What are physical changes in late adulthood?
 In this section, you’ll learn more about physical changes in late adulthood. While late adulthood is generally a time of physical decline, there are no set rules as to when and how it happens. We are continually learning more about how to promote greater health during the aging process.
In this section, you’ll learn more about physical changes in late adulthood. While late adulthood is generally a time of physical decline, there are no set rules as to when and how it happens. We are continually learning more about how to promote greater health during the aging process.
Learning Objectives
- Describe age categories of late adulthood
- Explain trends in life expectancies, including factors that contribute to longer life
- Describe primary aging, including vision and hearing loss
- Explain secondary aging concerns that are common in late adulthood, including illnesses and diseases
- Describe and compare theories of aging
Defining Late Adulthood
Defining Late Adulthood: Age or Quality of Life?

We are considered in late adulthood from the time we reach our mid-sixties until death. Because we are living longer, late adulthood is getting longer. Whether we start counting at 65, as demographers may suggest, or later, there is a greater proportion of people alive in late adulthood than at any time in world history.
About 15.2 percent of the U.S. population or 49.2 million Americans are 65 and older (US Census Bureau, 2018). This number is expected to grow to 98.2 million by the year 2060, at which time people in this age group will comprise nearly one in four U.S. residents. Of this number, 19.7 million will be age 85 or older. Developmental changes vary considerably among this population, so it is further divided into categories of 65 plus, 85 plus, and centenarians for comparison by the census.
Demographers use chronological age categories to classify individuals in late adulthood. Developmentalists, however, divide this population into categories based on physical and psychosocial well-being, in order to describe one’s functional age. The “young old” are healthy and active. The “old old” experience some health problems and difficulty with daily living activities. The “oldest old” are frail and often in need of care. A 98-year-old woman who still lives independently has no major illnesses, and is able to take a daily walk would be considered as having a functional age of “young old”. Therefore, optimal aging refers to those who enjoy better health and social well-being than average.
Normal aging refers to those who seem to have the same health and social concerns as most of those in the population. However, there is still much being done to understand exactly what normal aging means. Impaired aging refers to those who experience poor health and dependence to a greater extent than would be considered normal. Aging successfully involves making adjustments as needed in order to continue living as independently and actively as possible. This is referred to as selective optimization with compensation. Selective Optimization With Compensation is a strategy for improving health and well being in older adults and a model for successful aging. It is recommended that seniors select and optimize their best abilities and most intact functions while compensating for declines and losses. This means, for example, that a person who can no longer drive, is able to find alternative transportation or a person who is compensating for having less energy learns how to reorganize the daily routine to avoid over-exertion. Perhaps nurses and other allied health professionals working with this population will begin to focus more on helping patients remain independent by optimizing their best functions and abilities rather than simply treating illnesses. Promoting health and independence are essential for successful aging.
Age Categories
Senescence, or biological aging, is the gradual deterioration of functional characteristics.

The Young Old—65 to 74
These 18.3 million Americans tend to report greater health and social well-being than older adults. Having good or excellent health is reported by 41 percent of this age group (Center for Disease Control, 2004). Their lives are more similar to those of midlife adults than those who are 85 and older. This group is less likely to require long-term care, to be dependent or to be poor, and more likely to be married, working for pleasure rather than income, and living independently. About 65 percent of men and 50 percent of women between the ages of 65-69 continue to work full-time (He et al., 2005).
Physical activity tends to decrease with age, despite the dramatic health benefits enjoyed by those who exercise. People with more education and income are more likely to continue being physically active. And males are more likely to engage in physical activity than are females. The majority of the young-old continue to live independently. Only about 3 percent of those 65-74 need help with daily living skills as compared with about 22.9 percent of people over 85. (Another way to consider think of this is that 97 percent of people between 65-74 and 77 percent of people over 85 do not require assistance!) This age group is less likely to experience heart disease, cancer, or stroke than the old, but nearly as likely to experience depression (U.S. Census, 2005).
The Old Old—75 to 84
This age group is more likely to experience limitations on physical activity due to chronic diseases such as arthritis, heart conditions, hypertension (especially for women), and hearing or visual impairments. Rates of death due to heart disease, cancer, and cerebral vascular disease are double that experienced by people 65-74. Poverty rates are 3 percent higher (12 percent) than for those between 65 and 74. However, the majority of these 12.9 million Americans live independently or with relatives. Widowhood is more common in this group-especially among women.
The Oldest Old—85 plus
The number of people 85 and older is 34 times greater than in 1900 and now includes 5.7 million Americans. This group is more likely to require long-term care and to be in nursing homes. However, of the 38.9 million Americans over 65, only 1.6 million require nursing home care. Sixty-eight percent live with relatives and 27 percent live alone (He et al., 2005; U. S. Census Bureau, 2011).
The Centenarians
Centenarians, or people aged 100 or older, are both rare and distinct from the rest of the older population. Although uncommon, the number of people living past age 100 is on the rise; between the years 2000 and 2014, then the number of centenarians increased by over 43.6%, from 50,281 in 2000 to 72,197 in 2014. In 2010, over half (62.5 percent) of the 53,364 centenarians were age 100 or 101.
This number is expected to increase to 601,000 by the year 2050 (U. S. Census Bureau, 2011). The majority is between ages 100 and 104 and eighty percent are women. Out of almost 7 billion people on the planet, about 25 are over 110. Most live in Japan, a few live in the United States, and three live in France (National Institutes of Health, 2006). These “super-Centenarians” have led varied lives and probably do not give us any single answers about living longer. Jeanne Clement smoked until she was 117. She lived to be 122. She also ate a diet rich in olive oil and rode a bicycle until she was 100. Her family had a history of longevity. Pitskhelauri (in Berger, 2005) suggests that moderate diet, continued work and activity, inclusion in family and community life, and exercise and relaxation are important ingredients for long life.
