37

Citation
Abstract
Objectives: Negative clinical educational experiences for student nurses are predictors of negative attitudes and perceptions towards mental health. In clinical education, instructors take on this important role often with little to no formal training. This study explored nursing students’ perceptions of instructional best practices in mental health clinical education.
Methods: A qualitative descriptive design was used, and 10 Canadian baccalaureate nursing (BN) students were interviewed. These students had completed a six-week practicum on an acute inpatient psychiatric unit in either their second, third or fourth year of study.
Results: Through thematic analysis, three themes were identified: (1) Students valued feeling prepared at the beginning of the clinical placement. (2) Students felt empowered when instructors encouraged self-direction. (3) Students appreciated positive role modeling by their instructors.
Conclusions: Suggestions for clinical teaching strategies are made to mitigate student stress, increase confidence, and address the influence of mental health stigma on learning.
Keywords: best practices in clinical education; constructivism; mental health nursing instructor; qualitative description.
Introduction
Clinical education in mental health nursing practicums is designed to offer students the opportunity to integrate learned knowledge and skills in an area that is unique amongst other areas of health care. Mental health nursing is seen to be a unique specialty as the skills needed rely heavily on being able to communicate and develop therapeutic relationships with patients (Choi et al., 2016). Baccalaureate nursing (BN) students can feel limited confidence in their communication skills, and they may have prejudicial or stigmatized views of mental illness which can create barriers for effective clinical education (Goh et al., 2021; Janse van Rensburg, 2019; Knaak, Mantler, & Szeto, 2017; Stuhlmiller & Tolchard, 2019). This can be influenced by students experiencing concerns related to the management of agitated patients, fears of saying something wrong, or low mental health literacy (Abraham, Cramer, & Palleschi, 2018). Mental health literacy is defined as the level of knowledge and understanding of mental illness and treatment; decreasing stigma related to mental health problems; and, enhancing help-seeking efficacy (Kutcher, Wei, & Coniglio, 2016). For nurses who instruct students in psychiatric clinical settings, providing students with supportive measures to help reduce stress, increase practice confidence, and address mental illness stigma are essential features for education (Snyder, 2020; Vuckovic, Carlson, & Sunnqvist, 2021).
A current barrier to effective clinical education is the lack of formal training for nurses who instruct BN students in these kinds of psychiatric clinical settings. As outlined by Booth, Emerson, Hackney, and Souter (2016), education and nursing are two different disciplines, and clinical expertise does not naturally result in teaching expertise. Findings arising from existing literature only provide minimal insight toward how nurse instructors who practice in this specialized area can address the concerns that students may bring to their mental health learning experiences. Subsequently, the aim of this study was to address this gap by exploring students’ perceptions of best practices for nurses who instruct in mental health clinical settings.
Literature review
For the purpose of the study, a broad search was conducted using three databases: Cumulative Index to Nursing and Allied Health Literature (CINAHL®); MEDLINE/PubMed®; and Academic Search Complete through EBSCO. Broad search terms including Nursing Clinical Instructors OR Nursing Clinical Facilitator, Nursing Students Perceptions OR Attitudes, and Mental Health Clinical Placement OR Mental Health Clinical Education were used. These terms were entered separately and in varying combinations to generate the broadest search. Multiple search modes such as, but not limited to, Boolean/Phrase, and applying related words were used. Studies were limited to full text, English language, scholarly (peer reviewed) journals, and published dates of 2014–2021. This search generated 970 title matches. To further narrow the number of articles found, other search terms including effective education, undergraduate mental health nursing students, and clinical education were applied, resulting in 90 remaining title matches.
A critical review of the abstracts was completed, and articles were deemed relevant if they discussed concepts regarding nursing students or nursing clinical instructor’s perceptions of effective clinical education. Twenty articles were found to meet this inclusion criteria. The results included 12 qualitative studies, four quantitative studies, three studies using mixed methodology and one qualitative integrative review. The research articles included international representation from the following countries: Canada, Australia, Singapore, South Africa, United Kingdom and the United States. Of the 20 articles only three pertain to mental health clinical education, including one publication from 2010 (Grav, Juul, & Heilzen, 2010; Janse van Rensburg, 2019; Slemon, Jenkins, Bungay, & Brown, 2020; Stuhlmiller & Tolchard, 2019). While the Grav et al., (2010) publication was older than the 2014 inclusion criteria, the article was included due to its strong relevance to the study.
