is out of a person’s control. The thinking part of the brain (pre-frontal cortex) goes offline sort of speak. The energy used to run the thinking part of the brain is funneled to the survival and emotional parts of the brain. So, trying to use self-talk (i.e., telling oneself there is no reason to be anxious, or that everything will be okay) when the amygdala has been activated will not stop the stress response (Pittman and Karle, 2015). When a person can effectively use the thinking part of their brain, the emotional part of the brain can often be calmed by activating the parasympathetic nervous system (thus the thinking brain overrides the emotional brain). This is also reflective of the rest and digest process. It is often said that we feel anxious bodily, before we know it consciously.
At what point does a hyperactive amygdala become problematic? According to Schmidt, et al., (2018), “It is theorized that amygdala dysfunction may drive the inappropriate threat perception and emotional dysregulation believed to lie at the heart of many anxiety disorders.” When a person experiences ongoing and unnecessary fear responses, even after the elimination of the real or perceived threat, the amygdala can become dysregulated. This dysregulation not only causes a person to experience persistent feelings of anxiety, but it can lead to heightened states of fear and alertness. Thus, a person will continuously be in a stress response state of mind (fight, flight, or freeze) when no potential threat is detected. You can think of it as the amygdala being overly protective and activating the fear response just in case. It is at this point that the amygdala cues other systems to prepare the body for protection (even if it is not warranted). Again, when these systems are activated, a person may experience physiological symptoms such as a pounding heart, perspiration, shortness of breath, and increase in adrenaline. Yet, there are strategies that can be employed to counter-act these physiological reactions. And if you can recall, the amygdala plays a role in attaching emotions to memories. For this reason, people who struggle with specific phobias (fear of flying, snakes), may have an attached negative emotional memory stored in the amygdala. In many cases, a person may meet criteria for disordered anxiety such as generalized anxiety, specific phobia, or panic disorder.
Pathway 2: The Prefrontal Cortex (PFC)
When discussing anxiety and fear, many focus on the role of the amygdala. While the amygdala is a powerful force in the anxiety experience, the PFC also plays an important role in anxiety production and exacerbation. In fact, the PFC can create a false and misinterpreted narrative leading to unnecessary anxiety. This is why for example, CBT focuses on identifying and changing/modifying unhelpful thoughts. Furthermore, it can exacerbate any anxieties that were the result of the amygdala pathway (Pittman, 2015). In reality, the amygdala and PFC often work in concert, but their paths to anxiety are different. More importantly, involvement of the amygdala is required for their to be an actual anxiety or stress response.
The PFC pathway, also referred to as the “high road”, takes a less direct route to the amygdala when responding to stimuli (LeDoux, 2000). This route is known to take place on a more conscious level as where the amygdala pathway, takes place on an unconscious level. The high road pathway is slower thus allowing more time to process incoming information. Once the PFC receives information from the thalamus (in the form of sensory or non-sensory information), it attempts to correctly evaluate the incoming stimuli. The PFC, through high-level of cognitive processing, tries to determine if the perceived threat is real or not so it can convey this information to the amygdala. In those with anxiety, it may be the case that the PFC is underactive and not able to sufficiently communicate with an overstimulated amygdala. This is one scenario when we see disordered anxiety. If a person is focused on specific thoughts or images prior to experiencing anxiety symptoms, it is most likely driven by the PFC. Prefrontal cortex-based anxiety involves two different sources of stimuli: sensory-driven and non-sensory driven.
- Sensory driven: As you might recall, the thalamus is considered a router thus relaying information to different parts of the brain. For example, once the thalamus receives sensory information (i.e., sight, sound), it sends it to either the PFC or the amygdala. In the case of the PFC, it receives information from the thalamus to be processed. The challenge here is that the information being processed and interpreted is not always done correctly. This may be the result of the hippocampus encoding and storing memories associated with an adverse life experience (i.e., child abuse and neglect). It may also be due to disruption in communication between the right and left hemispheres (Pittman, 2015).
- Non-sensory driven: This type of anxiety experience happens in the absence of a person’s senses. The anxiety experience is brought on by thoughts and images. As you may recall, the brain is divided into two hemispheres and each hemisphere responsible for various functions. These functions may work independent of one another, or they may work in concert. More specifically, the left brain hemisphere is responsible for thought-based anxiety and the right brain image-based anxiety. Second, we know that thoughts and images alone, can initiate and/or exacerbate a fear response leading to feelings of anxiety (Pittman, 2015).