Blue Zones
Recent research on longevity reveals that people in some regions of the world live significantly longer than people elsewhere. Efforts to study the common factors between these areas and the people who live there is known as blue zone research. Blue zones are regions of the world where Dan Buettner claims people live much longer than average. The term first appeared in his November 2005 National Geographic magazine cover story, “The Secrets of a Long Life.” Buettner identified five regions as “Blue Zones”: Okinawa (Japan); Sardinia (Italy); Nicoya (Costa Rica); Icaria (Greece); and the Seventh-day Adventists in Loma Linda, California. He offers an explanation, based on data and first hand observations, for why these populations live healthier and longer lives than others.
The people inhabiting blue zones share common lifestyle characteristics that contribute to their longevity. The Venn diagram below highlights the following six shared characteristics among the people of Okinawa, Sardinia, and Loma Linda blue zones. Though not a lifestyle choice, they also live as isolated populations with a related gene pool.
- Family – put ahead of other concerns
- Less smoking
- Semi-vegetarianism – the majority of food consumed is derived from plants
- Constant moderate physical activity – an inseparable part of life
- Social engagement – people of all ages are socially active and integrated into their communities
- Legumes – commonly consumed
In his book, Buettner provides a list of nine lessons, covering the lifestyle of blue zones people:
- Moderate, regular physical activity.
- Life purpose.
- Stress reduction.
- Moderate caloric intake.
- Plant-based diet.
- Moderate alcohol intake, especially wine.
- Engagement in spirituality or religion.
- Engagement in family life.
- Engagement in social life.
The “Graying” Population and Life Expectancy
The “Graying” of America
The term “graying of America” refers to the fact that the American population is steadily becoming more dominated by older people. In other words, the median age of Americans is going up.
According to the U.S. Census Bureau’s 2017 National Population Projections, the year 2030 marks an important demographic turning point in U.S. history. By 2030, all baby boomers will be older than age 65. This will expand the size of the older population so that 1 in every 5 residents will be retirement age. And by 2035, it’s projected that there will be 76.7 million people under the age of 18 but 78 million people above the age of 65.

The 2030s are projected to be a transformative decade for the U.S. population. The population is expected to grow at a slower pace, age considerably and become more racially and ethnically diverse. Net international migration is projected to overtake natural increase in 2030 as the primary driver of population growth in the United States, another demographic first for the United States.
Although births are projected to be nearly four times larger than the level of net international migration in coming decades, a rising number of deaths will increasingly offset how much births are able to contribute to population growth. Between 2020 and 2050, the number of deaths is projected to rise substantially as the population ages and a significant share of the population, the baby boomers, age into older adulthood. As a result, the population will naturally grow very slowly, leaving net international migration to overtake natural increase as the leading cause of population growth, even as projected levels of migration remain relatively constant.
“Graying” Around the World
While the world’s oldest countries are mostly in Europe today, some Asian and Latin American countries are quickly catching up. The percentage of the population aged 65 and over in 2015 ranged from a high of 26.6 percent for Japan to a low of around 1 percent for Qatar and United Arab Emirates. Of the world’s 25 oldest countries, 22 are in Europe, with Germany and Italy leading the ranks of European countries for many years (He, Goodkind, & Kowal, 2015).
By 2050, Slovenia and Bulgaria are projected to be the oldest European countries. Japan, however, is currently the oldest nation in the world and is projected to retain this position through at least 2050. With the rapid aging taking place in Asia, the countries of South Korea, Hong Kong, and Taiwan are projected to join Japan at the top of the list of oldest countries and areas by 2050, when more than one-third of these Asian countries’ total populations are projected to be aged 65 and over.