Competency, teaching style, and personality were themes found to accurately identify characteristics of best practices for nurses instructing student nurses. Students favored instructors with expertise in the area of what they taught and preferred nurses who had advanced education on education theory (Collier, 2018; Janse van Rensburg, 2019). Teaching styles vary among instructors, and students found pedagogy effective that was rooted in being adaptive to students and instructors being able to deliver effective feedback (Niederriter, Eyth, & Thoman, 2017; Sweet & Broadbent, 2017). Personality traits seemed to have played the largest role in influencing students’ perceptions of whether instructors were perceived as effective educators. The literature reviewed for this study demonstrates that clinical instructors can impact the way students view their mental health clinical experiences (Ismail, Aboushady, & Esw, 2015; Meyer, Nel, & Downing, 2016; Slemon et al., 2020). Nurses who instruct act as role models, and they mentor students while ensuring that the nurses of tomorrow are prepared and capable of delivering the high level of care patients deserve.
This literature review also exposed how mental health clinical placements are a unique setting compared to other areas of nursing. The instructor is seen to have different challenges such as addressing high rates of anxiety among students while challenging prejudicial or stigmatic views towards mental health nursing. Though limited in the research, it seems that effective instructors provide students with a positive learning experience through being advocates for patients, championing therapeutic relationships and modeling empathy (Collier, 2018; Ismail et al., 2015; Meyer et al., 2016; Niederriter et al., 2017; Padagas, 2020; Reising, James, & Morse, 2018; Sadeghi, Oshvandi, & Moradi, 2019; Stuhlmiller & Tolchard, 2019). However, the current state of the literature is limited. A gap remains in the literature which fails to provide an in-depth understanding of the specific teaching strategies that clinical instructors can use to address the specific challenges instructors in Canada experience while facilitating mental health clinical education.
Conceptual framework
A constructivist framework, which holds participants’ experiences and perspectives in high regard, was used to guide this study. This framework offers researchers an opportunity to understand the unique ways in- dividuals construct knowledge and meaning from their experiences (Creswell, 2013). Further, the construc- tivist paradigm is based on a relativist ontology which asserts that there are multiple realities (Adom, Yeboah, & Ankrah, 2016). Reality is not singular, and rather is uniquely understood by the individual who is experi- encing it. By sharing their knowledge, the nursing students who participated in this research project provided meaning and guidance on clinical education, both for themselves and others. From a subjective epistemo- logical view, knowledge can be extended when researchers co-create new understanding and reconstruct existing perceptions with studies rich in authenticity and trustworthiness (Adom et al., 2016). In keeping with the axiological beliefs that are fundamental in constructivist thinking, the participants’ values were acknowledged, honored, and respected throughout the research activities (Creswell, 2013). This intention produced an informed description, and interpretation of the experience at the point that it existed in the real world for these nursing students.
Methods
Study design and sample
A qualitative descriptive design was implemented, where researchers seek to understand and describe the perspectives of people experiencing the phenomenon under investigation (Bradshaw, Atkinson, & Doody, 2017; Lincoln & Guba, 1985; Sandelowski, 2000, 2010). In qualitative descriptive research, the focus is on recognizing the subjective nature of problems, understanding individual human experiences, contributing to change and quality improvement in the practice setting; and not on increasing theoretical or conceptual understanding (Doyle, McCabe, Keogh, Brady, & McCann, 2020).
The purposeful sampling for this study included current students enrolled in a four-year BN program at one university located in Calgary, Alberta, Canada. To be included in the study, these students must have completed a six-week practicum on an acute inpatient psychiatric unit in either their second, third or fourth year of study. Ten students were recruited with eight female students, and two male students. Eight students were in their third year of education, and two were in their fourth year of education at the time of this study.
Data collection and analysis
Data was collected via transcripts from 10 semi-structured, Zoom videoconference interviews that were approximately 1-h each in length. An interview guide ensured consistency and members of the research team (who instruct in Canadian undergraduate mental health nursing courses) developed the guide around open-ended questions that allowed participants to describe their experiences and perspectives in their own words. Questions were sequenced from broad to narrow and time was allocated for follow up questions based on participants’ comments. An example interview question was: “Tell me about teaching strategies your instructor used that were especially effective.” Ethical approval was granted by the university to conduct the study; participants signed consent forms, and all data was de-identified. Finally, members of the research team did not possess evaluator capacities over any of the study participants.
Thematic analysis was implemented through a three-phase inductive, open coding approach (Alhojailan, 2012). The transcripts were read and re-read at different times over a four-month period. Text relevant to the purpose of the research was highlighted, field notes were incorporated and discussions among the research team were held. Using NVivo 12 (QSR International PTY LTD, 2018), three levels of themes were organized and titled respectively: basic themes (rudimentary micro understandings of the data); organizing themes (two or more basic themes that possess similarities and fit under a broader definition); and global themes (a summary and consolidation of themes previously identified) (Akinyode & Khan, 2018). The resulting themes provide what Alase (2017) refers to as a thick description of what participants experienced and the context or how they were affected.
