What happens during prenatal development?
 How did you come to be who you are? From beginning as a one-cell structure to your birth, your prenatal development occurred in an orderly and delicate sequence. There are three stages of prenatal development: germinal, embryonic, and fetal. Keep in mind that this is different than the three trimesters of pregnancy. Let’s take a look at what happens to the developing baby in each of these stages.
How did you come to be who you are? From beginning as a one-cell structure to your birth, your prenatal development occurred in an orderly and delicate sequence. There are three stages of prenatal development: germinal, embryonic, and fetal. Keep in mind that this is different than the three trimesters of pregnancy. Let’s take a look at what happens to the developing baby in each of these stages.
Learning Objectives
- Differentiate between development during the germinal, embryonic, and fetal periods
- Examine risks to prenatal development posed by exposure to teratogens
- Explain potential complications of pregnancy and delivery
Prenatal Development
“The body of the unborn baby is more complex than ours. The preborn baby has several extra parts to his body which he needs only so long as he lives inside his mother. He has his own space capsule, the amniotic sac. He has his own lifeline, the umbilical cord, and he has his own root system, the placenta. These all belong to the baby himself, not to his mother. They are all developed from his original cell.”
Periods of Prenatal Development
Let’s take a look at some of the changes that take place during each of the three periods of prenatal development: the germinal period, the embryonic period, and the fetal period.
The Germinal Period (Weeks 1-2)

Conception occurs when a sperm fertilizes an egg and forms a zygote, which begins as a one-cell structure. The mother and father’s DNA is passed on to the child at the moment of conception. The genetic makeup and sex of the baby are set at this point. The germinal period (about 14 days in length) lasts from conception to implantation of the zygote (fertilized egg) in the lining of the uterus.
During the first week after conception, the zygote divides and multiplies, going from a one-cell structure to two cells, then four cells, then eight cells, and so on. The process of cell division is called mitosis. After the fourth division, differentiation of the cells begins to occur as well. Differentiated cells become more specialized, forming different organs and body parts. They’re different than stem cells, which are flexible to develop into any type of cell. After 5 days of mitosis, there are 100 cells, and after 9 months there are billions of cells. Mitosis is a fragile process, and fewer than one-half of all zygotes survive beyond the first two weeks (Hall, 2004).
After the zygote divides for about 7–10 days and has 150 cells, it travels down the fallopian tubes and implants itself in the lining of the uterus. It’s estimated that about 60 percent of natural conceptions fail to implant in the uterus. The rate is higher for in vitro conceptions. Once the zygote attaches to the uterus, the next stage begins.
The Embryonic Period (Weeks 3-8)

The embryonic period lasts from the third through the eighth week after conception. After implantation at the end of the germinal period, this multi-cellular organism is called an embryo. Now blood vessels grow, forming the placenta. The placenta is a structure connected to the uterus that provides nourishment and oxygen from the mother to the developing embryo via the umbilical cord.
During this period, cells continue to differentiate. Basic structures of the embryo start to develop into areas that will become the head, chest, and abdomen. During the embryonic stage, the heart begins to beat and organs form and begin to function. At 22 days after conception, the neural tube forms along the back of the embryo, developing into the spinal cord and brain.
Growth during prenatal development occurs in two major directions: from head to tail (cephalocaudal development) and from the center outward (proximodistal development). This means that those structures nearest the head develop before those nearest the feet, and those structures nearest the torso develop before those away from the center of the body (such as hands and fingers).
The head develops in the fourth week and the precursor to the heart begins to pulse. In the early stages of the embryonic period, gills and a tail are apparent. But by the end of this stage, they disappear and the organism takes on a more human appearance. The embryo is approximately 1 inch in length and weighs about 4 grams at the end of this period. The embryo can move and respond to touch at this time.
About 20 percent of organisms fail during the embryonic period, usually due to chromosomal abnormalities. As in the case of the germinal period, often the mother does not yet know that she is pregnant. It is during this stage that the major structures of the body are taking form making the embryonic period the time when the organism is most vulnerable to the greatest amount of damage if exposed to harmful substances. Potential mothers are not often aware of the risks they introduce to the developing embryo during this time.
