21
November 25
Seven Dolors, Albany
From the outside the gothic ornate cross-shaped church was a feast for the eyes. From the inside the stained glass windows and Way of the Cross grabbed my attention from the moment I walked in and again when I realized their inscriptions were in German. I recognized St. Benedict and St. Scholastica, St. Blase, St. Christopher, St. Peter and Paul, St. Gertrude and the Infant of Prague but others were beyond me. The dolors , sorrows, were illustrated in a stunning set of seven circular stained glass images surrounding Mary. The traditional style of the church matched well with Father Edward, whose explanations of Biblical history were always presented with interesting detail and his own fascination readily apparent. From the two sentence gospel story of Luke 21:1-4 of the widow who tithed more than her share as an example, Father Edward highlighted the end of the Liturgical year being heavy with stories of persecution but also with hope and the knowledge that “our faith will rise and God will be in our lives.”
Dolors: Side Effects
Dolors. I tried not to dwell on the side effects or complain unless someone inquired specifically, but there were dolors throughout the cancer treatment because cancer is cancer–an ever present, all-encompassing, insidious, emotionally- invasive nuclear bomb–not only mutation at the cellular level. With each diagnosis I pictured it as an atomic bomb, the ripples spreading far and the fall-out never-ending. With each diagnosis I missed my healthy past and mourned the unknown but darker future.
With a few friends sharing their experience after being diagnosed recently with breast cancer and remembering being handed a Chemo 101 folder nine years before, I attended a Chemotherapy Education class at the Coborn Cancer Center. Honestly I also was in for the cool Thirty-One bag of treats that came with the appointment. The class was me in a patient education room with a revolving cast of medical professionals. First I met with an upbeat dietitian who showed me several sections in a ½ inch thick spiral bound book. Next, a chemo nurse who provided general hygiene information and side effect management, flagging sections in the manual. Finally, a pharmacist explained how meds are ordered and dosed and the importance of not mixing in other supplements. I noticed she was struggling as she explained the process and then confided that she was a cancer survivor. “You’re concerned about recurrence?” I guessed. She could only nod, closed her eyes briefly and then continued. I had two friends who had been inspired to become nurses after breast cancer treatment and could see the joy serving others brought them but this poor woman was heavily weighed by her fears every day seeing other patients’ recurrence.
From head to toe, it seemed cancer had affected me physically and mentally, I could list a few woes as well. Note: if you are squeamish you might find sections repulsive and if you are my son, you might want someone to screen this part for you.
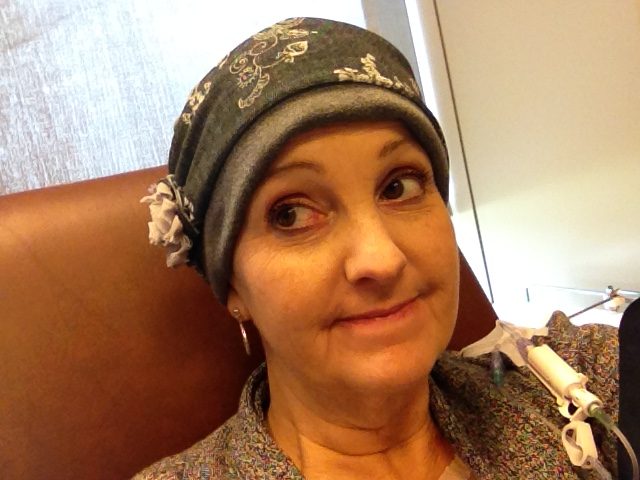
Side effect–Hair loss: Is it worse to have no hair or unwanted hair? I had three courses of chemotherapy a

nd lost my hair each time. It was actually a bit painful plus goosebumps on a bald head was a very unusual sensation. My collection of wigs, scarves and baseball hats saw me through months of baldness with my favorite chemo scarf in a classic French toile print on deep red fabric that my dad picked out and Mom sewed. Mom and Dad teamed together in my first round and made chic headcovers that were a cross between a surgical cap and a chef’s hat. Sherri, my sister-in-law, used her mad sewing skills to make beautiful and stylish headcovers for round three.

I found it interesting when regrowth would appear and the part on my forehead was still in place, the hair follicles trained until it was ¼ inch and it went feral, no longer parting. It also came in 0h-so-soft, baby hair, that people would ask to touch. Unfortunately, the color was what I called Loreal Old Rodent 114B, which I covered with semi-permanent dye. It was very curly after AC chemo and more wavy after TCHP, but each time eventually grew back to stick straight and I would work to train in a side part. Each time I bought one container of Tigi Catwalk Curls Rock Curl Amplifier and by the time the product was gone so were the curls.