Life Expectancy
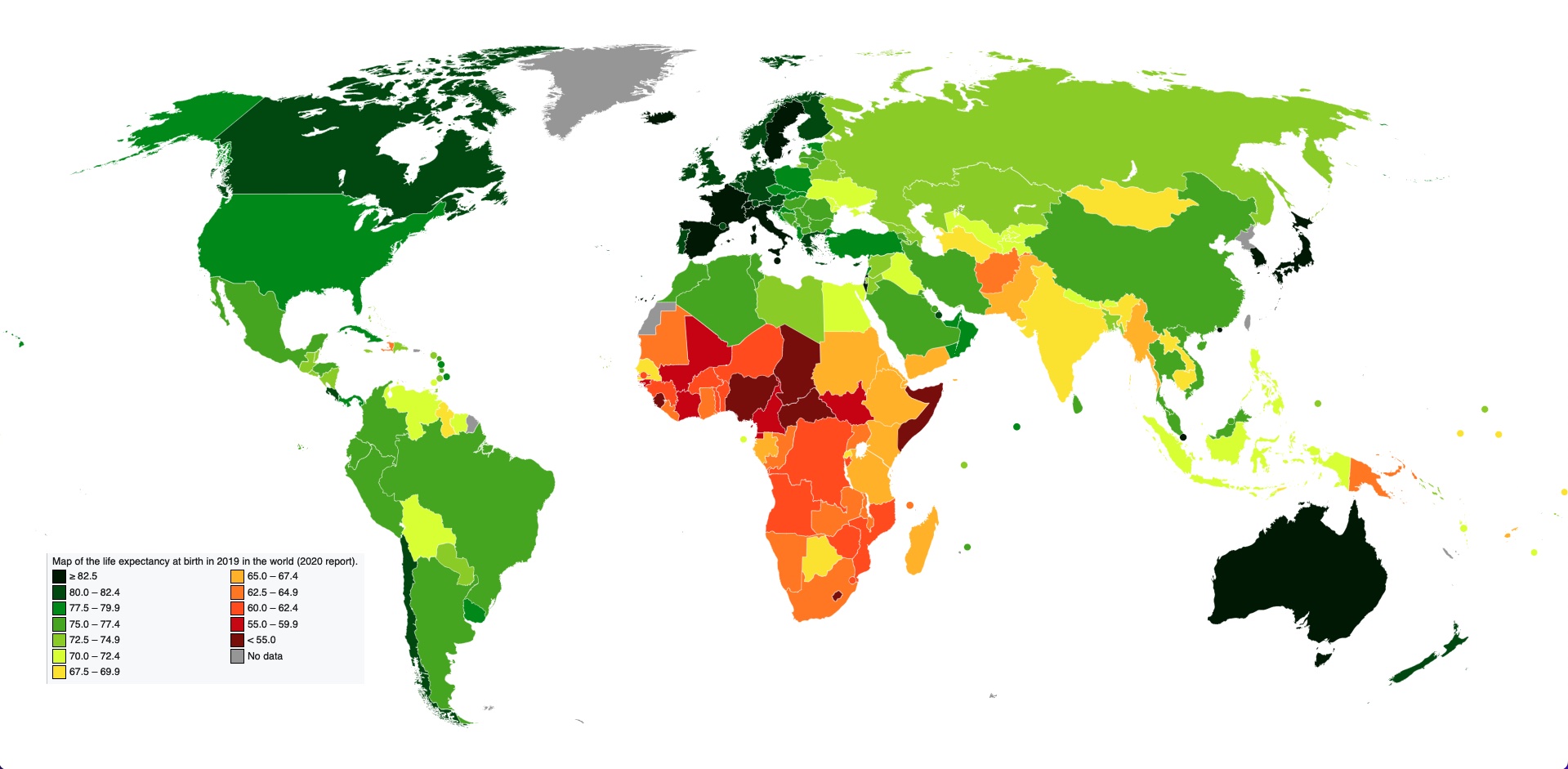
Life expectancy is a statistical measure of the average time an organism is expected to live, based on the year of birth, current age, and other demographic factors including gender. The most commonly used measure of life expectancy is at birth (LEB). There are great variations in life expectancy in different parts of the world, mostly due to differences in public health, medical care, and diet, but also affected by education, economic circumstances, violence, mental health, and sex.
Life Expectancy in the United States
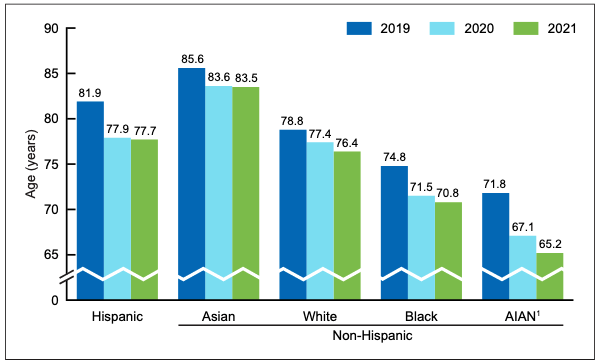
According to the CDC (2022), life expectancy in the U.S. now stands at 76.1 years. Life expectancy dropped 1.8 years in 2020 and 0.9 years in 2021, largely due to the coronavirus pandemic (74% of the decline) and to drug overdoses (fentanyl). Before 2020, life expectancy had been slowly but steadily increasing in the U.S.; its currently at its lowest level since 1996. Women continue to outlive men, with life expectancy being 74.2 years for males, and 79.1 years for females. Life expectancy varies according to race and ethnicity. It is highest for Asian Americans, then Hispanics, for both males and females, and lower for blacks and American Indians or Alaskan Natives.
Statistics from the U.S. Census Bureau reveal that the 85-and over age group is the fastest-growing age group in America. According to the Census Bureau and AgingStats.gov, the over-65 population grew from 3 million in 1900 to 40 million in 2010, an increase of more than 1200%. But during this same time, the over-85 population grew from just over 100,000 in 1900 to 5.5 million in 2010–an increase of 5400%!
When calculating life expectancy, we consider all of the elements of heredity, health history, current health habits, and current life experiences which contribute to a longer life or subtract from a person’s life expectancy. Recent studies concluded that cutting calorie intake by 15 percent over two years can slow aging and protect against diseases such as cancer, diabetes, and Alzheimer’s (Redman et al., 2018).
Some life factors are beyond a person’s control, and some are controllable. The rising cost of health care is a source of financial vulnerability to older adults. Vaccines are especially important for older adults. As you get older you’re more likely to get diseases like the flu, pneumonia, and shingles, and to have complications that can lead to long-term illness, hospitalization, and even death.
Things that contribute to longer life expectancies include eating a healthy diet that is rich in plants and nuts. Staying physically active, not smoking, and consuming moderate amounts of alcohol, tea, or coffee are also reported to be beneficial to leading a long life. Other recommendations include being conscientious, prioritizing your happiness, avoiding stress and anxiety, and having a strong social support network. Establishing a consistent sleep schedule and maintaining between 7-8 hours of sleep per night is also beneficial (Petre, 2019).
