Drew Belsha
Introduction
Male infertility is a multi-faceted health condition. There are various causes, symptoms, and treatments of infertility. In the United States, infertility is defined as not being able to get pregnant after one year or longer of unprotected sex (Centers for Disease Control and Prevention [CDC], 2021). Most attention is put on the female condition when it comes to infertility, but it is important to explore the male side of fertilization to understand where issues could arise.
Studies estimate that infertility affects about 15% of couples worldwide and the male is responsible solely for 20-30% of infertility cases or contribute in some way to 50% of the infertility cases (Agarwal et al., 2015). The rates and prevalence of male infertility vary across regions and borders. Infertility rates ranked highest in Africa and Central/ Eastern Europe (Agarwal et al., 2015). This statistic may not show the true picture due to cultural expectations and societal practices. In some cultures, men are expected to be strong leaders who produce offspring to continue the family name; if this is not possible, this is where some cultural practices step in to assist with procreation such as polygamy. Some cultures regard men so highly that the blame for infertility and lack of children is placed on the female (Agarwal et al., 2015). Determining rates of infertility could also be difficult due to different global health practices and infertility definitions. Other countries determine couples infertile after only a couple months. Male infertility may be regarded differently depending on culture and expectations, but it is important to understand the causes, symptoms, diagnostics, and treatments that accompany infertility to raise awareness around the condition and promote healthy lifestyles for men.
Causes of Infertility
The causes of male infertility may be due to biological issues or physiological issues. Every male body is different in how they function; to understand the individual risk of infertility, a doctor should be consulted to determine the reason.
Sperm cells are fast-growing and are forever being replenished in a healthy male. To get pregnant, a sperm cell must meet with a female egg in the female reproductive tract to fertilize the egg into an embryo and further develop into a fetus. Sperm cells have the possibility of damage during the maturation process since so many are being produced all the time. One of the examined causes for male infertility is oxidative stress. Oxidative stress is the number of free radicals or incomplete molecules present in the body; if these molecules are held in the body for too long, these particles can interfere with body processes. Oxidative stress damages sperm in their earlier stages of maturation. Damaged sperm may still be able to fertilize an egg, although it can still cause birth defects or miscarriage (Bisht et al., 2017).
Men can develop varicoceles, which are similar to a varicose vein, but they are present in the scrotum. Varicoceles enlarge the veins associated with taking oxygen-poor blood away from the scrotum (Jensen et al., 2017). About 15% of healthy men and 35% of men experiencing infertility are diagnosed with a varicocele (Alsaikhan et al., 2016). Varicoceles occur at any time but usually form due to birth defects. If a male has a diagnosed varicocele, it does not mean he is infertile, although varicoceles are the most common correctable cause of male infertility. Semen quality and sperm function are severely impaired by a varicocele. Varicoceles impact sperm production by increasing the internal temperature of the scrotum to levels that are not favorable to producing sperm (Fainberg & Kashanian, 2019). They can be treated by surgery such as a varicocelectomy (Jensen et al., 2017).
Sexually transmitted infections are also responsible for infertility in men. Viruses are able to damage sperm and negatively affect the DNA. The known viruses that harm male reproduction possibilities include hepatitis B, hepatitis C, and human immunodeficiency virus (HIV) (Garolla et al., 2013). If a male is infected with one of these viruses, antiviral drugs may be prescribed which could also affect sperm quality and production in addition to the issues created by the infecting virus. STIs may not be detected by symptoms in men as they are in women, but their sperm can still be damaged which may spread the infection to a partner or to an offspring (Garolla et al., 2013).
Signs of Infertility for Men
Men typically do not know of fertility issues until they are trying to conceive with a partner. Men cannot tell they are infertile without medical tests. A semen analysis is the most common first step in understanding a man’s fertility chances (Chertoff, 2018). With the naked eye, the only issue that could be distinguished from semen is the amount ejaculated. Small volumes of ejaculate could contribute to infertility or trouble conceiving.
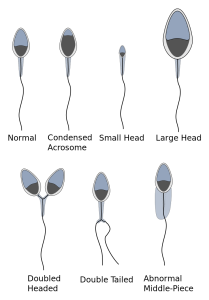
A semen analysis includes a sperm count. A normal sperm count measures from 15 million sperm to more than 200 million sperm per milliliter of semen (Chertoff, 2018). Sperm from the semen analysis is also visualized under a microscope to check for the shape and their motility. Sperm counts are also used to determine the health and wellness of a man; their sperm count reflects health factors such as blood pressure, body mass index and others (Chertoff, 2018).
Diagnosis and Treatment Options
Diagnosis of infertility for men usually starts with a semen analysis. From there, a doctor will decide if medications, surgery, or different types of fertility assistance will be needed to get pregnant. Ultrasound may be conducted to find blockages along the path of sperm maturation. Other testing practices, such as hormone testing and urinalysis, provide insight on where a problem is occurring in terms of a man’s ability to reproduce.