Data saturation was reached by the eighth interview, when weekly discussions among the researchers identified that participants’ comments had become repetitive and no new information was forthcoming. However, two additional interviews were conducted to ensure data saturation. Faulkner and Trotter (2017) explained that data saturation occurs when researchers believe that further data collection would yield similar results.
Trustworthiness was established using Lincoln and Guba’s (1985) criteria of credibility, transferability, dependability, and confirmability. Credibility, or truthfulness of the study was established through member checking, or respondent validation. Participants were provided with their transcripts as well as a summary of the themes. All participants confirmed the accuracy of the transcripts. Although two participants did not reply, eight of the 10 participants confirmed that the themes were accurate and resonated with them. Transferability, or applicability of the study to other contexts was established by providing rich, thick description. Dependability, or demonstrating that findings can be repeated was established with an audit trail. Confirmability, or degree of neutrality was established through reflexive journaling and weekly research meetings.
Findings
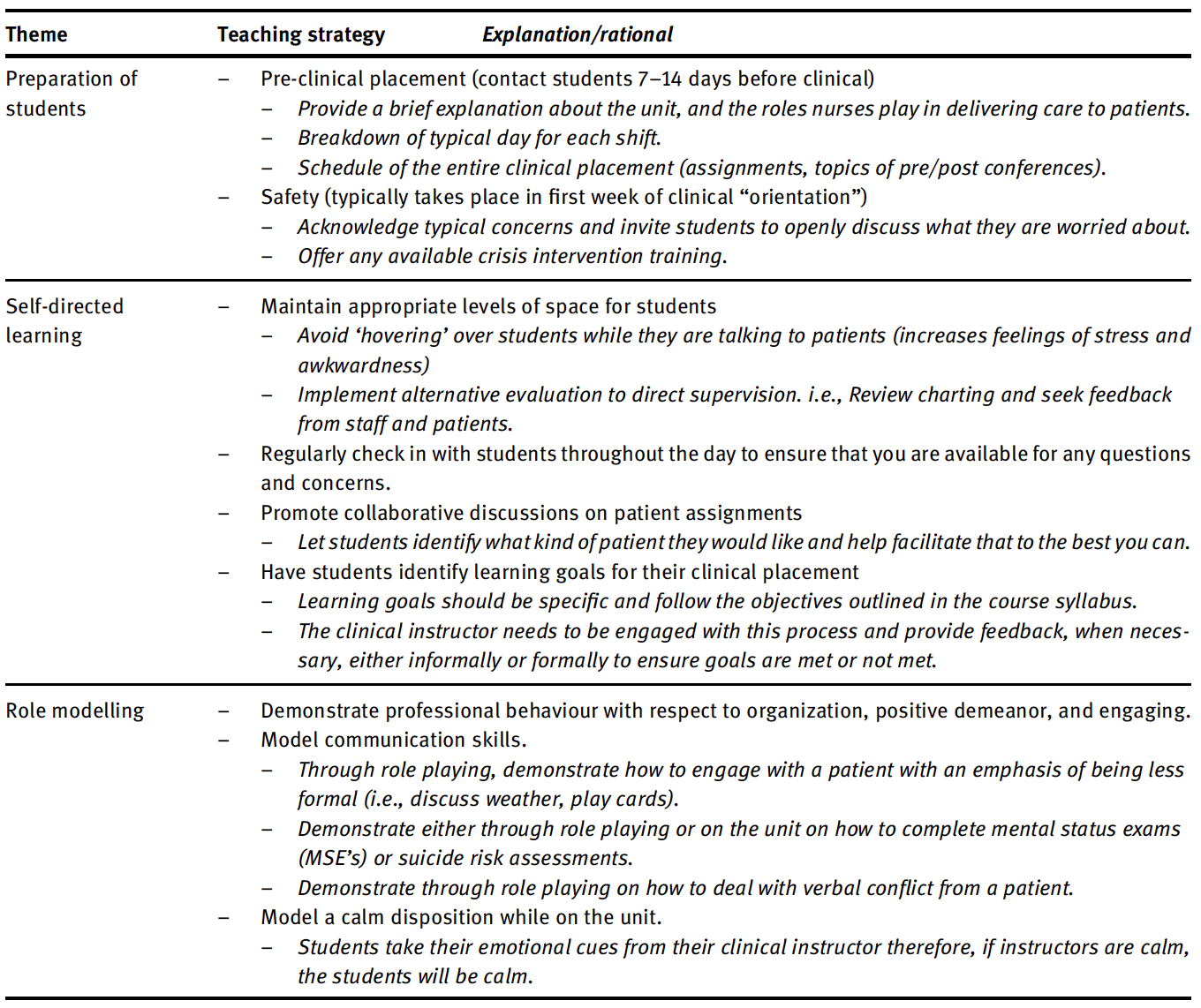
The following three themes represent key findings. First, students valued feeling prepared at the beginning of the clinical placement. Second, students felt empowered when instructors encouraged self-direction. Third, students appreciated positive role modeling by their instructors. See Table 1 for best practices in psychiatric mental health nursing derived from these themes.