The Fetal Period (Weeks 9-40)

When the organism is about nine weeks old, the embryo is called a fetus. At this stage, the fetus is about the size of a kidney bean and begins to take on the recognizable form of a human being as the “tail” begins to disappear.
From 9–12 weeks, the sex organs begin to differentiate. By the 12th week, the fetus has all its body parts including external genitalia. In the following weeks, the fetus will develop hair, nails, teeth and the excretory and digestive systems will continue to develop. At the end of the 12th week, the fetus is about 3 inches long and weighs about 28 grams.
At about 16 weeks, the fetus is approximately 4.5 inches long. Fingers and toes are fully developed, and fingerprints are visible. During the 4-6th months, the eyes become more sensitive to light and hearing develops. The respiratory system continues to develop. Reflexes such as sucking, swallowing, and hiccuping develop during the 5th month. Cycles of sleep and wakefulness are present at that time as well. Throughout the fetal stage, the brain continues to grow and develop, nearly doubling in size from weeks 16 to 28. The majority of the neurons in the brain have developed by 24 weeks although they are still rudimentary and the glial or nurse cells that support neurons continue to grow. At 24 weeks the fetus can feel pain (Royal College of Obstetricians and Gynecologists, 1997).
The first chance of survival outside the womb, known as the age of viability is reached at about 22 to 26 weeks (Moore & Persaud, 1998). By the time the fetus reaches the sixth month of development (24 weeks), it weighs up to 1.4 pounds. Hearing has developed, so the fetus can respond to sounds. The internal organs, such as the lungs, heart, stomach, and intestines, have formed enough that a fetus born prematurely at this point has a chance to survive outside of the mother’s womb.
Between the 7th and 9th months, the fetus is primarily preparing for birth. It is exercising its muscles, its lungs begin to expand and contract. It is developing fat layers under the skin. The fetus gains about 5 pounds and 7 inches during this last trimester of pregnancy which includes a layer of fat gained during the 8th month. This layer of fat serves as insulation and helps the baby regulate body temperature after birth.
Around 36 weeks, the fetus is almost ready for birth. It weighs about 6 pounds and is about 18.5 inches long, and by week 37 all of the fetus’s organ systems are developed enough that it could survive outside the mother’s uterus without many of the risks associated with premature birth. The fetus continues to gain weight and grow in length until approximately 40 weeks. By then, the fetus has very little room to move around and birth becomes imminent.

Environmental Risks
Teratology
Good prenatal care is essential. The developing child is most at risk for some of the most severe problems during the first three months of development. Unfortunately, this is a time at which most mothers are unaware that they are pregnant. It is estimated that 10% of all birth defects are caused by prenatal exposure or teratogen. Teratogens are factors that can contribute to birth defects which include some maternal diseases, drugs, alcohol, malnutrition, and stress. These exposures can also include environmental and occupational exposures. Today, we know many of the factors that can jeopardize the health of the developing child. Teratogen-caused birth defects are potentially preventable.
The study of factors that contribute to birth defects is called teratology. Teratogens are usually discovered after an increased prevalence of a particular birth defect. For example, in the early 1960s, a drug known as thalidomide was used to treat morning sickness. Exposure of the fetus during this early stage of development resulted in cases of phocomelia, a congenital malformation in which the hands and feet are attached to abbreviated arms and legs.
A Look at Some Teratogens
Alcohol

One of the most commonly used teratogens is alcohol. Because half of all pregnancies in the United States are unplanned, it is recommended that women of child-bearing age take great caution against drinking alcohol when not using birth control and when pregnant (Surgeon General’s Advisory on Alcohol Use During Pregnancy, 2005). Alcohol consumption, particularly during the second month of prenatal development, but at any point during pregnancy, may lead to neurocognitive and behavioral difficulties that can last a lifetime.