To first combat infertility, a man should be living a healthy lifestyle; including not smoking, regular exercise, a healthy diet, and avoiding alcohol and other drugs. Healthy sperm will make a healthy child; and to have healthy sperm, a man needs to be holistically healthy himself.
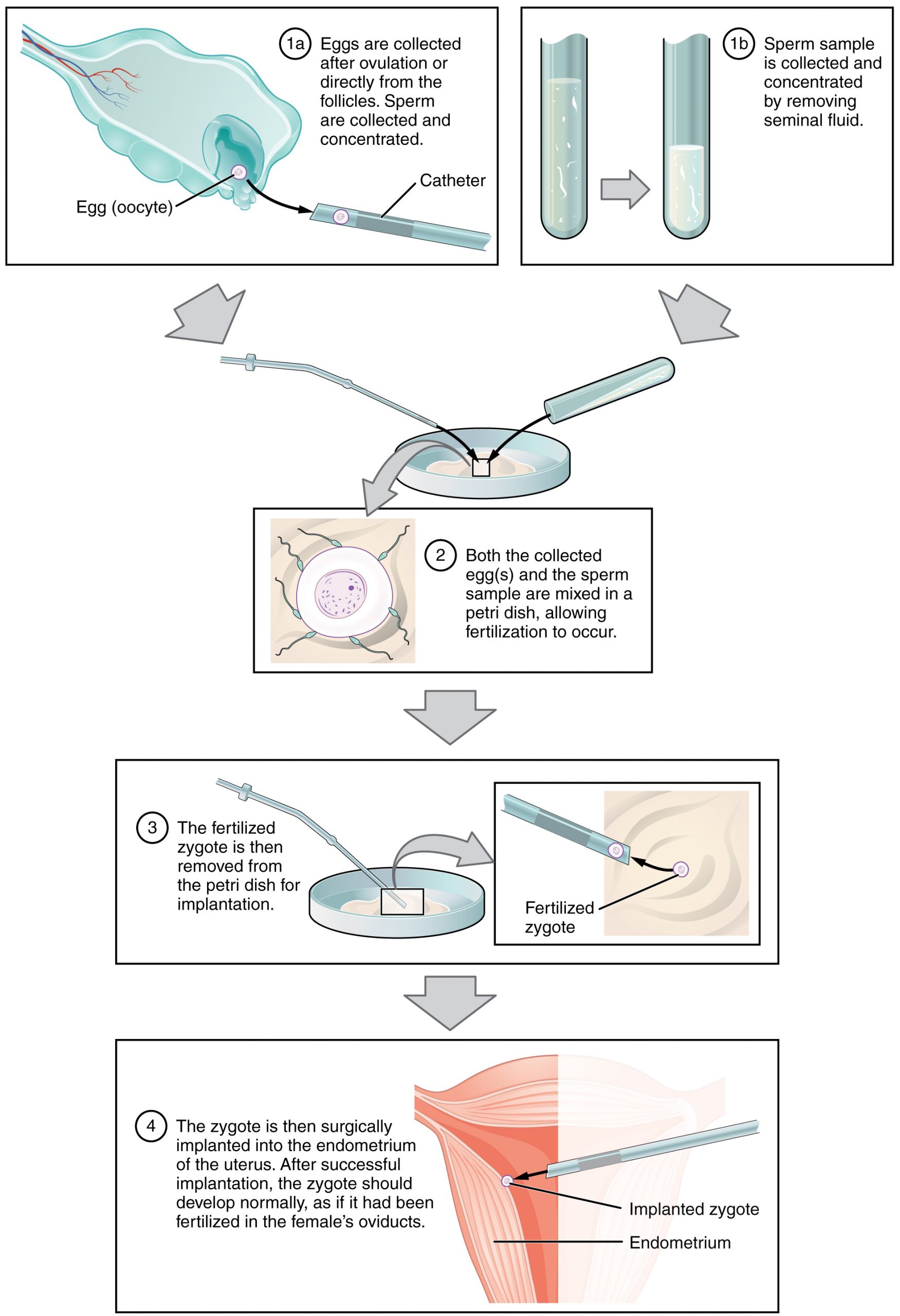
If there is a blockage or varicocele, surgery is the best option to repair the damaged areas of the male reproductive system. Medications such as antibiotics or antivirals could treat infections that affect sperm function. Hormone replacement could fix issues arising from unbalanced hormone levels (Mayo Foundation for Medical Education and Research, 2021). Other options to aid in conceiving include assisted reproductive technology or simply ART. ART treatments involve isolating sperm to artificially fertilize an egg. One treatment commonly used is intracytoplasmic sperm injection; this is used when the sperm has been analyzed as having a hard time penetrating the egg (American Society for Reproductive Medicine, 2014). This procedure can be used along with others to increase the chance of fertilization.
Other Concerns Related to Infertility
The topic of infertility, especially when it concerns men, can be very taboo or difficult to talk about. Doctors and healthcare professionals are there to help with this condition and process without judgment. They are also great sources of finding support groups or mental health specialists to assist with any concern. Studies have found that men dealing with an infertility diagnosis to be more likely to suffer from depression and anxiety (Miner et al., 2018). The same study suggested that online support groups may be a comfortable meeting place for men to meet others who are going through the same pressures. Society seems to demand unfair expectations from men and sees masculinity as being strong and hiding emotions. Masculinity is not defined by being able to have children naturally, therefore the stigma needs to be changed. Multi-dimensional health, including mental, emotional, and physical health is masculine. All-around health and wellness will also aid in the possibility of fertility.