It is when the thinking brain sends information to the emotional brain that the perceived danger is not real, that the alarm system shuts down and the body begins to calm down. You can think of it as going from a high arousal state to a low arousal state. A state that is manageable.
Here is an illustration to help you digest the high road to anxiety which involves cognition. For instance, let’s say you are out hiking in the woods, and you encounter a bear. This encounter most likely would immediately activate your amygdala, your survival system. Your body immediately prepares for survival mode in the form of flight, fight, or freeze. As a result of this activation, you experience a rush of adrenaline, increased heart and breathing rate, and increased alertness. On the other hand, if you were to encounter a bear at the zoo (the bear is behind a barricade thus not creating any risk to you as the observer), this visual sensory input would go from the thalamus to your PFC to be evaluated. Given you are not in immediate danger and not exposed to an uncaged bear, the PFC conveys this to the amygdala who then does not sound off the alarm. This involves processing what we call contextual information via the PFC and hippocampus. In a nutshell, the thinking brain is providing reassurance to the emotional brain that danger is not present and that everything is okay.
Prior to moving on, I want to say a bit more about the role of the hippocampus. Again, the hippocampus plays a role in creating, encoding, and storing both positive and negative memories. It also communicates with both the amygdala and PFC and contributes to both the calming and activating of certain memories. The hippocampus tends to be extra sensitive to memories associated with adverse life events (leading to negative memories). This is one of the reasons why people develop a conditioned fear response to certain triggers or stimuli (i.e., situations, contexts, or objects). However, repeated activation of certain negative memories can trigger and lead to the production of symptoms reflective of anxiety. This repeated activation and the modifying of memory is known as reconsolidation (Fernandez, et al., 2017). Conversely, recalling a time when you had a panic attack, survived, and felt better shortly after the attack. This type of memory can increase a person’s confidence that they can manage future panic attacks (Greenberg, 2019).
Left hemisphere: What is the role of the left hemisphere in anxiety. This is where distressing thoughts such as worry and rumination (or what I call marinating or perseverating) take place. It is often assumed that engaging in these types of distressing thoughts will help reduce feelings of anxiety which is quite the contrary. For example, ruminating on a problem as a form of problem-solving or a way to find a solution reinforces the pathway to anxiety. These types of distressing thoughts activate the amygdala which results in both the physiological (rapid heart rate, shortness of breath, feeling dizzy) and behavioral (avoidance, fidgety) symptoms of anxiety.
Right hemisphere: The right hemisphere has less to do with language and logic, but rather deals with creativity, imagination, emotions, and intuition. The primary trigger for anxiety via the right hemisphere is a person’s senses (sight, sound, touch). For example, a person who struggles with flying, may be asked to imagine getting ready for their flight. Perhaps they are asked to visualize the process of getting ready for a flight to Mexico starting with packing at home. Depending on where a person is in terms of anxiety recovery, this can be quite triggering. Even the sight of an airplane on TV can be activating for those who have a fear of flying. These triggering visualizations or images activate the amygdala. In return, the amygdala prepares itself for protection.
Cognitive Fusion
Do you recall from module #2 how many thoughts our brain can generate in a day? It can generate up to 50,000 thoughts per day! That is a lot of thoughts to have to manage and navigate. The way in which we manage and navigate our thoughts can have an impact on the initiation and exacerbation of anxiety regardless of which anxiety pathway. According to Steven Hayes (2005), the developer of Acceptance and Commitment Therapy (ACT), describes cognitive fusion as “when we are so tightly stuck to our thoughts, we become “fused” to them. When we’re experiencing cognitive fusion, we can’t separate ourselves from our thoughts. Our thoughts become our reality.” They shape our identify. This simply means believing in the absolute truth of your thoughts (Pittman, 2015). Take worry for example. Worry can be quite seductive as many believe that putting energy into worrying will relieve their anxieties. The truth is worry exacerbates anxiety. Here is another example to consider. You are working with a client who has the belief that if they ride the subway to work (the thought) that they will have a major panic attack (the experience/the truth). These thoughts can activate our amygdala which results in bodily changes including, a rapid heart rate, shortness of breath, and/or sweating. Thus, our thoughts can not only have an impact on how we experience and interact with our world, but they can also lead to symptoms of anxiety.