One thing I knew for certain: many people equate health with hair. If you aren’t bald or in that obvious stage of regrowth, many assume you have recovered. I didn’t feel it was necessary to educate the casual comment, “You look well” with a nod to the hair. On the inside I would wince whenever someone would say, “You look so good in that short haircut. I could never do short hair.” I lacked the smartassness to reply, “Me either,” but would reply in my thoughts, “Um, it was not a choice and you probably could do short hair if you had no other option.”
With the first diagnosis, I could not find much information about how long it would take to grow back to the point where it looked like a pixie cut and not a sick person so I enlisted the help of Ben who dutifully took a picture of me every Monday for 30 weeks to document the hair growth. The best part was he was never satisfied unless I had a genuine smile and he would take extra shots each week until he had captured a real smile. I put it together as a video montage and uploaded it to YouTube. Search for ChiaLinda; yes, like a chia pet, and enjoy our collaboration.
The best wig I had was purchased at Aurora Salon a mere two miles from our home. Kristen was incredibly helpful in picking styles and colors from her in-stock selections then ordered three wigs for me to try. Two were okay but the third was the best hair I would ever have. I was wearing it at ROCORI during conferences and passed a woman in the hallway I knew from a tap dance class we took together. “Oh, I love what you have done with your hair!” she gushed as she reached out to touch a strand, then recoiled, “A wig? Is that something just for fun?” I explained the situation and assuaged her embarrassment by taking her reaction as a compliment. I thought I would burn it after my hair grew in, but I kept that highlighted bob buried deep in a box with scarves, wig shampoo etc. I dug it out and wore it after the next chemo treatments left me bald again.

When my hair was really falling out, I enacted a bit of shredder’s revenge on our dog Jet, whose hair I had swept up for years. I stood out on the deck and called her close then rubbed my head over hers while shedding on her. Then I swept it up because finding hair was always another small stab. I generally shaved my hair short once the shedding began and did a top-to-bottom house cleaning to sweep or vacuum up every last strand, even cleaning out the vacuum brush roller after so I wouldn’t be saddened when I saw the hair I’d lost. Plus, that is one awful task and I could then go over a year without cleaning it again.
For my third round of chemo, cooling caps were an option, but I was fighting off brain cancer and felt that I needed every hot chemo drug surging through my head, even in the hair follicles. Also I had read briefly through the Penguin Cap process and it was daunting! I was not great with hair, but not having any or having to wait for it to grow back into a style I wanted was frustrating.
Perhaps some of the most unusual advice: never take your nasal hair for granted. You might never have pondered what good it was, but if you had none, you’d know. Your nose runs and not like when you have a cold with a runny nose. Nothing stops it: without hair to catch on you don’t form boogers. I am telling you it is possible to miss boogers. No amount of sniffling will keep up if you get a cold with a bald nose. The TCHP chemo combo caused my nose to run so it was a constant battle. I could actually feel my nose tickle during infusions. It did improve over the weeks until the next infusion and old faucet nose would start dripping again. Next time you are having a bad day, take in a deep breath, toss your head and appreciate your gorgeous, luxuriant nasal hair.
After AC with round one, my hair grew back so curly and thick on my head, but also in creepy mutton chops of light-colored fuzz along my face. After I researched a bit, I shaved it clean off and it never re-appeared. It was both annoying and comical to have unwanted hair after months of being head-to-toe bald. And while it was nice not to shave my legs or have any other grooming chores, it was like an odd flash of puberty when the unwelcome pubic and axillary hair reappeared.
Side effect–Gastrointestinal Woes: In the Hollywood version of cancer, the emaciated bald cancer patient is bent over the toilet barfing their guts out. Every patient is different and their drug regimen is different with each drug carrying a list of formidable side effects. Often the list contained side effects that seem diametrically opposed like diarrhea and constipation. How can you have both? Well, read on if you are brave! In four rounds of AC chemo I had a predictable pattern: chemo for breakfast every other Thursday, Friday and Saturday with insomnia and hunger from steroids given as pretreat meds, mild nausea kept at bay throughout the weekend by an array of post-treatment meds, culminating in constipation from the anti-nausea meds until Tuesday. I had never experienced constipation before and was amazed at how uncomfortable it made me. The steroids gave me added pep and an insatiable appetite so I was uncomfortably full yet so hungry.