Chapter Review Questions
1. How is male infertility defined in the US?
A. Not being able to get pregnant after 1 time of unprotected sex
B. Not being able to get pregnant after 1 year of unprotected sex
C. Not being able to get pregnant after 6 months of unprotected sex
D. Not being able to get pregnant after 1 year of protected sex
2. At what age of sperm maturity does oxidative stress have an impact on fertility?
A. Late stages
B. Right before ejaculation
C. Early stages
3. What is the most common or first step diagnostic test that helps diagnose male infertility?
A. Prostate exam
B. Urinalysis
C. Semen analysis
D. Ultrasound
Resources
Agarwal, A., Mulgund, A., Hamada, A., & Chyatte, M. R. (2015). A unique view on male infertility around the globe. Reproductive Biology and Endocrinology: RB&E, 13 (37). 10.1186/s12958-015-0032-1
Alsaikhan, B., Alrabeeah, K., Delouya, G., & Zini, A. (2016). Epidemiology of varicocele. Asian Journal of Andrology, 18(2), 179-181. 10.4103/1008-682X.172640
American Society for Reproductive Medicine. (2014). What is intracytoplasmic sperm injection (ICSI)?. Reproductive facts. https://www.reproductivefacts.org/news-and-publications/patient-fact-sheets-and-booklets/documents/fact-sheets-and-info-booklets/what-is-intracytoplasmic-sperm-injection-icsi/
Batiha, O., Al-Deeb, T., Al-Zoubi, E., & Alsharu, E. (2020). Impact of COVID-19 and other viruses on reproductive health. Andrologia, 52(9), e13791. https://doi.org/10.1111/and.13791
Bisht, S., Faiq, M., Tolahunase, M., & Dada, R. (2017). Oxidative stress and male infertility. Nature Reviews Urology, 14(8), 470-485. 10.1038/nrurol.2017.69
Centers for Disease Control and Prevention. (2021, April 13). Infertility FAQs. https://www.cdc.gov/reproductivehealth/infertility/index.htm#:~:text=In%20general%2C%20infertility%20is%20defined,6%20months%20of%20unprotected%20sex
Chertoff, J. (2018, August 29). What is a normal sperm count? Healthline. https://www.healthline.com/health/mens-health/normal-sperm-count
Fainberg, J., & Kashanian, J. A. (2019). Recent advances in understanding and managing male infertility. F1000 Research, 8, F1000 Faculty Rev-670. 10.12688/f1000research.17076.1
Garolla, A., Pizzol, D., Bertoldo, A., Menegazzo, M., Barzon, L., & Foresta, C. (2013). Sperm viral infection and male infertility: Focus on HBV, HCV, HIV, HPV, HSV, HCMV, and AAV. Journal of Reproductive Immunology, 100(1), 20-29. 10.1016/j.jri.2013.03.004
Jensen, C. F. S., Østergren, P., Dupree, J. M., Ohl, D. A., Sønksen, J., & Fode, M. (2017). Varicocele and male infertility. Nature Reviews Urology, 14(9), 523-533. 10.1038/nrurol.2017.98
Mayo Foundation for Medical Education and Research. (2021, April 13). Male Infertility. Mayo clinic. https://www.mayoclinic.org/diseases-conditions/male-infertility/diagnosis-treatment/drc-20374780
Miner, S. A., Daumler, D., Chan, P., Gupta, A., Lo, K., & Zelkowitz, P. (2018). Masculinity, mental health, and desire for social support among male cancer and infertility patients. American Journal of Men’s Health, 13(1) 1557988318820396. 10.1177/1557988318820396
The proportion of a population who have a specific characteristic in a given time period.
to beget or bring forth offspring
marriage in which a spouse of either sex may have more than one mate at the same time
characteristic of or appropriate to an organism's healthy or normal functioning
the entire process by which diploid gamete-producing cells are transformed into haploid gametes that includes both meiosis and physiological and structural changes
an especially reactive atom or group of atoms that has one or more unpaired electrons
especially : one that is produced in the body by natural biological processes or introduced from an outside source (such as tobacco smoke, toxins, or pollutants) and that can damage cells, proteins, and DNA by altering their chemical structure
surgical treatment of varicocele by excision of the affected veins often with removal of part of the scrotum
the quality or state of being motile : capability of movement
A type of imaging test to examine the internal organs using very high frequency sound waves
chemical analysis of urine
relating to or concerned with wholes or with complete systems rather than with the analysis of, treatment of, or dissection into parts
injection by a microneedle of a single sperm into an egg that has been obtained from an ovary followed by transfer of the egg to an incubator where fertilization takes place and then by introduction of the fertilized egg into a female's uterus —abbreviation ICSI
