Modern (1940’s-present)
33
Katherine Summers
Introduction
Modern medical practices are dominated by western medicine. All over the world westernized medical practice, based on science, has become the standard for treating diseases and illnesses. However, before the development of scientifically based medicine complementary and alternative medical (CAM) practices were standard. Traditional Chinese Medicine (TCM) practices, like herbal remedies and acupuncture, have been around for over 2000 years and account for the majority of CAM practices. Westernized medicine focuses on treating the specific disease with drugs and medicine. While TCM takes a holistic approach by treating the balance of body, mind and spirit, using herbal remedies and practices like acupuncture [5].
Both methods have different approaches to health issues, however there is potential for them to collaborate on the issue of women’s reproductive health. Women experience a plethora of health problems surrounding their reproductive organs, from period symptoms, pregnancy and menopause. The go to solution for issues like hormonal imbalance and period pains is to pop a pill to fix the problem. Then, if that pill doesn’t work try another, while also hoping that the plethora of potential side effects do not manifest. This approach is not very personalized and puts women at further risk of developing serious avoidable side effects. Under the TCM approach period pains and menopause side effects can be treated with herbs and acupuncture to relieve stress and balance the body. This article will discuss the ways that culture separates eastern and western medicine in women’s health regarding specifically focusing on the treatment of menopause and fertility, specifically in vitro fertilization, IVF.
Western Medicine Treatments for Menopause
Western medicine has become the conventional method for health treatments. The western medical profession is a predominantly male field and until recent years, informed by scientific research that often failed to incorporate female experiences [2]. Even today there are a lot of misdiagnosis surrounding women’s health however in the 1970s medicalization of menopause was considered complete [6].
For women going through menopause there are a couple treatment options. As a clarification menopause can be more accurately described as climacteric syndrome which is the decline of ovarian hormone levels which alters brain neurotransmission and provokes musculoskeletal pains, mood disorders, poor sleep quality and hot flashes. The most common side effect of menopause is vasomotor symptoms (VMS) which is responsible for hot flashes and night sweats [1]. For women above 60 years old the recommended treatment is menopausal hormone therapy (MHT), which can be done with estrogen (ET) and progesteron (EPT) therapy [7]. However this treatment requires women to not have contradictions or excess cardiovascular or breast cancer risks. The treatment can be tailored to a patient depending on pre-existing risks and willingness for treatment. These personalized treatments focus on the starting dose of MHT, the route of administration and the individual situation, risks and treatment goals [7]. While hormone treatments are successful in treating VMS caused by menopause, there are significant risks, like thromboembolic events, breast cancer and cardiovascular disease, and corresponding side effects to adding hormones into your body to regulate VMS.
Eastern Medicine Treatments for Menopause
Eastern medicine, specifically TCM, is about human physiology and pathology, as well as the diagnosis and treatment of disease and it reflects on the relationship between man and nature [4]. TCM has a clinical system that consists of four parts: medical theory, principle, prescription, and herb. The basic principle of disease identification and treatment is the concept of treatment based on syndrome differentiation (TSD). TSD includes advanced methods like “black box method” that explore the internal structure of a mechanism by observing the relationship between external inputs and outputs [4]. The TCM architecture is summarized in Figure 1, where the interrelated knowledge is composed of two subsystems that have multiple functions.