Table 1: Best instructional practices in psychiatric mental health nursing clinical education.
Theme one: students’ valued feeling prepared at the beginning of the clinical placement
Participants identified a spectrum of emotions as they began their mental health clinical rotation. Emotions of fear, stress, anxiety, and excitement were amongst the most cited. There was a consensus amongst the participants that these emotions were fueled by a general lack of knowledge about mental health nursing. This participant highlights their limited knowledge:
When asked about their perception of mental health nursing prior to their rotation, participants described having very little understanding of what mental health nursing entailed other than what they had been exposed to through the media, their peers, or personal/familial experiences. The most common concerns expressed focused on personal safety and feeling unprepared or ill-equipped to handle crises such as an aggressive patient. This was seen to be a unique issue exclusive to mental health nursing as all the participants denied having these types of concerns prior to entering previous clinical areas. This is how one participant described their anticipatory anxiety leading up to their rotation:
Participants emphasized how their clinical instructor played an important role in mitigating their anxiety, both before and during their practicum. In particular, best instructional practices that helped students feel prepared at the beginning of clinical were pre-placement contact and addressing safety concerns. These are discussed in the following section.
Pre-placement contact
In this study, pre-placement contact refers to clinical instructors contacting students via email prior to the start of a clinical rotation. The contact typically occurred between seven and 14 days prior to students first day on a unit. Participants noted the content of the email greetings varied. Participants 2, 4, 5, and 7 mentioned how receiving resources to prepare for clinical, such as brief explanations of the unit, commonly used medications, and unit schedules, were helpful.
Participants also described that in addition to a simple greeting, and providing resources, clinical in- structors took this opportunity to ask information of the students that they deemed important for the instructor to know. Participants 4, 6, and 9 commented on how the opportunity to privately describe their personality, interests, and importantly, their individual learning styles was valuable to them. They described how the best instructional questioning practices related to uncovering ways they learned in the clinical setting and any challenges they were facing in their personal life that might hinder learning. Participants equated this gesture with feeling supported and assured that the instructor valued their perspectives as well as their mental wellness.
Feeling unprepared was frequently identified as a factor that increased the level of stress and anxiety. For example, one participant described how beneficial it was for them to receive a schedule that outlined what a typical day looked like on the unit as well a schedule of the overall clinical rotation. This participant discussed struggling to conceptualize what a nurse’s role was on the mental health unit, which further increased their stress. They explained:
They were like super specific with the details which helped us because some clinical instructors don’t say anything like until the last minute, but they were quite like prepared I guess ahead of time. So that really helped the students get organized before meeting as a group. (Participant 9)
Addressing safety concerns
During the first week of any clinical rotation, instructors often take the first day(s) to orientate students and discuss unit and patient information. In psychiatric mental health settings however, this everyday practice must be extended to address safety concerns.
Participants in this study consistently identified that they worried about their personal safety. They viewed the patient population as unpredictable and dangerous. Four participants (3, 6, 7, and 10) admitted that their perception of mentally ill patients as dangerous was influenced by media portrayals of people suffering from acute mental illness as violent. They found that during this orientation phase, their anxieties of personal safety were best mitigated by instructional practices such as facilitating group discussions around safety protocols, inviting students to discuss their potential fears, and having them participate in any available crisis intervention training. Participants preferred a direct approach that was clear and impactful for students to un- derstand. This was evident by this participant’s comment:
Theme two: students felt empowered when instructors encouraged self-direction
Self-direction was defined by the participants as an approach where the instructor remains somewhat ‘hands off’ and allowed students to have an increased amount of space and autonomy in their own learning. Six of the participants (1, 2, 5, 7, 8, and 9) described how they found a self-directed approach increased their sense of empowerment.
Having autonomy in their learning was observed to help build confidence in their own abilities and offer a glimpse into what it is like to be a nurse:
Another student commented on how this approach was transformative in affirming their decision to choose nursing as a career:
Participants explained that despite this seemingly distancing ‘hands-off’ approach, they knew the instructor was available on the unit as they regularly checked in with them throughout the day and were observing “from afar.” In lieu of hovering around students while they were talking with their patients, participants described alternative instructional practices that could be used to evaluate progress. For example, reviewing students’ charting, and seeking feedback from staff and patients. Students conveyed their desire for independence, but they also expected their instructor to be present to assure them that they were not left on their own.
