What are physical changes during adulthood?

Hippocrates (author of the famous “Hippocratic oath”) was of the opinion that “walking is the best medicine.” This was his learned opinion in 400 BCE and there is now considerable, and increasing, evidence that he may have been correct.
As we will see, there are simple physiological changes that accompany middle adulthood. Senescence or the gradual decline in organ functioning due to age, will be covered in greater detail when we get to late adulthood. These changes are somewhat inevitable, but modifiable by lifestyle factors: the importance of physical activity would be difficult to overstate looking at the evidence. Exercise does not necessarily mean running marathons, it may simply mean a commitment to using your legs in a brisk fashion for thirty minutes. “Use it or lose it” is a good mantra for this stage of development—the technical term for the loss of muscle tissue and function as we age is sarcopenia. From age 30, the body loses 3-8% of its muscle mass per decade, and this accelerates after the age of 60 (Volpi et al., 2010). Diet and exercise can ameliorate both the extent and lifestyle consequences of these kinds of processes. In this section, we will examine some of the changes associated with middle adulthood and consider how they impact human life.
Learning Objectives
- Detail the most important physiological changes occurring in men and women during middle adulthood
- Describe how physiological changes during middle adulthood can impact life experience, health, and sexuality

Physical Mobility in Middle Adulthood
The importance of not succumbing to the temptations of a sedentary lifestyle was as obvious to Hippocrates in 400 BCE as it is now. Piasecki et al. (2018) are of the opinion that sarcopenia (loss of muscle tissue and function as we age) in legs might be the result of leg muscles becoming detached from the nervous system. Further, Piasescki et al. (2018) believe that exercise encourages new nerve growth slowing the progression of sarcopenia. Persons aged 75 may have up to 30-60% fewer nerve endings in their leg muscles than they did in their early 20s.
Sarcopenia has only recently been recognized as an independent disease entity since 2016 (ICD-10). In 2018 the U.S. Center for Disease Control and prevention assigned sarcopenia its own discrete medical code. Disease entities that affect mobility will become an increasingly costly phenomenon and will affect the quality of life of millions of people as the population ages. In many ways, it is a natural phenomenon, and many doctors and researchers have been reticent to overly pathologize natural changes associated with age. However, mobility is now becoming a central concern, and some researchers are now identifying some conditions like osteosarcopenia, which describes the decline of both muscle tissue (sarcopenia) and bone tissue (osteoporosis). Diagnoses and pharmaceuticals which deal with the central question of mobility will become ever more important, even more so as the burgeoning costs associated with caring for those with mobility issues become apparent.
The years between 30 and 60 can see the onset of rheumatoid arthritis (RA). This is the third most common form of arthritis and its specific etiology is unknown at this time. RA occurs when antibodies attack normal synovial fluid in the joints mistaking them for an alien threat. It affects women more than men by a factor of around 3 to 1. Peak onset for women is reckoned to be sometime in the early 40s. This has led to the conclusion, albeit a preliminary one, that RA is caused by hormonal changes. Women who are pregnant, and have RA, often experience a temporary remission, again leading to the identification of hormonal changes in the body as the most likely culprit. Women also experience symptoms at an earlier age. This condition is often associated with people in their 60s, but only about a third first experience symptoms at this age, though they become more acute with the passage of time.
Human beings reach peak bone mass around 35-40. Osteoporosis is a “silent disease” which progresses until a fracture occurs. The sheer scale and cost of this illness is radically underestimated. It is often associated with women due to the fact that bone mass can deteriorate in women much more quickly in middle age due to menopause. After menopause women can lose 5-10% bone mass per year, rendering it advisable to monitor intakes of calcium and Vitamin D, and evaluate individual risk factors. Beginning in their 60s, though, men and women lose bone mass at roughly the same rate. The number of American men diagnosed with osteoporosis is currently around the 2 million mark, with a further 12 million reckoned to be at risk. The National Osteoporosis Foundation (NOF) estimates that 50% of women and 25% of men over the age of 50 will suffer a bone fracture due to osteoporosis. Attention at this stage of life may bring pronounced health benefits now and later for both women and men. Fixing the damage takes a considerable amount of the Medicare budget.