A major reason a person will statistically live longer once they reach an older age is simply that they have made it this far without anything killing them. Also, there appear to be several factors which may explain changes in life expectancy in the United States and around the world—health conditions are better, many diseases have been eliminated or better controlled through medicine, working conditions are better and better lifestyle choices are being made. Such factors significantly contribute to longer life expectancies.
Understanding Life Expectancy
Life expectancy is also used in describing the physical quality of life. Quality of life is the general well-being of individuals and societies, outlining negative and positive features of life. Quality of life considers life satisfaction, including everything from physical health, family, education, employment, wealth, safety, security, freedom, religious beliefs, and the environment. According to the CDC (2020), getting adequate physical activity is an evidence-based way to increase quality of life. Learn more about how much activity and types of activities recommended for older adults in this 4-minute podcast from the CDC.

Increased life expectancy brings concern over the health and independence of those living longer. Greater attention is now being given to the number of years a person can expect to live without disability, which is called active life expectancy. When this distinction is made, we see that although women live longer than men, they are more at risk of living with a disability (Weitz, 2007).
What factors contribute to poor health in women? Marriage has been linked to longevity, but spending years in a stressful marriage can increase the risk of illness. This negative effect is experienced more by women than men and seems to accumulate over the years. The impact of a stressful marriage on health may not occur until a woman reaches 70 or older (Umberson et al., 2006). Sexism can also create chronic stress. The stress experienced by women as they work outside the home as well as care for family members can also ultimately have a negative impact on health (He et al., 2005).
The shorter life expectancy for men in general, is attributed to greater stress, poorer attention to health, more involvement in dangerous occupations, and higher rates of death due to accidents, homicide, and suicide. Social support can increase longevity. For men, life expectancy and health seems to improve with marriage. Spouses are less likely to engage in risky health practices and wives are more likely to monitor their husband’s diet and health regimes. But men who live in stressful marriages can also experience poorer health as a result.
Health and Sexuality
It has been suggested that an active sex life can increase longevity among the elderly. Dr. Maggie Syme found in her research on sexuality in old age that, “Having a sexual partnership, with frequent sexual expression, having a good quality sex life, and being interested in sex have been found to be positively associated with health among middle-aged and older adults” (Syme, 2014). Positive sexual health in older age is gradually becoming more of a common topic and less taboo. Population percentage increase among older Americans has resulted in placing more attention on the needs of this age group, including their ideas on sexual health, desires, and attitudes. This shift in attitudes and behaviors, combined with medical advances to prolong a sexually active life, has changed the landscape of aging sexuality.
There are a number of associated health benefits with practicing positive sexual health. Positive sexual health often acts as a de-stressor promoting increased relaxation. Researchers also report health benefits such as decreased pain sensitivity, improved cardiovascular health, lower levels of depression, increased self-esteem, and better relationship satisfaction. This could also imply that there are negative consequences of poor sexual health or lack of sexual activity, including depression, low self-esteem, increased frustration, and loneliness.
Key players in improving the quality of life among older adults are the adults themselves. By exercising, reducing stress, not smoking, limiting use of alcohol, consuming more fruits and vegetables, and eating less meat and dairy, older adults can expect to live longer and more active lives (He et al., 2005). Regular exercise is also associated with a lower risk of developing neurodegenerative disorders, especially Alzheimer’s disease, and Parkinson’s disease. Stress reduction both in late adulthood and earlier in life is also crucial. The reduction of societal stressors can promote active life expectancy. In the last 40 years, smoking rates have decreased, but obesity has increased, and physical activity has only modestly increased.
Health in Late Adulthood: Primary Aging
Normal Aging
The Baltimore Longitudinal Study on Aging (BLSA, 2011) began in 1958 and has traced the aging process in 1,400 people from age 20 to 90. Researchers from the BLSA have found that the aging process varies significantly from individual to individual and from one organ system to another. Kidney function may deteriorate earlier in some individuals. Bone strength declines more rapidly in others. Much of this is determined by genetics, lifestyle, and disease. However, some generalizations about the aging process have been found:
- Heart muscles thicken with age
- Arteries become less flexible
- Lung capacity diminishes
- Brain cells lose some functioning but new neurons can also be produced
- Kidneys become less efficient in removing waste from the blood
- The bladder loses its ability to store urine
- Body fat stabilizes and then declines
- Muscle mass is lost without exercise
- Bone mineral is lost. Weight-bearing exercise slows this down.

Primary and Secondary Aging
Healthcare providers need to be aware of which aspects of aging are reversible and which ones are inevitable. By keeping this distinction in mind, caregivers may be more objective and accurate when diagnosing and treating older patients. And a positive attitude can go a long way toward motivating patients to stick with a health regime. Unfortunately, stereotypes can lead to misdiagnosis. For example, it is estimated that about 10 percent of older patients diagnosed with dementia are actually depressed or suffering from some other psychological illness (Berger, 2005). The failure to recognize and treat psychological problems in older patients may be one consequence of such stereotypes.
Primary Aging
Senescence is biological aging associated with the gradual deterioration of functional characteristics. It is the process by which cells irreversibly stop dividing and enter a state of permanent growth arrest without undergoing cell death. This process is also referred to as primary aging and thus, refers to the inevitable changes associated with aging (Busse, 1969). These changes include changes in the skin and hair, height and weight, hearing loss, and eye disease. However, some of these changes can be reduced by limiting exposure to the sun, eating a nutritious diet, and exercising.