There is no acceptable safe limit for alcohol use during pregnancy, but binge drinking (5 or more drinks on a single occasion) or having 7 or more drinks during a single week places a child at particularly high risk. In extreme cases, alcohol consumption can lead to fetal death, but more frequently it can result in fetal alcohol spectrum disorders (FASD). This terminology is now used when looking at the effects of exposure and replaces the term fetal alcohol syndrome. It is preferred because it recognizes that symptoms occur on a spectrum and that all individuals do not have the same characteristics. Children with FASD share certain physical features such as flattened noses, small eye openings, small heads, intellectual developmental delays, and behavioral problems. Those with FASD are more at risk for lifelong problems such as criminal behavior, psychiatric problems, and unemployment (CDC, 2006).
The terms alcohol-related neurological disorder (ARND) and alcohol-related birth defects (ARBD) have replaced the term Fetal Alcohol Effects to refer to those with less extreme symptoms of FASD. ARBD includes kidney, bone, and heart problems.
Malnutrition
Pregnant women who are not getting enough calories and important micro-nutrients are at increased risk for having low birth weight babies (under 2,500 grams or 5 1/2 pounds) and other complications. One vital nutrient is folic acid, found in leafy green vegetables, legumes, egg yolk, liver, and citrus fruit (Greenberg et al., 2011). Folic acid deficiency during pregnancy is associated with neural tube disorders, like spina bifida, where the end of the spine does not close) and anencephaly, when the brain does not fully develop. Some common genetic variations reduce how women metabolize folic acid, which is why women of reproductive age are recommended to take 400 micrograms of folic acid each day (US Preventive Services Task Force, 2017).
Tobacco
Smoking is also considered a teratogen because nicotine travels through the placenta to the fetus. When the mother smokes, the developing baby experiences a reduction in blood oxygen levels. Tobacco use during pregnancy has been associated with low birth weight, placenta previa, birth defects, preterm delivery, fetal growth restriction, and sudden infant death syndrome. Smoking in the month before getting pregnant and throughout pregnancy increases the chances of these risks. Quitting smoking before getting pregnant is best. However, for women who are already pregnant, quitting as early as possible can still help protect against some health problems for the mother and baby.
Drugs
Prescription, over-the-counter, or recreational drugs can have serious teratogenic effects. In general, if medication is required, the lowest dose possible should be used. Combination drug therapies and first trimester exposures should be avoided. Almost three percent of pregnant women use illicit drugs such as marijuana, cocaine, ecstasy, and other amphetamines, and heroin. These drugs can cause low birth-weight, withdrawal symptoms, birth defects, or learning or behavioral problems. Babies born with a heroin addiction need heroin just like an adult addict. The child will need to be gradually weaned from the heroin under medical supervision; otherwise, the child could have seizures and die.
Environmental Chemicals
Environmental chemicals can include exposure to a wide array of agents including pollution, organic mercury compounds, herbicides, and industrial solvents. Some environmental pollutants of major concern include lead poisoning, which is connected with low birth weight and slowed neurological development. Children who live in older housing in which lead-based paints have been used have been known to eat peeling paint chips thus being exposed to lead. The chemicals in certain herbicides are also potentially damaging. Radiation is another environmental hazard that a pregnant woman must be aware of. If a mother is exposed to radiation, particularly during the first three months of pregnancy, the child may suffer some congenital deformities. There is also an increased risk of miscarriage and stillbirth. Mercury leads to physical deformities and intellectual disabilities (Dietrich, 1999).
Sexually Transmitted Infections
Sexually transmitted infections (STIs) can complicate pregnancy and may have serious effects on both the mother and the developing baby. Most prenatal care today includes testing for STIs, and early detection is important. STIs, such as chlamydia, gonorrhea, syphilis, trichomoniasis, and bacterial vaginosis can all be treated and cured with antibiotics that are safe to take during pregnancy. STIs that are caused by viruses, like genital herpes, hepatitis B, or HIV cannot be cured. However, in some cases these infections can be treated with antiviral medications or other preventive measures can be taken to reduce the risk of passing the infection to the baby.