Collaborative goal setting
Participants commented on how they felt especially empowered when instructors engaged them in collaborative goal setting. Students felt that their autonomy was enhanced when their instructors collaborated with them to create individual learning goals that targeted what students themselves wanted to learn about psychiatric disorders, and the areas where they wanted to improve their communication skills. One example of best instructional practice identified was to invite students to select their own patients when possible:
Theme three: students appreciated positive role modeling by their instructors
All 10 participants in this study identified how significant it was for their professional development and education that the clinical instructor be a positive role model throughout the clinical rotation. They noted that characteristics of a positive role model were professionalism, organization, having a positive disposition, and demonstrating an engaging demeanor.
The importance of positive role modelling in clinical education is well known (Jack, Hamshire, & Chambers, 2017; Melrose, Park, & Perry, 2021). However, the nuance of how it is executed is unique in psychiatric clinical areas. Participants were concerned that they could not communicate effectively with patients. Specific issues included discomfort posing assessment questions related to suicide, trauma, and psychosis. For example:
Another participant described being worried that they would say something wrong and potentially harm the patient.
In response to their concerns, participants described best instructional practices that instructors implemented to mitigate these concerns and strengthen their confidence. They mentioned how effective role-playing with instructors and fellow students was. Role playing gave students a chance to observe their instructor demonstrating expected behaviors and to “test” their own skills in simulated scenarios. Additionally, participants described how valuable it was to observe their instructors interacting with patients. This participant high- lighted their appreciation of positive role modeling:
This participant also discussed how the clinical instructor would model informal approaches to mental status assessments.
They encouraged me to step out of my comfort zone, but also still be safe with that. Step out of my comfort zone and go communicate and talk to these patients where they’re sitting in the common area and just kind of like sit down with them … like talk to them as like they’re your friends I guess and like rather than going there and asking specific questions about like, “How are you feeling today?” (Participant 10)
By modelling effective communication and normalizing a less formal approach in conversing with patients, participants reported feeling less pressured to “say the right thing.” In turn, this reduced students’ anxiety, increased their feelings of empathy, and gave them needed tools to engage in stronger therapeutic student- patient relationships.
Discussion
Stigma towards mental illness exerts a negative influence on learning (Canadian Association of Schools of Nursing & Canadian Federation of Mental Health Nurses, 2015; İnan, Günüşen, Duman, & Ertem, 2019). Given the inaccurate portrayals of mentally ill individuals in the media, it is not unexpected that many people, including health professionals and students, hold stigmatized views. Research examining the pervasive nature of mental illness-related stigma in healthcare concluded that a lack of understanding of mental illness was a strong predictor for fostering stigmatic views among health care workers and students (Knaak et al., 2017). Many nursing students are unaware of their stigmatized views prior to entering their clinical placement (Choi et al., 2016). Transformations in thinking can only occur when students are supported towards questioning their ideas and embracing a willingness to take on new perspectives (Tsimane & Downing, 2020; Knaak, Karpa, Robinson, & Bradley, 2016). This can be done by addressing mental health literacy, which increased with nurses who cared for patients who had mental illness (İnan et al., 2019; Knaak et al., 2017).
Findings from the present study align with this thinking. Prior to their rotation on an acute psychiatric inpatient unit, students described stigmatized views, fears for their personal safety and limited confidence in their ability to communicate effectively with patients. By preparing students before and during their rotation; using a self-directed approach; and modeling competent nursing care, instructors increased their students’ awareness and mental health literacy. Following their rotation, students all agreed that their experiences were positive, their thinking had transformed, and that the stigma they initially felt was misguided. Clearly, best instructional practice in mental health nursing is grounded in addressing stigma.
The etiology of stigma and the process of changing the way people think about mental illness is complex, and it is beyond the scope of this article to fully address the concept. High levels of stress impact mental wellness and make it difficult to embrace new perspectives. Nursing students entering mental health clinical placements are vulnerable to stress and may struggle to cope academically and personally when presented with stressors (Galvin, Suominen, Morgan, O’Connell, & Smith, 2015; Oner Altiok & Ustun, 2013; Registered Nurses Association of Ontario, 2017). High levels of stress create challenges for students as it impacts their confidence, ability to learn, and decision making (Oner Altiok & Ustun, 2013). Emotional distress can worsen and significantly hinder students’ educational experiences (Choi et al., 2016).