Skin and hair change with age. The skin becomes drier, thinner, and less elastic during the aging process. Scars and imperfections become more noticeable as fewer cells grow underneath the surface of the skin. Exposure to the sun, or photoaging, accelerates these changes. Graying hair is inevitable, and hair loss all over the body becomes more prevalent.
Height and weight vary with age. Older people are more than an inch shorter than they were during early adulthood (Masoro in Berger, 2005). This is thought to be due to a settling of the vertebrae and a lack of muscle strength in the back. Older people weigh less than they did in mid-life. Bones lose density and can become brittle. This is especially prevalent in women. However, weight training can help increase bone density after just a few weeks of training.
Muscle loss occurs in late adulthood and is most noticeable in men as they lose muscle mass. Maintaining strong leg and heart muscles is important for independence. Weight-lifting, walking, swimming, or engaging in other cardiovascular and weight bearing exercises can help strengthen the muscles and prevent atrophy.
Vision
Some typical vision issues that arise along with aging include:
- The lens becomes less transparent and the pupils shrink.
- The optic nerve becomes less efficient.
- Distant objects become less acute.
- Loss of peripheral vision (the size of the visual field decreases by approximately one to three degrees per decade of life.)
- More light is needed to see and it takes longer to adjust to a change from light to darkness and vice versa.
- Driving at night becomes more challenging.
- Reading becomes more of a strain and eye strain occurs more easily.
The majority of people over 65 have some difficulty with vision, but most are easily corrected with prescriptive lenses. Three percent of those 65 to 74 and 8 percent of those 75 and older have hearing or vision limitations that hinder activity. The most common causes of vision loss or impairment are glaucoma, cataracts, age-related macular degeneration, and diabetic retinopathy (He et al., 2005).
- Glaucoma occurs when the pressure in the fluid of the eye increases, either because the fluid cannot drain properly or because too much fluid is produced. Glaucoma can be corrected with drugs or surgery. It must be detected early enough.
- Cataracts are cloudy or opaque areas of the lens of the eye that interfere with passing light, frequently develop. Cataracts can be surgically removed or intraocular lens implants can replace old lenses.
- Macular degeneration is the most common cause of blindness in people over the age of 60. Age-related macular degeneration (AMD) affects the macula, a yellowish area of the eye located near the retina at which visual perception is most acute. A diet rich in antioxidant vitamins (C, E, and A) can reduce the risk of this disease.
- Diabetic retinopathy, also known as diabetic eye disease, is a medical condition in which damage occurs to the retina due to diabetes mellitus. It is a leading cause of blindness. There are three major treatments for diabetic retinopathy, which are very effective in reducing vision loss from this disease: laser photocoagulation, medications, and surgery.
Hearing
Hearing Loss is experienced by 25% of people between ages 65 and 74, then by 50% of people above age 75. Among those who are in nursing homes, rates are even higher. Older adults are more likely to seek help with vision impairment than with hearing loss, perhaps due to the stereotype that older people who have difficulty hearing are also less mentally alert.
Conductive hearing loss may occur because of age, genetic predisposition, or environmental effects, including persistent exposure to extreme noise over the course of our lifetime, certain illnesses, or damage due to toxins. Conductive hearing loss involves structural damage to the ear such as failure in the vibration of the eardrum and/or movement of the ossicles (the three bones in our middle ear). Given the mechanical nature by which the sound wave stimulus is transmitted from the eardrum through the ossicles to the oval window of the cochlea, some degree of hearing loss is inevitable. These problems are often dealt with through devices like hearing aids that amplify incoming sound waves to make vibration of the eardrum and movement of the ossicles more likely to occur.
When the hearing problem is associated with a failure to transmit neural signals from the cochlea to the brain, it is called sensorineural hearing loss. This type of loss accelerates with age and can be caused by prolonged exposure to loud noises, which causes damage to the hair cells within the cochlea. Presbycusis is an age-related sensorineural hearing loss resulting from degeneration of the cochlea or associated structures of the inner ear or auditory nerves. The hearing loss is most marked at higher frequencies (higher pitched sounds). Presbycusis is the second most common illness next to arthritis in aged people.
One disease that results in sensorineural hearing loss is Ménière’s disease. Although not well understood, Ménière’s disease results in a degeneration of inner ear structures that can lead to hearing loss, tinnitus (constant ringing or buzzing), vertigo (a sense of spinning), and an increase in pressure within the inner ear (Semaan & Megerian, 2011). This kind of loss cannot be treated with hearing aids, but some individuals might be candidates for a cochlear implant as a treatment option. Cochlear implants are electronic devices consisting of a microphone, a speech processor, and an electrode array. The device receives incoming sound information and directly stimulates the auditory nerve to transmit information to the brain.
Being unable to hear causes people to withdraw from conversation and others to ignore them or shout. Unfortunately, shouting is usually high pitched and can be harder to hear than lower tones. The speaker may also begin to use a patronizing form of ‘baby talk’ known as elderspeak (See et al., 1999). This language reflects the stereotypes of older adults as being dependent, demented, and childlike. Hearing loss is more prevalent in men than women. And it is experienced by more white, non-Hispanics than by Black men and women. Smoking, middle ear infections, and exposure to loud noises increase hearing loss.
Nutrition and Aging Research
The Jean Mayer Human Nutrition Research Center on Aging (HNRCA), located in Boston, Massachusetts, is one of six human nutrition research centers in the United States supported by the United States Department of Agriculture and Agricultural Research Service. The goal of the HNRCA, which is managed by Tufts University, is to explore the relationship between nutrition, physical activity, and healthy and active aging.