With my recurrence, I had eight rounds of TCHP. Unlike AC, the side effects varied each round, maybe because there were four drugs, each with a list of side effects, some the same, others unique to one drug. Thankfully, they were not simultaneous and so were tolerable. However, there was a side effect overlap with each treatment. After constipation from the anti-nausea meds, Perjeta’s diarrhea would start. Several times it was the same trip to the bathroom in what I dubbed a poonami: every sort of poo in one setting. More than once I was sure I had unloaded food I had not yet eaten. It was hard to control and often kept me at home. Honestly, 2016 ongoing my life was a gastrointestinal challenge to keep things running smoothly, but not too smoothly. Experiencing the side effects was not a treat, but worrying the side effects would affect the quality of life too much was not on the list, but one of the worst side effects!
Side effect–Aches and Pains: After each chemo treatment, Neulasta was an injection given to boost white blood cell development to support my immune system. It was several thousand dollars per injection per round of chemotherapy but much cheaper than having blood counts so low that I’d end up neutropenic and needing to be hospitalized for tens of thousands of dollars for a few nights stay. Neulasta was injected after chemo initially but then studies showed it was more effective if delivered a day after treatment so an auto-injector with a timer was developed and taped to my skin for at home injection. The injector made all kinds of beeps and LED lights flashed. I appreciated the Neulasta for keeping me out of the hospital but it caused some impressive bone pain. Other chemo patients and I would compare our locations. I seemed to feel it most in my legs and cheekbones and skulls. It created a headache unlike anything else, but was very predictable and gone in a few days. I tried to “offer it up” as my Mom would recommend anytime we had pain as kids. I pictured the pain growing healthy white blood cells and took Claritin as it really helped even if no one could explain why.
At age 39 in 2009, the four doses of AC threw me into chemical menopause. Along with the classic internal inferno problems, early menopause did a number on my bones. Osteopenia was diagnosed and bone-building bisphosphonates were prescribed to treat it. I added more calcium and vitamin D and hung up my ice skates and cross country skis and all high-heeled footwear. I enjoyed the sports and fancy feet, but the risk of falling outweighed the rewards. The bisphosphonates were delivered via a shot every 12 weeks for two years and produced some impressive bone pain, but no fractures = win!
Pain: Surprisingly, I never felt ill from the cancer itself. The treatments had side effects and I had some rib pain for a few months before we detected cancer in the fifth rib, but I never experienced weight loss or any sign that anything was amiss. It was very hard to hear that once I hit stage IV, we were in more of a palliative approach to treatment. We could use radiation for bone pain, but were not expecting to treat it. I felt pain, but “earned pain.” My primary doctor used that term and it helped me differentiate between pain from activity versus cancer progression. I knew cancer pain was usually worse at night so I was acutely aware of pain at night if it lasted more than a few days. The worry about the pain was often worse than the pain.
Side effect–Scarring: Due to the scars from multiple surgical procedures that left my chest a roadmap of breast cancer placemarkers, I joked that I needed a three or four piece swimsuit. My donor site for the new girls ran from hip to hip. I had five drain holes that left perfect circular scars. The axillary node dissection puckered my armpit. Four explanted ports left slightly raised two inch scars, plus the current port buried under its scar on my chest. The radiation did not leave visible scars, but that area would always be more tender.
Lymphedema:Lymph nodes are removed to check for cancer spread. I had three removed in 2008 and eight in 2017. There is no set number of lymph nodes, but since I was missing a twelve pack, I was uber-careful not to have blood pressure or blood drawn on my right arm and wore compression sleeves with fun tattoo patterns like pirate themed or butterflies for the first year and then after whenever I could feel a heaviness. I measured my upper arm every day religiously with three freckles as landmarks to watch for swelling. Lymphedema is a complication with few treatment options once it progresses so I was vigilant about my arm. The swelling can be mild or to the point where the arm loses all function. Thanks to Scott’s coworker occupational therapist with extra lymphedema training, I had an Alf-the-alien-colored compression wrap system that I would use if there was even the slightest bit of swelling. It was a 90 minute daily process wrapping from neck to knee then laying still while the system buzzed through its process, the tubing in the wrap inflating and deflating from my torso to my right shoulder, arm, wrist and finally my fingers. I also had a medically prescribed Jobst compression sleeve similar to what a dog trainer would wear on their arm, a big padded blue sleeve. Some studies showed that the changes in air pressure could trigger lymphedema so I hauled that huge sleeve sacrificing precious luggage space. It was a struggle to don and doff and would leave huge dimples in my arm, but was effective.