Best instructional practice must take students’ mental wellness into consideration. Students in this study welcomed instructors’ efforts to get to know them, and to understand barriers that could impede their learning, including issues affecting their own mental wellness. Comments such as: “What if I say the wrong thing …. will I be safe?” illustrate potential emotional distress. Experiencing stress in psychiatric clinical settings is not limited to students, mental health nurses are reported to have some of the highest stress among any group of nurses as well (Galvin et al., 2015). Promoting mental wellness and striving to mitigate stress associated with working and learning in this specialized area is not straightforward.
Promoting mental wellness includes balancing instructional support with students’ personal control over their learning. In their seminal research examining occupational stress, Johnson and Hall (1988) identified that when individuals have only limited control over job requirements but are in jobs that demand a great deal of them (such as nursing students trying to prepare for and succeed in clinical rotations), they experience significant mental strain. In mitigating this strain, Johnson and Hall (1988) found that the high demand being experienced by students is effectively buffered when both feelings of support and control are also high (Galvin et al., 2015). These results were similar to the present study, as the best practices students described addressed both instructional support and personal control of learning.
Instructional support
When students feel supported by their clinical instructors, they are more likely to have positive and successful learning experiences (Collier, 2018). The present study extends this understanding by articulating specific strategies that instructors can implement to provide needed support in mental health clinical placements. Mental health placements are unique, and instructors must recognize student concerns related to stigma, stress, limited mental health literacy, and their personal safety in order to support their students.
Supportive teaching strategies, such as instructors contacting students prior to their clinical placement, is a simple but very important first step. The information solicited by this type of contact provides clinical instructors with important insights about their students. It opens the door to better understand who they are as nursing students, what their goals are, how they plan to achieve them, and the kinds of challenges they face in other areas of their lives. In keeping with the constructivist thinking that guided this research, clinical instructors can use this insight to tailor their approach and construct an environment which better meets the individual needs of students. As described by participants in this study, when clinical instructors aim to understand the student experience, such as their mental wellness concerns, the students felt more supported and ultimately had positive educational experiences.
Personal control of learning
A striking finding from this study was how empowered students felt when instructors supported self-direction and provided opportunities for them to feel a sense of personal control over their learning. When instructors remained present and accessible, but still very ‘hands-off,’ they communicated their confidence in students’ abilities. When they invited students to choose their own patients, they conveyed their respect for students’ capacity to think critically.
Instructional practices that facilitate personal control of learning are well documented in the nursing education literature (Torbjørnsen, Hessevaagbakke, Grov, & Bjørnnes, 2021). However, limited direction exists for mental health clinical instructors, particularly on acute inpatient units. Findings from this study, which present specific strategies, such as remaining ‘hands-off’ (when in other clinical areas this strategy may not be advisable) make an important contribution to the field. This study found that in mental health clinical place- ments, students preferred having more control and independence in their education as it increased their level of performance. In clinical practice on medical units, this approach may be difficult to implement as students require closer supervision in performing skills or interventions such as hanging intravenous medications, as the potential to harm someone is greater. In mental health clinical education, the interventions are mostly communicating with patients and thus are less risky and do not require this level of supervision. Students in this study unequivocally identified this difference between clinical areas and were surprised at how much they enjoyed the independence they received, which positively impacted their view of the overall experience.
Further, students felt a sense of personal control over their learning when instructors worked collaboratively with them to set goals. This strategy created a more harmonious and less hierarchal experience. Participants found that the clinical instructor was less intimidating in this role and they did not feel as though they were being constantly evaluated, which students internalized as being trusted and competent in delivering care.
Limitations
In this small-scale descriptive study, limitations include a modest sample size and data collection from one English speaking institution. Further, implementing a single interview approach with each participant did not allow for repeated or follow-up conversations. Videoconference interviews may have restricted the interviewer’s observations of participants’ non-verbal communication cues. As instructors in mental health nursing courses, the research team may have inadvertently introduced biased interview guide questions and interpreted data in relation to their own subjective experiences. Possible future research on a larger scale should include multi-site and multi-jurisdictional sampling and research team members. Methodologies that integrate a series of interviews with participants, focus group sessions and survey instruments could build on the foundation established by the present study. Supplemental teaching strategies, such as simulation activities should be investigated further in relation to students’ perceptions of best practice in mental health nursing practicums.
Conclusions
The findings of this study indicated that nursing students valued feeling prepared at the beginning of the clinical placement; they felt empowered when instructors encouraged self-direction; and they appreciated positive role modeling by their instructors. The present study extends knowledge and understanding of clinical education in mental health by describing specific and effective strategies clinical instructors can implement into their practice. Additionally, this study demonstrated how mental health stigma and students’ mental wellness were unique challenges that played significant roles in how they learned during their clinical placement. Implementing these practices can positively impact students’ learning, their mental health literacy, and potentially, the care they provide to patients with mental illness throughout their careers.