Maternal Diseases
Maternal illnesses increase the chance that a baby will be born with a birth defect or have a chronic health problem. Some of the diseases that are known to potentially have an adverse effect on the fetus include diabetes, cytomegalovirus, toxoplasmosis, Rubella, varicella, hypothyroidism, and Strep B. If the mother contracts Rubella during the first three months of pregnancy, damage can occur in the eyes, ears, heart, or brain of the unborn child. On a positive note, Rubella has been nearly eliminated in the industrial world due to the vaccine created in 1969. Diagnosing these diseases early and receiving appropriate medical care can help improve the outcomes. Routine prenatal care now includes screening for gestational diabetes and Strep B.
Maternal Stress
Stress represents the effects of any factor able to threaten the homeostasis of an organism; these either real or perceived threats are referred to as the “stressors” and comprise a long list of potential adverse factors, which can be emotional or physical. Because of a link in blood supply between a mother and fetus, it has been found that stress can leave lasting effects on a developing fetus, even before a child is born. The best-studied outcomes of fetal exposure to maternal prenatal stress are preterm birth and low birth weight. Maternal prenatal stress is also considered responsible for a variety of changes of the child’s brain, and a risk factor for conditions such as behavioral problems, learning disorders, high levels of anxiety, attention deficit hyperactivity disorder, autism, and schizophrenia. Furthermore, maternal prenatal stress has been associated with a higher risk for a variety of immune and metabolic changes in the child such as asthma, allergic disorders, cardiovascular diseases, hypertension, hyperlipidemia, diabetes, and obesity (Konstantinos et al., 2017).
WHAT DO YOU THINK? Should Women Who Use Drugs During Pregnancy Be Arrested and Jailed?
As you now know, women who use drugs or alcohol during pregnancy can cause serious lifelong harm to their child. Some people have advocated mandatory screenings for women who are pregnant and have a history of drug abuse, and if the women continue using, to arrest, prosecute, and incarcerate them (Figdor & Kaeser, 1998). This policy was tried in Charleston, South Carolina, as recently as 20 years ago. The policy was called the Interagency Policy on Management of Substance Abuse During Pregnancy and had disastrous results.
The Interagency Policy applied to patients attending the obstetrics clinic at MUSC, which primarily serves patients who are indigent or on Medicaid. It did not apply to private obstetrical patients. The policy required patient education about the harmful effects of substance abuse during pregnancy. . . . [A] statement also warned patients that protection of unborn and newborn children from the harms of illegal drug abuse could involve the Charleston police, the Solicitor of the Ninth Judicial Court, and the Protective Services Division of the Department of Social Services (DSS). (Jos, Marshall, & Perlmutter, 1995, pp. 120–121)
This policy seemed to deter women from seeking prenatal care, deterred them from seeking other social services, and was applied solely to low-income women, resulting in lawsuits. The program was canceled after 5 years, during which 42 women were arrested. A federal agency later determined that the program involved human experimentation without the approval and oversight of an institutional review board (IRB). What were the flaws in the program and how would you correct them? What are the ethical implications of charging pregnant women with child abuse?
Factors influencing prenatal risks
There are several considerations in determining the type and amount of damage that might result from exposure to a particular teratogen (Berger, 2004). These include:
- The timing of the exposure: Structures in the body are vulnerable to the most severe damage when they are forming. If a substance is introduced during a particular structure’s critical period (time of development), the damage to that structure may be greater. For example, most organs are forming during the embryonic period, like the ears and arms reach their critical periods at about 6 weeks after conception. If a mother exposes the embryo to certain substances during this period, the arms and ears may be malformed.
- The amount of exposure: Some substances are not harmful unless the amounts reach a certain level. The higher the dose, the greater likelihood of harm. Also, the longer the duration, the greater the chance of harm. The critical level depends in part on the size and metabolism of the mother.
- Genetics: Genetic make-up also plays a role in the impact a particular teratogen might have on the child. This is suggested by fraternal twin studies who are exposed to the same prenatal environment, yet do not experience the same teratogenic effects. The genetic make-up of the mother can also have an effect; some mothers may be more resistant to teratogenic effects than others.