Glow-in-the-dark private parts! Well, not exactly, but during the chemo education I received after the recurrence, the nurse mentioned sex was safe with this regimen. “Wait, are there some where it is not?” She listed a few, including my first round of AC. Not only was I unaware, but I was confident there had been no reduction in the love-making department at that time. Scott and I spent the trip home from St. Cloud to Richmond trying to come up with clever ways to explain it including a reference to Three Mile Island’s tunnel of love, but Nuclear Nooky was the winner!
Side Effect–Fatigue: Fatigue is defined by Mayo Clinic staff as “Unrelenting exhaustion, that lasts longer, is more profound and isn’t relieved by rest. It’s a nearly constant state of weariness that develops over time and reduces your energy, motivation and concentration. Fatigue at this level impacts your emotional and psychological well-being, too” Mayo. I had a two-prong approach to combating any tiredness: caffeine but only until noon and by never saying, “I am tired.” I firmly believed our bodies can hear us and not only with our ears. I strongly believe that when we complain about being tired, it compounds and reinforces the problem. In truth, I wanted to be unwavering against fatigue and every mutinous mutation. At the end of five months of TCHP in March 2016 I walked a mile. One mile. It took me 34 minutes. It was grueling! I felt like I was hit by a rendering truck, maybe backed over a few times. I was so deconditioned by the chemo but so proud that I made the distance.
Throughout my treatments I was proud that I rarely napped because if I napped, I would struggle to sleep at night. While home from UMD in his senior year, Ben caught me asleep while we watched a movie and expressed his surprise to Scott. It was a rare occurrence.
Side Effect–Emotional and Mental Distress: Cancer’s effects were nuclear in my life; the mushroom cloud of an atomic bomb perfectly pictifies the emotional and mental fallout. After a diagnosis, we were always overwhelmed by the support of friends and family. The news would travel fast, which I preferred over needing to tell someone. Social media with Facebook and CaringBridge helped me let everyone know how I was doing physically and emotionally. I was always relieved when our family would return to its normal state of operations rather than feeling Scott, Mack and Ben were being careful or treating me differently. We had a great relationship, further strengthened by being able to talk about anything including end of life.
Side Effect–Worry: “It’s nothing til it’s something,” was the mantra I tried to use to combat worry. Inevitably I would run through every possible scenario from best to worst results. “Let go and let God” was another mantra I tried, but my brain seemed hard-wired to worry. There was overall concern and then clinical, data-driven concern like tumor markers. When they are in the normal range, the tumor markers, which gave an indication of the amount of circulating tumor cells in my blood, were just a number. A little increase was often followed by decrease, but when a pattern formed slowly over the course of a year in a gradual, but steady upward trend from the test results posted every three months. As the numbers increased so did my concern and the amount of time I ran scenarios: was this going to show up in imaging as a tumor? If so, where? Brain, bone, liver, lung? –all the popular hangouts for BC tumors. Would it be better in one location than another? The worry itself was like a tumor. I had to summon all my positive thinking mantras to quiet the chattering worry bugs.
End of Treatment: This nebulous phenomenon is hard to explain, but after treatment is completed, I experienced a sense of unease. After dozens of appointments, I suddenly had nothing until a follow-up in six months. Other survivors agreed that none of us missed the appointments, but it was disturbing not to have someone checking our blood levels or having scans on the watch for recurrence. I wanted to celebrate fully, but there was a cloud of wariness each time that held me back.
Side Effect–Grief: There was the grief, the loss of the life I had, being prematurely yanked from my career, seeing all the pain my health caused others, the stress and worry with every test and scan, and oh, the tears. According to a BBC website, I had shed 598 oz or 74 cups in my lifetime, just one calculation from their “How much of your body is your own” section. In case you were wondering, it also calculates the amount of poo and farts you have produced in your lifetime. (Go ahead, check the bibliography now for the website then please come back and finish the book.)