The HNRCA has made significant contributions to U.S. and international nutritional and physical activity recommendations, public policy, and clinical healthcare. These contributions include advancements in the knowledge of the role of dietary calcium and vitamin D in promoting nutrition and bone health, the role of nutrients in maintaining the optimal immune response, the prevention of infectious diseases, the role of diet in the prevention of cancer, obesity research, modifications to the Food Guide Pyramid, contribution to USDA nutrient data bank, advancements in the study of sarcopenia, heart disease, vision, brain and cognitive function, front of packaging food labeling initiatives, and research of how genetic factors impact predisposition to weight gain and various health indicators. Research clusters within the HNRCA address four specific strategic areas: 1) cancer, 2) cardiovascular disease, 3) inflammation, immunity, and infectious disease and 4) obesity.
Primary aging can be compensated for through exercise, corrective lenses, nutrition, and hearing aids. Just as important, by reducing stereotypes about aging, people of age can maintain self-respect, recognize their own strengths, and count on receiving the respect and social inclusion they deserve.
Health in Late Adulthood: Secondary Aging
Secondary Aging
Secondary aging refers to changes that are caused by illness or disease. These illnesses reduce independence, impact the quality of life, affect family members and other caregivers, and bring financial burden. The major difference between primary aging and secondary aging is that primary aging is irreversible and is due to genetic predisposition; secondary aging is potentially reversible and is a result of illness, health habits, and other individual differences.
Chronic Illnesses

In the United States, six in 10 Americans adults had at least one chronic medical condition and the number is expected to increase (CDC, 2022). The most common chronic conditions are high blood pressure, arthritis, respiratory diseases like emphysema, and high cholesterol. Cigarette smoking is the leading cause of preventable death and disease in the U.S.
According to research by the Centers for Disease Control and Prevention, chronic disease is also especially a concern in the elderly population in America. Chronic diseases like stroke, heart disease, and cancer are among the leading causes of death among Americans aged 65 or older. While the majority of chronic conditions are found in individuals between the ages of 18 and 64, it is estimated that at least 80% of older Americans are currently living with some form of a chronic condition, with 50% of this population having two or more chronic conditions. The two most common chronic conditions in the elderly are high blood pressure and arthritis, with diabetes, coronary heart disease, and cancer also being reported at high rates among the elderly population. The presence of type 2 diabetes, high blood pressure, and obesity, is termed “metabolic syndrome” and impacts 50% of individuals over the age of 60.
Heart disease is the leading cause of death from a chronic disease for adults older than 65, followed by cancer, stroke, diabetes, chronic lower respiratory diseases, influenza and pneumonia, and, finally, Alzheimer’s disease (which we’ll examine further when we talk about cognitive decline). Though the rates of chronic disease differ by race for those living with chronic illness, the statistics for the leading causes of death among the elderly are nearly identical across racial/ethnic groups.
Heart Disease
As stated above, heart disease is the leading cause of death from chronic disease for adults older than 65. Cardiovascular disease (CVD) is a class of diseases that involve the heart or blood vessels. CVD includes coronary artery diseases (CAD) such as angina and myocardial infarction (commonly known as a heart attack). Other CVDs include stroke, heart failure, hypertensive heart disease, rheumatic heart disease, cardiomyopathy, heart arrhythmia, congenital heart disease, valvular heart disease, carditis, aortic aneurysms, peripheral artery disease, thromboembolic disease, and venous thrombosis.
The underlying mechanisms vary depending on the disease. Coronary artery disease, stroke, and peripheral artery disease involve atherosclerosis. This may be caused by high blood pressure, smoking, diabetes mellitus, lack of exercise, obesity, high blood cholesterol, poor diet, and excessive alcohol consumption, among others. High blood pressure is estimated to account for approximately 13% of CVD deaths, while tobacco accounts for 9%, diabetes 6%, lack of exercise 6%, and obesity 5%.
It is estimated that up to 90% of CVD may be preventable. Prevention of CVD involves improving risk factors through healthy eating, exercise, avoidance of tobacco smoke, and limiting alcohol intake. Treating risk factors, such as high blood pressure, blood lipids and diabetes is also beneficial. The use of aspirin in people, who are otherwise healthy, is of unclear benefit.
Cancer
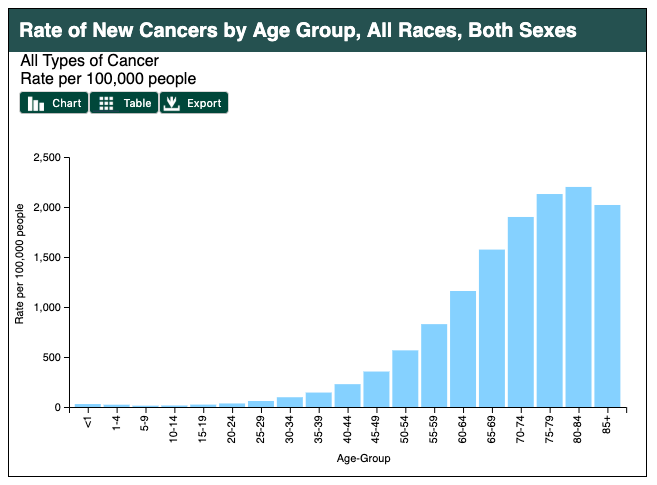
Age in itself is one of the most important risk factors for developing cancer. Currently, 60% of newly diagnosed malignant tumors and 70% of cancer deaths occur in people aged 65 years or older. Many cancers are linked to aging; these include breast, colorectal, prostate, pancreatic, lung, bladder, and stomach cancers. Men over 75 have the highest rates of cancer at 28 percent. Women 65 and older have rates of 17 percent. Rates for older non-Hispanic Whites are twice as high as for Hispanics and non-Hispanic Blacks. The most common types of cancer found in men are prostate and lung cancer. Breast and lung cancer are the most common forms in women.