Understanding cognitive fusion is important for treatment and intervention. Underscoring the importance of creating self-awareness, challenging and questioning our own thoughts is part of the treatment process. It is also important to remember that thoughts are just that…Thoughts. Part of the goal is to prevent unhealthy or problematic cognitive fusion. We can prevent this by engaging in the process of cognitive defusion. This simply means learning how to accept our thoughts as just thoughts without allowing them to get stuck in our heads or perseverating on them. You can think about it as acknowledging your thoughts without giving them power by buying into them. Applying cognitive defusion practices assists people in changing their relationship to unhelpful thoughts. As part of this intervention, a person will learn to create space between their thoughts and reactions. This pause, this space, allows people to recognize and question patterns in how they think and feel. The ability to be mindful and curious about anxiety provoking thoughts is a major step in the healing process.
The Role of Neurotransmission
While this module has focused on the pathways to anxiety via the pre-frontal cortex and the amygdala, it is important to remember that communication along these pathways does so via neurotransmission. As discussed in module 2, neurons (aka nerve cells) communicate via the process of neurotransmission. If you recall, there are several types of neurotransmitters each with a different function. The functions are inhibitory, excitatory, or a combination of both. The influence of neurotransmitters function has a direct link to the experience of anxiety. For example, one of the primary neurotransmitters associated with worry is serotonin. Serotonin assists with regulating mood and is often found to be deficient in those with anxiety and depression. In the case of anxiety, if there is sufficient serotonin, it can assist with shifting gears with thinking (i.e., decision making), thus helping to manage worry (Wehrenberg, 2018). Another important neurotransmitter is GABA. This inhibitory neurotransmitter is known for producing a calming effect as it slows down the triggering of anxiety-based messages within the brain (Wehrenberg, 2018). As you think about the pathways to anxiety, it is important to remember that different parts of the brain play a role in communication responsible for sending, receiving, interpreting, and creating a response.
Conclusion
In order to effectively assess and treat anxiety, understanding the building blocks of anxiety, is critical. For example, being able to determine the pathways to anxiety will aid in determining which treatment approaches are most appropriate. Furthermore, understanding the pathways requires knowledge of the nervous system structures and functions. It also requires an understanding of the role of memories and cognition (i.e., cognitive fusion).
Learning Activities
- Video challenge. Video record yourself explaining the role of the amygdala, thalamus, and pre-frontal cortex as they pertain to fear and anxiety.
- You are a therapist and provide therapeutic services at a local mental health clinic. One of your roles is to mentor undergraduate students. You are currently mentoring a BSW student who has an interest in treating people with anxiety. During one of your meetings, your mentee asks you what you know about the peripheral nervous system and its relation to anxiety disorders. Verbatim, how would you respond to your mentee?
References
Fernandez, R.S., Pedreira, M., Boccia, M.M. (2017). Does reconsolidation occur in natural settings? Memory reconsolidation and anxiety disorders. Clinical Psychology Review, 57, pp.45-58
Greenberg, M. (Sept. 30, 2019). Understanding Brain Circuits of Fear, Stress, and Anxiety. Psychology Today. https://www.psychologytoday.com/us/blog/the-mindful-self-express/201909/understanding-brain-circuits-fear-stress-and-anxiety
Hayes, S. C., & Smith, S. (2005). Get out of your mind and into your life: The new acceptance and commitment therapy. Oakland, CA: New Harbinger.
Knight, L.K., and Depue, B.E. (2019) New Frontiers in Anxiety Research: The Translational Potential of the Bed Nucleus of the Stria Terminalis. Front. Psychiatry 10 (510). doi: 10.3389/fpsyt.2019.00510
LeDoux, J.E. (2000). Emotion circuits in the brain. Annual Review of Neuroscience 23, 155-184.
LeDoux, J. (1998). The emotional brain: The mysterious underpinnings of emotional life. Simon and Schuster.
Marchand, W.R. (2010). Cortico-basal ganglia circuitry: a review of key research and implications for functional connectivity studies of mood and anxiety disorders. Brain Struct Funct 215, 73–96.
Oler, J.A., & Fudge, J.L. (2019). Prefrontal cortex: A tale of two pathways. Insight. https://elifesciences.org/articles/51990
Pittman, C.M., & Karle, E.M. (2015). Rewiring the anxious brain. How to use the neuroscience of fear to end anxiety, panic and worry. New harbinger publications.
Stanford Medicine (2013, Nov. 20). Size, connectivity of brain region linked to anxiety level in young children, Stanford study shows. https://www.eurekalert.org/news-releases/516115
Schmidt, C.K., Khalid, S., Loukas, M. & Tubbs, R.S. (2018). Neuroanatomy of Anxiety: A Brief Review. Cureus, 10 (1). doi: 10.7759/cureus.2055
Wehrenberg, M. (2018). The 10 best-ever anxiety management techniques (2nd ed). Norton and company.
Images