- Being male or female: Males are more likely to experience damage due to teratogens than are females. It is believed that the Y chromosome, which contains fewer genes than the X, may have an impact.

Complications of Pregnancy and Delivery

There are a number of common side effects of pregnancy. Not everyone experiences all of these nor do women experience them to the same degree. And although they are considered “minor” these problems are potentially very uncomfortable. These side effects include nausea (particularly during the first 3-4 months of pregnancy as a result of higher levels of estrogen in the system), heartburn, gas, hemorrhoids, backache, leg cramps, insomnia, constipation, shortness of breath or varicose veins (as a result of carrying a heavy load on the abdomen). What is the cure? Delivery!
Major Complications
The following are some serious complications of pregnancy that can pose health risks to mother and child and that often require special care.
- Gestational diabetes is when a woman without diabetes develops high blood sugar levels during pregnancy.
- Hyperemesis gravidarum is the presence of severe and persistent vomiting, causing dehydration and weight loss. It is more severe than the more common morning sickness.
- Preeclampsia is gestational hypertension. Severe preeclampsia involves blood pressure over 160/110 with additional signs. Eclampsia is seizures in a pre-eclamptic patient.
- Deep vein thrombosis is the formation of a blood clot in a deep vein, most commonly in the legs.
- A pregnant woman is more susceptible to infections. This increased risk is caused by an increased immune tolerance in pregnancy to prevent an immune reaction against the fetus.
- Peripartum cardiomyopathy is a decrease in heart function which occurs in the last month of pregnancy, or up to six months post-pregnancy.
Maternal Mortality
Maternal mortality is unacceptably high. About 295,000 women died during and following pregnancy and childbirth in 2017. The vast majority of these deaths (94%) occurred in low-resource settings, and most could have been prevented. The high number of maternal deaths in some areas of the world reflects inequalities in access to quality health services and highlights the gap between rich and poor. The MMR in low-income countries in 2017 is 462 per 100,000 live births versus 11 per 100,000 live births in high-income countries. The high number of maternal deaths in some areas of the world reflects inequities in access to health services and highlights the gap between rich and poor.
Women in less developed countries have, on average, many more pregnancies than women in developed countries, and their lifetime risk of death due to pregnancy is higher. A woman’s lifetime risk of maternal death is the probability that a 15-year-old woman will eventually die from a maternal cause. In high-income countries, this is 1 in 5400, versus 1 in 45 in low-income countries. Every day in 2017, approximately 810 women died from preventable causes related to pregnancy and childbirth.
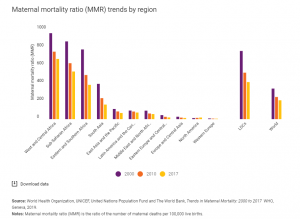
Figure 18. The number of women and girls who died each year from complications of pregnancy and childbirth declined from 451,000 in 2000 to 295,000 in 2017. These improvements are particularly remarkable in light of rapid population growth in many of the countries where maternal deaths are highest. Still, over 800 women are dying each day from complications in pregnancy and childbirth. And for every woman who dies, approximately 20 others suffer serious injuries, infections or disabilities (UNICEF, 2025). Even though maternal mortality in the United States is relatively rare today because of advances in medical care, it is still an issue that needs to be addressed. Sadly, about 700 women die each year in the United States as a result of pregnancy or delivery complications. The Centers for Disease Control and Prevention define a pregnancy-related death as the death of a woman while pregnant or within 1 year of the end of a pregnancy–regardless of the outcome, duration, or site of the pregnancy–from any cause related to or aggravated by the pregnancy or its management, but not from accidental or incidental causes.
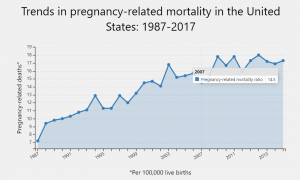
Since the Pregnancy Mortality Surveillance System was implemented, the number of reported pregnancy-related deaths in the United States steadily increased from 7.2 deaths per 100,000 live births in 1987 to 17.3 deaths per 100,000 live births in 2017. The graph above shows trends in pregnancy-related mortality ratios between 1987 and 2017 (the latest available year of data).
