Mekong Malaria Elimination Program – Rationale and Implementation
Program Implementation
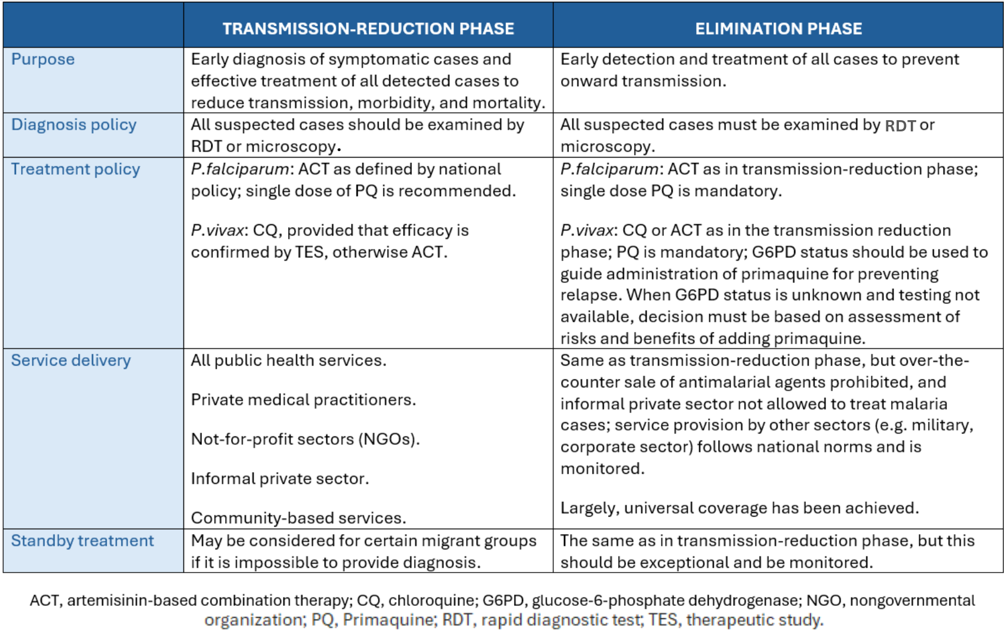
The action phases for the NMCEP parallel the MME Program’s two implementation stages (WHO, 2015). The latter’s transmission reduction stage corresponds to the NMCEP’s active malaria control and pre-elimination phase, while the elimination stage is compatible with elimination and prevention of re-introduction (Table 1). Applicable to both phases, rapid diagnostic tests or light microscopical examination of Giemsa-stained blood films are used to diagnose malaria at many health facilities (WHO, 2015). For treatment, the first-line ACT is administered for P. falciparum cases in both transmission reduction and elimination phases, while P. vivax cases require chloroquine or ACT, combined with a 14-day primaquine course for elimination.
As an index used as by the NMCEP, slide positivity rate (SPR) is defined as the percentage of suspected cases that is clinically confirmed to be malaria-infected (Jensen et al., 2009). This metric is particularly useful for continuously changing malaria incidence and therefore is often utilized to identify the transition point between phases (MoH, 2011) (Figure 4). In order to advance from the pre-elimination phase, SPR needs to be less than 5% of confirmed malaria cases (MoH, 2011). Once SPR is determined as zero, the elimination phase is considered to be completed, thereby instigating the final phase of preventing re-introduction of malaria to the region. In settings where there is no recorded case of malaria for three successive years, a certification of malaria-free status is issued by the WHO (MoH, 2011).

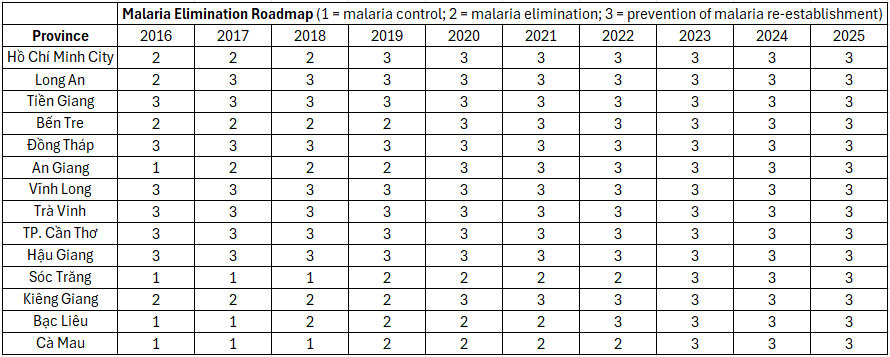
In 2017, the MoH approved the Malaria Elimination Roadmap (Table 2), which plots three zones of malaria management for 63 Việt Nam provinces from 2016 to 2025. Zone 1 suggests stable control of malaria cases. Zone 2 indicates the eradication of malaria for that region. Zone 3 designates provinces that can avert re-establishment of malaria. The roadmap serves as an annual objective for local authorities to implement preventive strategies and proposals for their respective provinces (MoH, 2020).
Vector control and personal protective measures, both focusing on mosquitoes, are major components of the NMCEP (WHO, 2018). The goal of the MME Program’s transmission reduction phase is to encompass at-risk populations with LLINs or IRS, explicitly migrant and mobile populations (WHO, 2015). For the subsequent elimination phase, besides incorporating prior objectives, all populations in active foci of malaria receive coverage to target early interruption of transmission.
Before the introduction of LLINs and LLHNs in 2009 (CDC, 2019), the ITN that provides an outer protective layer, enveloping each person sleeping under one, was the most popular protective measure in Việt Nam against mosquito bites (Canavati et al., 2021). Although LLINs are similar to ITNs, they differ in the scale of distribution to households, allowing for extensive coverage of communities residing in areas of transmission (WHO, 2015). LLHNs function to protect forest workers, migrants and high-risk mobile groups. This preventive method has been adapted to southern Việt Nam’s tropical climate, harnessing the already popular hammock (WHO, 2015). In addition, the Government also offers retreatment for those who prefer to use their own nets or who reside in less endemic areas, depending on the types of insecticide available in each location (WHO, 2018). Furthermore, IRS is considered a crucial aspect of vector control in Việt Nam. IRS with an alpha-cypermethrin formulation is carried out as a routine mass preventive measure in high-risk areas and as a focal responsive initiative in the event of an outbreak (WHO, 2018). However, a descriptive scheme for IRS has yet to be developed, nor has the plan for appropriate use of insecticides or the action to be taken in the case of insecticide resistance (WHO, 2018).
In 2015, the NMCEP was reviewed for its effectiveness, which resulted in several modifications to improve implementation. First, the Action Plan for Information, Education & Communication was developed to provide knowledge about malaria control and elimination (MoH, 2011). Second, a preventive plan to hinder the development and spread of artemisinin-resistant (AR) malaria parasites domestically and internationally was also initiated by the MoH (2011). From 2016 to 2020, the NMCEP was reviewed repeatedly for stronger interventions. It was determined that the “artemisinin-resistance containment” model should be more rigorous in preventing drug-resistant parasite isolates. Studies of drug resistance management were conducted, with action taken to delay the growth of AR malaria parasites (MoH, 2020). Tafenoquine and primaquine is each proven to be a safe and currently an effective anti-malaria drug for the treatment of P. vivax in Việt Nam. The initial step is to assess the drug’s effect on glucose-6-phosphate dehydrogenase-deficient patients as introducing an untested protocol may lead to a serious repercussion of hemolysis (WHO, 2015; MoH, 2020).