The health benefits that walking and other physical activity have on the nervous system are becoming increasingly obvious to those who study aging. Adami et al (2018) found pronounced links between weight-bearing exercise and neuron production. We tend to think of the brain as a central processing unit giving instructions to the body via the conduit of the central nervous system, but contemporary science is now coalescing around the idea that muscles and nerves also communicate with the brain—it is a two-way informational and sustaining process. Many studies suggest that voluntary physical activity (VPA) extends and improves the quality of life. Such studies show that even moderate physical activity can bring large gains.
In addition, there is often an increase in chronic inflammation at this time of life with no discernible discrete cause (as opposed to acute inflammation associated with something like an infection). Inflammation is the body’s natural way of responding to injury or harmful pathogens in the body. The function of inflammation is to eliminate the initial cause of injury and initiate tissue repair, but when this happens consistently and for longer periods of time, the body’s stress response systems become overworked. This can have serious effects on health, such as fatigue, fever, chest or abdominal pain, rashes, or greater susceptibility to diseases such as cancer, rheumatoid arthritis, and heart disease. Untreated acute inflammation, autoimmune disorders, or long-term exposure to irritants are some contributing factors, as is social isolation (Nersessian et al, 2018).
Chronic inflammation has been implicated as part of the cause of the muscle loss that occurs with aging. Chronic inflammatory disorder is now implicated in a whole series of chronic diseases such as dementia, and the biomedical evidence for its centrality is now emerging in the medical research literature.
Because of the aging population, health issues associated with autoimmune disease, chronic inflammation, and bone mass density will become central concerns in health and social policy in the coming decades.
Normal Physiological Changes in Middle Adulthood
There are a few primary biological physical changes in midlife. There are changes in vision, hearing, more joint pain, and weight gain (Lachman, 2004). Vision is affected by age. As we age, the lens of the eye gets larger but the eye loses some of the flexibility required to adjust to visual stimuli. This is known as presbyopia. Middle-aged adults often have trouble seeing up close and many need reading glasses. Night vision is also affected as the pupil loses some of its ability to open and close to accommodate drastic changes in light.
Presbycusis is the most common cause of hearing loss, afflicting one out of four persons between ages 65 and 74, and one out of two by age 75. This loss accumulates after years of being exposed to intense noise levels and is generally due to the loss or damage of nerve hair cells inside the cochlea. It is more common in men, but men are also more likely to work in noisy occupations, which may explain their nearly doubled rates of hearing loss levels. Hearing loss is also exacerbated by cigarette smoking, high blood pressure, and stroke. High-frequency sounds are the first affected by such hearing loss. Hearing loss could be prevented by guarding against being exposed to extremely noisy environments.
There is new concern over hearing loss as early as childhood with the widespread use of headphones, as loud and/or prolonged listening can cause damage to the cilia, or the tiny sensory hairs, within the cochlea. Another cause of hearing loss in middle age is otosclerosis, a physiological condition affecting the middle ear and its bone structure. This occurs when one of the bones in the middle ear, the stapes, acquires a rigidity via abnormal bone growth which it should not have. Unable to vibrate, it induces hearing impairment. Otosclerosis is often described as a rare condition, but it afflicts a good number of Americans, with white women being more prone, though there has been some speculation that this was the origin of deafness in the composer Beethoven. Its cause is unknown, but chronic inflammation may be a risk factor. We tend to associate hearing loss with older adults, but the peak onset is in the middle adulthood age bracket.