Side Effect–Financial Concern: Thankfully I always had health insurance while dealing with the catastrophic expenses of treatment. I kept track of all bills during my first diagnosis and with the total cost of treatment including reconstructive plastic surgery with hospital stay could have purchased a lovely lake home.Even though no one ever suggested it, I carried the burden of knowing I had driven up our district health insurance premiums. The costs of stage III treatment were even greater as I was hospitalized with sepsis and the immunotherapy drugs were very expensive on the year-long treatment plan. Metastatic cancer meant treatments for the rest of my life: chemotherapy drugs plus brain radiation with surveillance MRI’s and PET scans screening their effectiveness in addition to immunotherapy drugs. None of it cheap, but to me it was priceless as it gave me more time.When our insurance committee chose to join a larger pool which helped make outliers like me less detrimental with larger numbers, it assuaged my sense of burden on my coworkers. I know there were many years where I never reached my deductible and was not thankful enough for my health! Prior to cancer, I was also blissfully unaware of the political milieu. Health insurance lifetime limits and pre-existing conditions exclusions from eligibility were debated during the passing of the Affordable Care Act. I would have been destitute without those provisions. Being forced to choose which treatments or scans without insurance would have been a financial cancer.
Side Effect–Fiction affliction: A peculiar feature during treatment for stage III was I struggled to read fiction. It was too ephemeral in my heavy reality so I turned to non-fiction. This might not be of note except it also prompted me to change my career from library media specialist to English teacher. I wanted to be with students more and technology less, to make an impact with students directly in the classroom and not indirectly by fixing a login here and a network snafu there. I eventually got back to enjoying fiction, but had the same recoil when the brain tumors appeared. Fiction could not hold my attention so I mainly read non-fiction in history and biographies. While writing Once Upon the End, I read mainly memoirs–about one a week for a year. A boy’s story about growing up during the 1940’s in an orphanage in Duluth, a girl with multiple schizophrenic family members, stories of saints–Maximillain Kolbe, St. Bernadette of Lourdes, Jim & Jeannie Gaffigan’s memoirs of dealing with her brain tumors, I needed to hear others’ stories as I wrote a bit of my own.
Side Effect–Chemo Brain: There was no clinical evidence to be found for chemo brain so I decided it would not happen, as resolutely as when I refused to have chicken pox but had “the dots” as a preschooler. So while I did not have chemo brain, the ever-present concern was a distraction that kept me from being 100% focused. I could be distracted by work or family or entertainment, but the reminders like side effects and appearance with hair loss kept cancer on the front burner. I also blamed appointments and shuffling work and family around appointments to be a valid excuse for any slack in mental acuity. During February 2009 I had 19 appointments. My appointments had appointments. Nineteen appointments plus all the normal demands of life. When the appointments eased up, I felt more clear. It also coincided with treatment ending.
Side Effect: Fear of the Future: I realized my prognosis made others uneasy. A friend interrupted her description of her retirement plans abruptly, grabbed my arm and lamented, “I am such a bitch!” for her guilt in looking forward. I shoved her playfully ala Elaine Benes and assured her that I was not hurt or offended, maybe jealous. I told her a lot of my life plans were “Maybe.” Maybe had been a working title of this book since it seemed a lot of my plans were tentative. I also realized when I wrote this that I had spent my life saying tentative so there is always room for growth.
I dreaded the loss of control taking away my abilities one by one then leaving me lingering. Although knowledge is power, it also made me aware of a future I did not want; I had read my fair share of books about the end of life before Dad and Mom passed and had helped with their cares. I would try to use their reactions to model my own losses. I remember parenting my parents when discussing why driving was no longer an option for my Dad. He was not angry or defensive, just sad. Somehow that was worse. We looked out the large windows of their second floor apartment and I asked, “which way is north?” Dad peered out the window and looked up and down the street, likely for any sign to help. “You’re right. If I can’t find north, I can’t drive anymore.” Sometimes I would have a headache and wonder if this would be The One. A tumor located where treatment was a challenge or would cause seizures or loss of physical control. For example, losing my ability to drive would be a huge blow to my independence. I had a list of family and friends who had offered rides, but having to ask would be a bugbear.
Lingering: Most likely, I will not be aware if I linger. I only want enough time for the boys to say goodbye then off to met my Maker. When the nursing staff knows my time is close, please let me go. Based on what I have read about end-of-life,silence is preferred as talking and saying my name might keep me from moving on. Prayers of course would be welcome! But the only lingering I want is in Heaven. My title refers to hovering: hovering seems more intentional and has a more positive connotation than lingering to me.