For many reasons, older adults with cancer have different needs than younger adults with the disease. For example, older adults:
- May be less able to tolerate certain cancer treatments.
- Have a decreased reserve (the capacity to respond to disease and treatment).
- May have other medical problems in addition to cancer.
- May have functional problems, such as the ability to do basic activities of daily living (ADL’s: dressing, bathing, eating) or more advanced activities (called instrumental activities of daily living, IADL’s, such as using transportation, going shopping or handling finances), and have less available family support to assist them as they go through treatment. IADL’s require more complex planning and thinking whereas ADL’s are basic self-care tasks.
- May not always have access to transportation, social support or financial resources.
- May have different views of quality versus quantity of life

Hypertension and Stroke
Hypertension or high blood pressure and associated heart disease and circulatory conditions increase with age. Stroke is a leading cause of death and severe, long-term disability. Most people who’ve had a first stroke also had high blood pressure (HBP or hypertension). High blood pressure damages arteries throughout the body, creating conditions where they can burst or clog more easily. Weakened arteries in the brain, resulting from high blood pressure, increase the risk for stroke—which is why managing high blood pressure is critical to reducing the chance of having a stroke. Hypertension disables 11.1 percent of 65 to 74 year olds and 17.1 percent of people over 75. Rates are higher among women and blacks. Rates are highest for women over 75. Coronary disease and stroke are higher among older men than women. The incidence of stroke is lower than that of coronary disease, but it is the No. 5 cause of death and a leading cause of disability in the United States.
Arthritis
While arthritis can affect children, it is predominantly a disease of the elderly. Arthritis is more common in women than men at all ages and affects all races, ethnic groups and cultures. In the United States a CDC survey based on data from 2013–2015 showed 22.7% (58.5 million) of adults aged ≥18 years had self-reported doctor-diagnosed arthritis, and 9.2% (23.7 million or 43.5% of those with arthritis) had arthritis-attributable activity limitation (AAAL) (Barbour et al., 2017). With an aging population, this number is expected to increase.
Arthritis is a term often used to mean any disorder that affects joints. Symptoms generally include joint pain and stiffness. Other symptoms may include redness, warmth, swelling, and decreased range of motion of the affected joints. In some types of arthritis, other organs are also affected. Onset can be gradual or sudden.
There are over 100 types of arthritis. The most common forms are osteoarthritis (degenerative joint disease) and rheumatoid arthritis. Osteoarthritis usually increases in frequency with age and affects the fingers, knees, and hips. Rheumatoid arthritis is an autoimmune disorder that often affects the hands and feet. Other types include gout, lupus, fibromyalgia, and septic arthritis. They are all types of rheumatic disease
Treatment may include resting the joint and alternating between applying ice and heat. Weight loss and exercise may also be useful. Pain medications such as ibuprofen and paracetamol (acetaminophen) may be used. In some a joint replacement may be useful.

Diabetes
Type 2 diabetes (T2D), formerly known as adult-onset diabetes, is a form of diabetes characterized by high blood sugar, insulin resistance, and a relative lack of insulin. Common symptoms include increased thirst, frequent urination, and unexplained weight loss. Symptoms may also include increased hunger, feeling tired, and sores that do not heal. Often symptoms come on slowly. Long-term complications from high blood sugar include heart disease, strokes, diabetic retinopathy which can result in blindness, kidney failure, and poor blood flow in the limbs which may lead to amputations.
Type 2 diabetes primarily occurs as a result of obesity and lack of exercise. Some people are more genetically at risk than others. Type 2 diabetes makes up about 90% of cases of diabetes, with the other 10% due primarily to type 1 diabetes and gestational diabetes. In type 1 diabetes there is a lower total level of insulin to control blood glucose, due to an autoimmune induced loss of insulin-producing beta cells in the pancreas. Diagnosis of diabetes is by blood tests such as fasting plasma glucose, oral glucose tolerance test, or glycated hemoglobin (A1C).
Type 2 diabetes is partly preventable by staying a normal weight, exercising regularly, and eating properly. Treatment involves exercise and dietary changes. If blood sugar levels are not adequately lowered, the medication metformin is typically recommended. Many people may eventually also require insulin injections. In those on insulin, routinely checking blood sugar levels is advised; however, this may not be needed in those taking pills. Bariatric surgery often improves diabetes in those who are obese.
Rates of type 2 diabetes have increased markedly since 1960 in parallel with obesity. As of 2015, there were approximately 392 million people diagnosed with the disease worldwide compared to around 30 million in 1985. Typically it begins in middle or older age, although rates of type 2 diabetes are increasing in young people. Type 2 diabetes is associated with a ten-year-shorter life expectancy.

Osteoporosis
Osteoporosis comes from the Greek word for “porous bones” and is a disease in which bone weakening increases the risk of a broken bone. It is defined as having a bone density of 2.5 standard deviations below that of a healthy young adult. Osteoporosis increases with age as bones become brittle and lose minerals. It is the most common reason for a broken bone among the elderly.
Osteoporosis becomes more common with age. About 15% of white people in their 50s and 70% of those over 80 are affected. It is four times more likely to affect women than men—in the developed world, depending on the method of diagnosis, 2% to 8% of males and 9% to 38% of females are affected. In the United States in 2010, about eight million women and one to two million men had osteoporosis. White and Asian people are at greater risk are more likely to have osteoporosis than non-Hispanic blacks.