Weight gain, sometimes referred to as the middle-aged spread, or the accumulation of fat in the abdomen is one of the common complaints of midlife adults. Men tend to gain fat on their upper abdomen and back while women tend to gain more fat on their waist and upper arms. On average, American adults gain 1-2 pounds per year through their 20’s, 30’s, 40’s and 50’s (Zheng et al., 2017). Greater weight gain increases the risk of chronic diseases. Many adults are surprised at this weight gain because their diets have not changed, but it’s likely their activity level has. It was formerly believed that metabolism slows during adulthood, but a large study of 6,500 people from newborns to 95-year-olds found that it didn’t (Pontzer et al., 2021). Metabolism is fastest in the first year of life then gradually slows until around 20. During adulthood, between 20 and 60-years-old, metabolism was steady and then started declining after 60 (Pontzer et al., 2021). Adults have to pay more attention to their activity levels and eating habits to stay healthy and maintain their earlier physique.
Many of the changes that occur in midlife can be easily compensated for (by buying glasses, exercising, and watching what one eats, for example.) Most midlife adults experience generally good health. However, the percentage of adults who have a disability increases through midlife; while 7 percent of people in their early 40s have a disability, the rate jumps to 30 percent by the early 60s. This increase is highest among those of lower socioeconomic status (Bumpass & Aquilino, 1995).
What can we conclude from this information? Again, lifestyle has a strong impact on the health status of midlife adults. Smoking tobacco, drinking alcohol, poor diet, stress, physical inactivity, and chronic diseases such as diabetes or arthritis reduce overall health. It becomes important for midlife adults to take preventative measures to enhance physical well-being. Those midlife adults who have a strong sense of mastery and control over their lives, who engage in challenging physical and mental activity, who engage in weight-bearing exercise, monitor their nutrition, and make use of social resources are most likely to enjoy a plateau of good health through these years. Not only that, but those who begin an exercise regimen in their 40s may enjoy comparable benefits to those who began in their 20s according to Saint-Maurice et al. (2019), who also found that while it is never too late to begin, continuing to do as much as possible, is just as important.
The Climacteric
One biologically based change that occurs during midlife is the climacteric. During midlife, men may experience a reduction in their ability to reproduce. Women, however, lose their ability to reproduce once they reach menopause.
Menopause
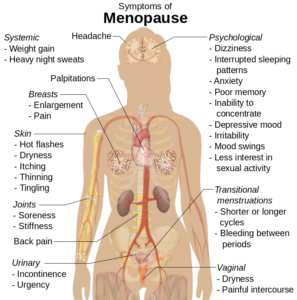
Menopause refers to a period of transition in which a woman’s ovaries stop releasing eggs and the level of estrogen and progesterone production decreases. After menopause, a woman’s menstruation ceases (U. S. National Library of Medicine and National Institute of Health [NLM/NIH], 2007).
Changes typically occur between the mid-40s and mid-50s. The median age range for a woman to have her last menstrual period is 50-52, but ages vary. A woman may first begin to notice that her periods are more or less frequent than before. These changes in menstruation may last from 1 to 3 years. After a year without menstruation, a woman is considered menopausal and no longer capable of reproduction. (Keep in mind that some women, however, may experience another period even after going for a year without one.) The loss of estrogen also affects vaginal lubrication which diminishes and becomes more watery. The vaginal wall also becomes thinner, and less elastic.
Menopause is not seen as universally distressing (Lachman, 2004). Changes in hormone levels are associated with hot flashes and sweats in some women, but women vary in the extent to which these are experienced. Depression, irritability, and weight gain are not necessarily due to menopause (Avis, 1999; Rossi, 2004). Depression and mood swings are more common during menopause in women who have prior histories of these conditions rather than those who have not. The incidence of depression and mood swings is not greater among menopausal women than non-menopausal women.