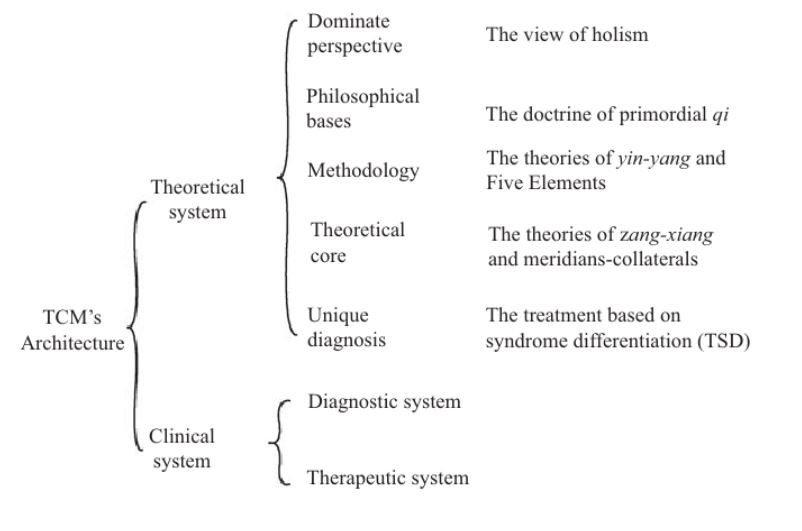
Figure 1. Structure of TCM’s architecture [4]
The main TCM treatments used for symptoms of menopause are acupuncture and herbal remedies. Acupuncture is the insertion of small needles into specific parts of the body and VMS has been proved to reduce with treatments of acupuncture. A study published by the medical journal of menopause found that acupuncture treatments were associated in a significant reduction in VMS, with an an increase in several quality of life measures. While significant clinical improvement was seen after only 3 sessions, maximum benefits were seen after 8 treatments with benefits persisting many months after treatments are stopped[1]. The acupuncture points are determined on a unique basis for each patient. Specialists conduct a physical exam, which includes pulse palpation and tongue inspection. A combination of medical history and results from a physical exam inform patient diagnosis and advise acupuncturists on point selection and individualized treatment plans. The subsequent improvement in quality of life when undergoing acupuncture treatments are sleep quality, menopause related symptoms, depressive symptoms, anxiety, perceived stress, and health-related quality of life. The use of herbal medicines to treat menopausal symptoms have also shown to be effective means of treating menopausal symptoms [3]. Specifically incorporating black cohosh root and dong quai in your diet through teas and foods helps relieve symptoms like hot flashes.
Intersection of Eastern and Western Medical Treatments
Eastern and western medicine treatments have both proved effective when treating menopausal symptoms, specifically VMS. Western medicine focuses on the use of hormonal therapy, however there is considerable risk of breast cancer and cardiovascular disease with this treatment. Eastern medicine uses acupuncture and herbal remedies to treat VMS holistically by focusing on your entire bodily health rather than one specific issue. There are no severe side effects to eastern medicine practices. However the use of eastern medicinal practices is not as well accepted and practiced. Why is this? Cultures that rely heavily on scientific research as the basis for practice do not support the pseudoscience of eastern techniques. A study evaluating the relationship between traditional chinese medicine and western practitioners, found that TCM practitioners were more likely to support and adapt to western practices than western doctors. Western practitioners tend to hold prejudices against eastern medicine and question its efficacy. Both practices are used and well established in different parts of the world and with further research there is potential for them to be combined to create the best treatment for menopause.
References
[1] Avis, N. E., Crawford, S. L., Greendale, G., Bromberger, J. T., Everson-Rose, S. A., Gold, E. B., et al. (2015). Duration of menopausal vasomotor symptoms over the menopause transition. JAMA Internal Medicine, 175(4), 531-539. doi:10.1001/jamainternmed.2014.8063 [doi] <https://pubmed.ncbi.nlm.nih.gov/25686030/>
[2] Gershon, L. (2021, “). Myth and misdiagnosis have plagued women’s health for centuries. Smithsonian Magazine, <https://www.smithsonianmag.com/smart-news/western-medicines-woman-problem-180977925/>
[3] Hardy, M. L. (2000). Herbs of special interest to women. Journal of the American Pharmaceutical Association (1996), 40(2), 234-242. doi:<https://doi.org/10.1016/S1086-5802(16)31064-6>
[4] Jiuzhang, M., & Lei, G. (2009). A general introduction to traditional chinese medicine (1st ed.). Baton Rouge: Taylor & Francis Group.
[5] Lam, T. P., & Sun, K. S. (2013). Dilemma of integration with western medicine – views of traditional chinese medicine practitioners in a predominant western medical setting. Complementary Therapies in Medicine; Complement Ther Med, 21(4), 300-305. doi:10.1016/j.ctim.2013.04.003 <https://www-sciencedirect-com.libproxy.clemson.edu/science/article/pii/S0965229913000824>
[6] Singh, A., Kaur, S., & Walia, I. (2002). A historical perspective on menopause and menopausal age. Bulletin of the Indian Institute of History of Medicine (Hyderabad), 32(2), 121-135. <https://pubmed.ncbi.nlm.nih.gov/15981376/>
[7] Stuenkel, C. A., Davis, S. R., Gompel, A., Lumsden, M. A., Murad, M. H., Pinkerton, J. V., et al. (2015). Treatment of symptoms of the menopause: An endocrine society clinical practice guideline. The Journal of Clinical Endocrinology & Metabolism, 100(11), 3975-4011. doi:10.1210/jc.2015-2236 <https://doi.org/10.1210/jc.2015-2236>