Research funding: Athabasca University Graduate Student Research Fund (GSSRF) that covered the costs related to transcription, and incentives for participants.
Author contributions: All authors have accepted responsibility for the entire content of this manuscript and approved its submission.
Competing interests: Authors state no conflict of interest.
Informed consent: Informed consent was obtained from all individuals included in this study.
Ethical approval: Ethical approval was obtained from both Athabasca University and Mount Royal University research ethics boards.
References
Abraham, S. P., Cramer, C., & Palleschi, H. (2018). Walking on eggshells: Addressing nursing students’ fear of the psychiatric clinical setting. Journal of Psychosocial Nursing and Mental Health Services, 56(9), 5–8.
Adom, D., Yeboah, A., & Ankrah, K. A. (2016). Constructivism philosophical paradigm: Implications for research, teaching, and learning. Global Journal of Arts Humanities and Social Sciences, 4(10), 1–9. https://www.academia.edu/download/ 60883069/Constructivism-Philosophical-Paradigm-Implication-for-Research-Teaching-and-Learning20191012-85439- 1fft6xx.pdf.
Akinyode, B., & Khan, T. (2018). Step by step approach for qualitative data analysis. International Journal of Built Environment and Sustainability, 5(3), 163–174.
Alase, A. (2017). The interpretative phenomenological analysis (IPA): A guide to a good qualitative research approach. International Journal of Education and Literacy Studies, 5(2), 9–19.
Alhojailan, M. I. (2012). Thematic analysis: A critical review of its process and evaluation. West East Journal of Social Sciences, 1(1), 39–47. https://fac.ksu.edu.sa/sites/default/files/ta_thematic_analysis_dr_mohammed_alhojailan.pdf.
Booth, T. L., Emerson, C. J., Hackney, M. G., & Souter, S. (2016). Preparation of academic nurse educators. Nurse Education in Practice, 19, 54–57.
Bradshaw, C., Atkinson, S., & Doody, O. (2017). Employing a qualitative description approach in health care research. Global Qualitative Nursing Research, 4, 1–8.
Canadian Association of Schools of Nursing & Canadian Federation of Mental Health Nurses. (2015). Entry-to-practice mental health and addiction competencies for undergraduate nursing education. http://www.casn.ca/wp-content/uploads/2015/11/ Mental-health-Competencies_EN_FINAL-3-Oct-26-2015.pdf.
Choi, H., Hwang, B., Kim, S., Ko, H., Kim, S., & Kim, C. (2016). Clinical education in psychiatric mental health nursing: Overcoming current challenges. Nurse Education Today, 39, 109–115.
Collier, A. D. (2018). Characteristics of an effective nursing clinical instructor: The state of the science. Journal of Clinical Nursing, 27(1–2), 363–374.
Creswell, J. W. (2013). Qualitative inquiry and research design: Choosing among five approaches (3rd ed.). Thousand Oaks, CA: Sage Publications.
Doyle, L., McCabe, C., Keogh, B., Brady, A., & McCann, M. (2020). An overview of the qualitative descriptive design within nursing research. Journal of Research in Nursing, 25(5), 443–455.
Faulkner, S. L., & Trotter, S. P. (2017). Data saturation. Hoboken, NJ: Wiley Online Library.
Galvin, J., Suominen, E., Morgan, C., O’Connell, E. J., & Smith, A. P. (2015). Mental health nursing students’ experiences of stress during training: A thematic analysis of qualitative interviews. Journal of Psychiatric and Mental Health Nursing, 10, 773.
Goh, Y., Owyong, J. Q. Y., Seetoh, Y. M., Hu, Y., Chng, M., & Li, Z. (2021). Exploring pedagogies used in undergraduate mental health nursing curriculum: An integrative literature review. International Journal of Mental Health Nursing, 1, 47.
Grav, S., Juul, L. M. E., & Heilzen, O. (2010). Undergraduate nursing student experiences of their mental health clinical placement. Nordic Journal of Nursing Research & Clinical Studies, 30(1), 4–8.
İnan, F. Ş., Günüşen, N., Duman, Z. Ç., & Ertem, M. Y. (2019). The impact of mental health nursing module, clinical practice and an anti-stigma program on nursing students’ attitudes toward mental illness: A quasi-experimental study. Journal of Professional Nursing, 35(3), 201–208.
Ismail, M-N. L., Aboushady, M-N. R., & Esw, A. (2015). Clinical instructor’s behavior: Nursing student’s perception toward effective clinical instructor’s characteristics. Journal of Nursing Education and Practice, 6(2), 96–105.
Jack, K., Hamshire, C., & Chambers, A. (2017). The influence of role models in undergraduate nurse education. Journal of Clinical Nursing, 26(23–24), 4707–4715.