Cultural influences seem to also play a role in the way menopause is experienced. For example, once after listing the symptoms of menopause in a psychology course, a woman from Kenya responded, “We do not have this in my country or if we do, it is not a big deal,” to which some U.S. students replied, “I want to go there!” Indeed, there are cultural variations in the experience of menopausal symptoms. Hot flashes are experienced by 75 percent of women in Western cultures, but by less than 20 percent of women in Japan (Obermeyer in Berk, 2007).
Women in the United States respond differently to menopause depending upon the expectations they have for themselves and their lives. White, career-oriented women, African-American, and Mexican-American women overall tend to think of menopause as a liberating experience. Nevertheless, there has been a popular tendency to erroneously attribute frustrations and irritations expressed by women of menopausal age to menopause and thereby not take her concerns seriously. Fortunately, many practitioners in the United States today are normalizing rather than pathologizing menopause.
Concerns about the effects of hormone replacement have changed the frequency with which estrogen replacement and hormone replacement therapies have been prescribed for menopausal women. Estrogen replacement therapy was once commonly used to treat menopausal symptoms. But more recently, hormone replacement therapy has been associated with breast cancer, stroke, and the development of blood clots (NLM/NIH, 2007). Most women do not have symptoms severe enough to warrant estrogen or hormone replacement therapy (HRT). Women who do require HRT can be treated with lower doses of estrogen and monitored with more frequent breast and pelvic exams. There are also some other ways to reduce symptoms. These include avoiding caffeine and alcohol, eating soy, remaining sexually active, practicing relaxation techniques, and using water-based lubricants during intercourse.
Fifty million women in the USA aged 50-55 are post-menopausal. During and after menopause a majority of women will experience weight gain. Changes in estrogen levels lead to a redistribution of body fat from hips and back to stomachs. This is more dangerous to general health and wellbeing because abdominal fat is largely visceral, meaning it is contained within the abdominal cavity and may not look like typical weight gain. That is, it accumulates in the space between the liver, intestines, and other vital organs. This is far more harmful to health than subcutaneous fat which is the kind of fat located under the skin. It is possible to be relatively thin and retain a high level of visceral fat, yet this type of fat is deemed especially harmful by medical research.
Andropause
Do males experience a climacteric? Yes. While they do not lose their ability to reproduce as they age, they do tend to produce lower levels of testosterone and fewer sperm. However, men are capable of reproduction throughout life after puberty. It is natural for sex drive to diminish slightly as men age, but a lack of sex drive may be a result of extremely low levels of testosterone. About 5 million men experience low levels of testosterone that results in symptoms such as a loss of interest in sex, loss of body hair, difficulty achieving or maintaining an erection, loss of muscle mass, and breast enlargement. This decrease in libido and lower testosterone (androgen) levels is known as andropause, although this term is somewhat controversial as this experience is not clearly delineated, as menopause is for women. Low testosterone levels may be due to glandular diseases such as testicular cancer. Testosterone levels can be tested and if they are low, men can be treated with testosterone replacement therapy. This can increase sex drive, muscle mass, and beard growth. However, long term HRT for men can increase the risk of prostate cancer (The Patient Education Institute, 2005).
The debate around declining testosterone levels in men may hide a fundamental fact. The issue is not about individual males experiencing individual hormonal change at all. We have all seen the adverts on the media promoting substances to boost testosterone: “Is it low-T?” The answer is probably in the affirmative, if somewhat relative. That is, in all likelihood, they will have lower testosterone levels than their fathers. However, it is equally likely that the issue does not lie solely in their individual physiological makeup, but is rather a generational transformation (Travison et al, 2007). Why this has occurred in such a dramatic fashion is still unknown. There is evidence that low testosterone may have negative health effects on men. In addition, there are studies that show evidence of rapidly decreasing sperm count and grip strength. Exactly why these changes are happening is unknown and will likely involve more than one cause.