The reasons for the overall increase in pregnancy-related mortality are unclear. What do you think are some reasons for this surprising increase in the United States? What can be done to change this statistic?
Watch It: Maternal Mortality in the United States
In the United States, black women are disproportionately more likely to die from complications related to pregnancy or childbirth than any other race; they are three or four times more likely than white women to die due to pregnancy-related death and are more likely to receive worse maternal care. Black women from higher income groups and with advanced education levels also have heightened risks—even tennis superstar Serena Williams had near-deadly complications during the birth of her daughter, Olympia. Why is this the case in our modern world? Watch this video to learn more.
Considerable racial/ethnic disparities in pregnancy-related mortality exist.2,3 During 2014–2017, the pregnancy-related mortality ratios were:
- 41.7 deaths per 100,000 live births for non-Hispanic Black women.
- 28.3 deaths per 100,000 live births for non-Hispanic American Indian or Alaska Native women.
- 13.8 deaths per 100,000 live births for non-Hispanic Asian or Pacific Islander women.
- 13.4 deaths per 100,000 live births for non-Hispanic White women.
- 11.6 deaths per 100,000 live births for Hispanic or Latina women.
Variability in the risk of death by race/ethnicity may be due to several factors including access to care, quality of care, prevalence of chronic diseases, structural racism, and implicit biases.
Why do Women Die in Pregnancy and Childbirth Worldwide?
Women die as a result of complications during and following pregnancy and childbirth. Most of these complications develop during pregnancy and most are preventable or treatable. Other complications may exist before pregnancy but are worsened during pregnancy, especially if not managed as part of the woman’s care. The major complications that account for nearly 75% of all maternal deaths are:
- severe bleeding (mostly bleeding after childbirth)
- infections (usually after childbirth)
- high blood pressure during pregnancy (pre-eclampsia and eclampsia)
- complications from delivery
The remainder are caused by or associated with infections such as malaria or related to chronic conditions like cardiac diseases or diabetes.
Why do Women Die in Pregnancy and Childbirth in the United States?
Compare the data that you learned about above with percentages of pregnancy-related deaths in the United States during 2014–2017.
- Other cardiovascular conditions, 15.5%.
- Infection or sepsis, 12.7%.
- Cardiomyopathy, 11.5%.
- Hemorrhage, 10.7%.
- Thrombotic pulmonary or other embolism, 9.6%.
- Cerebrovascular accidents, 8.2%.
- Hypertensive disorders of pregnancy, 6.6%.
- Amniotic fluid embolism, 5.5%.
- Anesthesia complications, 0.4%.
- Other noncardiovascular medical conditions, 12.5%.
The cause of death is unknown for 6.7% of all 2014–2017 pregnancy-related deaths.
While the contributions of hemorrhage, hypertensive disorders of pregnancy (i.e., preeclampsia, eclampsia), and anesthesia complications to pregnancy-related deaths have declined, the contributions of cardiovascular, cerebrovascular accidents, and other medical conditions have increased.12 Studies show that an increasing number of pregnant women in the United States have chronic health conditions such as hypertension,13,14 diabetes,14-17 and chronic heart disease.12,18 These conditions may put a woman at higher risk of complications during pregnancy or in the year postpartum.
Miscarriage
Pregnancy loss is experienced in an estimated 20-40 percent of undiagnosed pregnancies and in another 10 percent of diagnosed pregnancies. Usually, the body aborts due to chromosomal abnormalities and this typically happens before the 12th week of pregnancy. Cramping and bleeding result and normal periods should return after several months. Or it may be necessary to have a surgical procedure called D&E (dilation and evacuation). Some women are more likely to have repeated miscarriages due to chromosomal, amniotic, or hormonal problems; but miscarriage can also be a result of defective sperm (Carroll et al., 2003).