Side Effect–Awareness of Mortality: Each scan found me facing my mortality. Once as I drove from Paynesville to Sartell via Highway 23 without Scott because of COVID visitor restrictions, I was met with my mortality in two bursts. The interchange of Hwy 23 and Interstate 94 had recently been prepped to be redesigned to improve safety. As I drove East, a semi decided it would dart across 23 in front of me. I slammed on the brakes with plenty of space, but close enough that the blast of air from the rig rocked my car. I honked and swore. Then proceeded with my heart pounding madly. It had distracted me from worrying about the MRI results I was facing. I had barely gotten up to speed when a truck ran through the stop sign on the 94 on-ramp from the Twin Cities. I slammed on the brakes, honked and swore. The rush of adrenaline hadn’t dissipated from the first. Everyone can relate to that intense awareness after a near accident when your entire existence feels elevated. Except for me it doesn’t go away. There I was post two near accidents while en route to find out if I was closer to dying. I laughed and appreciated the check that I am not guaranteed to see cancer as my end. That awareness and elevated sensation is duller, but it created an appreciation for terminal cancer everyone can relate to. In my world the semi just keeps crossing.
Side Effect–Uncomfortable Hospital Stays: My stays were fairly uneventful, but Mom had quite an experience. When Mom was at The University of Minnesota Fairview Hospital dealing with her ovarian cancer diagnosis, I drove solo or with Dad nearly every day. Dad did not like staying but we needed to stay overnight to meet with all the doctors and fellows and specialists. Dad chose to stay in the very stuffy family room, but I could tell at least half the people would be loud snorers and I would not get any sleep packed in with strangers so I chose to stay in Mom’s room. She had the double room to herself until a very old, thin woman was assigned the other bed. Mom had the bed near the window, so I was very circumspect about passing by the other bed. Her roommate was very uncomfortable and very vocal about it. No one really knows the pain tolerance of another but she screamed when they took her temperature and wailed when they took her blood pressure.
Mom and I exchanged raised eyebrows and tried to read our books as they took her vitals. The nurses murmured that she did not belong in the oncology ward given her condition. After they left, she began moaning softly then loudly. She yelled repeatedly, “I want my meffamone.” The nurse brought her water and warm blankets. “I want my meffamone.”
“Methadone,” I whispered to Mom, “drug addiction.” Mom’s eyes widened and she reached for her rosary to pray for the distressed soul. The roomie quieted down and Mom found medicine-assisted sleep. I was restless, but determined to be quiet. There was no bed or recliner so I had shoved two waiting room-style chairs together facing each other and angled toward the window sill that was a similar height. I had a pillow for one chair and shimmied under the back of the other with my feet on the window sill. It was not ideal. I had earbuds and kept playing Gregorian chants to calm my mind, but slept little.
Around 2:15 am a rounding nurse checked on the roommate who had been very quiet for the past few hours. The nurse’s panic calls for assistance woke us up. The woman’s heart rate was low, her temperature was low and she was non-responsive. I have no idea how HIPAA (Health Insurance Portability and Accountability Act) laws work, but we heard a lot. She was still coming off heroin in addition to a chemotherapy infusion two days ago. Apparently not a good cocktail. Within minutes the other side of the room was full of medical personnel trying to revive her. They were able to stabilize her and quickly moved her to another location. One nurse came back for her belongings and found only one shoe. We also learned she was not an old woman, but close to my age.
When I left the room the next morning to rustle up some breakfast, I admonished Mom, “Lay off the heroin, missy,” then saw an orderly on the other side of the room whose eyebrows had nearly left his face. Mom’s naughty grin in response was etched in my memory.
Side Effect: Death May Occur: I wrote about Mom’s decision to end treatments in my November 14th journal entry. She also had to make a decision that had kept me awake. She woke one morning with vision changes, noticing odd rings of light around the streetlights. Her wonderful PCA helped arrange an appointment to have her eyes checked. It ended up being a problem with the temporal artery and a procedure was scheduled to fix it. Thankfully Patti was checking on all things medical and knew Mom had had this procedure in the past and it was a once-in-a-lifetime deal. The doctor called me to explain that without the procedure option, Mom could take steroids, but they would hasten the cancer growth. I tossed and turned unable to grab quality sleep trying to phrase the question, “Would you rather go blind or live longer?” I agonized until I visited Mom early the next day.
“Hmmm, I’ll take the steroids. I want my eyesight,”she answered without pause or self-pity, but as nonchalant as if ordering off a restaurant menu. Her strength was a testament to me then and a rock for me as I faced treatment choices. In my prayers I asked for grace to deal with any new diagnoses or problems. Mom’s faith was never more evident than at the end. I prayed for spiritual resilience and worried that my faith was fragile when doubt crept in or scans showed progression. Dad was so peaceful and slept out. We were fortunate not to see either in pain and struggling. Please pray for a graceful landing for me too.