Janse van Rensburg, E. S. (2019). Educators: Are you adequately supporting nursing students during mental health placements? International Journal of Africa Nursing Sciences, 10, 43–48.
Johnson, J., & Hall, E. (1988). Job strain, workplace social support, and cardiovascular disease: A cross-sectional study of a random sample of the Swedish working population. American Journal of Public Health, 78, 1136–1342.
Knaak, S., Karpa, J., Robinson, R., & Bradley, L. (2016). “They are Us-We are Them”: Transformative learning through nursing education leadership. Healthcare Management Forum, 29(3), 116–120.
Knaak, S., Mantler, E., & Szeto, A. (2017). Mental illness-related stigma in healthcare: Barriers to access and care and evidence- based solutions. Healthcare Management Forum, 30(2), 111–116.
Kutcher, S., Wei, Y., & Coniglio, C. (2016). Mental health literacy: Past, present, and future. Canadian Journal of Psychiatry, 61(3), 154–158.
Lincoln, Y. S., & Guba, E. G. (1985). Naturalistic inquiry. Thousand Oaks, CA: Sage Publications.
Melrose, S., Park, C., & Perry, B. (2021). Creative clinical teaching in the health professions. Edmonton, AB, Canada: Athabasca University Press. https://www.aupress.ca/books/120303-creative-clinical-teaching-in-the-health-professions/.
Meyer, G. M., Nel, E., & Downing, C. (2016). Basic student nurse perceptions about clinical instructor caring. Health SA Gesondheid, 21, 444–452.
Niederriter, J., Eyth, D., & Thoman, J. (2017). Nursing students’ perceptions on characteristics of an effective clinical instructor. SAGE Open Nursing, 3, 1–8.
Oner Altiok, H., & Ustun, B. (2013). The stress sources of nursing students. Educational Sciences: Theory and Practice, 13(2), 760–766. https://files.eric.ed.gov/fulltext/EJ1017246.pdf.
Padagas, R. (2020). Nursing students’ expectations of their clinical instructors: Practical implications in nursing education. Romanian Journal for Multidimensional Education/Revista Romaneasca Pentru Educatie Multidimensionala, 12(4), 393–410.
QSR International Pty Ltd. (2018). NVivo. https://www.qsrinternational.com/nvivo-qualitative-data-analysis-software/home. Version 12.
Registered Nurses Association of Ontario. (2017). RNAO nurse educator: Mental health and addiction resource -Integrating mental health and addiction into the undergraduate nursing curriculum (202 pages). http://rnao.ca/sites/rnao-ca/files/Nurse_ Educator_MHA_Resource.pdf.
Reising, L. D., James, B., & Morse, B. (2018). Student perceptions of clinical instructor characteristics affecting clinical experiences. National League of Nursing, 39(1), 4–9.
Sadeghi, A., Oshvandi, K., & Moradi, Y. (2019). Explaining the inhibitory characteristics of clinical instructors on the process of developing clinical competence of nursing students: A qualitative study. Journal of Family Medicine and Primary Care, 8(5), 1664–1670. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6559080/.
Sandelowski, M. (2000). Whatever happened to qualitative description? Research in Nursing & Health, 23(4), 334–340.
Sandelowski, M. (2010). What’s in a name? Qualitative description revisited. Research in Nursing & Health, 33(1), 73–84.
Slemon, A., Jenkins, E., Bungay, V., & Brown, H. (2020). Undergraduate students’ perspectives on pursuing a career in mental health nursing following practicum experience. Journal of Clinical Nursing, 29(1–2), 163–171.
Snyder, B. L. (2020). Practicing what we preach: Teaching psychiatric-mental health student nurses to care for themselves. Journal of Psychosocial Nursing and Mental Health Services, 58(6), 40–45.
Stuhlmiller, C., & Tolchard, B. (2019). Understanding the impact of mental health placements on student nurses’ attitudes towards mental illness. Nurse Education in Practice, 34, 25–30.
Sweet, L., & Broadbent, J. (2017). Nursing students’ perceptions of the qualities of a clinical facilitator that enhance learning. Nurse Education in Practice, 22, 30–36.
Torbjørnsen, A., Hessevaagbakke, E., Grov, K., & Bjørnnes, A. (2021). Enhancing students learning experiences in nursing programmes: An integrated review. Nurse Education in Practice, 52, 103038.
Tsimane, T., & Downing, C. (2020). A model to facilitate transformative learning in nursing education. International Journal of Nursing Science, 7, 269–276.
Vuckovic, V., Carlson, E., & Sunnqvist, C. (2021). ‘Working as a real nurse’: Nursing students’ experiences of a clinical education ward in psychiatric care. Issues in Mental Health Nursing, 42, 1038–1047.