In the U.S., a pregnancy loss before the 20th week of pregnancy is referred to as a miscarriage, while the term stillbirth refers to the loss of a baby after 20 weeks’ gestation. A woman must still go through labor or a c-section to deliver her baby. Stillbirth affects about 1 in 160 births, and each year about 24,000 babies are stillborn in the United States. That is about the same number of babies that die during the first year of life and it is more than 10 times as many deaths as the number that occur from Sudden Infant Death Syndrome (SIDS).
Conclusions
As you can see, what may seem like a simple process is in fact a beautiful and delicate journey. Each pregnancy and birth story is unique and comes with surprises and sometimes challenges. As medical technology has rapidly improved, women are empowered with more information and more choices when it comes to their pregnancy and birth. However, just because interventions are available does not mean that this is the path for all mothers. As we learned in the case with Serena Williams, even in the U.S. sometimes medical care can go awry. Each mother needs to be an active advocate for herself and her baby during her pregnancy and delivery.
Where do you think we are headed with how medical advances are used in pregnancy and delivery? More women are able to get pregnant with reproductive assistance, oftentimes past the age that they would naturally conceive. At the beginning of the module, the topic of “designer babies” was introduced. After completing this module, do you think that we are headed towards this in the near future? What are the ethical ramifications?
Additional Supplemental Resources
Websites
- The Human Genome Project (Links to an external site.)
- The Human Genome Project (HGP) was an inward voyage of discovery led by an international team of researchers looking to sequence and map all of the genes — together known as the genome — of members of our species, Homo sapiens. Beginning in October 1990 and completed in April 2003, the HGP gave us the ability, for the first time, to read nature’s complete genetic blueprint for building a human being.
- Institute for Behavioral Genetics (Links to an external site.)
- Founded in 1967, IBG is one of the top research facilities in the world for genetic research on behavior. Data collection and analysis are ongoing for several internationally renowned studies including the Colorado Adoption Project, the Colorado Twin Registry, the National Youth Survey Family Study, the Colorado Learning Disabilities Research Center, and the National Longitudinal Study of Adolescent Health.
Videos
- Fertilization
- This video, created by Nucleus Medical Media, shows human fertilization, also known as conception. Shown at a cellular level magnification, sperm struggle through many obstacles in the female reproductive tract to reach the egg. Then genetic material from the egg and a single sperm combines to form a new human being.
- Conception to birth- Visualized
- Image-maker Alexander Tsiaras shares a powerful medical visualization, showing human development from conception to birth and beyond.
- What are DNA and Genes?
- The Genetic Science Learning Center sponsored by the University of Utah delivers educational materials on genetics, bioscience, and health topics. All humans have the same genes arranged in the same order. And more than 99.9% of our DNA sequence is the same. But the few differences between us (all 1.4 million of them!) are enough to make each one of us unique.
- What is Inheritance?
- The Genetic Science Learning Center sponsored by the University of Utah delivers educational materials on genetics, bioscience, and health topics. This video explains the importance of genetic variation.
- Down Syndrome- Ability Awareness
- What comes to mind when you think of a person who has Down Syndrome? Do you have a preconceived idea of what their abilities might be? Chris Burke talks about his experience and his work at the National Down Syndrome Society.
- Prenatal Testing Options
- The University of Michigan provides this video that explains the difference between prenatal screening and diagnostic testing. Pregnant women are faced with the decision of whether to undergo prenatal screening and testing – and, if so – which of the many options to choose from.
- Prenatal Development: What We Learn Inside the Womb
- Let’s watch what we experience and learn inside the womb from the fetus’ perspective.
- TED talk: How CRISPR lets us Edit our DNA
- Geneticist Jennifer Doudna co-invented a groundbreaking new technology for editing genes, called CRISPR-Cas9. The tool allows scientists to make precise edits to DNA strands, which could lead to treatments for genetic diseases … but could also be used to create so-called “designer babies.” Doudna reviews how CRISPR-Cas9 works — and asks the scientific community to pause and discuss the ethics of this new tool.