Parkinson’s Disease
Parkinson’s disease (PD) is a long-term degenerative disorder of the central nervous system which mainly affects the motor system, although as the disease worsens, non-motor symptoms become increasingly common. Early in the disease, the most obvious symptoms are shaking, rigidity, slowness of movement, and difficulty with walking, but thinking and behavioral problems may also occur. Dementia becomes common in the advanced stages of the disease, and depression and anxiety also occur in more than a third of people with PD.
The cause of Parkinson’s disease is generally unknown, but believed to involve both genetic and environmental factors. Those with a family member affected are more likely to get the disease themselves. There is also an increased risk in people exposed to certain pesticides and among those who have had prior head injuries, while there is a reduced risk in tobacco smokers (though smokers are at a substantially greater risk of stroke) and those who drink coffee or tea. The motor symptoms of the disease result from the death of cells in the substantia nigra, a region of the midbrain, which results in not enough dopamine in these areas. The reason for this cell death is poorly understood but involves the build-up of proteins into Lewy bodies in the neurons.
In 2015, PD affected 6.2 million people and resulted in about 117,400 deaths globally. Parkinson’s disease typically occurs in people over the age of 60, of which about one percent are affected. Males are more often affected than females at a ratio of around 3:2. The average life expectancy following diagnosis is between 7 and 14 years. People with Parkinson’s who have increased the public’s awareness of the condition include actor Michael J. Fox, Olympic cyclist Davis Phinney, and professional boxer Muhammad Ali.
Theories on Aging

Why do we age?
There are a number of attempts to explain why we age and many factors that contribute to aging. The peripheral slowing hypothesis suggests that overall processing speed declines in the peripheral nervous system, affecting the brain’s ability to communicate with muscles and organs. Some of the peripheral nervous system (PNS) is under a person’s voluntary control, such as the nerves carrying instructions from the brain to the limbs. As well as controlling muscles and joints, the PNS sends all the information from the senses back to the brain.
The generalized slowing hypothesis theory suggests that processing in all parts of the nervous system, including the brain, are less efficient with age. This may be why older people have more accidents. Genetics, diet, lifestyle, activity, and exposure to pollutants all play a role in the aging process. (Plude & Doussard-Roosevelt, 1989).
Cell Life
Cells divide a limited number of times and then stop. This phenomenon, known as the Hayflick limit, is evidenced in cells studied in test tubes which divide about 50 times before becoming senescent. In 1961, Dr. Hayflick theorized that the human cell’s ability to divide is limited to approximately 50-times, after which they simply stop dividing (the Hayflick limit theory of aging). According to telomere theory, telomeres have experimentally been shown to shorten with each successive cell division (Jin, 2010).
Senescent cells do not die. They simply stop replicating. Senescent cells can help limit the growth of other cells which may reduce the risk of developing tumors when younger, but can alter genes later in life and result in promoting the growth of tumors as we age (Dollemore, 2006). Limited cell growth is attributed to telomeres which are the tips of the protective coating around chromosomes. Each time cells replicate, the telomere is shortened. Eventually, loss of telomere length is thought to create damage to chromosomes and produce cell senescence.
Biochemistry and Aging
Free Radical Theory of Aging
The free radical theory of aging (FRTA) states that organisms age because cells accumulate free radical damage over time. A free radical is any atom or moleculewhich has a single unpaired electron in an outer shell. This means that as oxygen is metabolized, mitochondria in the cells convert the oxygen to adenosine triphosphate (ATP) which provides energy to the cell. Unpaired electrons are a byproduct of this process and these unstable electrons cause cellular damage as they find other electrons with which to bond. These free radicals have some benefits and are used by the immune system to destroy bacteria. However, cellular damage accumulates and eventually reduces the functioning of organs and systems. Many food products and vitamin supplements are promoted as age-reducing. Antioxidant drugs have been shown to increase the longevity in nematodes (small worms), but the ability to slow the aging process by introducing antioxidants in the diet is still controversial.

Protein Crosslinking
This theory focuses on the role blood sugar, or glucose plays in the aging of cells. Glucose molecules attach themselves to proteins and form chains or crosslinks. These crosslinks reduce the flexibility of tissue and thus it becomes stiff and loses functioning. The circulatory system becomes less efficient as the tissue of the heart, arteries and lungs lose flexibility. Joints grow stiff as glucose combines with collagen.
DNA Damage
Through the normal growth and aging process, DNA is damaged by environmental factors such as toxic agents, pollutants, and sun exposure (Dollemore, 2006). This results in deletions of genetic material, and mutations in the DNA duplicated in new cells. The accumulation of these errors results in reduced functioning in cells and tissues. Theories that suggest that the body’s DNA genetic code contains a built-in time limit for the reproduction of human cells are called the genetic programming theories of aging. These theories promote the view that the cells of the body can only duplicate a certain number of times and that the genetic instructions for running the body can be read only a certain number of times before they become illegible. Such theories also promote the existence of a “death gene” which is programmed to direct the body to deteriorate and die, and the idea that a long life after the reproductive years is unnecessary for the survival of the species (Kunlin, 2010).
Decline in the Immune System
As we age, B-lymphocytes and T-lymphocytes become less active. These cells are crucial to the immune system as they secrete antibodies and directly attack infected cells. The thymus, where T-cells are manufactured, shrinks as aging progresses. This reduces our body’s ability to fight infection (Berger, 2005).
