Katherine Skola
Introduction
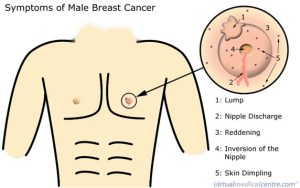
Breast cancer is a type of cancer that occurs in the breast due to cells growing out of control. It can spread to other parts of the body through the lymphatic system. Breast cancer is often thought to be only in women, but men can also develop it because they also have breast tissue. Even though men can get breast cancer, they are at a lower risk with a 1 in 833 chance of being diagnosed in their lifetime (American Cancer Society, 2021). Because rates are lower in men than in women, it is often not talked about as something of concern to men and signs and symptoms may be overlooked. The signs and symptoms for men are similar to those of women including painless lumps in the breast tissue, changes in skin on breast, changes to the nipple, and discharge from the nipple (Mayo Clinic, 2020). The lumps in men might be more noticeable due to men generally having less breast tissue than women which could explain how breast cancer in men has more involvement with the lymphatic system. Despite similar symptoms as women, breast cancer in men is not often diagnosed until it is in stages 3 or 4 which may be harder to treat (Yalaza et al., 2016).
Risk Factors
The risk factors for men getting breast cancer are similar to that of women. Some common risk factors include older age, family history of breast cancer, and obesity (Mayo Clinic, 2020). Male breast cancer is often diagnosed at age 60, but cancer risk increases as men age. Men who have any family members who have had breast cancer have double the risk of developing the disease compared to those without a family history (Sanguinetti et al., 2016). Obesity increases the risk for breast cancer in men due to the fat cells in the body converting androgens into estrogen which increases the risk for developing breast cancer (American Cancer Society, 2021). Men born with Klinefelter Syndrome have more estrogen and it increases the risk of breast cancer between 20 and 60 times compared to the general public (American Cancer Society, 2021).
Another risk factor that cannot be prevented is race. Black men are 1.6 times more likely to develop breast cancer, are often diagnosed at later stages, and have a worse five-year overall survival rate compared to other races (Shin et al., 2014). Like breast cancer in women, however, the chance of a male developing breast cancer is likely due to many risk factor effects at the same time (Sanguinetti et al., 2016). Because of this, there is no one risk factor shown to cause breast cancer but stopping risk factors that are preventable can help decrease the chance of developing it.
Men can take action to help reduce the likelihood of getting breast cancer through lifestyle choices. Because obesity is a risk factor for breast cancer, actions such as a healthy diet and physical activity can prevent obesity and reduce the chance of getting breast cancer and other serious diseases.
When to Seek Help
Men should seek help from a doctor when signs and symptoms such as lumps in the breasts, changes to the nipple, or discharge are seen. These symptoms, alone or together, could be early signs of breast cancer and can help diagnosis at an earlier stage. Most men do not see a doctor about breast cancer unless they have a family history or are experiencing symptoms due to the rarity of it. Men who have the BRCA1/2 gene, however, should start screenings at age 35 as they are at an increased risk due to genetics (Susan G. Komen, 2020). If men feel any type of lump or experience any symptoms, they should go to their doctor immediately to seek help.
Diagnosis
Diagnosis of breast cancer is not screened for as often as women due to the lower rates in males. There are no recommended image-based screenings for males that are not showing symptoms such as lumps or if they have a family history (Woods et al., 2019). This causes many diagnoses to be made at later stages for males than for females. When screening is done, imaging tests are the most common. These include diagnostic mammograms, ultrasounds, nipple discharge tests, and a breast biopsy (Burstein et al., 2018). The diagnostic mammogram uses x-ray exams to look for changes in breast tissue while the breast is pressed between two plates. Ultrasounds are used to examine tissue and are often used to examine changes found in mammograms. During a nipple discharge test, fluid collected from the nipple is looked at for cancer cells. A breast biopsy is normally done after other tests detect cancer. In this test, cells from the area found in other tests are taken and looked at to see if it has cancer cells. Seeing a physician regularly and performing self-breast exams can help catch cancer at an earlier stage and allow treatment to start sooner. Below is a link to a video explaining how to perform a self-breast exam for males from the Male Breast Cancer Coalition (2017).
Treatment
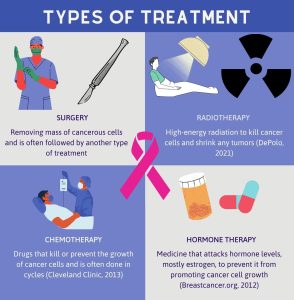
The treatment used for male breast cancer is dependent on multiple factors, as is the treatment for women. Because cancer is often caught in later stages in males, treatment options vary on the stage of cancer. Treatment options include surgery, radiotherapy, chemotherapy, and sometimes hormone therapy (Yalaza et al., 2016). Surgery includes removing the mass of cancerous cells and is often followed by another type of treatment. Radiotherapy uses high-energy radiation to kill cancer cells and shrink any tumors (DePolo, 2021). Chemotherapy is given to a patient and is made up of drugs that kill or prevent the growth of cancer cells. It is given in cycles and is given before or after surgery depending on the size of the tumor (Cleveland Clinic, 2013). Hormone therapy uses medicine to attack hormone levels, mostly estrogen, to prevent it from promoting cancer cell growth. There are many types of hormone therapy drugs, but because rates of breast cancer in men are so low, there is no evidence of which works best (Breastcancer.org, 2012). Treatment for breast cancer in males has not been tested with studies. Because the rates are so low, treatment is often guided by results from studies done on women with breast cancer (Cancer Treatment Centers of America, 2019). It is important for men to work closely with doctors on treatment options, especially with hormone therapy treatment as it can affect each man differently.