The Climacteric and Sexuality
Sexuality is an important part of people’s lives at any age. Midlife adults tend to have sex lives that are very similar to that of younger adults. And many women feel freer and less inhibited sexually as they age. However, a woman may notice less vaginal lubrication during arousal and men may experience changes in their erections from time to time. This is particularly true for men after age 65. Men who experience consistent problems are likely to have other medical conditions (such as diabetes or heart disease) that impact sexual functioning (National Institute on Aging, 2005).
Couples continue to enjoy physical intimacy and may engage in more foreplay, oral sex, and other forms of sexual expression rather than focusing as much on sexual intercourse. The risk of pregnancy continues until a woman has been without menstruation for at least 12 months, however, and couples should continue to use contraception. People continue to be at risk of contracting sexually transmitted infections such as genital herpes, chlamydia, and genital warts. Seventeen percent of new cases of AIDS in the United States are in people 50 and older. Of all people living with HIV, 47% are aged 50 or over. Practicing safe sex is important at any age- safe sex is not just about avoiding an unwanted pregnancy… it is about protecting yourself from STIs (sexually transmitted infections) as well. Hopefully, when partners understand how aging affects sexual expression, they will be less likely to misinterpret these changes as a lack of sexual interest or displeasure in the partner and be more able to continue to have satisfying and safe sexual relationships.
Exercise, Nutrition, and Health
The impact of exercise

Exercise is a powerful way to combat the changes we associate with aging. Exercise builds muscle, increases metabolism, helps control blood sugar, increases bone density, and relieves stress. Unfortunately, fewer than half of midlife adults exercise and only about 20 percent exercise frequently and strenuously enough to achieve health benefits. Many stop exercising soon after they begin an exercise program-particularly those who are very overweight. The best exercise programs are those that are engaged in regularly—regardless of the activity, but a well-rounded program that is easy to follow includes walking and weight training. Having a safe, enjoyable place to walk can make a difference in whether or not someone walks regularly. Weight lifting and stretching exercises at home can also be part of an effective program. Exercise is particularly helpful in reducing stress in midlife. Walking, jogging, cycling, or swimming can release the tension caused by stressors, and learning relaxation techniques can have healthful benefits. Exercise can be thought of as preventative health care; promoting exercise for the 78 million “baby boomers” may be one of the best ways to reduce health care costs and improve quality of life (Shure & Cahan, 1998).
Nutrition
Aging brings about a reduction in the number of calories a person requires. Many Americans respond to weight gain by dieting. However, eating less does not necessarily mean eating right and people often suffer vitamin and mineral deficiencies as a result. Very often, physicians will recommend vitamin supplements to their middle-aged patients. As stated above, chronic inflammation is now identified as one of the so-called “pillars of aging”. The link between diet and inflammation is yet unclear, but there is now some information available on the Diet Inflammation Index (Shivappa et al., 2014)., which in popular parlance, supports a diet rich in plant-based foods, healthy fats, nuts, fish in moderation, and sparing use of red meat— often referred to as “the Mediterranean Diet.”
The ideal diet is one low in fat, low in sugar, high in fiber, low in sodium, and low in cholesterol. In 2005, the Food Pyramid, a set of nutritional guidelines established by the U. S. Government was updated to accommodate new information on nutrition and to provide people with guidelines based on age, sex, and activity levels. The ideal diet is low in sodium (less than 2300 mg per day). Sodium causes fluid retention which may, in turn, exacerbate high blood pressure. The ideal diet is also low in cholesterol (less than 300 mg per day) and high in fiber. Fiber is thought to reduce the risk of certain cancers and heart disease. Finally, an ideal diet is low in sugar. Sugar is not only a problem for diabetics; it is also a problem for most people. Sugar satisfies the appetite but provides no protein, vitamins, or minerals. It provides empty calories. High starch diets are also a problem because starch is converted to sugar in the body. A 1-2 ounce serving of red wine (or grape juice) may have beneficial effects on health, as red wine can increase “good cholesterol” or HDLs (high-density lipoproteins) in the blood and provide antioxidants important for combating aging.