Conclusion
Breast cancer in men and women is not that different. Despite there being a difference in the amount of breast tissue and hormone levels, there are a lot of similarities when it comes to signs and symptoms, the diagnosis process, and treatment options. Breast cancer in men is often detected later than it is in women, so it is important for men to learn the signs and symptoms of breast cancer as well as know the risk factors that could increase their risk for developing it. The overall survival rate for men diagnosed with breast cancer is 45.8% while women have a 60.4% survival rate (DePolo, 2019). With an overall lower survival rate, it is important to educate men about their risk of getting breast cancer and how to look for signs and symptoms. Many men that are faced with breast cancer also face issues with mental health. Because there are lower rates of breast cancer in men, many are not involved in support groups and do not join women support groups (Cancer Treatment Centers of America, 2019). Without these support groups, the mental health of men with breast cancer is important to discuss. Almost a quarter of men with breast cancer experience stress symptoms related to breast cancer (Brian et al., 2016). With lower rates in men than in women, breast cancer and its effect on men is often not talked about. Bringing awareness to the topic can help provide information on something that was formally not seen as a type of cancer for men.

Chapter Review Questions
1. What age should men with the BRCA 1/2 gene start getting screened for breast cancer?
A. 60
B. 35
C. 20
D. 40
2. Which of the following types of diagnostic screening for breast cancer in men was not discussed in this chapter?
A. Mammograms
B. Nipple discharge test
C. Ultrasounds
D. MRI Scan
3. How many men with breast cancer experience stress related symptoms related to breast cancer?
A. Almost a quarter
B. Almost half
C. Almost three quarters
D. All men with breast cancer
References
American Cancer Society. (2021). Breast cancer in men. https://www.cancer.org/cancer/breast-cancer-in-men.html
Brian, K., Williams, B., Iredale, R., France, L., & Gray, J. (2016). Psychological distress in men with breast cancer. Journal of Clinical Oncology, 24(1). 10.1200/jco.2006.10.064
Burstein, H., Harris, J., Morrow, M., Jain, S., Gradishar, W., Wolff, A., Domchek, S., & Davidson,N. (2018). Tests for breast cancer in men. American Cancer Society. https://www.cancer.org/cancer/breast-cancer-in-men/detection-diagnosis-staging/how-diagnosed.html
Cancer Treatment Centers of America. (2019). What’s the difference? Male breast cancer and female breast cancer. https://www.cancercenter.com/community/blog/2019/07/whats-the-difference-female-male-breast-cancer#:~:text=About%201%20percent%20of%20all,diagnosed%20in%20the%20United%20States.
Cleveland Clinic. (2013). Chemotherapy for breast cancer. Cleveland Clinic. https://my.clevelandclinic.org/health/treatments/8340-chemotherapy-for-breast-cancer
DePolo, J. (2019). Men with breast cancer have lower survival rates than women. Breastcancer.org. https://www.breastcaner.org/reasearch-news/men-with-bc-have-lower-survival-rates
DePolo, J. (2021). Radiation therapy. Breastcancer.org. https://www.breastcancer.org/treatment/radiation
Breastcancer.org. (2012, September 17). Hormonal Therapy for Male Breast Cancer. https://www.breastcancer.org/symptoms/types/male_bc/treatment/hormonal
Male Breast Cancer Coalition. (2017, April 27). MEN’s Breast Self Exam [Video]. Youtube. https://www.youtube.com/watch?v=H5493-Jispw
Mayo Clinic. (2020, February 28). Male Breast Cancer. https://www.mayoclinic.org/diseases-conditions/male-breast-cancer/symptoms-causes/syc-20374740#:~:text=Signs%20and%20symptoms%20of%20male,that%20begins%20to%20turn%20inward
Sanguinetti, A., Polistena, A., Lucchini, R., Monacelli, M., Galassee, S., Avenia, S., Triola, R., Bugiantella, W., Cirocchi, R., Rondelli, F., & Avenia, N. (2016). Male breast cancer, clinical presentation, diagnosis and treatment: twenty years of experience in our breast unit. International Journal of Surgery Case Reports, 20. 10.1016/j.ijscr.2016.02.004
Shin, J., Kachnic, L., & Hirsch, A. (2014). The impact of race in male breast cancer treatment and outcome in the united states: a population-based analysis of 4,279 patients. International Journal of Breast Cancer, 2014. 10.1155/2014/685842
Susan G. Komen. (2020). Breast cancer screening for men at higher risk. https://www.komen.org/breast-cancer/screening/when-to-screen/high-risk-men/
Woods, R., Salkowski, L., Elezaby, M., Burnside, E., Strigel, R., & Fowler, A. (2019). Image-based screening for men at high risk for breast cancer: benefits and drawbacks. Breast Imaging, 60(1), 84-89. 10.1016/j.clinimag.2019.11.005
Yalaza, M., İnan, A., & Bozer, M. (2016). Male breast cancer. Journal of Breast Health, 12(1), 1-8. doi:10.5152/tjbh.2015.2711
the part of the circulatory system that is concerned especially with scavenging fluids and proteins which have escaped from cells and tissues and returning them to the blood, with the phagocytic removal of cellular debris and foreign material, and with the immune response and that consists especially of lymphoid tissue, lymph, and lymph-transporting vessels
an abnormal condition in a male characterized by usually two X and one Y chromosomes, infertility, smallness of the testicles, sparse facial and body hair, and enlarged breasts.
most well known genes linked to breast cancer that can be passed from either parent
A type of imaging test to examine the internal organs using very high frequency sound waves
emission or transmission of energy in the form of waves through space or through material.
